Abstract
Objective. To compare the clinical outcomes associated with successful percutaneous coronary intervention (PCI) versus initial medical therapy (MT) in patients with coronary chronic total occlusions (CTOs). Methods. Between January 2007 and December 2016, a total of 1702 patients with ≥1 CTO were enrolled. Patients who had a failed CTO-PCI were excluded. After exclusion, 1294 patients with 1520 CTOs were divided into the MT group initially (did not undergo a CTO-PCI attempt) (n = 800) and successful PCI group (n = 494). Propensity-score matching was also performed to adjust for baseline characteristics. The primary outcome was cardiac death. Results. The median overall follow-up duration was 3.6 (IQR, 2.1–5.0) years, there was no significant difference between the two groups with respect to the prevalence of cardiac death (MT vs. successful PCI: 6.6 vs. 3.8%, adjusted hazard ratio [HR] 0.93, 95% confidence interval [CI] 0.41–2.14, p = .867). In the propensity-matched population (286 pairs), there were no significant differences in the prevalence of cardiac death (MT vs. successful PCI: 5.9% vs. 3.1%, HR 0.51, 95% CI 0.23–1.15, p = .104) and major adverse cardiovascular events (MACE) (HR 0.76, 95% CI 0.53–1.09, p = .130) between the two groups. Conclusion. In the treatment of patients with CTOs, successful PCI is not associated with improved long-term cardiovascular survival or reduced the risk of MACE compared with MT alone initially.
Introduction
Percutaneous coronary intervention (PCI) of coronary chronic total occlusion (CTO) remains one of the most challenging scenarios for interventional cardiologists despite the advent of equipment and techniques [Citation1]. Several studies have reported that successful revascularization is associated with symptomatic relief of angina, as well as improved left ventricular function, long-term survival, and quality of life [Citation2–6]. However, only approximately 13.6–35% of CTOs are currently treated by revascularization [Citation7,Citation8], mainly because CTO-PCI procedures may be with elevated radiation exposure, lower procedural success rate, a higher expense and risk of complication when compared with non-CTO elective PCI [Citation9,Citation10]. Therefore, some clinicians are more likely to treat patients who have CTO with medical therapy (MT) alone. However, to date, most studies focused on the clinical outcomes of successful CTO revascularization compared with failed PCI, and few studies have compared the clinical outcomes of patients with CTOs who undergo successful CTO-PCI versus those who only undergo MT and did not undergo a CTO-PCI attempt, a population that has not been considered previously [Citation11]. Therefore, this study aimed to compare the clinical outcomes associated with successful CTO-PCI versus MT initially in patients with CTOs.
Methods
Study population
A total of 16224 patients who underwent diagnostic coronary angiography from January 2007 to December 2016 were included at the First Affiliated Hospital of Dalian Medical University (Dalian, China). Of these patients, 1702 had at least one CTO. Those who underwent previous CABG, developed acute ST-segment elevation myocardial infarction during the preceding 48 h, underwent CABG and failed CTO-PCI were excluded. Thus, 1294 patients with at least one CTO were included for analysis. The subjects were assigned to a MT group or successful CTO-PCI group according to the initial treatment strategy. Revascularization or MT was selected according to the presence of symptoms, high co-morbidity or high risk for revascularization, indication of heart surgery (SYNTAX score >22 with/without valve disease), the suitability of the target distal vessel for revascularization (diameter >2.0 mm and non-negligible distal bed length) [Citation12] and patients’ economic burden. The cost of CTO-PCI was thirty to fifty thousand yuan (nearly 4.3–7.2 thousand dollars) in our hospital. The baseline clinical, laboratory, and angiographic characteristics were collected from the database and medical records. Follow-up was obtained from clinical hospital records or telephone interviews. The institutional review board approved the present study.
Definitions and study outcomes
A “CTO lesion” was defined as an obstruction of a native coronary artery with a thrombolysis in myocardial infarction (TIMI) flow grade of 0, and an estimated duration of >3 months [Citation2]. For patients with more than one CTO, only one CTO vessel was targeted and no further attempt was made during the study period. “PCI success” was defined as stent placement with residual stenosis of <20% and TIMI flow grade of ≥2 after PCI as visually estimated from an angiogram. The “primary outcome” was cardiac death during follow-up. The secondary outcome was myocardial infarction (MI), and target vessel revascularization (TVR) and major adverse cardiac event (MACE). “MACE” was defined as the composite of cardiac death, MI, and TVR. All-cause deaths were considered to be of cardiac cause unless a definite noncardiac cause could be established. “Cardiac death” was considered to be of cardiac origin unless a definite non-cardiac cause could be established. MI was defined as recurrent symptoms with new electrocardiographic changes compatible with MI or cardiac markers at least twice the upper limit of normal [Citation13]. TVR was defined as the repeated revascularization of the CTO vessel. “Chronic kidney disease (CKD)” was defined as a creatinine clearance rate of <60 ml/min. All patients underwent two-dimensional echocardiography.
Statistical analysis
Continuous variables were compared using the Student's t-test or Mann–Whitney U test, where applicable, and are presented as the mean ± standard deviation or median and interquartile range (IQR). Categorical data were tested using the chi-square test or Fisher's exact test, as appropriate, and are presented as percentages. To reduce the risk of bias in treatment selection and any other related potential confounding factor, baseline characteristics were adjusted using propensity scores. The latter were estimated using multiple logistic regression analyses. Event-free survival during follow-up was evaluated according to the Kaplan–Meier method and compared with the log-rank test. Covariates that were significant on univariate analysis or clinically relevant were included in multivariate models. Adjusted hazard rates were compared by Cox regression based on age, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), previous MI, CKD, left ventricular ejection faction (LVEF), hard to afford cost, taking clopidogrel, CTO of the left anterior descending coronary artery (LAD) and left circumflex coronary artery, blunt stump, calcification, Japanese-chronic total occlusion (J-CTO) score and SYNTAX score. A full non-parsimonious model was developed that included all the variables listed in and . All tests were two-tailed. A p value of <.05 was considered significant. All analyses were conducted using Stata V.13 software (StataCorp LLC, College Station, TX, USA)
Table 1. Baseline clinical characteristics in the MT and successful PCI groups.
Table 2. Angiographic characteristics in the MT and successful PCI groups.
Results
Baseline characteristics
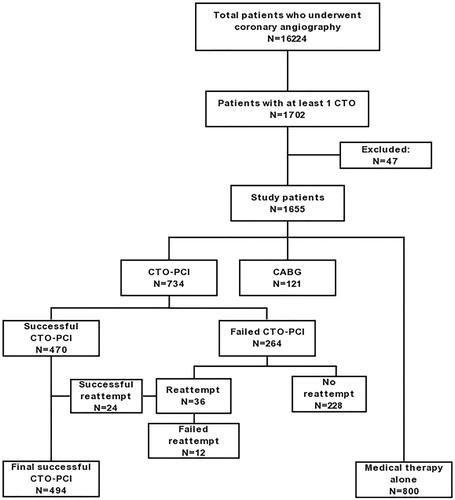
After exclusion, a total of 1294 patients with 1520 CTOs were enrolled in this study. The overall prevalence of CTO was 10.5%. A CTO was treated by MT in 800 patients and 734 underwent PCI. In the PCI group, 470 patients had successful PCI and 264 patients had a failed PCI. Additionally, of the 264 patients in the failed CTO-PCI group, 36 patients underwent repeated CTO-PCI procedures, and 24 patients got successful CTO-PCI (). Therefore, there were a total of 494 patients in successful PCI group and 800 patients in MT group. Regarding the CTO lesions, most CTO target lesions were located in the right coronary artery (RCA) (41.7%), followed by the LAD (30.2%) and the circumflex (24.0%). 76% of cases were located in the proximal or middle portion of the coronary arteries.
Figure 1. Flow chart of the study population. CABG: coronary artery bypass grafting; CTO: chronic total occlusion; PCI: percutaneous coronary intervention.
and show the baseline and angiographic characteristics of the enrolled patients. As compared with patients in successful PCI group, those in MT group were older and more often had previous MI, CKD, hard to afford cost, CTO of left circumflex coronary artery, blunt stump calcification, with high TC, LDL-C, J-CTO score and SYNTAX score, but low LVEF; whereas they were less likely to take clopidogrel and to have CTO of the LAD.
286 matched pairs of patients were created after undertaking propensity score-matching for the entire population. No significant differences were observed in baseline characteristics between the MT and successful PCI groups in the propensity-score matched population.
Clinical outcomes
The median overall follow-up duration was 3.6 (IQR, 2.1–5.0) years. The follow-up was available for 88.7% of patients. Thirty-one noncardiac deaths were caused by malignant tumor (14 patients), stroke (6 patients), multiple organ failure (5 patients), severe respiratory disease (3 patients) and accident (3 patients). The other seventy-two patients were considered cardiac deaths. A higher prevalence of cardiac death was observed in patients referred for MT (MT vs. successful PCI: 6.6 vs. 3.8%, unadjusted hazard ratio [HR] 0.57, 95% confidence interval [CI] 0.34–0.97, p=.038) than those referred for successful PCI. After multivariate analyses, Cox regression analyses showed no significant differences in the terms of cardiac death (adjusted HR 0.93, 95% CI 0.41–2.14, p=.867), all-cause death (adjusted HR 0.89, 95% CI 0.42–1.97, p=.726), MI (adjusted HR 0.91, 95% CI 0.40–2.09, p=.832) and MACE (adjusted HR 1.51, 95% CI 0.93–2.46, p=.099) between the two groups, whereas the rate of TVR (HR 1.94, 95% CI 1.02–3.70, p=.044) was significantly higher in the MT group than in the successful PCI group () ().
Figure 2. Kaplan–Meier curves for cardiac death (A), myocardial infarction (MI) (B), target-vessel revascularization (TVR) (C), and major adverse cardiovascular events (MACE) (D) in total patients. MT: medical therapy; PCI: percutaneous coronary intervention.
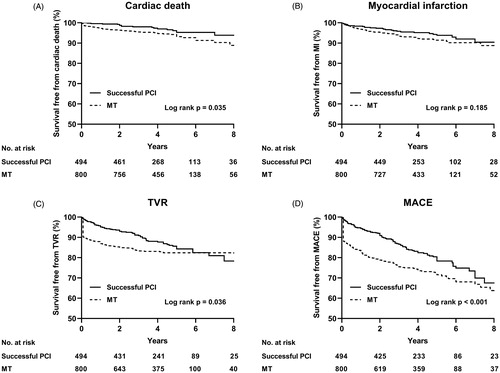
Table 3. Clinical outcomes in all patients during follow-up.
In propensity-matched patients, there were no significant differences between the two groups with respect to the incidence of cardiac death (MT vs. successful PCI: 5.9% vs. 3.1%, HR 0.51, 95% CI 0.23–1.15, p=.104), all-cause death (HR 0.55, 95% CI 0.21–1.23, p=.135), MI (HR 0.92, 95% CI 0.49–1.74, p=.800), TVR (HR 0.84, 95% CI 0.54–1.31, p=.449) and MACE (HR 0.76, 95% CI 0.53–1.09, p=.130) between the two groups () ().
Figure 3. Kaplan–Meier curves for cardiac death (A), myocardial infarction (MI) (B), target-vessel revascularization (TVR) (C) and major adverse cardiovascular events (MACE) (D) in propensity-matched patients. MT: medical therapy; PCI: percutaneous coronary intervention.
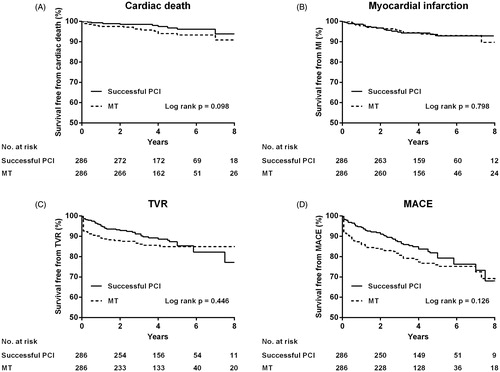
Table 4. Clinical outcomes in propensity-matched patients during the follow-up.
To reduce the impact of different target-vessels on clinical outcomes, we done a subgroup analysis. Among each target-vessel, there was no significant difference in the prevalence of cardiac death between the MT and successful PCI groups ().
Table 5. Clinical outcomes in all patients during follow-up according to each target-vessel.
Discussion
We compared the long-term clinical outcomes of medical therapy versus successful PCI in patients with CTO. The main findings of the present study are (1) successful CTO-PCI compared with initial MT alone was not associated with reducing risk of cardiac death or MACE; (2) patients who underwent MT had a higher prevalence of target-vessel revascularization.
Owing to the development of equipment and techniques, PCI of CTOs has achieved high technical and procedural success rates with a low risk for procedural complications [Citation14,Citation15]. Nevertheless, more than half of all CTO patients were not managed by PCI [Citation7]. According to the DECISION-CTO (Drug-Eluting Stent Implantation Versus Optimal Medical Treatment in Patients with Chronic Total Occlusion) and the EuroCTO (Randomized Multicenter Trial to Evaluate the Utilization of Revascularization or Optimal Medical Therapy for the Treatment of Chronic Total Coronary Occlusions), PCI does not associate with significantly lesser risks for major adverse cardiac events, death, and repeated revascularization, as compared with medical therapy alone [Citation16,Citation17]. Furthermore, clinicians are more concerned about the clinical outcomes of the CTO patients who underwent successful PCI or treated by medication. However, to date, there was little data on long-term clinical outcomes of initial MT in CTO patients compared with successful PCI.
In the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial, PCI was not superior to MT as an initial strategy in patients with stable coronary artery disease (CAD) [Citation18]. Similarly, our study also showed successful CTO-PCI did not associate with reducing the prevalence of cardiac death. Probably because a majority of patients in our study had stable CAD, and similar study population were also included in the COURAGE trial.
A lot of studies compared the clinical outcomes of successful CTO-PCI and failed PCI in patients with CTOs, and have suggested a better outcome with respect to successful revascularization [Citation5,Citation19]. In our study, patients in the MT group did not undergo a CTO-PCI attempt before, a population that has not been considered previously [Citation11]. Hence, in contrast to previous studies, our study better reflects the clinical significance and overall risk of compared with MT alone in CTO patients.
In the present study, patients in the MT group tended to be older and more often had lesion in the left circumflex coronary artery, blunt stump, calcification, high J-CTO score and SYNTAX score. Furthermore, they also had a lower LVEF (i.e. worse cardiac function). These data are in accordance with previous study [Citation20]. Therefore, a substantial portion of these CTO patients were unsuitable for PCI.
To reduce the impact of confounding factors, we performed a propensity score-matching and the results showed that successful PCI is not associated with improved long-term cardiovascular survival or reduced the prevalence of MACE, as compared with MT alone, consistent with the finding of Lee and colleagues [Citation21]. We also done a subgroup analysis and successful CTO-PCI didn’t reduce cardiac death compared with initial MT among each target-vessel. Our previous study also suggests that successful CTO-PCI didn’t reduce cardiac death compared with MT [Citation22]. These findings suggest that, considering the incidence of PCI-related complications, prognosis and high expense, aggressive CTO-PCI should be considered carefully.
There were several limitations of our study. First, this was observational study and selection bias could have occurred, even though propensity score-matched analysis was performed. Second, the amount of viable myocardium or ischemia of study patients was not routinely evaluated.
In conclusion, in the treatment of patients with CTOs, successful PCI is not associated with improved long-term cardiovascular survival or reduced the risk of MACE compared with initial medical therapy alone. Aggressive CTO-PCI should be considered carefully.
Acknowledgements
We acknowledge and thank Ying Liu, Kun Chen, and Haichen Lv for their invaluable assistance.
Disclosure statement
The authors report no conflicts of interest to declare.
Additional information
Funding
References
- Freeman PF, Rasmussen JG, Villadsen AB, et al. Chronic total coronary occlusion: treatment results. Scand Cardiovasc J. 2017;51:197–201.
- Sianos G, Werner GS, Galassi AR, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. 2012;8:139–145.
- Sirnes PA, Myreng Y, Mølstad P, et al. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur Heart J.1998;19:273–281.
- Valenti R, Migliorini A, Signorini U, et al. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur Heart J. 2008;29:2336–2342.
- George S, Cockburn J, Clayton TC, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol. 2014;64:235–243.
- Wijeysundera HC, Norris C, Fefer P, et al. Relationship between initial treatment strategy and quality of life in patients with coronary chronic total occlusions. EuroIntervention. 2014;9:1165–1172.
- Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian multicenter chronic total occlusions registry. J Am Coll Cardiol. 2012;59:991–997.
- Grantham JA, Marso SP, Spertus J, et al. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv. 2009;2:479–486.
- Suzuki S, Furui S, Kohtake H, et al. Radiation exposure to patient's skin during percutaneous coronary intervention for various lesions, including chronic total occlusion. Circ J. 2006;70:44–48.
- Gada H, Whitlow PL, Marwick TH. Establishing the cost-effectiveness of percutaneous coronary intervention for chronic total occlusion in stable angina: a decision-analytic model. Heart. 2012;98:1790–1797.
- Godino C, Bassanelli G, Economou FI, et al. Predictors of cardiac death in patients with coronary chronic total occlusion not revascularized by PCI. Int J Cardiol. 2013;168:1402–1409.
- Azzalini L, Jolicoeur EM, Pighi M, et al. Epidemiology, management strategies, and outcomes of patients with chronic total coronary occlusion. Am J Cardiol. 2016;118:1128–1135.
- Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions: a case for standardized definitions. Circulation. 2007;115:2344–2351.
- Galassi AR, Tomasello SD, Reifart N, et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7:472–479.
- Konstantinidis NV, Sofidis G, Kolettas V, et al. Bifurcation CTO recanalization with contemporary antegrade and retrograde techniques in a patient with two chronically occluded coronary arteries. Hellenic J Cardiol. 2016;57:371–374.
- Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39:2484–2493.
- Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion: the DECISION-CTO trial. Circulation. 2019;139:1674–1683.
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503–1516.
- Jones DA, Weerackody R, Rathod K, et al. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc Interv. 2012;5:380–388.
- Yang JH, Kim BS, Jang WJ, et al. Optimal medical therapy vs. percutaneous coronary intervention for patients with coronary chronic Total occlusion: a propensity-matched analysis. Circ J. 2016;80:211–217.
- Lee PH, Lee SW, Park HS, et al. Successful recanalization of native coronary chronic total occlusion is not associated with improved long-term survival. JACC Cardiovasc Interv. 2016;9:530–538.
- Guo L, Zhong L, Chen K, et al. Long-term clinical outcomes of optimal medical therapy vs. successful percutaneous coronary intervention for patients with coronary chronic total occlusions. Hellenic J Cardiol. 2018;59:281–287.
