Abstract
Objectives. The One-minute Sit-To-Stand Test (STST) is a relatively novel physical performance test in the field of pulmonology. It measures the exercise tolerance of the patient. In this pilot study, we evaluated its predictive value for the postoperative course in cardiac surgery patients. Design. This was a prospective observational cohort study of patients undergoing elective aortic valve replacement. STST was applied in the patients, along with pulmonary function testing, a day prior to surgery, on postoperative day 7, and 3 months after surgery. A Short Form-36 health related quality of life survey (SF-36) was also included. The patients were divided into two groups according to the preoperative STST outcome: group A (≤20 repetitions, n = 12), and group B (>20 repetitions, n = 18). Results. We enrolled 30 patients in the study between May 2017 and May 2019. No complication were observed during the STST. The standard perioperative measures were identical for both groups. However, group A exhibited a significantly longer artificial ventilation time, as well as worse pulmonary function (VC, FVC, TLCO), on postoperative day 7. Concerning the SF-36, group A displayed a worse pre- and postoperative evaluation in both physical functioning and vitality. Conclusions. STST is a short and practical physical performance test that could enable a better prediction of the postoperative course after cardiac surgery. Patients with lower preoperative STST performance may require longer postoperative artificial ventilation, as they may present worse in some parameters of pulmonary functions and quality of life. However, these findings must be corroborated in larger studies.
Introduction
The One-minute Sit-to-Stand test (STST) is a relatively novel physical performance test that is currently popular in the field of pulmonology [Citation1–4]. It has been used to measure the impact of respiratory rehabilitation on the exercise tolerance and the activities of daily living in patients with chronic obstructive pulmonary disease [Citation5]. STST has shown a comparable assessment potential for exercise tolerance to the more traditional Six-Minute Walk test (6MWT) [Citation6,Citation7]; however, it requires less time and space. To the best of our knowledge, this test has not yet been applied in cardiac surgery patients.
As proven by the 6MWT and 5-meter gait speed test, the addition of a physical performance test to standard risk prediction scores (EuroScore or STS score) may provide more insight into the prognosis and postoperative course of cardiac surgery patients [Citation8,Citation9].
In this pilot study, we applied STST in the field of cardiac surgery for the first time. The primary aim was to examine its potential to predict the postoperative course. The secondary aim was to evaluate the dynamics of exercise tolerance after cardiac surgery and to analyze relationship of STST with pulmonary function and quality of life.
Material and methods
The present analysis is based on a prospective observational cohort study of elderly patients undergoing elective biological aortic valve replacement (AVR) at our institution. The inclusion criteria were as follows: (i) indication for AVR, (ii) >65 years of age. The exclusion criteria were: (i) re-do surgery and (ii) concomitant cardiac surgery. Informed consent was obtained from all individual participants. The study was approved by the Instituteʼs Ethics Committee. STST, pulmonary function testing (PFT), and the Short Form-36 health related quality of life survey (SF-36) were performed a day prior to surgery. Both STST and PFT were repeated on postoperative day 7, after which the patients were discharged (if appropriate). A full control evaluation (STST, PFT and SF-36) was performed in our outpatient department 3 months after the surgery.
According to previous studies, 20 STST repetitions were set as a cut off value between normal and low exercise tolerance [Citation10–13]. The patients were divided into two groups according to the preoperative STST outcome: group A (≤20 repetitions); group B (>20 repetitions).
One-Minute sit-to-Stand test
The STST was performed in strict conditions [Citation14]. In brief, the patient was seated in a 46 cm high chair with his, or her, feet touching the ground and hands placed on the hips to prevent cheating. The patient was then instructed to perform as many stand up/sit down repetitions as possible in one minute (see ). The test started after a 3 s countdown. The examiner informed the patient verbally about the current number of repetitions after each set of 5. The patient was instructed to stop immediately in case of exhaustion or discomfort of any kind. The data were recorded by two examiners (JG and MV).
Pulmonary function testing
Spirometry, bodyplethysmography, and transfer factor assessment were performed according to the American Thoracic Society/European Respiratory Society guidelines [Citation15]. The results are expressed as percentage of the predicted values for adults. We examined the following parameters: obstruction: forced expiratory volume in the first second (FEV1), forced expiratory volume in the first second divided by vital capacity (FEV1/VC), Tiffeneau-Pinelli index–forced expiratory volume in the first second divided by forced vital capacity (FEV1/FVC), maximal expiratory flow at 50% of vital flow capacity (MEF50%), airway resistance (Raw); restriction: vital capacity (VC), forced vital capacity (FVC), total lung capacity (TLC); pulmonary hyperinflation: residual volume (RV), residual volume divided by total lung capacity (RV/TLC); diffusion: transfer factor of the lung for carbon monoxide (TLCO), transfer coefficient of the lung for carbon monoxide (KCO). All the measurements were performed by a respiratory technician in a single device (Bodystyk and Diffustik, Geratherm Respiratory GmbH, Bad Kissingen, Germany) and evaluated by a highly experienced respiratory physician (VK).
Surgery and perioperative care
Aortic valve replacement was performed through full sternotomy (n = 17) or upper hemisternotomy (i.e. ministernotomy, n = 13) approach. The surgical procedure itself was performed in the standard fashion, i.e. the native aortic valve was completely excised, the annulus was decalcified (if necessary) and the bioprosthesis (Crown PRT, LivaNova, London, UK) was implanted using double pledgetted interrupted stitches. The patient was weaned from the cardiopulmonary bypass, chest tubes were introduced, and the sternum was closed using steel wires.
After surgery, the patient was transported to the intensive care unit (ICU) and extubated when the standard extubation criteria of our department were met: patient awareness, <50mL/hour chest tube drainage, >35.5 °C core temperature, hemodynamic stability (>2.2 l/min/m2 cardiac index; stable blood pressure (100–140 systolic torr) with or without vasoactive support, <120 beats per minute, no arrhythmias), satisfactory arterial blood gases on full ventilation (PaO2/FiO2 >150 torr, PCO2 <50 torr, pH 7.30–7.50). The chest tubes were extracted on postoperative day 2. As soon as the patient did not require vasoactive support, he, or she, was transported to the standard ward and discharged soon afterwards.
Statistical analysis
All the calculations were done with the NCSS 11 Statistical Software (2016, Kaysville, Utah, USA). The data are shown as either categorical or continuous variables. The categorical variables are expressed as numbers and percentages. The continuous variables are expressed as median and interquartile range. The quantitative variables were tested by a Two-sample Student’s t-test for normally distributed variables and Mann-Whitney U or Kolmogorov-Smirnov tests for non-normally distributed variables. The categorical data were tested by Pearson’s Chi-square or Fisher’s exact tests. Perioperative dynamics of STST outcomes were evaluated by a Paired Student’s t-test or Wilcoxon’s test.
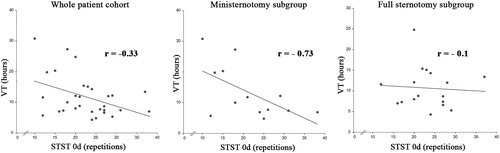
A Spearman’s correlation was performed to determine the relationship between the preoperative STST outcome and artificial ventilation time. The correlation analysis was performed in full sternotomy and ministernotomy subgroups separately, as well. The strength of relationship is expressed as a correlation coefficient. A p value of <.05 was considered statistically significant for all tests.
Results
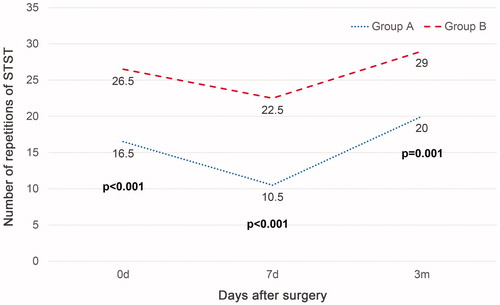
Between May 2017 and May 2019, 30 patients were enrolled in the study. All of them completed their postoperative follow-up. We recorded a significant early postoperative drop in STST outcome in both groups (p = .02 for group A; p = .003 for group B), later improving to preoperative values 3 months after surgery (p = .13 for group A; p = .17 for group B) (see ). No cases of chest pain, dyspnea or other complications were recorded during STST. However, three patients (2 from group A and one from group B) were unable to perform the test on postoperative day 7. Therefore, we recorded its value as zero. In other instances, some of the patients were unable to perform the test without interruption, particularly so on postoperative day 7. The most common reason for this occurrence was knee or hip joint stiffness.
Figure 2. One-minute sit-to-stand test outcomes dynamics. 0d: preoperative measurement; 7d: measurement on the postoperative day 7; 3m: measurement 3 months after surgery.
The preoperative data are shown in . No significant difference was observed in standard preoperative measures between the groups. Concerning both operative and postoperative data, group A had a significantly longer artificial ventilation time (VT) than group B. No other significant difference was recorded in perioperative measures, as seen in . The mortality rate was zero in our cohort.
Table 1. Preoperative patient data.
Table 2. Operative and postoperative patient data.
Both groups had comparable pulmonary function preoperatively. However, group A had significantly lower FVC and TLCO on postoperative day 7 and lower VC 3 months after surgery in comparison with group B. Regarding the SF-36, group B did better than group A in the categories of physical functioning and vitality (both pre- and postoperative), pain (preoperative) and social functioning (postoperative) (see ). A complete list of STST, PFT and SF-36 results has been included in the Supplementary data.
Table 3. One-minute Sit-to-stand test and significant pulmonary function and quality of life testing outcomes.
Because of the significant difference in the VT between the groups, we analyzed the relationship between preoperative STST outcome and postoperative VT outcomes (). An r value of −0.33 indicated a negative correlation between these variables. Subsequently, we performed a separate analysis of full sternotomy and ministernotomy subgroups. In the former, the correlation coefficient was r = −0.1, whereas in the latter it was r = −0.73, thus showing a stronger association in the ministernotomy subgroup.
Discussion
Relatively novel, the STST physical performance test has been implemented in clinical practice to assess the exercise tolerance of patients with pulmonary disease [Citation1,Citation2,Citation5,Citation7,Citation14]. The reference value for a healthy elderly population ranges between 20 and 35 repetitions per minute [Citation10–13]. With this in mind, we set 20 repetitions as a cut off value to easily discriminate the patients with good exercise tolerance from those with low. To the best of our knowledge, STST has not been used in cardiac surgery patients before.
This pilot study demonstrates that STST can be applied to an elective patient indicated for AVR without severe complications. However, since all of the patients in the cohort survived, we were unable to determine its ability to predict mortality. Regardless, STST may be used to predict VT length, which has not been observed with other physical performance tests [Citation16,Citation17]. The negative correlation between STST and VT was stronger in the minimally invasive subgroup of patients, suggesting that such approach is more predictable and that STST could be beneficial in the application of the Early Recovery After Surgery protocol (ERAS). Nevertheless, it must be kept in mind that this is only a pilot study with a reduced number of participants, these preliminary results must be validated in future studies.
Risk prediction plays an important role in the decision process and in the treatment of cardiac surgery candidates. The standard scoring systems (e.g. EuroScore II or STS score) focus on mortality and are thus unable to predict morbidity and the postoperative course [Citation18,Citation19]. Arenaza et al. demonstrated that the addition of 6MWT to the standard EuroScore II can provide useful prognostic information about the patient [Citation8]. In this context, several authors refer to frailty, which is defined as a vulnerability of patient to stressors due to the absence of physical reserves [Citation20]. The evaluation of frailty might predict the postoperative course of the patient [Citation9,Citation20,Citation21]. According to Fried et al., a patient is considered as frail when at least three of the following criteria are met: unintentional weight loss (10 lbs in the previous year), self-reported exhaustion, weakness (grip strength), slow walking speed, and low physical activity [Citation22]. Sundermann et al. proposed a comprehensive assessment of frailty able to predict the perioperative, as well as one-year mid-term, prognosis of the patient [Citation18,Citation19,Citation21]. There is strong evidence suggesting that frailty can be assessed with a 5-meter gait speed test [Citation9,Citation23], which may be used alone or in combination with a well-known risk prediction model, STS score. Proposed by Afilalo et al., the test has a strong potential to predict the outcome in both early and midterm postoperative periods [Citation16,Citation17]. Apart from it, there are several other physical performance tests that may be used: 5-times sit to stand test [Citation24], 30-seconds sit to stand test [Citation6], one repetition maximum test, one leg heel rise test [Citation4] etc. None of these tests have been used, or at least not extensively, in cardiac surgery, regardless of their ability to predict the postoperative course.
Even though there may be a logical connection between exercise tolerance and frailty, STST cannot evaluate any of the Friedʼs frailty criteria and therefore should not be referred to as a frailty test. Nevertheless, as cardiac surgery remains a strong stressor for the organism, exercise tolerance tests could be at least as good in the prediction of the postoperative course as any from the above-mentioned frailty tests. However, the observations made in the present report remain to be validated.
Limitations
The main limitation of our study was the low number of patients included; a limitation set by its nature as a pilot study. For the same reason, our study does not include a direct comparison with any other physical performance tests. Future studies are needed to confirm our preliminary findings and determine “which test is the best”. We included only low risk patients undergoing isolated AVR, the outcomes must be verified on greater range of patients and procedures. Although the comparison of the respective subgroups did not show a significant difference in the outcome, using only one surgical approach could improve the prediction accuracy of STST.
Conclusion
The one-minute sit-to-stand test is a short and practical physical performance test that may have potential to predict the early postoperative course of cardiac surgery patients. A lower preoperative STST performance might be associated with longer postoperative VT, as the patients with higher STST results have better postoperative pulmonary function (i.e. the parameters of restriction and diffusion) and they report better physical functioning and vitality according to the quality of life evaluation. Exercise tolerance is reduced in the first postoperative week; however, it returns to preoperative values after 3 months. Regardless, the results observed in the present study should be validated in larger studies.
Supplemental Material
Download MS Word (17.7 KB)Acknowledgement
The authors would like to thank the nurses involved in this study for their patience, cooperation and patient care. Special thanks to Dr. Eva Cermakova for conducting the statistical analyses. Thanks to Dr. Daniel Díaz for his assistance in proofreading this manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bohannon RW, Crouch R. 1-minute sit-to-stand test: systematic review of procedures, performance, and clinimetric properties. J Cardiopulm Rehabil Prev. 2019;39(1):2–8.
- Briand J, Behal H, Chenivesse C, et al. The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease. Ther Adv Respir Dis. 2018;12:175346661879302.
- van der Leeden M, Balland C, Geleijn E, et al. In-hospital mobilization, physical fitness, and physical functioning after lung cancer surgery. Ann Thorac Surg. 2019;107(6):1639–1646.
- Segura-Orti E, Martinez-Olmos FJ. Test-retest reliability and minimal detectable change scores for sit-to-stand-to-sit tests, the six-minute walk test, the one-leg heel-rise test, and handgrip strength in people undergoing hemodialysis. Phys Ther. 2011;91(8):1244–1252.
- Vaidya T, de Bisschop C, Beaumont M, et al. Is the 1-minute sit-to-stand test a good tool for the evaluation of the impact of pulmonary rehabilitation? Determination of the minimal important difference in COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:2609–2616.
- Gurses HN, Zeren M, Denizoglu Kulli H, et al. The relationship of sit-to-stand tests with 6-minute walk test in healthy young adults. Medicine. 2018;97(1):e9489.
- Kohlbrenner D, Benden C, Radtke T. The 1-minute sit-to-stand test in lung transplant candidates: an easy-to-use alternative to the 6-minute walk test? Respir Care. 2020;65(4):437–443.
- de Arenaza DP, Pepper J, Lees B, et al. Preoperative 6-minute walk test adds prognostic information to Euroscore in patients undergoing aortic valve replacement. Heart. 2010;96(2):113–117.
- Bagnall NM, Faiz O, Darzi A, et al. What is the utility of preoperative frailty assessment for risk stratification in cardiac surgery? Interact Cardiovasc Thorac Surg. 2013;17(2):398–402.
- Strassmann A, Steurer-Stey C, Lana KD, et al. Population-based reference values for the 1-min sit-to-stand test. Int J Public Health. 2013;58(6):949–953.
- Ritchie C, Trost SG, Brown W, et al. Reliability and validity of physical fitness field tests for adults aged 55 to 70 years. J Sci Med Sport. 2005;8(1):61–70.
- Ozalevli S, Ozden A, Itil O, et al. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respirat Med. 2007;101(2):286–293.
- Rocco CC, Sampaio LM, Stirbulov R, et al. Neurophysiological aspects and their relationship to clinical and functional impairment in patients with chronic obstructive pulmonary disease. Clinics. 2011;66(1):125–129.
- Reychler G, Boucard E, Peran L, et al. One minute sit-to-stand test is an alternative to 6MWT to measure functional exercise performance in COPD patients. Clin Respir J. 2018;12(3):1247–1256.
- Miller MR, Crapo R, Hankinson J, et al. General considerations for lung function testing. Eur Respir J. 2005;26(1):153–161.
- Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56(20):1668–1676.
- Afilalo J, Kim S, O’Brien S, et al. Gait speed and operative mortality in older adults following cardiac surgery. JAMA Cardiol. 2016;1(3):314–321.
- Sundermann S, Dademasch A, Praetorius J, et al. Comprehensive assessment of frailty for elderly high-risk patients undergoing cardiac surgery. Eur J Cardiothorac Surg. 2011;39(1):33–37.
- Sundermann S, Dademasch A, Rastan A, et al. One-year follow-up of patients undergoing elective cardiac surgery assessed with the Comprehensive Assessment of Frailty test and its simplified form. Interact Cardiovasc Thorac Surg. 2011;13(2):119–123.
- Yanagawa B, Graham MM, Afilalo J, et al. Frailty as a risk predictor in cardiac surgery: beyond the eyeball test. J Thorac Cardiovasc Surg. 2018;156(1):172–176.e2.
- Sundermann SH, Dademasch A, Seifert B, et al. Frailty is a predictor of short- and mid-term mortality after elective cardiac surgery independently of age. Interact Cardiovasc Thorac Surg. 2014;18(5):580–585.
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156.
- Kamiya K, Hamazaki N, Matsue Y, et al. Gait speed has comparable prognostic capability to six-minute walk distance in older patients with cardiovascular disease. Eur J Prev Cardiolog. 2018;25(2):212–219.
- Melo TA, Duarte ACM, Bezerra TS, et al. The five times sit-to-stand test: safety and reliability with older intensive care unit patients at discharge. Rev Bras Ter Intensiva. 2019;31(1):27–33.