1. Introduction
Chronic graft-versus-host disease (GVHD), a host-reactive inflammatory process in which a donor-derived cellular response is directed against host tissues, is a major and prevalent late complication of allogeneic hematopoietic stem cell transplantation (HSCT). Chronic GVHD is a significant cause of non-relapse morbidity and mortality in post-allogeneic HSCT patients.
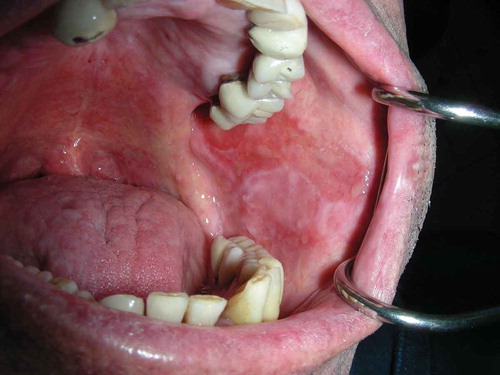
The oral cavity and salivary glands are involved in 25–80% of chronic GVHD patients [Citation1]; and the oral cavity may be the only site with manifestations of chronic GVHD [Citation2]. Moreover, oral lesions could persist after aggressive systemic therapy [Citation3]. Chronic GVHD may cause an erosive lichen planus-like oral mucosal disease (Figure 1) or present as a superficial mucocele, pyogenic granuloma, and verruciform xanthoma [Citation4]. In addition, individuals post HSCT, and especially chronic GVHD patients, have a higher risk of developing oral squamous cell carcinoma [Citation5]. Patients may also suffer from an altered sense of taste (dysgeusia), from Sjögren-like salivary gland disease that may cause hyposalivation and xerostomia, or from sclerodermatous disease that may affect the tongue and peri-oral tissues restricting function and limiting mouth opening [Citation6]. These manifestations may result in symptoms (mild discomfort to intense pain), impair oral function, nutrition, and socialization, leading to poor oral health and reduced quality of life, and may also be life-threatening [Citation7]. This concise Invited Editorial will focus on the management of oral mucosal lichenoid lesions in chronic GVHD.
2. When?
The aims of the management of oral manifestations of chronic GVHD are (a) symptom relief, (b) maintenance of oral function, nutrition, and socialization, and (c) early diagnosis and treatment of carcinoma. Fortunately, the mouth is readily accessible, enabling the topical application of medications. Topical treatment provides direct benefits to the affected oral epithelium and minimizes systemic effects (due to reduced absorption of topically applied medications). Topical treatment may be better than systemic treatment when: (a) the oral lesion does not respond to conventional systemic treatment; (b) the oral cavity is the only site affected; (c) the patient suffers from side effects related to systemic treatment (usually corticosteroids); (d) the treating hematologist wants to reduce the systemic effects of the treatment, e.g. to reduce infection risk; (e) trying to determine whether a long-lasting oral ulcer should be biopsied. The high risk of oral carcinoma in this population means that long-standing ulcers that do not respond well to a short 2-week topical corticosteroid course should be biopsied [Citation8].
3. What?
Currently, there is no specific treatment modality for the oral mucosal disease of chronic GVHD [Citation3]. Systemic therapy commonly used for chronic GVHD includes corticosteroids, calcineurin inhibitors, mTOR inhibitors (e.g. sirolimus), imatinib, and rituximab. However, topical corticosteroids are the main therapeutic agents for the oral mucosal manifestation of chronic GVHD [Citation9]. The following corticosteroids are commonly used for oral lesions: prednisolone, beclomethasone, betamethasone, triamcinolone, dexamethasone, clobetasol, budesonide, and fluocinonide. Studied protocols include: clobetasol propionate 0.05% mouth rinse (1 minute, 3 times/day); dexamethasone 0.1 mg/mL mouth rinse (4–6 minutes, 3–6 times/day or 1 minute, 3 times/day); and budesonide 0.3–0.6 mg/mL mouth rinse (15 minutes, 2–4 times/day) [Citation8,Citation10].
Non-steroidal agents such as topical cyclosporine A, tacrolimus (FK506) with or without dexamethasone, and azathioprine may be used topically as a second line in oral chronic GVHD. However, these medications have a black box warning about an increased risk of malignant transformation [Citation11].
Non-pharmacological methods for accelerating the healing of oral lesions of chronic GVHD and relieving the associated pain include: extracorporeal photopheresis; phototherapy using with ultraviolet B or psoralen-ultraviolet A (PUVA); and photobiomodulation [Citation12]. A novel treatment approach using a topical platelet-rich gel was reported to reduce pain and accelerate healing [Citation13].
4. How?
Although topical administration of corticosteroids is considered safe, it may cause local and systemic adverse effects. The systemic adverse effects may develop due to the absorption of topically applied high or ultra-high potency corticosteroids, especially through damaged mucosa, and are similar to the adverse effects of systemic treatment but with lower frequency and severity. The local adverse effects of long-term topical corticosteroids treatment include candidiasis (candidosis), atrophy of the tissue, taste alterations, xerostomia, burning sensations, and oral hairy leukoplakia (rare) [Citation8]. Due to these possible side effects even with topical medications, it is recommended that specialists with appropriate clinical training and experience manage the treatment of chronic GVHD patients, and closely monitor these patients, especially in the presence of other known risk factors.
Although topical corticosteroids are recommended for oral mucosal diseases, there are only a few commercially produced preparations for the oral mucosa. Therefore, the patient may be treated with individually prepared formulations, which may be expensive, or with commercially produced preparations designated for skin use, which may have an unpleasant taste or texture. Preparations designed for topical therapy of oral lesions include spray, mouthwash, gel, cream, and ointment.
5. Expert opinion
The management of oral mucosal lesions in the chronic GVHD patient may be a challenge. For example, given that the HSCT-related oral mucositis has resolved, the differential diagnosis of an erosive or ulcerative lesion includes the following: GVHD manifestation, herpes simplex virus (HSV) reactivation due to immunodeficiency [Citation14], local adverse effect of targeted therapy (e.g. sirolimus) or of topical therapy, or even squamous cell carcinoma; in addition, it may be an unrelated lesion, such as traumatic ulcer. Another challenge is the treatment of GHVD-related lesions. First, any potential mechanical irritation (such as the sharp edge of dental restoration or appliance) should be ruled out. Later, the clinician may consider topical therapy.
Various corticosteroid preparations may vary in their anti-inflammatory potency and formulation, and selection is based on lesion size and severity, cost, patient preference, and availability [Citation15]. In case of a few small or moderate discrete lesions, the application of gel or ointment over the lesions may be preferred, whereas for large lesions, or lesions in multiple locations or involving posterior areas, a rinse or spray may be more effective.
It should be noted that, in order to achieve a clinical effect, the preparation needs to be in contact with the mucosa for several minutes. In the oral cavity, hydrophilic gels or solutions remain in contact with the mucosa longer than creams or ointments. The patient should be instructed to gently dry the mucosa with gauze just before the application of non-liquid preparations, to apply the medication, and then spit 4 to 15 minutes later. The patient should also be told to avoid rinsing, drinking, or eating for about 30 minutes. Longer contact time may be achieved by applying gauze soaked with the medication or by using a custom-made dental appliance, e.g. when there is significant gingival involvement.
Alcohol-free solutions are preferred over alcohol-based (elixir) solutions which may cause a burning sensation in the atrophic or ulcerated mucosa. In addition, we educate the patients that the solution is a medication (not a simple mouthwash), and should be used as directed.
Usually, ulcerative lesions that do not respond are subjected to biopsy and pathological examination because of the high risk of oral squamous cell carcinoma in this population. In non-suspicious, non-responding symptomatic ulcers, we consider topical tacrolimus (0.1%), photobiomodulation, intralesional steroid injection (e.g. triamcinolone acetonide, 1–5 mg per cm2 of the lesion), or systemic therapy as recommended for systemic chronic GVHD (Figure 2).
Figure 2. Clinical decision-making in managing of erosive lichen planus-like oral mucosal disease in chronic graft-versus-host disease (GVHD); in case of an unresponsive or suspected lesion, a biopsy and pathologic examination should be considered.
Considering that topical steroid therapy may increase fungal infections, chronic GVHD patients with other risk factors for oral candidiasis, such as hyposalivation or anemia, are given prophylactic topical antifungals (e.g. nystatin solution). In these patients, the application of steroid gels or ointments directly on the lesions is preferred to a mouthwash which may affect the entire oral cavity. As mentioned above, in addition to candidiasis, topical therapy in the oral cavity may cause atrophy of the tissue, taste alterations, xerostomia, burning sensations, and oral hairy leukoplakia; because these are also common oral manifestations/complications of chronic GVHD itself, the clinician should be able to differentiate between GVHD and the adverse effect of medications.
Control of oral pain is a critical component of overall management and restoration of quality of life and oral function. Topical anesthetics (e.g. viscous lidocaine) may be effective in relieving oral pain in general, particularly before eating or oral hygiene procedures [Citation3]. Systemic analgesics, including opioids, and topical and/or systemic cannabis may be used to reduce pain in persistent cases.
Oral mucosal lesions of chronic GVHD can challenge the clinician. Currently, there is no perfect treatment for these complex patients, but by combing the available options which include systemic and topical corticosteroids, other non-steroid medications, and novel non-pharmacologic methods, the clinician can tailor the treatment to meet the requirements of each patient.
Declaration of interest
Y Zadik was a coinvestigator for the study NCT00887263 sponsored by Dr. Falk Pharma GmbH. He has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Treister N , Duncan C , Cutler C , et al. How we treat oral chronic graft-versus-host disease. Blood. 2012;120:3407–3418.
- Elad S , Zadik Y , Caton JG , et al. Oral mucosal changes associated with primary diseases in other body systems. Periodontol 2000. 2019;80:28–48.
- Fall-Dickson JM , Pavletic SZ , Mays JW , et al. Oral complications of chronic graft-versus-host disease. J Natl Cancer Inst Monogr. 2019;2019:lgz007.
- Kuten-Shorrer M , Woo SB , Treister NS. Oral graft-versus-host disease. Dent Clin North Am. 2014;58:351–368.
- Elad S , Zadik Y , Zeevi I , et al. Oral cancer in patients after hematopoietic stem-cell transplantation: long-term follow-up suggests an increased risk for recurrence. Transplant. 2010;90:1243–1244.
- Zadik Y. Restricted mouth opening in chronic graft-versus-host disease. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:201–202.
- Elad S , Zadik Y , Yarom N . Oral Complications of Nonsurgical Cancer Therapies. Atlas Oral Maxillofac Surg Clin North Am. 2017;25:133–147.
- Zadik Y , Elad S , Shapira A , et al. Treatment of oral mucosal manifestations of chronic graft-versus-host disease: dexamethasone vs budesonide. Expert Opin Pharmacother. 2017;18:235–242.
- Elad S , Jensen SB , Raber-Durlacher JE , et al. Clinical approach in the management of oral chronic graft-versus-host disease (chronic GVHD) in a series of specialized medical centers. Support Care Cancer. 2015;23:1615–1622.
- Park AR , La HO , Cho BS , et al. Comparison of budesonide and dexamethasone for local treatment of oral chronic graft-versus-host disease. Am J Health Syst Pharm. 2013;70:1383–1391.
- Treister N , Li S , Kim H , et al. An open-label phase II randomized trial of topical dexamethasone and tacrolimus solutions for the treatment of oral chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2016;22:2084–2091.
- Epstein JB , Raber-Durlacher JE , Lill M , et al. Photobiomodulation therapy in the management of chronic oral graft-versus-host disease. Support Care Cancer. 2017;25:357–364.
- Bojanic I , Mravak Stipetic M , Pulanic D , et al. Autologous blood as a source of platelet gel for the effective and safe treatment of oral chronic graft-versus-host disease. Transfusion. 2018;58:1494–1499.
- Elad S , Zadik Y , Hewson I , et al. A systematic review of viral infections associated with oral involvement in cancer patients: a spotlight on Herpesviridea. Support Care Cancer. 2010;18:993–1006.
- Elad S , Aljitawi O , Zadik Y . Oral graft-versus-host disease: a pictorial review and a guide for dental practitioners. Int Dent J. in press.