ABSTRACT
Introduction
Acute myeloid leukemia (AML) is the most common type of acute leukemia in adults, but the results for patients with AML are still unsatisfactory. The discovery of new mutations in AML, including IDH mutations, has opened the door for treatment with targeted agents. Ivosidenib is a selective, potent inhibitor of the IDH1 mutant protein.
Areas covered
This review summarizes the mechanism of action, safety profile and efficacy of ivosidenib for patients with IDH1-mutated AML. The authors then provide their expert perspectives on the use of the drug including their future perspectives.
Expert opinion
Ivosidenib is a promising, most probably practice changing, new drug for the treatment of IDH1-mutated AML. Current phase III trials are ongoing to evaluate the addition of ivosidenib to the current standards-of-care. In the near future, more drug combinations are awaited. Challenges for the future include the development of resistance and establishing the duration of maintenance therapy.
1. Introduction
Acute myeloid leukemia (AML) is the most common type of acute leukemia in adults [Citation1,Citation2]. It is a clonal disorder of hematopoietic stem cells and characterized by the inability of immature myeloid cells (blasts) to differentiate. The proliferation of blasts leads to accumulation, with impairment of normal hematopoiesis, resulting in severe infections, anaemia, and haemorrhage. Although AML can occur in any age group, it is predominantly a disease in older adults, with a median age at diagnosis of 68 years [Citation3]. During recent years, considerable progress has been made in deciphering the molecular, genetic, and epigenetic basis of AML and in defining new diagnostic and prognostic markers. A growing number of recurring genetic changes have been recognized in the new World Health Organization (WHO) classification of AML [Citation4–7]. Recurrent mutations in isocitrate dehydrogenases 1 and 2 (IDH1 and IDH2) are among the most common mutations in AML (taken together approximately 20% of patients) [Citation8,Citation9]. IDH mutations increase in frequency with increasing age. IDH1 mutations are less common than IDH2 mutations in AML, with a frequency of around 7–14% and 8–19% respectively. IDH1 and IDH2 mutations only rarely co-occur in the same patient [Citation2,Citation10].
Nowadays, approximately 40–45% of young and 15–20% of elderly AML patients can be cured Citation11–16]. These results for patients with AML are still unsatisfactory and urge for new treatment modalities. The discovery of targetable mutations in AML, including IDH mutations, has paved the way to develop targeted agents. Ivosidenib is a selective, potent inhibitor of the IDH1 mutant protein that is currently approved in the United States (US) for the treatment of adult patients with AML with an IDH1 mutation who are relapsed or refractory (R/R) to prior therapy and for patients who are ≥75 years old or who have comorbidities that preclude the use of intensive induction chemotherapy. The aim of this manuscript is to critically evaluate ivosidenib for the treatment of AML.
2. Overview of the market
Current strategies for AML can be generally divided into intensive and non-intensive treatments. Intensive chemotherapy, usually restricted to fit individuals, typically consists of cytarabine combined with an anthracycline-based drug, is aimed to achieve a complete remission (CR). Post-remission treatment to prevent relapse, can consist of either allogeneic stem cell transplantation (allo-SCT), high dose chemotherapy followed by autologous stem cell transplantation (auto-SCT), or one or more cycles of additional chemotherapy. Choice for the type of post-remission treatment is based on risk factors for relapse as determined at diagnosis, and may be impacted by the measurable residual disease (MRD) status after induction therapy, measured by multiparameter flow cytometry (MFC) or by real-time quantitative polymerase chain reaction (qPCR) (or new emerging technologies, including digital PCR and next-generation sequencing (NGS)) for molecular MRD targets in AML, core-binding factor (CBF) translocations, and mutations in NPM1 [Citation7,Citation17,Citation18]. Patients unable to receive intensive treatments may be treated with low-intensity therapies consisting of monotherapy with hypomethylating agents (HMAs) and recently in the US approved, in combination with venetoclax, blood product transfusions, and supportive care including prophylaxis for infections. Fitness of the patient is commonly assessed by the treating physician based on chronological age, functional age, biological age and co-morbidities. Several scoring systems could be of help in classifying fitness, like a comprehensive geriatric assessment (CGA), Charlson Comorbidity Index (CCI), the 3 MS test, Short Physical Performance Battery (SPPB), hematopoietic stem cell transplantation-comorbidity index (HCT-CI) and WHO-performance score (WHO-PS) [Citation19]. However, there is not one objective and comprehensive method generally accepted in current practice or study designs which clearly differentiates patients in fit or frail. The FDA relies on a score system defined by Ferrara [Citation20].
Even though the survival of patients with AML has improved over the past 5 decades, related to advances in supportive care, better use of existing drugs, advances in transplantation, and a better understanding of the disease biology enabling a more accurate prognostication, the survival of patients with AML is still unsatisfactory. AML is fatal in approximately half of younger patients and in about 80% of older patients, therefore treatments to prevent relapse and to improve long term survival outcomes are urgently needed Citation11–16,Citation21]. Better understanding of the underlying molecular abnormalities driving leukemogenesis have led to the development of various targeted therapies for AML. Since 2017 several new agents have expanded the treatment arsenal for patients with AML, these include targeted as well as non-targeted therapies. The US Food and Drug Administration (FDA) has approved glasdegib, venetoclax, ivosidenib, midostaurin, enasidenib, gilteritinib, CPX-351, and gemtuzumab ozogamicin (GO), the European Medicines Agency (EMA) has done likewise for midostaurin, CPX-351, and GO [Citation22–26].
Since mutations in IDH1 and IDH2 are among the most common mutations in AML, these seem an attractive target for therapy. The incidence of mutations in IDH1 varies between studies but is estimated to lie between 14%, which increases to 16% if only cases with normal cytogenetics are analyzed [Citation5,Citation6]. While reports are inconsistent, most studies looking into the prognostic significance of recurrent mutations in AML report an adverse prognosis if the sole abnormality that can be detected in normal cytogenetic AML is a mutation in IDH1. Nevertheless, prognosis appears to be highly correlated by the presence of other mutations [Citation27–29].
Various compounds targeting mutant IDH enzymes have been developed. Inhibitors that specifically target mutant IDH1 other than ivosidenib are IDH305 and Olutasidenib (FT2102). Vorasidenib (AG881), and BAY1436032, are targeting both IDH1 and IDH2 mutations; these new inhibitors are currently being tested in phase I/II trials [Citation30–34]. Other non-target therapies that seem effective in IDH1-mutated AML are venetoclax + azacitidine, CB-839, which is an oral glutaminase inhibitor and PARP-inhibitors [Citation35,Citation36]. Here, we focus on ivosidenib for the treatment of patients with AML.
3. Introduction to the compound
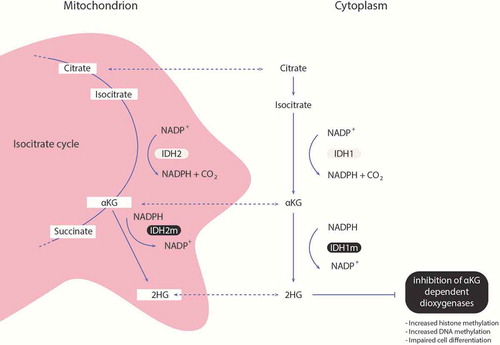
Mutations of the IDH1 enzyme have been identified in several tumors, including AML [Citation37,Citation38]. The IDH enzymes play an important role in the isocitrate cycle, where they convert isocitrate to α-ketoglutarate (α-KG). IDH1 enzymes are localized in the cytoplasm and peroxisomes and IDH2 in the mitochondria. Mutations occur in recurrent, specific locations of the gene, for IDH1 mainly in the Arg132 residue (R132), which results in the replacement of arginine into a cysteine, histidine, glycine or serine [Citation5,Citation9]. The resulting mutant IDH proteins convert α-KG to the oncometabolite 2-hydroxygluterate (2-HG), causing its accumulation. This results in hypermethylation of DNA and histones leading to a block in differentiation thereby promoting leukemogenesis, see [Citation38–42] Various compounds targeting mutant IDH enzymes have been developed. Ivosidenib is a first in class targeted mutant IDH1 inhibitor (see Box 1).
3.1. Chemistry
Ivosidenib is a highly specific, allosteric, reversible inhibitor of mutated IDH1, also known as AG-120 and formerly known as AGI-16,678 (Tibsovo, Agios Pharmaceuticals). The chemical name is (2S)-N-[(1S)-1-(2-Chlorophenyl)-2-[(3,3-difluorocyclobutyl)amino]-2-oxoethyl]-1-(4-cyanopyridin-2-yl)-N-(5-fluoropyridin-3-yl)-5-oxopyrrolidine-2-carboxamide [Citation43,Citation44]. Its mechanism of action is inhibition of the mutant IDH1 enzyme, which decreases 2-HG levels leading to the reversal of IDH mutation induced histone and DNA hypermethylation, and to differentiation of leukemic blasts [Citation45,Citation46].
3.2. Pharmacodynamics
The pharmacodynamic effects observed included inhibition of 2-HG in the blood and bone marrow. After multiple doses of ivosidenib at 500 mg daily, the mean plasma 2-HG levels decreased to levels seen in healthy persons. Approximately 71% of patients achieved a ≥ 90% reduction in plasma 2-HG with ivosidenib 500 mg daily at cycle 2 day 1, and 2-HG inhibition was durably maintained at this dose, with no additional 2-HG inhibition at doses above 500 mg daily. Plasma 2-HG levels suppression did not seem to correlate with patient response, indicating that 2-HG reduction alone is not sufficient for a response [Citation43,Citation44].
3.3. Pharmacokinetics and metabolism
Ivosidenib was rapidly absorbed, the median time to peak ivosidenib plasma concentration was 3 hours, with a mean half-life of 72 to 138 hours after a single dose, supporting a daily dose regimen. A steady state was achieved within 14 days of administration. A single-dose food effect study in healthy subjects indicated that a high-fat meal increased the mean peak plasma concentration by 98% [Citation47]. Therefore, it is advised that ivosidenib should not be administered with a high fat meal. CYP3A4 is the main route of metabolism, although 77% was excreted unchanged in the feces and 17% in the urine (10% unchanged). A population pharmacokinetic model of ivosidenib has been recently performed, suggesting that no dose adjustments were needed according to the patient and disease conditions, but the pharmacokinetics of ivosidenib in patients with severe renal insufficiency and with severe hepatic impairment (Child-Pugh C) is unknown. The concomitant use of azoles (moderate/strong CYP3A4 inhibitors) results in reduction of ivosidenib clearance [Citation43,Citation44,Citation48].
4. Clinical efficacy
An overview of the discussed trials is summarized in .
Table 1. Clinical trials evaluating ivosidenib in AML
4.1. Phase I/II studies
A phase I dose-escalation and dose-expansion study of ivosidenib monotherapy was performed in patients with R/R IDH1-mutated AML (NCT02074839) [Citation44]. 268 patients were enrolled, 258 received study medication (78 in dose escalation, 180 in expansion). At the data-cutoff (12 May 2017), 179 patients with R/R AML had started ivosidenib at a dose of 500 mg daily, including 33% of patients with a secondary leukemia (sAML) that failed prior therapy and about 24% of patients had relapsed after allo-SCT. Median age was 67 years (range 18–87 years). Patients were assigned to receive 500 mg ivosidenib oral daily until disease progression, poor tolerance, or allo-SCT (12% of patients). The primary end-point, the rate of CR or CR with partial hematologic recovery (CRh) was 30.4%, with a median time to CR or CRh of 2.7 months and a median duration of response of 6.5 months. 21.6% of patients reached a CR with a median time to CR of 2.8 months with a median duration of response of 9.3 months. About 41.6% of had an overall response with a median time to first response of 1.9 months and a median duration of response of 6.5 months. 35% of patients became transfusion-independent for a period of 56 days or more during treatment and 56% of patients who were at baseline independent of transfusions remained transfusion independent. Plasma 2-HG levels were suppressed in almost all patients, regardless of response. Further co-occurring mutation analysis revealed that no specific preexisting genotype was significantly predictive of clinical response or resistance to ivosidenib treatment throughout the study. However, a recent comprehensive genomic analysis of samples from a cohort of patients from this study showed that RTK pathway mutations (baseline mutations in the individual RTK pathway genes of NRAS and PTPN11, and in the RTK pathway genes as a group (defined in this analysis as NRAS, KRAS, PTPN11, KIT, and FLT3)), are associated with primary resistance to ivosidenib [Citation49]. Clearance of mutant IDH1 was seen in 21% of patients. This subset of patients showed a longer duration of remission (11.1 vs 6.5 months) and longer overall survival (14.5 vs 10.2 months) than those without IDH1 mutation clearance. These data support the ability of ivosidenib to induce deep molecular remissions. This study led to the FDA approval of ivosidenib.
In a phase Ib study (NCT02677922), 23 treatment-naïve patients with an IDH1-mutated AML were treated with ivosidenib 500 mg once daily in combination with subcutaneous azacitidine 75 mg/m2 for 7 days (in a 28-day schedule) [Citation50]. Patients had a median age of 76 years (range 61–88), over half of the patients (52%) were ≥75 years. De novo and sAML was present in 65% and 35% of patients, respectively. As of 19 February 2019, 10 patients (43.5%) remained on study treatment. Patients have been treated for a median of 15 cycles (range 1–30). The overall response rate (ORR) was 78%, including 61% who achieved a CR. Median time to response was 1.8 months and to CR 3.7 months, median response duration has not been reached. IDH1 mutation clearance in bone marrow mononuclear cells was observed in 69% of patients with CR or CRh, including 71% with CR [Citation50,Citation51].
In an open-label, multicenter, phase I study (NCT02632708), patients eligible for intensive chemotherapy with newly diagnosed IDH1-mutated AML were treated with induction therapy (daunorubicin 60 mg/m2/day or idarubicin 12 mg/m2/day for 3 days with cytarabine 200 mg/m2/day for 7 days) in combination with ivosidenib 500 mg once daily [Citation52]. After induction, patients could receive ≤4 cycles of consolidation therapy while continuing ivosidenib. Patients who completed or were ineligible for consolidation could continue on maintenance ivosidenib until the end of study. For patients who proceed to allo-SCT, ivosidenib treatment was discontinued prior to allo-SCT and was not resumed post-transplant. As of 1 May 2018, 47 patients had been treated with ivosidenib (median age 63 years, range 24–76) including 34% patient with sAML. Among the 41 patients evaluable for efficacy, a response of CR, CR with incomplete hematological recovery (CRi) or CR with incomplete platelet recovery (CRp) was achieved in 93% of patients with de novo AML and 46% of patients with sAML. Seventeen patients proceeded to allo-SCT. In patients who achieved a CR, IDH1 mutational clearance was observed in 41%. Flow cytometry minimal residual disease (MRD)-negative CRs were observed in 89% of those with an IDH1 mutation.
Several other phase I/II studies are currently ongoing. An open-label phase II clinical study for biomarker-based treatment of unfit for chemo AML patients, aims to assess the feasibility and efficacy of a combination based approach to the treatment of IDH1-mutant AML by combining ivosidenib with azacitidine (NCT03013998). Those patients who have achieved a response, defined as a CR or CRi, by the end of cycle 6, will continue on combination therapy for a total of 12 cycles and then patients will go onto receive monotherapy with ivosidenib until disease progression or unacceptable side effects that mandate discontinuation of therapy. Patients who cannot complete 12 cycles of azacitidine may proceed onto monotherapy with ivosidenib. Combinations of HMA and IDH inhibitors are interesting, because this combination enhanced cell differentiation, as measured by increases in hemoglobinization and expression of differentiation markers, and potentiated cell death, compared with either agent alone [Citation53,Citation54].
In another phase Ib/II trial ivosidenib and venetoclax with or without azacitidine is investigated in patients with IDH1-mutated R/R AML or treatment-naive patients who are not eligible for standard induction chemotherapy (NCT03471260). Venetoclax is an oral selective inhibitor of the anti-apoptotic B-cell lymphoma-2 (BCL-2) and is active in vitro against IDH mutated cells [Citation36]. This finding was reproduced in clinical trials of venetoclax monotherapy in R/R or untreated AML and combined with HMA or low-dose cytarabine in R/R myeloid malignancies, showing a CR/CRi of 33% and a 27% response rate in IDH-mutated patients, respectively [Citation26,Citation55,Citation56]. In elderly untreated AML patients who are unfit for intensive therapies, combinations of HMA and venetoclax obtained in an IDH mutated subgroup a CR/CRi rate of 71% and a median OS of 24.4 months [Citation26].
Furthermore, a phase II study (NCT04044209) is active; here ivosidenib is combined with nivolumab (an immune checkpoint inhibitor), for patients with IDH1-mutated R/R AML. Ivosidenib is also being tested as maintenance therapy after allo-SCT in IDH1-mutated malignancies in a phase I dose-escalation trial (NCT03564821).
4.2. Phase III studies
Currently, there a two phase III studies recruiting previously untreated IDH1-mutated AML patients. In one study patients who are candidates for non-intensive treatment can be included, the other study is for newly diagnosed patients eligible for intensive chemotherapy. AGILE is a global, randomized, double-blind, placebo-controlled trial in patients with previously untreated IDH1-mutated AML who are candidates for non-intensive treatment (NCT03173248). 392 patients are being randomized 1:1 to receive either ivosidenib 500 mg daily or placebo in combination with azacitidine. Randomization is stratified by region and by de novo versus sAML [Citation51]. In the global, randomized, double-blind, placebo-controlled HOVON/AML-SG AML study (NCT03839771), depending on the mutation ivosidenib/enasidenib or placebo is added to intensive chemotherapy in induction and consolidation, followed by maintenance therapy for up to 2 years in newly diagnosed patients with an IDH-mutated AML, who are eligible for intensive chemotherapy. 484 AML patients with an IDH1 or IDH2 mutation will be randomized in a 1:1 ratio.
5. Safety and tolerability
In the phase I study (NCT02074839) of ivosidenib monotherapy adverse events (AEs) occurred in 99% patients treated with ivosidenib, however, treatment was well tolerated since the majority of these AEs were grades 1–2 and deemed unrelated to treatment. They included diarrhea (31%), leukocytosis (30%), febrile neutropenia (29%), nausea (28%), fatigue (26%), dyspnea (25%), prolonged QT interval (25%), peripheral edema (22%), anemia (22%), fever (21%) and cough (21%). There were no adverse events related deaths, although the treatment-related grade ≥3 adverse events occurred in 21% of patients, and the most common were prolonged QT interval, IDH differentiation syndrome (IDH-DS) and leukocytosis. IDH-DS occurred in about 11% of patients with a median onset time of 29 days, including grade ≥3 IDH-DS in 5.4%. No cases of IDH-DS led to permanent treatment discontinuation of study drug or death [Citation44]. In the phase 1b/2 study (NCT02677922) with ivosidenib combined with azacitidine, the spectrum of adverse events was consistent with monotherapy experiences with ivosidenib or azacitidine. Investigators reported 4 cases of IDH differentiation syndrome. Of those, three were deemed to be serious adverse events, but all four cases resolved [Citation50]. Ivosidenib combined with induction and consolidation was well tolerated, based on the frequency of grade ≥3 non-hematologic adverse events and hematologic recovery [Citation52]. In the studies combining ivosidenib with intensive treatment the frequency of IDH-DS was much lower.
5.1. IDH-differentiation syndrome
The IDH-DS is a potentially fatal complication of treatment with ivosidenibIDH mutated timely identification and proper management is essential. The incidence of IDH-DS in patients with R/R AML treated with ivosidenib and enasidenib on pivotal trials leading to FDA approval ranged from 14%,; FDA review of marketing applications for ivosidenib identified 72/179 (40%) potential cases for ivosidenib, 34/179 (19%) were adjudicated as IDH-DS [Citation57].
The etiology of IDH-DS is incompletely understood, but IDH-DS has been linked to a large burden of maturing myeloid cells and their production of inflammatory cytokines. This differentiating process, as seen with other differentiating agents (e.g. treatment of acute promyelocytic leukemia with all-trans retinoic acid and/or arsenic trioxid), may alter the balance in expression of adhesion molecules and chemo-attractants (cytokines) that mediate tissue infiltration by maturing blood cells. The inflammatory state that results can lead to the clinical manifestation of a ‘differentiation syndrome’.
The most important prognostic risk factors for development of IDH-DS are baseline peripheral blood blast ≥25% and bone marrow blasts ≥48%. Furthermore, exploratory genomic analysis indicated that mutations in TET2 may increase the relative risk of IDH-DS. Median time to onset of IDH-DS was 20 days (range: 1–78), most (88%) cases occurred >7 days following initiation of ivosidenib.
Clinical features may include some or all of the following: respiratory compromise, interstitial pulmonary infiltrates, pleural and/or pericardial effusion, hypoxia, unexplained fever, rash, weight gain, and clinical deterioration. The most common clinical criteria were dyspnea and pulmonary infiltrates or pleuropericardial effusion; hypotension was the least common criterion. Laboratory features may include an increase in absolute neutrophil count (ANC) and/or platelets. An increase in mature leukocytes in the bone marrow may be observed. However, no single sign or symptom may be considered per se as diagnostic of the syndrome, and other causes should be sought and excluded.
Conditions consistent with signs and symptoms of IDH-DS but refractory to treatment for the initially suspected cause(s), or that worsen within the first 48 hours after treatment initiation, should be managed as potential IDH-DS. It is recommended that the measures indicated below are undertaken at the earliest manifestations of IDH-DS with pulmonary or renal manifestations. Patients with IDH-DS and pulmonary and/or renal manifestations should be hospitalized for continued close observation; in case of uncertainty with the diagnosis, e.g. presence of less specific symptoms, patients should be closely monitored, as condition may rapidly deteriorate. Management guidelines for suspected IDH-DS include prompt administration of dexamethasone 10 mg IV every 12 hours until disappearance of signs and symptoms for at least 3 days, hydroxyurea 1–3 grams orally twice or three times daily for patients with an elevated white blood cell (WBC) count (>30x10e9/L). Furosemide and/or leukapheresis are recommended if indicated clinically. Ivosidenib can be withheld at investigators’ discretion and resumed once signs/symptoms of IDH-DS resolved [Citation57,Citation58].
6. Regulatory affairs
On 20 July 2018, the FDA approved ivosidenib for adult patients with R/R AML with a susceptible IDH1 mutation as detected by an FDA-approved test. Approval was based on the AG120-C-001 study [Citation44,Citation59]. The FDA concluded that ivosidenib provided meaningful, short-term, clinical benefit to a subset of patients with R/R IDH1-mutated AML. Long-term safety follow-up data will be provided as per postmarketing requirement. On 2 May 2019, the FDA approved ivosidenib for newly-diagnosed AML with a susceptible IDH1 mutation, as detected by an FDA-approved test, in patients who are at least 75 years old or who have comorbidities that preclude the use of intensive induction chemotherapy [Citation60]. On 12 December 2016, orphan designation was granted by the European Commission for ivosidenib for the treatment of AML. Drug approval of ivosidenib by EMA is under evaluation.
7. Expert opinion
Until recently the general therapeutic strategy in patients with AML has not changed substantially in the last 30 years, For decades, the backbone of chemotherapy consisted of the combination of an anthracycline and cytosine-arabinoside, addition of a third agent has not resulted in an improvement of outcome. However the outcome improvement observed, especially in the younger patients, can mainly be attributed to better supportive care and the increased availability of stem cell transplantation. The unraveling of the molecular and genetic landscape of AML creating the possibility to identify potential therapeutic targets has led to a change in the treatment. Emerging developments are now present in the FLT3 and IDH mutated AMLs. IDH1 mutations occur in about 7–14% of patients with AML [Citation5,Citation6]. Ivosidenib is the first IDHm inhibitor that was approved by FDA [Citation60]. Although this approval was based on a phase I dose-escalation and dose-expansion trial in a selected patient population, the results are impressive for a group of patients with an extremely poor prognosis [Citation44]. Importantly, transfusion-independence was also achieved in a substantial part of these patients, which is of great clinical benefit, especially in older AML patients. Additional phase I studies combining ivosidenib plus azacitidine as well as added to intensive chemotherapy, showed very promising results [Citation50,Citation52]. Importantly two randomized phase III studies, one for patients eligible for intensive treatment, the HOVON/AML-SG AML study (NCT03839771) in which ivosidenib is added to intensive chemotherapy, consolidation and maintenance, and one for patients ineligible for non-intensive treatment in which ivosidenib is combined with azacitidine, the AGILE study (NCT03173248) are currently ongoing. Results from these randomized, double-blind, placebo-controlled trials have to be awaited before ivosidenib can be incorporated in the first-line treatment as standard of care for patients with IDH1-mutated AML, but it is anticipated that the addition of ivosidenib can lead to improvement of long term survival. Both IDH inhibitors are also extremely important for the treatment of relapsed/refractory IDHm AML, a condition associated with a very dismal outcome. As discussed above remarkable results are achieved in this AML population including high and durable CR rates. The availability of these inhibitors urges for comprehensive genetic screening not just at diagnosis, but also at relapse [Citation7,Citation61]. Maintenance treatment is also incorporated in several studies (e.g. NTC03013998, NCT03564821, NCT03839771). The optimal duration of maintenance treatment and how effective it will be is not yet known. The ongoing trials are not designed to answer this question, which is highly important concerning associated toxicity and economic considerations. Data on IDH1 mutation clearance and measurable residual disease (MRD) might be of help to resolve this question. Various studies have demonstrated a strong correlation between MRD status and the cumulative risk for relapse in AML patients. The long-term clinical impact of IDH mutation clearance is under investigation, but preliminary data suggest that clearance of the mutation results in a prolonged duration of response and improved overall survival.
Challenges remain in deciding which drug(s) to use when several therapeutic options are available. It has to be recognized that the recently approved drug combination of venetoclax with azacitidine is also highly active in IDHm AML. Since the availability of several new agents for patients with AML, it might be interesting to combine different drugs, especially when there are co-occurring druggable mutations. IDH1 mutations in AML frequently co-occur with FLT3-ITD (in 15–27%) and NPM1 mutations, therefore ivosidenib and a FLT3-inhibitor could be added to the current standard-of-care therapy to improve outcome. Several studies are currently initiated in IDH1 mutated patients. Examples are combinations of ivosidenib with venetoclax (NCT03471260) or nivolumab (NCT04044209). The expanded number of available agents makes it possible to explore other combinations, while also triple combinations are investigated. However, establishing the right drug combinations and schedules with acceptable toxicity profiles might be challenging.
Resistance to IDH inhibitors has already been described, resulting in progressive disease with increases in plasma 2-HG concentration and re-occurrence of leukemic blasts. This underlines the need to identify strategies to prevent the occurrence of resistance. Preliminary data indicate that ivosidenib combined with venetoclax might prevent the development of resistance [Citation36,Citation62,Citation63].
With new therapies, there is a need for increased awareness of how to anticipate, mitigate and manage common complications associated with these new agents. With ivosidenib, adverse events of special interest are the IDH-DS, leucocytosis and prolongation of the QT interval, which can be managed with appropriate guidance, as shown in trials performed thus far.
In conclusion, ivosidenib is a promising new drug for the treatment of IDH1-mutated AML in this exciting era of targeted approaches for AML.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
One reviewer declares serving as an advisor for Agios Pharmaceuticals. Peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Box 1. Drug summary box
Table
Article highlights
AML is the most common type of leukemia in adults; the results for patients with AML are still unsatisfactory and urge for new treatment modalities.
Recurrent mutations in IDH1 are among the most common mutations in AML, with a frequency of around 7–14%.
Ivosidenib is a first in class targeted mutant IDH1 inhibitor.
Phase I studies with ivosidenib monotherapy and ivosidenib in combination with azacitidine or intensive chemotherapy showed very promising results with an acceptable safety profile.
Two randomized phase III studies, one for patients eligible for intensive treatment, and one for patients ineligible for non-intensive treatment in which ivosidenib is combined with azacitidine, are currently ongoing; it is anticipated that the addition of ivosidenib can lead to improvement of long-term survival, especially in patients with clearance of the mutation.
Adverse events of special interest are the IDH-DS, leucocytosis and prolongation of the QT interval.
The expanded number of available agents in the treatment of AML makes it possible to explore other drug combinations with ivosidenib.
Challenges remain in choosing the right drug combinations with acceptable toxicity profiles, optimal duration of maintenance therapy, and overcoming the development of resistance.
This box summarizes the key points contained in the article.
Additional information
Funding
References
- Burnett A, Wetzler M, Lowenberg B. Therapeutic advances in acute myeloid leukemia. J Clin Oncol. 2011 Feb 10;29(5):487–494. PubMed PMID: 21220605; eng.
- Dohner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015 Sep 17;373(12):1136–1152. PubMed PMID: 26376137; eng.
- Cancer stat facts: leukemia - acute myeloid leukemia (AML).
- Grimwade D, Ivey A, Huntly BJ. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood. 2016 Jan 7;127(1):29–41. PubMed PMID: 26660431; PubMed Central PMCID: PMCPMC4705608. eng.
- Ley TJ, Miller C, Ding L, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013 May 30;368(22):2059–2074. PubMed PMID: 23634996; PubMed Central PMCID: PMCPMC3767041. eng.
- Papaemmanuil E, Gerstung M, Bullinger L, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016 Jun 9;374(23):2209–2221. PubMed PMID: 27276561; PubMed Central PMCID: PMCPMC4979995. eng.
- Dohner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017 Jan 26;129(4):424–447. PubMed PMID: 27895058; eng.
- Medeiros BC, Fathi AT, DiNardo CD, et al. Isocitrate dehydrogenase mutations in myeloid malignancies. Leukemia. 2017 Feb;31(2):272–281. PubMed PMID: 27721426.
- Mardis ER, Ding L, Dooling DJ, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med. 2009 Sep 10;361(11):1058–1066. PubMed PMID: 19657110; PubMed Central PMCID: PMCPMC3201812. eng.
- Fathi AT, Wander SA, Faramand R, et al. Biochemical, epigenetic, and metabolic approaches to target IDH mutations in acute myeloid leukemia. Semin Hematol. 2015 Jul;52(3):165–171. PubMed PMID: 26111463; eng.
- Tallman MS, Gilliland DG, Rowe JM. Drug therapy for acute myeloid leukemia. Blood. 2005 Aug 15;106(4):1154–1163. PubMed PMID: 15870183; eng.
- Petersdorf SH, Kopecky KJ, Slovak M, et al. A phase 3 study of gemtuzumab ozogamicin during induction and postconsolidation therapy in younger patients with acute myeloid leukemia. Blood. 2013 Jun 13;121(24):4854–4860. PubMed PMID: 23591789; PubMed Central PMCID: PMCPMC3682338. eng.
- Burnett AK, Hills RK, Milligan D, et al. Identification of patients with acute myeloblastic leukemia who benefit from the addition of gemtuzumab ozogamicin: results of the MRC AML15 trial. J Clin Oncol. 2011 Feb 1;29(4):369–377. PubMed PMID: 21172891; eng.
- Buchner T, Berdel WE, Haferlach C, et al. Age-related risk profile and chemotherapy dose response in acute myeloid leukemia: a study by the German acute myeloid leukemia cooperative group. J Clin Oncol. 2009 Jan 1;27(1):61–69. PubMed PMID: 19047294; eng.
- Fernandez HF, Sun Z, Yao X, et al. Anthracycline dose intensification in acute myeloid leukemia. N Engl J Med. 2009 Sep 24;361(13):1249–1259. PubMed PMID: 19776406; PubMed Central PMCID: PMCPMC4480917. eng.
- Moore JO, George SL, Dodge RK, et al. Sequential multiagent chemotherapy is not superior to high-dose cytarabine alone as postremission intensification therapy for acute myeloid leukemia in adults under 60 years of age: cancer and Leukemia Group B Study 9222. Blood. 2005 May 1;105(9):3420–3427. PubMed PMID: 15572587; PubMed Central PMCID: PMCPMC1895015. eng.
- Estey EH. Acute myeloid leukemia: 2019 update on risk-stratification and management. Am J Hematol. 2018 Oct;93(10):1267–1291. PubMed PMID: 30328165; eng.
- Schuurhuis GJ, Heuser M, Freeman S, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD working party. Blood. 2018 Mar 22;131(12):1275–1291. PubMed PMID: 29330221.
- Rao AV. Fitness in the elderly: how to make decisions regarding acute myeloid leukemia induction. Hematology Am Soc Hematol Educ Program. 2016 Dec 2;2016(1):339–347. PubMed PMID: 27913500.
- Ferrara F, Barosi G, Venditti A, et al. Consensus-based definition of unfitness to intensive and non-intensive chemotherapy in acute myeloid leukemia: a project of SIE, SIES and GITMO group on a new tool for therapy decision making. Leukemia. 2013 Apr;27(5):997–999. PubMed PMID: 23653072; eng.
- Thein MS, Ershler WB, Jemal A, et al. Outcome of older patients with acute myeloid leukemia: an analysis of SEER data over 3 decades. Cancer. 2013 Aug 1;119(15):2720–2727. PubMed PMID: 23633441; PubMed Central PMCID: PMCPMC3821042. eng.
- Raj RV, Abedin SM, Atallah E. Incorporating newer agents in the treatment of acute myeloid leukemia. Leuk Res. 2018 Nov;74:113–120. PubMed PMID: 30401522; eng.
- Bohl SR, Bullinger L, Rucker FG. New targeted agents in acute myeloid leukemia: new hope on the rise. Int J Mol Sci. 2019 Apr 23;20(8). PubMed PMID: 31018543; PubMed Central PMCID: PMCPMC6515298. eng. DOI: 10.3390/ijms20081983.
- Cerrano M, Itzykson R. New treatment options for acute myeloid leukemia in 2019. Curr Oncol Rep. 2019 Feb 4;21(2):16. PubMed PMID: 30715623; eng.
- Kucukyurt S, Eskazan AE. New drugs approved for acute myeloid leukaemia in 2018. Br J Clin Pharmacol. 2019 Aug 30. PubMed PMID: 31469910; eng. DOI:10.1111/bcp.14105
- DiNardo CD, Pratz K, Pullarkat V, et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019 Jan 3;133(1):7–17. PubMed PMID: 30361262; PubMed Central PMCID: PMCPMC6318429. eng.
- Xu Q, Li Y, Lv N, et al. Correlation between isocitrate dehydrogenase gene aberrations and prognosis of patients with acute myeloid leukemia: a systematic review and meta-analysis. Clin Cancer Res off J Am Assoc Cancer Res. 2017 Aug 1;23(15):4511–4522. PubMed PMID: 28246275; eng.
- Feng JH, Guo XP, Chen YY, et al. Prognostic significance of IDH1 mutations in acute myeloid leukemia: a meta-analysis. Am J Blood Res. 2012;2(4):254–264. PubMed PMID: 23226625; PubMed Central PMCID: PMCPMC3512179. eng.
- Zhou KG, Jiang LJ, Shang Z, et al. Potential application of IDH1 and IDH2 mutations as prognostic indicators in non-promyelocytic acute myeloid leukemia: a meta-analysis. Leuk Lymphoma. 2012 Dec;53(12):2423–2429. PubMed PMID: 22616558; eng.
- DiNardo CD, Schimmer AD, Yee KWL, et al. A phase I study of IDH305 in patients with advanced malignancies including relapsed/refractory AML and MDS that harbor IDH1R132 mutations. Blood. 2016;128(22):1073.
- Watts JM, Baer MR, Lee S, et al. A phase 1 dose escalation study of the IDH1m inhibitor, FT-2102, in patients with acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS). J clin oncol. 2018;36(15_suppl):7009.
- Cho YS, Levell JR, Liu G, et al. Discovery and evaluation of clinical candidate IDH305, a brain penetrant mutant IDH1 inhibitor. ACS Med Chem Lett. 2017 Oct 12;8(10):1116–1121. PubMed PMID: 29057061; PubMed Central PMCID: PMCPMC5641959. eng.
- Chaturvedi A, Herbst L, Pusch S, et al. Pan-mutant-IDH1 inhibitor BAY1436032 is highly effective against human IDH1 mutant acute myeloid leukemia in vivo. Leukemia. 2017 Oct;31(10):2020–2028. PubMed PMID: 28232670; PubMed Central PMCID: PMCPMC5629366. eng.
- Mellinghoff IK, Penas-Prado M, Peters KB, et al. Phase 1 study of AG-881, an inhibitor of mutant IDH1/IDH2, in patients with advanced IDH-mutant solid tumors, including glioma. J clin oncol. 2018;36(15_suppl):2002.
- Stone RM. Which new agents will be incorporated into frontline therapy in acute myeloid leukemia? Best Pract Res Clin Haematol. 2017 Dec;30(4):312–316. PubMed PMID: 29156201; eng.
- Chan SM, Thomas D, Corces-Zimmerman MR, et al. Isocitrate dehydrogenase 1 and 2 mutations induce BCL-2 dependence in acute myeloid leukemia. Nat Med. 2015 Feb;21(2):178–184. PubMed PMID: 25599133; PubMed Central PMCID: PMCPMC4406275. eng.
- Yen KE, Bittinger MA, Su SM, et al. Cancer-associated IDH mutations: biomarker and therapeutic opportunities. Oncogene. 2010 Dec 9;29(49):6409–6417. PubMed PMID: 20972461; eng.
- Dang L, White DW, Gross S, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009 Dec 10;462(7274):739–744. PubMed PMID: 19935646; PubMed Central PMCID: PMCPMC2818760. eng.
- Figueroa ME, Abdel-Wahab O, Lu C, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010 Dec 14;18(6):553–567. PubMed PMID: 21130701; PubMed Central PMCID: PMCPMC4105845. eng.
- Chowdhury R, Yeoh KK, Tian YM, et al. The oncometabolite 2-hydroxyglutarate inhibits histone lysine demethylases. EMBO Rep. 2011 May;12(5):463–469. PubMed PMID: 21460794; PubMed Central PMCID: PMCPMC3090014. eng.
- Lu C, Ward PS, Kapoor GS, et al. IDH mutation impairs histone demethylation and results in a block to cell differentiation. Nature. 2012 Feb 15;483(7390):474–478. PubMed PMID: 22343901; PubMed Central PMCID: PMCPMC3478770. eng.
- Ward PS, Patel J, Wise DR, et al. The common feature of leukemia-associated IDH1 and IDH2 mutations is a neomorphic enzyme activity converting alpha-ketoglutarate to 2-hydroxyglutarate. Cancer Cell. 2010 Mar 16;17(3):225–234. PubMed PMID: 20171147; PubMed Central PMCID: PMCPMC2849316. eng.
- Badar T, Kantarjian HM, Nogueras-Gonzalez GM, et al. Improvement in clinical outcome of FLT3 ITD mutated acute myeloid leukemia patients over the last one and a half decade. Am J Hematol. 2015 Nov;90(11):1065–1070. PubMed PMID: 26299958; PubMed Central PMCID: PMCPMC4618182. eng.
- DiNardo CD, Stein EM, de Botton S, et al. Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J Med. 2018 Jun 21;378(25):2386–2398. PubMed PMID: 29860938; eng.
- Kernytsky A, Wang F, Hansen E, et al. IDH2 mutation-induced histone and DNA hypermethylation is progressively reversed by small-molecule inhibition. Blood. 2015 Jan 8;125(2):296–303. PubMed PMID: 25398940; PubMed Central PMCID: PMCPMC4295919. eng.
- Wang F, Travins J, DeLaBarre B, et al. Targeted inhibition of mutant IDH2 in leukemia cells induces cellular differentiation. Science (New York, NY). 2013 May 3;340(6132):622–626. PubMed PMID: 23558173; eng.
- Dai D, Yang H, Nabhan S, et al. Effect of itraconazole, food, and ethnic origin on the pharmacokinetics of ivosidenib in healthy subjects. Eur J Clin Pharmacol. 2019 Aug;75(8):1099–1108. PubMed PMID: 31011758; eng.
- Le K, Wada R, Dai D, et al. Population pharmacokinetics of ivosidenib (AG-120) in patients with IDH1-mutant advanced hematologic malignancies. Blood. 2018;132(Supplement 1):1394.
- Choe S, Wang H, DiNardo CD, et al. Molecular mechanisms mediating relapse following ivosidenib monotherapy in IDH1-mutant relapsed or refractory AML. Blood Adv. 2020;4(9):1894–1905.
- DiNardo CD, Stein AS, Fathi AT, et al. Mutant isocitrate dehydrogenase (mIDH) inhibitors, enasidenib or ivosidenib, in combination with azacitidine (AZA): preliminary results of a phase 1b/2 study in patients with newly diagnosed acute myeloid leukemia (AML). Blood. 2017;130(Supplement 1):639.
- Stein E, Dinardo CD, Jang JH, et al. AGILE: A phase 3, multicenter, randomized, placebo-controlled study of ivosidenib in combination with azacitidine in adult patients with previously untreated acute myeloid leukemia with an IDH1 mutation. J clin oncol. 2018;36(15_suppl):TPS7074–TPS7074.
- Stein EM, DiNardo CD, Fathi AT, et al. Ivosidenib or enasidenib combined with induction and consolidation chemotherapy in patients with newly diagnosed AML with an IDH1 or IDH2 mutation is safe, effective, and leads to MRD-negative complete remissions. Blood. 2018;132(Supplement 1):560.
- Yen K, Chopra VS, Tobin E, et al. Abstract 4956: functional characterization of the ivosidenib (AG-120) and azacitidine combination in a mutant IDH1 AML cell model. Cancer Res. 2018;78(13 Supplement):4956.
- Chopra VS, Avanzino B, Mavrommatis K, et al. Abstract 2280: functional characterization of combining epigenetic modifiers azacitidine and AG-221 in the TF-1: IDH2R140QAML model. Cancer Res. 2016;76(14 Supplement):2280.
- Konopleva M, Pollyea DA, Potluri J, et al. Efficacy and biological correlates of response in a phase II study of venetoclax monotherapy in patients with acute myelogenous leukemia. Cancer Discov. 2016 Oct;6(10):1106–1117. PubMed PMID: 27520294; PubMed Central PMCID: PMCPMC5436271. eng.
- DiNardo CD, Rausch CR, Benton C, et al. Clinical experience with the BCL2-inhibitor venetoclax in combination therapy for relapsed and refractory acute myeloid leukemia and related myeloid malignancies. Am J Hematol. 2018 Mar;93(3):401–407. PubMed PMID: 29218851; eng.
- Norsworthy KJ, Mulkey F, Scott EC, et al. Differentiation syndrome with ivosidenib and enasidenib treatment in patients with relapsed or refractory IDH-mutated AML: a U.S. Food and Drug Administration systematic analysis. Clin Cancer Res off J Am Assoc Cancer Res. 2020 May 11. PubMed PMID: 32393603; eng.
- Fathi AT, DiNardo CD, Kline I, et al. Differentiation syndrome associated with enasidenib, a selective inhibitor of mutant isocitrate dehydrogenase 2: analysis of a phase 1/2 study. JAMA Oncol. 2018;4(8):1106–1110.
- Roboz GJ, DiNardo CD, Stein EM, et al. Ivosidenib induces deep durable remissions in patients with newly diagnosed IDH1-mutant acute myeloid leukemia. Blood. 2019 Dec 16 PubMed PMID: 31841594; eng. DOI:10.1182/blood.2019002140.
- Norsworthy KJ, Luo L, Hsu V, et al. FDA approval summary: ivosidenib for relapsed or refractory acute myeloid leukemia with an isocitrate dehydrogenase-1 mutation. Clin Cancer Res off J Am Assoc Cancer Res. 2019 Jun 1;25(11):3205–3209. PubMed PMID: 30692099; eng.
- Tallman MS, Wang ES, Altman JK, et al. Acute myeloid leukemia, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(6):721. English.
- Harding JJ, Lowery MA, Shih AH, et al. Isoform switching as a mechanism of acquired resistance to mutant isocitrate dehydrogenase inhibition. Cancer Discov. 2018 Dec;8(12):1540–1547. PubMed PMID: 30355724; PubMed Central PMCID: PMCPMC6699636. eng.
- Intlekofer AM, Shih AH, Wang B, et al. Acquired resistance to IDH inhibition through trans or cis dimer-interface mutations. Nature. 2018 Jul;559(7712):125–129. PubMed PMID: 29950729; PubMed Central PMCID: PMCPMC6121718. eng.