1. Introduction
At COP26 in 2021, 50 countries committed to developing low-carbon, climate-resilient health systems [Citation1]. The legislation encompassing the health system has been the driver of change in some countries. For example, Colombia’s 2016 National Climate Change Policy mandated greenhouse gas emission mitigation from all sectors. The health sector’s response included creating environmental management groups and adapting health-care processes to minimize waste production [Citation2].
Achieving net zero emissions and otherwise reducing environmental degradation and consequent harms to human health and health equity requires assessment, measurement, and management of environmental impacts. This editorial examines the role of health technology assessment (HTA) and explores how HTA agencies could incorporate environmental impacts into their frameworks and processes and the potential impacts of doing so.
2. HTA could incorporate environmental sustainability information
HTA is a multidisciplinary process that aims to assess the value of health technologies from the perspective of the health-care system, individual patients, and (in some cases) wider society [Citation3]. HTA guides decisions about how to allocate limited health system resources. The term ‘health technologies’ describes much more than technical equipment; it includes ‘medicines, medical devices, assistive technologies, techniques, and procedures developed to solve health problems and improve the quality of life’ [Citation4]. HTA helps to assess the overall value of technologies across a range of domains in promotion of an equitable, efficient, and high-quality health system [Citation3]. A primary purpose of HTA is to inform decision-making about which health technologies are recommended in which circumstances (appropriate use) and/or which are funded (including reimbursement and disinvestment).
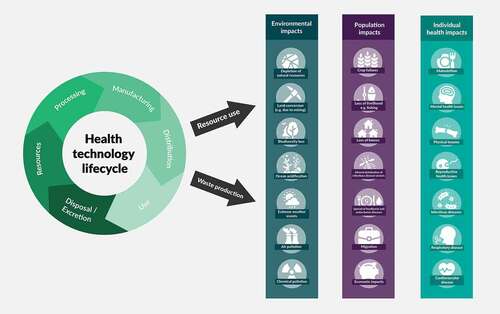
Global surveys of health professionals and the public show high levels of concern regarding climate change and support for health-sector action to mitigate it [Citation5,Citation6]. Health technologies have environmental impacts across the lifecycle (). For example, the production, use, and disposal of medications and devices have a significant carbon footprint (approximately 30% of the English NHS carbon footprint [Citation7]), and water pollution due to disposal of pharmaceuticals is disrupting marine and riverine ecosystems. By incorporating information about environmental impacts into their assessments, HTA agencies could enable the evolution of HTA in line with societal values and priorities [Citation8]. HTA agencies already routinely guide difficult decisions involving complex trade-offs between health outcomes, financial costs, stakeholder perspectives, and ethical considerations. The most clinically effective option is not always recommended because sometimes HTA determines that it offers limited overall value to the health system, taking into account factors apart from clinical effectiveness [Citation3].
Figure 1. Environmental impacts and human health impacts of health technologies across their lifecycle.
The Canadian Agency for Drugs and Technologies in Health (CADTH)’s 2022–2025 strategy includes methodological adaptation to incorporate environmental sustainability [Citation9], and the National Institute for Health and Care Excellence (NICE)’s 2021–2026 strategy includes the intention to include environmental impact data in its guidance [Citation10]. Several other organizations internationally are exploring whether and how to include environmental considerations in HTA, and many conferences and meetings have included discussions on this topic including HTA international’s Annual Meeting, June 2023, and ISPOR North America’s HTA Roundtable, May 2023. INAHTA (The International Network of Agencies for Health Technology Assessment) have a learning group on environmental sustainability.
To incorporate environmental impacts into HTA in a socially acceptable, justifiable manner, transparent processes, data of appropriate detail and quality, and standardized appraisal methods are required. Deliberative committees that make recommendations based on HTA must also adapt to include environmental considerations in their deliberations. At some HTA agencies, expert committees carrying out HTA already consider factors beyond clinical and cost-effectiveness, for example patients’ perspectives, and ethical considerations, as part of a deliberative process. The committee may consider qualitative data, which can influence its recommendations without altering quantitative cost-effectiveness estimates. Thus, quantitative data are not necessarily required, and qualitative environmental information could influence recommendations and decision-making.
Multiple players inform health system decision-making, including manufacturers, regulators, clinicians, professional societies, procurement specialists, and patients. Local and federal governments may also have an influence, e.g. through environment ministries. How much responsibility lies with the health sector? We argue that all stakeholders have a responsibility to contribute to reducing health systems’ environmental impacts, and HTA agencies have a particular responsibility, corresponding to their unique skills and position. Environmental agencies specialize in collecting data and measuring and reducing environmental impacts but lack the remit and expertise to conduct analyses weighing environmental impacts alongside health and other factors. If and how environmental data are incorporated within HTA and decision-making would vary globally, depending on the nature, role, and governance of each HTA agency in the health landscape.
2.1. Incorporating environmental considerations into HTA could be highly impactful
Incorporating environmental considerations into HTA could be highly impactfu, and influence decisions across a broad range of health technologies. The outcomes of HTA directly influence whether, and in which circumstances, health technologies are available to patients. Delivering sustainable healthcare requires streamlining care and avoiding unnecessary care to avoid waste, which HTA can support as it provides information to guide appropriate and effective use of health technologies. For example, a CADTH HTA of remote monitoring for cardiac conditions detailed factors, such as alignment with patients’ lifestyles, that are required to ensure effectiveness of remote monitoring; hence, it could reduce ineffective (wasteful) use and mitigate late detection of disease progression to reduce demand for healthcare [Citation11] and the subsequent environmental impacts.
Over half of health-sector greenhouse gas emissions are associated with procured technologies and equipment [Citation12]. In England, 10% of health system emissions relate to medical equipment and 20% to medicines and devices [Citation7], many of which may be assessed through HTA. Some countries do not have an HTA agency, and HTA agency processes vary between agencies [Citation13]. Not all technologies are eligible for and selected for HTA; for example, most HTA agencies’ remits exclude generic drugs, and HTA agencies’ limited resources are insufficient to assess the sheer volume of different types of health-care devices and equipment. Nonetheless, new health technologies are assessed in comparison to the current standard of care or other existing alternatives [Citation3]; thus, new and established technologies accounting for a sizable proportion of the health sector’s greenhouse gas emissions may have their environmental impacts presented and assessed.
Including environmental considerations in HTA could facilitate the comparison of health technologies with relatively similar health outcomes but different environmental impacts to guide funding and use recommendations. For example, single-use versus multiple-use instruments may have comparable health benefits when used for procedures but very different impacts in terms of waste production and greenhouse gas emissions [Citation12].
Positive impacts of HTA agencies considering environmental factors may extend beyond decisions directly informed by HTA. If HTA agencies establish frameworks and consider environmental sustainability, this could stimulate improved data collection and presentation practices from manufacturers. HTA agencies can also support measurement and management of environmental impacts of health systems by developing new, or selecting existing, standardized approaches to analyzing and presenting environmental data relevant to health-sector decision-making.Footnote1 Measurement approaches are more developed for some domains of environmental impact (), such as air pollutants and air pollution levels, than for others, such as land conversion and biodiversity. For example, nitrous oxide, a gas used as an anesthetic agent has a global warming potential of 265, meaning that 1 ton of nitrous oxide emissions causes the same amount of warming as 265 tons of carbon dioxide; meanwhile, there is no universally applied measurement approach for biodiversity loss.
Even where sector-wide approaches encourage or mandate companies to reduce the environmental impacts of their products across the lifecycle, HTA may have added impacts. Extending HTA to consider costs and benefits across a health technology’s lifecycle may increase attention to supply chains, spotlighting raw material sources and production processes, enhancing transparency around manufacturing, and promoting improved labor and environmental standards. Furthermore, by comparing the environmental costs and impacts of new products and interventions to those of standard care, HTA can incentivize manufacturers to develop products with lower environmental impacts. This could favor innovation that supports environmental sustainability, which might include developing technologies that have a primary function of reducing greenhouse gas emissions or are part of a circular economy where post-consumer ‘waste’ is recirculated as a resource.
2.2. There are risks associated with incorporating environmental considerations into HTA
Risks of incorporating environmental considerations into HTA relate to acceptability, resources for implementation, and impacts. Some members of the public, patients, or decision-makers may oppose diverting limited health system resources to environmental sustainability, particularly in the context of unmet health needs. The Colombian HTA agency, IETS, explored the acceptability of considering environmental impacts by approaching the Ministry of Health for their views. The Ministry affirmed their commitment to support mitigation of environmental harms, including by incorporating environmental impact assessment into HTA. IETS is now investigating which environmental impacts to assess and which stakeholders to involve in method’s development. In England, NICE ran a deliberative public engagement dialog to inform its approach to addressing environmental sustainability. The results showed strong support for NICE, taking responsibility to make healthcare more environmentally sustainable with participants accepting that trade-offs sometimes need to be made, but expressing a strong preference for prioritizing ‘win-win’ actions where health, environmental, and financial outcomes are aligned [Citation14].
A risk for implementation is that companies are unable or unwilling to dedicate sufficient resources to collecting and presenting data, and HTA agencies and other health system decision-makers do not or cannot develop and enforce standards, limiting the quality of data provided. Significant investments in human resources and developing technical skills and knowledge will be required from HTA agencies to incorporate environmental data, and there will be long timelines to see implementation of and impact from change to HTA methods globally. A further risk is that these investments could be deemed disproportionate if HTA processes were to find that the difference between the environmental impacts of the technologies compared is marginal and the impact on decisions is minimal.
To manage HTA resource requirements and minimize the risk that HTA agencies direct resources to analyses that will have minimal impact, we propose using ‘triage.’ If a technology is not expected to have substantially different environmental impacts than the current standard of care (based on relative environmental impacts and frequency of use), it may not require any environmental assessment or may only require limited assessment (e.g. focused on one part of the lifecycle or one domain of environmental impact ()). For example, for inhalers, the most significant source of greenhouse gases is the propellant gas in metered dose inhalers (MDIs); therefore, a decision might be made to only assess greenhouse gas impacts during the use of MDIs for treatment (from the propellant) and not greenhouse gas emissions related to manufacturing or distribution, for example.
HTA is primarily intended to inform system-level and not patient-level decision-making. Nonetheless, a risk of HTA agencies considering environmental impacts is that consequent recommendations to change practice have actual or perceived negative impacts on patient care. For example, dry powdered inhalers (DPIs) have a significantly lower carbon footprint than MDIs [Citation15]. Incorporating environmental considerations into HTA may lead to a recommendation to use a DPI unless there is an important reason to use an MDI. Some patients may be asked to consider switching to a DPI from MDI, and may not wish to, especially if their disease is well controlled. To mitigate the patient concerns or disease exacerbations due to treatment switches, treatments should only be changed where there is agreement from both patient and clinician.
2.3. Achieving a positive impact through incorporation of environmental considerations into HTA requires a proportionate approach and collaboration within and between sectors
Developing methods to add environmental information into already complex assessments of value will be challenging for HTA agencies [Citation8]. A major challenge is building capacity for and resources to access, validate, analyze, and collate data on environmental impact. Resource requirements will depend on the approach taken. For example, HTA agencies may choose to present environmental data separately from health outcomes and financial (cost-effectiveness) analyses or may choose to integrate environmental information with health and financial data in a single integrated health economic analysis [Citation6,Citation16]. Producing a single integrated analysis will require more resources and specialized expertise to identify how environmental impacts are weighed against other valued outcomes and design health economic methods.
CADTH’s Health Technology Expert Review Panel includes environmental impacts as one of the 10 domains in their deliberative framework. With the assumption that evidence needs will vary for different health technologies and decisions being made, a full analysis is not required for all 10 domains. Instead, CADTH takes a tailored approach in consideration of overall scarce HTA resources, and for each HTA determines an optimal set of evidence required. Quantifiable data are not required to inform deliberations. For some HTAs, a quantitative environmental impact assessment may be conducted, and for others, information on environmental impacts may come from experts who are part of or inform the deliberative committee. In all cases, the committee uses information on environmental impacts alongside evidence, information, and perspectives across other domains (e.g. clinical effectiveness, safety, cost-effectiveness, patients’ perspectives, and ethical considerations) to develop HTA recommendations [Citation17]. HTA agencies will need to direct resources to refine HTA processes to incorporate environmental aspects and to upskill expert committee members who are not accustomed to deliberating on environmental impacts.
While Marsh et al. argue that technologies must be assessed across the whole lifecycle, including environmental impacts of changes to care pathways as a result of their use [Citation8], we believe that triage is important to ensure that HTA resources are directed in a practical and proportionate manner. Appropriate assessment will strike a balance between exactitude and feasibility. If environmental impacts are analyzed for every HTA, this may not be as impactful as employing those resources elsewhere, e.g. for innovation toward more sustainable care models.
Delivering high-quality sustainable healthcare requires attention to disease prevention, rational use of interventions, and more. HTA agencies will ideally be proactive in requesting, analyzing, and presenting both positive and negative data on environmental impacts of health technologies to support health-care decision-makers across health systems. Changes to HTA practice must happen in concert with complementary and/or synergistic changes to wider health-care system policies addressing the roles of all relevant stakeholders in system change. This includes support from politicians to provide continued commitment to achieving net-zero and other environmentally sustaining policies, timely and sustained action from health-care managers in developing relevant policy changes to local settings, and buy-in from clinicians to implement the changes in practice. Furthermore, industry actors must be committed to conducting and publishing environmental impact analyses of their products in accordance with defined standards and to allowing those analyses to be scrutinized. HTA agencies must be responsive to priorities and opportunities for improvement in healthcare and ensure these are fed back to the system through relevant, timely, and realistic guidance that allows sufficient implementation.
3. Conclusions
Continued evolution of HTA to meet contemporary health system priorities and social values is both achievable and necessary. Health professionals and the public want health systems to support environmental sustainability; nonetheless, directing health system resources to incorporating environmental considerations into HTA may raise concerns about other health system priorities being compromised.
Measurement underpins effective action; hence, HTA agencies should continue to bring environmental impact assessment into its decision-making. To incorporate environmental information into HTA, agencies will require resources and specialist expertise. One way to limit the resources required is employing a triage process to direct analyses to health technologies, stages of the health technology’s lifecycle, and environmental domains that are expected to have the greatest impact.
Adapting HTA to incorporate environmental considerations could support transition to sustainable health systems. The results of HTA influence significant decisions about the use and funding of health technologies. Furthermore, HTA agencies incorporating environmental considerations into their processes could foster improvements in collection and presentation of environmental data by manufacturers and innovation in environmentally sustainable health technologies. HTA agencies must act now to identify and meet their environmental responsibilities.
4. Expert opinion
Research has explored the acceptability of incorporating environmental considerations into HTA, the type of environmental data that could be incorporated (e.g. qualitative and/or quantitative, in various environmental domains), methodological approaches to incorporate these data (including whether environmental considerations are included as costs or outcomes), and potential impacts of incorporating such data [Citation6,Citation8,Citation16,Citation17].
Key findings are that adapting HTA to incorporate environmental considerations is technically feasible and could be highly impactful, but implementation will require an agreement on approach and commitment to support HTA adaptation, including commitment of resources. Weaknesses of the research relate to its early stage; further method’s development, led by HTA agencies with involvement of multidisciplinary stakeholders, is required to design and test approaches.
The ultimate aim is to reach agreement on socially acceptable, justifiable, and feasible approaches to incorporate environmental impacts into HTA and see implementation of these approaches inform health-sector decision-making and reduce negative environmental impacts of healthcare. This can support the evolution of HTA in line with societal values and priorities. HTA informs decision making and resource allocation; hence, HTA agencies incorporating environmental considerations into their processes could have tangible impacts. It could foster improvements in collection and presentation of environmental data and innovation in environmentally sustainable health technologies; it could support transition to sustainable health systems.
To achieve this goal, further development of methods for quantifying or qualifying environmental impacts, in ways that permit comparability and assessment for bias, is required. Further exploration of public views on directing health system resources to incorporating environmental considerations into HTA is needed.
The biggest challenges to incorporating environmental information into HTA will include accessing data of sufficient quality and and reaching agreement on methods including which environmental impacts to include, how to assess those impacts, and the weight to be applied to these relative to other costs and outcomes. Technical challenges remain because many environmental impacts are not quantified or not well quantified across all aspects of the lifecycle of health technologies [Citation6]. Multidisciplinary collaboration, including inputs from environmental science, engineering, economics, and health policy, is required.
Further work is required to facilitate the consensus on the value accorded to environmental considerations and identify feasible approaches to implementation. Research may contribute to the development of a triage process to direct analyses to health technologies, stages of a health technology’s lifecycle, and environmental domains that are expected to have the greatest impact [Citation17].
Public engagement exercises have found that both health professionals and the wider public want health systems to support environmental sustainability, and also wish to see that other health system priorities are not compromised [Citation14]. A further challenge, therefore, will be achieving agreement to include information about environmental impacts where there is a trade-off, in particular for health or financial benefits or costs.
Environmental metrics are increasingly incorporated into reporting and decision-making in the health sector and in other sectors; therefore, we anticipate that HTA agencies will continue to develop test cases as they move toward considering environmental impacts following a triage process in all HTAs.
Declaration of interest
We have the following interests to declare: K Cresswell and K Shah are employed at NICE F Greaves was employed at NICE previously and S Walpole was a Clinical Fellow at NICE previously. S Walpole is an Associate of the Centre for Sustainable Healthcare and a Trustee of the Healthcare Infection Society. In previous employments, K Shah ’s employers have received funding from a variety of sources, including pharmaceutical companies and the Association of the British Pharmaceutical Industry. L Weeks is the Director of Health Technology Assessment at CADTH. L Mesa-Melgarejo is a chief of a technical unit of Institute of Health Technology Assessment (IETS) in Colombia. A Robajo is Executive Director of the Institute of Health Technology Assessment. The views expressed in this article are those of the authors and not necessarily those of CADTH, IETS or NICE. COI forms are available from the corresponding author. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
S Walpole and K Shah conceived of the article. All authors contributed to development and revisions of the final draft. S Walpole is the guarantor of the article. All authors read and approved the final version of the manuscript for publication.
Acknowledgments
The authors would like to thank Rachel Brandon for contributions to development of the figure and Nick Crabb and Juliet Kenny for comments on earlier drafts of this paper. Felix Greaves is supported by the NIHR North West London Collaboration for Applied Health Research.
Additional information
Funding
Notes
1. There is currently no internationally or nationally agreed framework for measuring environmental impacts across health sectors. Policymakers and researchers have applied various carbon footprinting methodologies to calculate greenhouse gas emissions from healthcare.
References
- World Health Organization; Countries commit to develop climate-smart health care at COP26 UN climate conference [Internet]. News release. 2021 [cited 2021 Dec 23]. Available from: https://www.who.int/news/item/09-11-2021-countries-commit-to-develop-climate-smart-health-care-at-cop26-un-climate-conference
- HCWH. Alianza entre el Ministerio de Salud y Protección Social de Colombia y Salud sin Daño para impulsar la descarbonización del sistema de salud colombiano [Internet]. [cited 2022 Mar 22]. Available from: https://saludsindanio.org/colombia-ssd
- O’Rourke B, Oortwijn W, Schuller T, et al. The new definition of health technology assessment: a milestone in international collaboration. Int J Technol Assess Health Care. 2020;36(3):187–190. doi: 10.1017/S0266462320000215
- WHO. Medical devices [Internet]. Heal Prod Policy Stand.2011 [[cited 2022 Oct 19]. Available from]. https://www.who.int/teams/health-product-policy-and-standards/assistive-and-medical-technology/medical-devices.
- Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Heal. 2021;5(5):e316–e323. InternetAvailable from: https://linkinghub.elsevier.com/retrieve/pii/S254251962100053X
- Hensher M. Incorporating environmental impacts into the economic evaluation of health care systems: perspectives from ecological economics [Internet]. Resour Conserv Recycl. 2020;104623. Available from https://www.sciencedirect.com/science/article/pii/S0921344919305294
- NHS England and NHS Improvement. Delivering a ‘net zero’ National Health Service [Internet]. (UK): National Health Service; 2020. Available from https://www.england.nhs.uk/greenernhs/publication/delivering-a-net-zero-national-health-service/
- Marsh K, Ganz ML, Hsu J, et al. Expanding health technology assessments to include effects on the environment. Value Heal. 2016 Mar 30;19:249–254. InternetAvailable from. doi: 10.1016/j.jval.2015.11.008
- CADTH. Ahead of the curve: shaping future-ready health systems 2022-2025 strategy [Internet]. Ottawa; 2022. Available from: https://strategicplan.cadth.ca/wp-content/uploads/2022/03/cadth_2022_2025_strategic_plan.pdf
- NICE. NICE strategy 2021 - 2026: dynamic, collaborative, excellent [Internet]. London; 2021. Available from: https://static.nice.org.uk/NICE strategy 2021 to 2026 - Dynamic, Collaborative, Excellent.pdf.
- CADTH. Remote Monitoring Programs for Cardiac Conditions [Internet]. 2022 [cited 2022 Oct 24]. Available from: https://www.inahta.org/upload/2022/CADTH Remote Monitoring INAHTA Brief_final.pdf.
- MacNeill AJ, Hopf H, Khanuja A, et al. Transforming the medical device industry: road map to a circular economy. Health Aff. 2020;39(12):2088–2097. InternetAvailable from: http://www.healthaffairs.org/doi/10.1377/hlthaff.2020.01118
- Oortwijn W, Broos P, Vondeling H, et al. Mapping of health technology assessment in selected countries. Int J Technol Assess Health Care. 2013;29(4):424–434. InternetAvailable from: https://www.cambridge.org/core/product/identifier/S0266462313000469/type/journal_article
- NICE. NICE listens: public dialogue on environmental sustainability [Internet]. London; 2023. Available from: https://www.nice.org.uk/about/what-we-do/our-research-work/nice-listens.
- Wilkinson AJK, Braggins R, Steinbach I, et al. Costs of switching to low global warming potential inhalers. An economic and carbon footprint analysis of NHS prescription data in England. BMJ Open. 2019;9(10):e028763. InternetAvailable from: http://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2018-028763
- Toolan M, Walpole S, Shah K, et al. Environmental impact assessment in health technology assessment: principles, approaches, and challenges. Int J Technol Assess Health Care. 2023;39(1):e13. InternetAvailable from: https://www.cambridge.org/core/product/identifier/S0266462323000041/type/journal_article
- Greenwood Dufour B, Weeks L, De Angelis G, et al. How we might further Integrate considerations of environmental impact when assessing the value of health technologies. Int J Environ Res Public Health. 2022;19(19):12017. InternetAvailable from: https://www.mdpi.com/1660-4601/19/19/12017
