1. New SARS-CoV-2 mutants
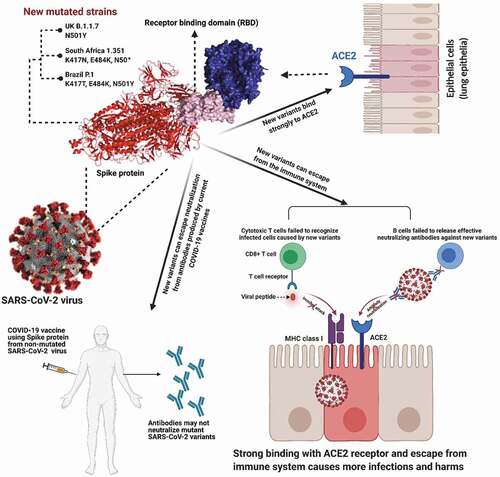
A novel strain of coronavirus, SARS-CoV-2, the causative agent of coronavirus disease (COVID-19) was first associated with severe acute respiratory disease in late 2019 and has triggered an ongoing pandemic since March 2020 [Citation1–3]. The pandemic has already had a serious impact on the global economy and has resulted thus far, to over 2.7 million deaths and over 122 million infections [Citation4]. The rampage of the COVID-19 pandemic is ongoing. Meanwhile, in a world effort a number of anti-SARS-CoV-2 vaccines were developed in record time by late 2020 for emergency use. The approval of vaccines in less than a year is unprecedented in human history and a triumph in medical research [Citation5]. The variants D614G was the first spike protein mutation of concern that spread worldwide within few months [Citation6]. By the end of June 2020, variants D614G were found in almost all the SARS-Cov-2 samples worldwide [Citation6]. However, the detection of mutant strains of SARS-CoV-2 in Brazil (P.1), South Africa (1.351), and the United Kingdom (UK) (B.1.1.7) have triggered huge concern around the world () [Citation7]. Based on available information, the highest rate of transmissibility and infection rates reported for the mutant strains of SARS-CoV-2 is the UK B.1.1.7 which has already spread to over 50 countries [Citation8,Citation9]. In comparison, the South African strain has spread to 20 countries [Citation10], and the Brazilian mutant strain has spread to Japan, Germany, and some other countries [Citation10]. The detection of the new mutant strains in many countries prompted border closures, lockdowns, and new restrictions and ultimately massive economic loss and further deaths. The UK B.1.1.7 strain is linked to higher number (>60%) of infections in the UK since its detection and is considered to be at least 50–70% more contagious than the original Wuhan strain. A recent study conducted by Imperial College London (Preprint), reported that the reproduction number (R) of B.1.1.7 is 1.45 compared to 0.92 for the original non-mutated SARS-CoV-2 virus [Citation11]. To control a pandemic the R-value should be below 1. Very recently, there are reports for the emergence of further new variants, primarily, the New York variant (B.1.526) and the California variant (B.1.427/B.1.429) which are spreading rapidly. By mid-February 2021, B.1.526 cases had risen to 27% of viral sequences in the database. By January 2021, the California variant accounted to 53% of cases sampled.
Table 1. A snapshot on the emerging new mutant strains of SARS-CoV-2 virus
Genetic mutations of viruses is a common phenomenon, and currently, 4000 mutations in the spike protein of SARS-CoV-2 have already been identified and most of them do not have any effect on the virus in regard to its ability to spread or cause disease [Citation7]. However, the Brazilian P.1, UK B.1.1.7, and South African 1.351 mutations are dangerous as they possess features such as, escape from the immune system, bind strongly with ACE2 receptor and may cause more harm [Citation10,Citation14]. More specifically the UK B.1.1.7 strain has received considerable attention due to its high transmissibility rate and has been identified by a unique number and combination of mutations. Currently 17 unique mutations with the UK variant have been identified [Citation15]. It is unclear whether mutations or combination of mutations are responsible for increased transmissibility of the UK B1.1.7 strain. In addition, it is speculated that the South African 1.351 mutant strain, has mutations located on the spike protein which helps strong binding to angiotensin-converting enzyme 2 (ACE2) and eventually contributes to higher transmission [Citation7]. Furthermore, mutations are known to help the virus to escape the immune system or replicate more efficiently once in the host. The Brazilin (P.1) strain also contains an escape mutant known as E484K where the negatively charged (E, glutamic acid) is substituted with a positively charged amino acid (K, lysine), resulting in a new and stronger binding site of ACE and also aids the virus to escape the immune system, making it more infectious ().
2. Can anti-SARS-CoV-2 vaccines currently in roll-out in many countries, protect against the new SARS-CoV-2 mutants?
The emergence of these new mutant strains could have a great impact on the efficacy of the anti-SARS-CoV-2 vaccines [Citation7]. Most of the vaccines have been designed to target the spike protein to stop its binding with ACE2 receptor. Due to the mutation in the spike protein of the coronavirus, the antibodies produced by the vaccines may not be able to recognize the mutant and hence will fail to neutralize the coronavirus [Citation16]. The spike region of the SARS-CoV-2 virus has several immunogenic regions. When a person gets infected with the SARS-CoV-2 virus their antibody responses are to specific immunogenic regions in the majority of the population. The vaccines developed thus far, were developed and approved before the emergence of the new highly contagious strains and assumed that current vaccines may not be effective against the new strains [Citation11]. This notion was further supported in a study where the South African 1.351 variant which has mutations in the immunogenic region of the spike protein and exposed to monoclonal antibodies raised against non-mutant SARS-CoV-2; South African 1.351 strain completely escaped the binding of the monoclonal antibodies [Citation17]. In another study [Citation4], blood samples of 20 volunteers who were either vaccinated with Moderna (mRNA1273) or PfizerBioNTech (BNT162b2) vaccines were analyzed to determine the level of anti-SARS-CoV-2 viral antibodies. Eight weeks after the second vaccination, all volunteers demonstrated a high level of IgM and IgG. However, K417N, or E484K, or N501Y mutations had reduced or abolished the neutralization efficiency of 14 out of 17 most potent monoclonal antibodies investigated. In another study, it was noted that the UK B.1.1.7 strain did not reduce the effectiveness of the vaccine, and, the South African 1.351 strain had slightly reduced effectiveness [Citation18]. In a another study, the efficacy of PfizerBioNTech (BNT162b2) vaccine against UK B.1.1.7 mutated strain was examined [Citation19]. The neutralizing antibody responses were measured after a single immunization using pseudoviruses expressing the wild-type spike protein or the 8 mutations found in the UK B.1.1.7 strain. The vaccine sera showed a wide range of neutralizing titers of < 1:4 and up to 1:3449 to the wild-type spike protein, and, significantly reduced titers (by 3.85-fold) against UK B.1.1.7 variant [Citation20]. Likewise, decreased neutralization to UK B.1.1.7 was also noted with 9 out 10 monoclonal antibodies targeting the N-terminal domain and 5 out of 29 targeting the receptor-binding motif of the spike protein. When E484K mutation was introduced there was further loss of neutralization. Further research is required to determine the impact of these findings on protective vaccine efficacy with the various vaccines in use as the evolving UK B.1.1.7 lineage strain will likely acquire the E484K mutation [Citation20].
In an another study conducted by University of Texas and Pfizer-BioNTech, three SARS-CoV-2 virus mutants were engineered, namely N501Y, Δ69/70+ N501Y+D614G, and E484K+N501Y+D614G. Neutralization titers of twenty human sera from Pfizer/BioNTech vaccine (BTN162b2) which cross reacted with three engineered mutant virus were 0.81 to 1.46fold compared to the wild type strain titers. This shows that there may be minimal effect on the vaccine efficacy with viruses bearing these mutations. Further, it was recently announced (February 8, 2021), by the South African authority announced that the AstraZeneca vaccine failed to provide protection against the South African 1.351 mutant strain. This strain accounts for 90% of new COVID-19 cases in South Africa. As a result, the South African authority decided to hold off the roll-out of AstraZeneca vaccine [Citation21]. Likewise, most of the approved vaccine has demonstrated similar effectiveness trend. A summary of the effectiveness of approved vaccines against mutated strains are presented in .
Table 2. Summary of the effectiveness of some approved vaccines against new variants [Citation22]
It is clear that some of the current vaccines may not be as effective against the new emerging mutant strains and further studies are required to ascertain this. If they are not effective, new vaccines may be required to be developed. This is not uncommon and as seen with the influenza virus, vaccines are needed to be updated regularly in order to increase the protection capacity against new mutated strains. Moderna, USA recently reported that they are developing booster doses to cover the new strains [Citation18]. PfizerBioNTech are also moving forward to include mutated South African 1.351 strain into their vaccine. It is likely that there will be another long wait to get the new vaccine, causing further international travel bans, local lockdowns, restrictions, and an increase in the number of infections, deaths, and economic loss [Citation23].
3. Expert opinion
The COVID-19 pandemic has created a dire and unprecedented situation worldwide. It has caused significant damage to the world economy and millions of deaths in just over one year. Anti-SARS-CoV-2 vaccines were fast-tracked to reduce further fatalities. Due to an integrated effort and commitment by the scientific community there are vaccines available such as, PfizerBioNTech (BNT162b2), Moderna (mRNA1273), Russia’s Sputnik V, China’s Sinovac (inactivated), AstraZeneca-University of Oxford and Johnson and Johnson vaccine (). However, the emergence of new mutant strains pose another great hurdle to the effectiveness of the vaccines. A handful of studies are already reporting that the new strains are more than 50% more contagious than the wild-type Wuhan SARS-CoV-2 virus and the approved vaccines may not be as effective against these strains and warrant further studies to confirm the efficacy of the current vaccines. It is un-avoidable that new vaccines will need to be developed to complement or replace the current vaccines and included as a cocktail with the current vaccines. Attacking several sites at once using a cocktail significantly reduces the chances of coronavirus escaping the immune system, making therapy very effective. The development of vaccines using more conserved protein with a low chance of mutation could be another strategy to overcome this emerging issue.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
A reviewer on this manuscript has disclosed that they have received grant funding from Merck & Co., Inc. Peer reviewers on this manuscript have no other relevant financial or other relationships to disclose.
Author contributions
All authors contributed to the conceptualization, design, writing and editing of the article. All authors have read, reviewed and approved the final paper.
Acknowledgments
The authors would like to thank The Thelma and Paul Constantinou Foundation, and The Pappas Family, whose generous philanthropic support made possible the preparation of this paper. The authors would also like to thank the Immunology and Translational Research Group for their significant contribution. Md. K.H was supported by the Victoria University Postgraduate Scholarship and the Vice-Chancellors top-up Scholarship Award. This article was supported in part by the funds of the Place Based Planetary Health Grant PH098 to VA from VU Research, Victoria University.
Additional information
Funding
References
- Alwan NA. Surveillance is underestimating the burden of the COVID-19 pandemic.Lancet.2020;396(10252):e24.
- Hossain MK, Hassanzadeganroudsari M, Apostolopoulos V. Apostolopoulos, V. COVID-19 Vaccines in the Pipeline, Are Antibodies Adequate? Vaccines2021, 9, 241. Available from: https://doi.org/10.3390/vaccines9030241
- Hossain MK, Hassanzadeganroudsari M, Feehan J, et al.COVID-19 vaccines in the pipeline, are antibodies adequate?Vaccines (Basel). 2021;9(3):241.
- Wang Z, Schmidt F,Weisblum Y, et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. bioRxiv. 2021. DOI: https://doi.org/10.1038/s41586-021-03324-6.
- Ball P. The lightning-fast quest for COVID vaccines-and what it means for other diseases. Nature. 2021;589(7840):16-18. DOI: https://doi.org/10.1038/d41586-020-03626-1.
- Callaway E. The coronavirus is mutating-does it matter? Nature. 2020;585(7824):174–177.
- Wise J. Covid-19: new coronavirus variant is identified in UK. BMJ 2020;371 :m4857 DOI:https://doi.org/10.1136/bmj.m4857.
- WHO. UK’s new COVID-19 strain reported in at least 60 countries. ALZAZEERA, [cited 2021 Jan 30]. Available from: https://www.aljazeera.com/news/2021/1/20/uk-new-covid-strain-reported-in-at-least-60-countries-who
- Collier D, Meng B, Ferreira I,etalImpact of SARS-CoV-2 B.1.1.7 Spike variant on neutralisation potency of sera from individuals vaccinated with Pfizer vaccine BNT162b2. medRxiv. 2021. 2021.2001.2019.21249840. DOI:https://doi.org/10.1101/2021.01.19.21249840
- Mahase E. Covid-19: what new variants are emerging and how are they being investigated? BMJ2021; 372 :n158 DOI:https://doi.org/10.1136/bmj.n158.
- Volz E, Mishra S, Chand M, et al. Transmission of SARS-CoV-2 Lineage B. 1.1. 7 in England: insights from linking epidemiological and genetic data. medRxiv. 2021. 2020.2012. 2030.20249034.
- West JAP, Barnes CO, Yang Z, et al. SARS-CoV-2 lineage B. 1.526 emerging in the New York region detected by software utility created to query the spike mutational landscape. 2021. DOI: https://doi.org/10.1101/2021.02.14.431043.
- Tchesnokova V, Kulakesara H, Larson L, et al. Acquisition of the L452R mutation in the ACE2-binding interface of Spike protein triggers recent massive expansion of SARS-Cov-2 variants. bioRxiv. 2021. DOI:https://doi.org/10.1101/2021.02.22.432189
- WHO. SARS-CoV-2 variants. [ cited 31 December 2020]. Available from: www.who.int/csr/don/31-december-2020-sarscov2--variants/en
- Wise J. Covid-19: new coronavirus variant is identified in UK. BMJ. 2020;371:m4857.
- Li -D-D, Li Q-H. SARS-CoV-2: vaccines in the pandemic era. Mil Med Res. 2021;8(1):1–15.
- Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv. 2021. DOI: https://doi.org/10.1101/2021.01.18.427166.
- Wu K, Werner AP, Moliva JI, et al. mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv. 2021. 2021.2001.2025.427948. DOI:https://doi.org/10.1101/2021.01.25.427948
- Gupta R, Collier D, De Marco A, et al. SARS-CoV-2 B. 1.1. 7 escape from mRNA vaccine-elicited neutralizing antibodies. 2021.
- Xie X, Liu Y, Liu J, et al. Neutralization of spike 69/70 deletion, E484K, and N501Y SARS-CoV-2 by BNT162b2 vaccine-elicited sera. bioRxiv. 2021;27(4):620-621. DOI: https://doi.org/10.1038/s41591-021-01270-4.
- BBC. South Africa halts AstraZeneca jab over new strain. (Ed.^(Eds). 2021. [cited 2021 Feb 8]. Available from: https://www.bbc.com/news/world-africa-55975052
- Wee CZJCS-L. Coronavirus Vaccine Tracker. (Ed.^(Eds). 2021. [cited 2021 Mar 14]. Available from: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html
- Gretler C. New virus strain’s transmissibility to cause more deaths: study. [cited 30 Jan 2020]. Available from: https://www.bloomberg.com/news/articles/2020-12-24/new-virus-strain-s-transmissibility-to-cause-more-deaths-study