ABSTRACT
Introduction
The historical focus of vaccines on child health coupled with the advent of novel vaccines targeting adult populations necessitates exploring strategies for adult vaccine implementation.
Areas covered
This scoping review extracts insights from the past decade’s experiences introducing adult vaccines in low- and middle-income countries. Among 25 papers reviewed, 19 focused on oral cholera vaccine, 2 on Meningococcal A vaccines, 2 on tetanus toxoid vaccine, 1 on typhoid vaccine, and 1 on Ebola vaccine. Aligned with WHO’s Global Framework for New TB Vaccines for Adults and Adolescents, our findings center on vaccine availability, accessibility, and acceptance.
Expert Opinion
Availability findings underscore the importance of understanding disease burden for prioritization, multi-sectoral collaboration during planning, and strategic resource allocation and coordination. Accessibility results highlight the benefits of leveraging existing health infrastructure and adequately training healthcare workers, and contextually tailoring vaccine delivery approaches to reach challenging sub-groups like working male adults. Central to fostering acceptance, resonant sensitization, and communication campaigns engaging the communities and utilizing trusted local leaders countered rumors and increased awareness and uptake. As we approach the introduction of a new adult TB vaccine, insights from this review equips decision-makers with key evidence-based recommendations to support successful and equitable vaccinations targeting adults.
1. Introduction
Significant strides in child survival have been made through the successful introduction of childhood vaccines over the last several decades [Citation1]. The launch of the World Health Organization’s (WHO) Expanded Program on Immunization (EPI) in 1974, coupled with the financial support provided to low- and middle-income countries (LMICs) through the establishment of Gavi, the Vaccine Alliance, in 2000, has greatly contributed to successful vaccine introductions [Citation2]. As the global vaccine market continues to expand, the introduction of new vaccines remains a complex endeavor, marked by multifaceted challenges along the entire implementation continuum, from prioritization of vaccines, national and global level evidence-based policy-making, and procurement, as well as delivery- and uptake-related aspects, such as health system capacity, vaccine delivery, equitable access, and public acceptance [Citation3]. The introduction and implementation of a new vaccine for LMICs is a particularly challenging and complex undertaking that requires significant planning, stakeholder buy-in, funding, and preparation.
Historically, global immunization efforts have primarily focused on immunizing infants to prevent childhood diseases and prevent disease throughout lifetime, with limited resources and attention given to adult populations. To date, there are few vaccines specifically targeting adult populations, and of the few vaccines that are recommended by the WHO, access and uptake is poor as reflected by suboptimal coverage [Citation4]. In sharp contrast to the well-established pediatric immunization schedules, which efficiently target children from birth and are often intricately integrated with neonatal and maternal health services, the infrastructure and delivery mechanisms for reaching adults are not as robust, especially in LMICs, with opportunities for health system engagement less frequent in adulthood [Citation5]. With limited attention and resource allocation for adult vaccination programs, research also remains limited on successful implementation approaches and lessons for effectively reaching adults [Citation3].
The only currently available vaccine for tuberculosis (TB), the Bacille Calmette-Guérin (BCG) vaccine, has been around for over a century and while routinely provided in many LMICs, the neonatal vaccine has limited protection beyond infancy and thus does not meaningfully reduce community transmission [Citation6]. However, there is significant anticipation for a novel TB vaccine as several new adult tuberculosis vaccines are in the clinical pipeline and have advanced to phase III trials [Citation6]. These vaccines are designed with primary endpoints that include the prevention of infection, prevention of disease, prevention of recurrence, and therapeutic use [Citation6]. Such developments could significantly overcome the limitations of the BCG vaccine and reduce the burden of TB in affected communities with targeted and routine usage – a hopeful goal with the potential to be realized within the next several years. Learning from other vaccine introductions targeting adults is critical to prepare for TB vaccine implementation. This includes factors that are facilitating as well as factors that serve as barriers in new vaccine introductions. There are many factors that can negatively impact vaccine introduction, such as low uptake and suboptimal distribution among target populations, for example [Citation3,Citation7–9]. Successful introductions provide us with valuable insights for what approaches work at scale – accounting for the complexity of real world contexts – and allow us to map potential strategies for introductions going forward [Citation10,Citation11]. Understanding which factors affect vaccine introduction is essential for addressing potential challenges, as well as identifying national and local strengths which could be harnessed for successful introduction [Citation12]. To our knowledge, there is no literature which has systematically synthesized lessons learned from an extensive range of vaccine introductions among adult populations in LMICs. This paper synthesizes the insights and lessons learned from different vaccine introductions among adult populations in LMICs from the last decade (i.e. 2013 to 2023). We conducted this scoping review to inform decision-making regarding the potential introduction of forthcoming stage 3 TB vaccine candidates targeted for adults to contribute toward health system and community readiness, optimal implementation, and robust uptake. By synthesizing the literature in this way, we further aimed to underscore areas where countries could more effectively anticipate potential challenges specific to priority populations.
2. Methods
2.1. Research question
Our primary objective for this review was to systematically explore the lessons learned from recent introductions of new vaccines targeted for adults, limited to countries classified as low-income, lower-middle-income, and upper-middle-income as defined by the World Bank [Citation13], with the overall aim of informing future new vaccine rollouts for adults. We sought to identify and synthesize country-specific experiences, challenges, and recommendations related to factors influencing health system and community readiness and vaccine uptake, to guide preparations and implementation strategies for the introduction of novel safe and effective adult vaccines, which may become available for introduction in the next 5–7 years [Citation14]. We also examined how vaccine uptake and demand generation factors, such as social mobilization, community sensitization and engagement, and addressing vaccine hesitancy, varied across priority populations in countries.
2.2. Literature search strategy
We developed search terms aimed at identifying published literature that describe the lessons learned during a new vaccine introduction from January 2013 to May 2023. These search terms were developed in collaboration with an experienced informationist at the Johns Hopkins Bloomberg School of Public Health. The studies considered were from countries classified as upper-middle-income, lower-middle-income, and low-income based on their status at the time of publication, according to the World Bank definition [Citation13]. Multiple search terms were developed for the population of interest, exposures (immunization with the selected vaccines), and outcomes (availability, accessibility, and acceptability). We conducted this review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [Citation15] and the extension for scoping reviews (PRISMA-ScR) [Citation16]. The databases included in our search strategy were PubMed, Embase and SCOPUS. We excluded pre-prints and gray literature to uphold the peer-reviewed rigor of our final review.
2.3. Inclusion and exclusion criteria
We included studies that evaluated the implementation of licensed phase 3 vaccines during their initial introduction to low income, lower middle income, and upper middle-income countries from January 2013 to May 2023. Using initial literature searches, our professional expertise, and mapping exercises of vaccine introduction statuses in LMICs, we compiled an initial list of adult vaccines relevant for our study. The vaccines of interest included RTS,S vaccine for malaria, pneumococcal conjugate vaccines (PCV) for pneumonia, Human Papillomavirus vaccine (HPV) for cervical cancer, Typhoid conjugate vaccines (TCV) or Typhoid Vi polysaccharide antigen for typhoid, oral cholera vaccines (OCV) for cholera, tetanus toxoid for tetanus (administered to people during pregnancy), meningococcal vaccine for meningitis, yellow fever (YF) vaccine for yellow fever, and Ebola vaccine (EBOV) for ebola fever. We excluded influenza vaccines and maternal influenza vaccination from our selected list of antigens as it is not included in the Expanded Program on Immunization (EPI) of many LMICs [Citation17]. Moreover, in 2018, only 2% and 15% of countries categorized as low income and lower middle income, respectively, reported the existence of a national influenza vaccine policy, thus, underscoring the limited evidence of comprehensive influenza vaccination strategies in these specific income strata [Citation18]. Only studies with full-text accessibility were included in the analysis. This review excluded studies that did not specifically investigate or analyze lessons from the introduction of new vaccines in the last 10 years. Exclusion criteria also encompassed studies that reported on mathematical models and studies that did not utilize primary data, including literature reviews discussing lessons learned, meta-analyses, animal studies, investigations conducted on non-human specimens, in vitro studies, studies not in the English language, studies conducted in higher-income countries, conference abstracts, and conference posters. Since this analysis focused on findings from vaccines introduced in the adult population, we excluded studies specifically targeting age groups under 18 years of age, further eliminating many HPV studies. Furthermore, commentaries, opinions, and letters to editors were also excluded. At the time of undertaking this scoping review, WHO had commissioned a scoping review of lessons learned from COVID-19 vaccine implementation, and to avoid duplicating efforts in an area where WHO is better positioned to lead due to its global authority and expertise we have excluded COVID-19 vaccine studies in this review.
2.4 Framework for synthesis of results
We structured the synthesis of our key findings in alignment with the 3 A’s (Available, Accessible and Acceptable) of the WHO Global Framework to prepare for Country Introduction of New TB Vaccines for Adults and Adolescents [Citation14]. This framework delineates three goals along with corresponding milestones and necessary activities to foster preparedness at the national level. For availability of newly approved TB vaccines and rapid scale-up of coverage, advance planning is critical to establish a sustainable and timely supply within the country. This proactive approach aims to engage vaccine manufacturers, facilitates regulatory approval, drives policy recommendations, enables affordable procurement at the national level, and ensures comprehensive data collection during clinical trials or pre-implementation research. For ensuring accessibility, a well-defined plan for delivering the vaccine to those in greatest need, irrespective of socio-economic status, geographical location, or other potential barriers to access, is highly recommended. Tailoring delivery strategies to each country’s unique circumstances is essential, taking into consideration financial constraints to ensure the most practical and cost-effective approaches. Even if a vaccine is available and accessible, its acceptance by communities or at-risk populations—especially when targeting a new priority demographic—requires extensive community engagement and demand generation efforts in advance. These may involve a diverse set of stakeholders ranging from policymakers and healthcare professionals to tuberculosis-affected communities and survivors, and other eligible patient groups.
2.5 Data extraction and analysis
A data extraction template was created within Covidence (Veritas Health Innovation Ltd, Australia) to systematically extract relevant information. This template was structured to capture study objectives, targeted study populations, geographical regions, disease/vaccine settings, the WHO global framework domain addressed (availability, accessibility, acceptability), reported outcomes, sample sizes, synthesis of key findings, strategies employed for vaccine delivery, assessments of health system readiness, as well as details regarding social mobilization, community engagement, communication strategies, and lessons learned from the implementation program.
3. Results
A total of 22,529 studies were imported into Covidence software for screening and review (see for PRISMA flow diagram). Following the removal of duplicates (n = 15,670), a total of 6,859 articles remained for initial screening. Four independent reviewers (AM, AG, AB and OG) conducted screening of titles and abstracts. 1,039 studies underwent a subsequent independent full-text review for eligibility by four reviewers. Studies that were initially included after title and abstract screening but were later excluded (n = 1,014) comprised studies not grounded in the actual implementation of vaccine introduction and exclusively centered on modeling, reviews discussing lessons learned from vaccine introduction and implementation but lacking primary data, studies conducted in age groups of under-5, 5–9 years and adolescents (under 18 years of age), studies from high-income countries and those that reported findings from COVID-19 vaccine introduction. Review articles were identified and screened for additional references; however, they were not incorporated into the final selection of articles for data extraction as part of our established exclusion criteria. Conflicts were documented and resolved during a comprehensive review of full texts by a third reviewer that had not previously reviewed the text (RL or AM).
Figure 1. PRISMA flow diagram.
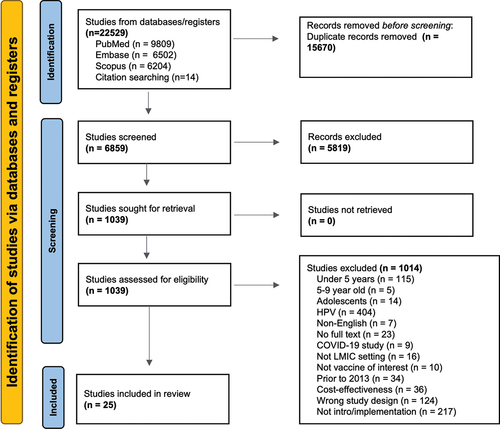
We identified 25 studies for our synthesis ( for an overview of the relevant data of the 25 publications). The studies included vaccines targeting cholera (n = 19), meningitis A (MenA) (n = 2), tetanus toxoid vaccine (TTV) in maternal women (n = 2), typhoid (n = 1), and ebola (n = 1). Most studies touched on each of the 3 A’s – availability, accessibility, and acceptability – of the WHO framework.
Table 1. Brief overview of included study characteristics (n = 25).
3.1. Availability
The availability of new vaccines with sufficient, sustainable, and timely supply is contingent upon key factors, including reviewing national epidemiological data, stakeholder involvement in defining the national policy pathway for new TB vaccines and informative research to support introduction decision-making and having procurement plans developed and ready. In line with the factors influencing availability, 11 of the 25 studies reviewed underscored the importance of extensive stakeholder engagement in policymaking, generating robust local disease burden data, and meticulous resource planning and mobilization as critical elements contributing to the successful introduction and adoption of new vaccines [Citation9,Citation19–28].
These 11 studies evaluated the implementation of OCV, meningococcal vaccines, typhoid vaccines, and maternal tetanus vaccines across Bangladesh, Cameroon, India, Kenya, Mali, Somalia, South Sudan, Uganda and Zimbabwe in emergency as well as campaign settings. The target population examined in these papers included the general adult population, and specific populations including, fisherman, refugee populations (displaced populations), and pregnant females. We summarize findings related to each factor in the subsequent sections.
3.1.1. Stakeholder involvement
In several studies, factors regarding policy-making and the steps to make a new vaccine available were discussed. Stakeholder engagement was noted in eight studies as a critical factor for successful implementation of immunization programs [Citation9,Citation19–22,Citation25,Citation27,Citation28]. Across the studies, the range of stakeholders involved included government and city officials, national immunization technical advisory groups (NITAGs), immunization program managers, global partners, such as WHO and UNICEF, community leaders, healthcare workers (HCW), and members from other sectors such as water, sanitation, and hygiene (WaSH). (See for an illustrative list of stakeholders involved in policymaking identified from these eight studies).
Table 2. Overview of stakeholders involved in policy-making and preparatory activities.
In South Sudan, the success of the OCV campaigns relied on strong leadership and collaboration from both the Ministry of Health (MoH) and the World Health Organization (WHO), with a key emphasis on clearly defining roles and responsibilities for various stakeholders, including designating a lead agency for each site [Citation20]. Similarly, in Uganda, under the leadership of the MOH, several stakeholders including WHO, UNICEF, UNHCR, and Medecins sans Frontiers contributed to the campaign, coming together prior to the campaign to identify roles and coordinate synergistic tasks [Citation25]. In both Bangladesh and Cameroon, the success of OCV campaigns was facilitated by broader stakeholder engagement, including proactive engagement and collaboration with diverse community stakeholders, such as community representatives, religious leaders, and media personnel [Citation21,Citation22]. This involvement commenced at least a month before the launch of the vaccination program. Bangladesh reported successful outcomes in terms of vaccine coverage through the collective efforts of the community members and volunteers in managing crowds and attending to those awaiting vaccination [Citation21]. Cameroon’s OCV campaign highlighted the active involvement of religious, administrative, and community leaders in building trust in the community and encouraging more people to get vaccinated as well as to mitigate external influences such as rumors and anti-vaccine campaigns. In Mali the preparatory work for the MenA campaign was credited with increasing multisectoral collaboration between the MoH, National Institute for Infectious Diseases, and the agency for social mobilization [Citation9,Citation22]. The findings of engaging multiple stakeholders, from national, to regional, to local community stakeholders align with the goal of acceptability of the vaccine – a necessary goal of the policy development and success. Studies demonstrating active community involvement and advocacy initiatives preceding the launch of adult vaccination programs consistently reported higher acceptance and uptake of the vaccines due to the concerted social mobilization efforts led by community and religious leaders, and other active community participants.
3.1.2. Understanding of local disease burden
Five studies noted the importance of local disease burden knowledge for demand generation and vaccine prioritization [Citation19,Citation23–26]. A baseline recognition of the magnitude of the disease burden problem as well as an understanding of the potential impact of a vaccine were significant for the prioritization of new vaccines like tetanus toxoid vaccine, oral cholera vaccine, and typhoid vaccines among decision-making bodies and beneficiaries in five studies. In Kenya, policy maker respondents cited knowledge of local disease burden as an important consideration for prioritizing and introducing new maternal vaccines [Citation19]. Policy makers in Malawi reported that while it is preferred, country-specific vaccine efficacy, safety, and cost effectiveness data were not required for decision-making, provided quality evidence from nearby countries was available [Citation24].
The campaign against typhoid in Harare, Zimbabwe emphasized the importance of knowledge of local typhoid patterns and collaboration between the Ministry of Health and its partners for vaccine acquisition, strategy selection, and regulatory approval [Citation26]. In an OCV study conducted in Uganda, it was found that 77% of community household survey respondents understood that the vaccine was one of the ways to prevent cholera. A survey among HCWs involved with the vaccinations revealed that most respondents were knowledgeable about the cause of cholera and the importance of safe water in cholera prevention [Citation25]. This high level of knowledge of cholera prevention indicates that awareness is an antecedent for uptake.
3.1.3. Adequate resource planning
As touched upon by ten studies, adequate resource planning was crucial for the availability of vaccines and the success of vaccine programs, with studies highlighting the importance of efficient use of available resources like health workers and logistics [Citation21,Citation26], consideration of local climate conditions [Citation22], monitoring of routine health services alongside campaign vaccine coverage [Citation9,Citation25,Citation29], and overcoming challenges for timely vaccine arrival [Citation20,Citation23,Citation25,Citation30,Citation31]. In Zimbabwe, the typhoid vaccination campaign succeeded in part because of operational experience gained from a recent and successful cholera vaccination campaign conducted in the same communities, in addition to benefiting from existing training resources that were utilized to prepare staff for monitoring adverse events following immunization (AEFI) [Citation26]. Similarly, Bangladesh’s OCV campaign used existing cold chain logistics for vaccine delivery along with other EPI vaccines, leveraging an existing immunization infrastructure which already stretches to remote communities [Citation21]. However, the OCV campaign conducted in Cameroon suggested that the implementation of mass vaccination campaigns should be done in dry seasons to facilitate effective implementation and resource management, especially in seaside towns [Citation22]. The importance of meticulous planning, integration with routine services, and resource allocation, was exemplified in Mali’s Men A campaign [Citation9,Citation29]. The MenA introduction showed several positive effects including enhanced governance, effective communication and surveillance, strong political commitment, and high community awareness of the disease reaching 80% of people in the community surveyed. However, the campaign led to an increase in the health workforce workload for the duration of the campaign, which was substantial in remote regions, and disrupted routine health services, particularly routine vaccination and to some extent, antenatal care (ANC) – data showed a 79% drop in daily child vaccinations during the campaign [Citation29]. The study recommended that when introducing a new vaccine through a campaign, coverage of routine health services should be monitored alongside campaign vaccine coverage in order to highlight where and how long routine services are disrupted, and to mitigate risks to these essential services [Citation29]. Meanwhile, Uganda’s OCV campaign revealed resource planning challenges that hindered campaign implementation, including issues with timely payment for campaign staff and problems with field transport [Citation25]. Another logistical planning issue Uganda faced were the unpredictable and non-committal campaign dates for the second round of vaccination due to unknown timelines of dose shipment and custom clearance, which in turn contributed to the decreased second OCV dose coverage [Citation25].
While some planning measures are within the control of countries, certain factors such as the availability of supply often are not. Challenges such as supply shortages and insufficient coverage of specific population cohorts highlight the need to consider flexible alternative vaccination strategies [Citation20,Citation25,Citation30,Citation31]. This may include highly targeted vaccination campaigns and single-dose vaccination strategies. Studies in Zimbabwe and South Sudan highlight the feasibility and effectiveness of these campaigns, especially in urban areas and in response to outbreaks [Citation23,Citation31]. In an OCV campaign conducted in Lusaka, a single-dose approach was employed to maximize vaccination coverage [Citation23]. With insufficient vaccine supply to cover at-risk populations during a 2015 cholera outbreak in Juba, South Sudan, the first public health use of a single dose regimen of OCV – half the standard dosing regimen – was implemented using a neighborhood targeted approach that prioritized vaccinating neighborhoods with significant transmission and vulnerable high-risk groups such as HCWs, prisoners, and internally displaced people (IDPs). This campaign achieved nearly 70% coverage and found the strategy to be a feasible and well-accepted way to combat supply shortages in a low-resource, volatile setting [Citation31].
3.2. Accessibility
Following the decision to introduce a vaccine, accessibility of the vaccine to its target audience is contingent on several factors such as vaccine implementation strategies, delivery systems in place, and sustained financing systems established [Citation14]. Across the studies included in our review, 18 studies touched on facilitators and barriers of accessibility. These were related to vaccination delivery models, challenges in accessing hard to reach individuals such as working male adults, and available existing health infrastructure and HCW education and program integration.
3.2.1. Vaccination service delivery models
Whether a vaccine is introduced as a routine or campaign vaccination can depend on factors such as the public health needs, the target population, and characteristics of the vaccine. The delivery platforms within these initiatives similarly vary based on the setting, healthcare infrastructure, vaccine characteristics, and target population. Routine vaccinations integrated in a country’s standard immunization schedule are typically administered on an ongoing basis at an established fixed site such as a healthcare facility or at schools when targeting adolescents. Campaigns tend to have specific objectives and are implemented on a more temporary basis as well as on a mass scale to capture a large group of individuals at once – such as, in response to an outbreak or to target specific populations like an underserved group. In all but the two studies on TTV routine introductions in Malawi and Kenya [Citation19,Citation24], introductions were implemented through campaigns. More specifically, the OCV, TCV, EBOV, and MenA studies captured in our review utilized a campaign strategy. Catch-up campaigns are one type of campaign to reach individuals who were missed and did not receive a routine vaccination at the time they should have within the schedule, or otherwise missed a dose from a campaign. The MenA study in Mali was introduced using a three phased mass catch-up campaign approach, which prevented the need for more expensive reactive campaigns but also had the drawback of causing disruptions to other ongoing routine services [Citation9].
In addition to fixed site vaccinations commonly used in routine vaccinations, delivery strategies can include door-to-door vaccination where community health workers (CHW) visit individual homes to administer the vaccines, mobile clinics that are versatile to set up temporary clinics in various locations, and self-administered vaccination where prefilled vaccines are given to individuals to administer to themselves at home. OCV studies in Malawi and Bangladesh both assessed approaches like a self-administered second dose strategy in which individuals received the second dose and instructions for self-administration, and Malawi also examined directly observed vaccination, where healthcare workers administered vaccines directly to the recipients [Citation32,Citation33]. The Community-Led Self-Administered Second Dose strategy entrusted community leaders with the responsibility of delivering the second vaccine dose, and this strategy was used to foster community engagement [Citation32,Citation33]. This strategy proved successful for improving coverage of OCV in Malawi and Bangladesh, with > 98% of a subsample of household respondents surveyed in Bangladesh appreciating that the novel method, consisting of bringing home a second oral dose in a reusable plastic ziplock bag to self-administer, was more convenient and practical than the usual method [Citation24,Citation32,Citation33].
While limited details were typically provided on the lessons from door-to-door strategies, OCV studies in Zambia, Uganda, Malawi, and South Sudan did note that the door-to-door strategies delivering vaccines directly to households often minimized barriers to access [Citation23,Citation25,Citation34–36]. Authors of the single dose OCV study in South Sudan reflected that given the highly targeted nature of the campaign to vaccinate the high transmission neighborhoods and high-risk individuals first, perhaps a door-to-door strategy would have been more appropriate than the fixed-site and mobile team strategy that was implemented [Citation31]. A combination of both door-to-door and fixed-site strategies, complemented by mobile teams reaching remote communities, further improved vaccine delivery efforts, particularly in hard-to-reach areas [Citation23,Citation26,Citation35].
3.2.2. Missed opportunities and challenges with hard-to-reach populations
Across all studies mentioning reasons for missed vaccinations, absence from home and limited convenient access to fixed sites were identified as key reasons [Citation25,Citation27,Citation34,Citation37–39]. In Somalia’s first acute OCV campaign, among the individuals who reported having missed a vaccine in the study’s household coverage survey, 42% said it was due to not being home [Citation27]. During Uganda’s first OCV campaign, it was found that while the vaccine was readily accepted among the community, those who did not take the vaccine were mostly among those missed when not at home [Citation25]. Notably, working male adults were highlighted in six studies as a group most often missed during campaigns [Citation31,Citation32,Citation34,Citation37–39]. An OCV campaign in Nigeria described how the use of fixed sites and house-to-house strategies favored women who tend to spend more time at home, in comparison to men who spend most time working outside of the house [Citation38]. Similarly, South Sudan’s OCV campaign also found adult men to be 27% less likely to have received the vaccine compared to adult women. Explanations for the particularly low adult male coverage in one commercial part of town hypothesized to be due to male businessmen working in the area during the day and commuting outside of the city after [Citation31]. Bangladesh’s OCV campaign revealed that lower vaccine coverage among adult males may have stemmed from the misconception that vaccines are mainly for mothers and children, in addition to the barrier of frequent absence from home due to travel (58%) and business (26%) [Citation37]. A study of Malawi’s first large scale OCV campaign similarly found coverage for adult males to be lower than women and children – the main reason for non-vaccination being absence from home during the campaign’s period [Citation39].
Authors described a range of strategies to improve uptake amongst adults including extending vaccination hours to accommodate working adults [Citation21,Citation26,Citation32,Citation37], extending the campaign to a non-working day [Citation21,Citation26,Citation32], setting up vaccination sites in locations frequently visited by adults (i.e. religious centers, markets and trading centers, and other public social gathering spots) [Citation23,Citation32,Citation33], conducting education campaigns to address misconceptions [Citation37], and using a combination of vaccination strategies (fixed, mobile, workplace, door-to-door) [Citation33,Citation35]. The convenient and well accepted second dose self-administration strategy tested in Bangladesh’s OCV campaign presents another novel strategy, specific for oral vaccines, to better serve hard-to-reach populations [Citation32]. Interestingly, despite the improved reach of the innovative self-administration strategy, the study still noted that adult men were difficult to reach as most were factory workers gone from early hours to late at night [Citation32]. In a reactive OCV campaign targeting fisherman in Lake Chilwa in Malawi, floating homes used by fisherman called ‘zimboweras’ were identified as the start of the outbreak and these fishermen were a particularly challenging subset to reach given the remote location and general lack of access to safe water and sanitation. A strategic effort was made to use the ‘tea rooms’ in the cluster of larger zimboweras and an area where daily goods are sold and food is prepared, as the delivery point for the vaccines, resulting in high acceptability and uptake [Citation33]. Similar to selecting convenient communal locations to deploy the vaccine, selecting an amenable time for campaigns was also proven to be an important factor for uptake. For example, Mozambique’s OCV campaign experienced lower than expected uptake due to the campaign rounds coinciding with school holidays – a time when most households move away to support farming and food production [Citation40]. Similar to avoiding school holidays, Cameroon’s OCV campaign found that selecting a more favorable climate season – in this case, the dry season – benefits OCV uptake [Citation41]. In addition, choosing a former immunization venue or other well-known community venue [Citation21,Citation23,Citation26] and utilizing technology such as geo-spatial mapping to better identify favorable venues [Citation35] were seen as ways to better ensure accessibility. Two studies, a Zimbabwe typhoid and Bangladesh OCV study, found success in keeping vaccination sites open all day and on weekends to reach those unable to receive vaccinations during the workday; the former distributed vaccines at churches, trading centers and markets to further reach more of the population [Citation26,Citation32]. provides a summary of strategies to improve reach and adult vaccination uptake from eight studies.
Table 3. Innovative strategies for adult vaccination uptake.
3.2.3. Health infrastructure, educating workers, integration
Five studies specifically emphasized the benefits of leveraging and strengthening existing EPI and health infrastructure [Citation21,Citation25,Citation27,Citation34,Citation39]. OCV introductions in Somalia, Bangladesh and Malawi found existing EPI cold chain infrastructure was adequate for additional vaccines, alleviating pressures to expand a country’s cold chain system [Citation21,Citation27,Citation32,Citation34,Citation39]. Piggybacking off past campaigns also eased implementation efforts in areas like Somalia, where experienced social mobilizers from the Polio Eradication Initiative (PEI) were utilized to catalyze the intense sensitization efforts that were made two days prior to an OCV campaign. Using Somalia’s existing cold-chain for EPI programs and readily available and experienced social mobilizers helped support the novel OCV campaign implementation and was felt to have contributed to the high levels of acceptability and coverage [Citation27]. New introductions also served as an opportunity to improve existing health systems by strengthening health systems technology such as AEFI reporting systems and improving data collection and reporting mechanisms [Citation9,Citation29]. For example, through the implementation of the MenA campaign in Mali, an emphasis of generating awareness of potential AEFIs for the new MenA vaccine brought upon a renewed attention to strengthening existing AEFI surveillance systems. In addition, disease surveillance staff capacity was also reported to have been enhanced as Mali newly introduced case-based surveillance of meningitis along with the vaccine rollout [Citation9].
Ensuring healthcare workers were well informed and educated on aspects such as disease etiology, vaccine characteristics and administration details, and AEFI management was found to play an important role in a successful vaccine program [Citation25,Citation42]. Ahead of an Ebola campaign in Nigeria, authors found little knowledge of the vaccine among HCW, reporting that none of the 193 participating HCW had correct knowledge of the ebola virus vaccine [Citation42]. After health education on Ebola virus vaccine, an overall increase in acceptance for the vaccine by HCW was found across the states [Citation42]. Partly due to the rapid emergency rollout timeline of Uganda’s first OCV campaign, surveyed staff (consisting mostly of vaccination team members) revealed 29% did not understand how to detect and manage AEFIs, calling for additional training needs [Citation25]. Other studies in Malawi, Mali, and Zambia noted coordinating trainings prior to campaigns as a necessary activity to ensure HCW were sufficiently educated and prepared [Citation9,Citation23,Citation24].
Integrating vaccine delivery with the delivery of other health services was deliberately discussed in two studies [Citation24,Citation29]. In Malawi, a successful strategy to make new maternal vaccines accessible was to integrate delivery with other antenatal care services [Citation24]. Malawi’s ANC systems effectively attracts pregnant women to access health services by fostering an environment that encourages familial involvement, including the option for women to be accompanied by their male partners. This in turn extends to the uptake of vaccines by women in the community when vaccination services are integrated within ANC visits. Health workers in a TTV study in Malawi described a perhaps more intense approach where health workers first offered women to receive TTV before being offered other services [Citation24]. In contrast, because the mass MenA campaign in Mali was provided in a traditional vertical manner and described to not have been well integrated with other health services, the campaign disrupted routine services in the majority of surveyed health facilities (67%) during the campaign period and the authors described missed potential opportunities for health systems strengthening – such as fostering greater collaborations among health service partners and delivering other health promotion or nutrition services to the population [Citation29].
3.3. Acceptability
While the availability and accessibility of a vaccine are important factors for a new vaccine introduction, they remain insufficient for program success if the uptake and acceptance of the vaccine by the target populations is missing [Citation14]. Therefore, it is essential that deliberate efforts are made toward understanding local vaccine perceptions, generating demand for the vaccine, effectively communicating vaccine information, and addressing questions and concerns to build confidence for a vaccine. Acceptance toward a new adult vaccine introduction was generally high across all studies. Several key factors impacted acceptance among the studies including knowledge of the disease and vaccine characteristics, rumors and how information was spread, community engagement, and communication and sensitization plans. In this review, all 25 papers at least briefly noted factors relating to acceptance of the vaccine programs.
3.3.1. Understanding about the disease and vaccine
Understanding vaccine safety and efficacy played a critical role in acceptance for many of the introductions with variability in community-level knowledge about disease transmission and prevention across the studies [Citation24,Citation25,Citation28,Citation37]. A greater need for community sensitization was reported in surveys following Uganda’s OCV campaign provided that those with more education were twice as likely to know the required number of doses as those with no education [Citation25]. When communities were lacking in awareness about the disease or the importance of the vaccine, uptake and policy implementation was found to be hindered [Citation19,Citation37]. For example, an OCV campaign in Bangladesh observed that urban males and higher-income groups particularly were less likely to accept a new vaccine as they perceived low vulnerability and susceptibility to diseases [Citation37]. Policy implementers interviewed in Kenya regarding TTV noted insufficient knowledge on the disease, and particularly misunderstandings of the vaccine often fueled by rumors, limited the acceptance of new vaccines and undermined vaccine rollout [Citation19].
Characteristics specific to oral vaccines were seen to have an impact on acceptance in both negative and positive ways. The ease of administration of oral vaccines and as an alternative to an injection often contributed to the acceptance of OCV [Citation32,Citation37]. However, OCV uptake was impacted by perceptions and tolerability of the vaccine’s taste and smell in India and Bangladesh [Citation28,Citation37]. A study on India’s OCV campaign found that bad taste of the vaccine (32%) and bad smell of the vaccine (25%) were reasons behind incomplete vaccination among one-dose households [Citation28].
3.3.2. Rumors and sources of information
Vaccine hesitancy due to fears and distrust from rumors and misconceptions were commonly described reasons for vaccine refusal [Citation9,Citation19,Citation24,Citation33,Citation37,Citation42]. Fear created by misinformation circulating on the contents of the Ebola vaccine and the potential risk of contracting EVD from the vaccine itself were noted by interviewed HCWs in Nigeria [Citation42]. In Malawi’s Lake Chiwa OCV study, fisherman reported rumors of forced eviction or attempts to hurt the fisherman with the injections as an ulterior motive tied to the campaign [Citation33]. In a study targeting urban high-risk populations in Bangladesh for OCV, rumors that the campaign was using the population as ‘guinea pigs’ to test the vaccine negatively affected community perceptions and hindered second dose uptake [Citation37]. Pregnant women, their family members, and health workers in a study of TTV in Malawi, expressed concerns of misperceptions that the vaccine is confused for a contraceptive, particularly given that the most common contraceptive utilized in Malawi resembles the TTV as both are injectable and distributed by community health workers [Citation24]. While pregnant females were generally receptive to vaccinations when available, misconceptions such as the one noted above or that vaccines cause abortion or infertility were present in Mali’s MenA, Malawi and Kenya’s TTV, and Malawi’s Lake Chilwa OCV study [Citation9,Citation19,Citation24,Citation33]. Policy-makers and implementers interviewed on tetanus toxoid vaccine implementation and the future of maternal vaccines in Kenya cited well-educated and respected individuals, including Catholic doctors staunch in their beliefs that the vaccine was tied to family planning, played a role in the controversies surrounding TTV and the prospect of future maternal vaccines [Citation19].
Three studies assessed where and from whom community members were receiving information that they trusted in order to help identify sources to leverage for spreading sensitization information and tackle misconceptions [Citation21,Citation27,Citation28]. In Somalia’s OCV campaign, household coverage surveys showed community health workers to be the main source of information (65.1%), followed by the radio (63.9%) [Citation27]. Notably, trusted sources of information about the vaccines and campaigns typically included neighbors, relatives, and CHW [Citation21,Citation27,Citation28]. In several OCV studies in Bangladesh, Somalia, and Guinea, campaigns that had oral dissemination of campaign information where neighbors or family members recommended the vaccine had greater acceptance [Citation21,Citation27,Citation30]. Studies with a maternal population noted that trusted health care advisors were particularly key sources of information for pregnant women [Citation24,Citation29]. Religious leaders and the growing access to social media, where small anti-vaccine campaigners are able to amplify their perspectives, were noted as sources hindering TTV uptake in Kenya and ones that could potentially negatively affect future vaccine implementation [Citation19].
3.3.3. Community engagement
Community engagement, sensitization activities, and communication strategies (especially prior to the campaigns) were key to raise awareness, build confidence, and generate acceptance among the target populations [Citation9,Citation19–24,Citation26,Citation29–35,Citation37–39,Citation41,Citation42]. Community engagement generally refers to the involvement and active participation of the local community in the vaccine program with the aim of fostering collaborative relationships between the community and program staff [Citation43,Citation44]. Sensitization generally refers to the process of raising awareness in local communities through effective communication strategies and equips individuals with information on the vaccine and campaign.
Utilizing community volunteers and community leaders – especially religious leaders – was perhaps the most prominent theme across all studies to generate vaccine acceptance, being noted in ten studies [Citation21–24,Citation26–28,Citation33,Citation41,Citation42]. For example, the typhoid introduction in Zimbabwe collaborated with social mobilizers from several churches to mitigate possible vaccine hesitancy among religious communities [Citation26]. Similarly, an OCV campaign in Cameroon targeted raising awareness of worshippers by visiting places of prayer and equipped several religious and community leaders to sensitize their communities [Citation22,Citation41]. In Malawi, pregnant women and their family members highlighted a desire for greater involvement of community leaders in the TTV initiative, indicating a demand for more support from village leaders and CHWs to encourage care seeking [Citation24]. In Somalia, in addition to the use of experienced polio social mobilizers (as previously described to supplement intensive sensitization efforts of local health authorities), volunteers and community leaders were noted to have been instrumental in achieving high acceptance and coverage in areas not accessible to humanitarian agencies, such as individuals displaced by drought in IDP camps [Citation27].
Engaging the community through public meetings to answer questions and provide information on the new vaccine roll-out, its purpose and importance, and logistical information prior to the launch, was a common method used in Bangladesh, Zambia, Cameroon, South Sudan, and Mozambique OCV studies to form a connection with the community and raise awareness [Citation23,Citation31,Citation32,Citation40,Citation41]. Meetings were strengthened when led by trained field workers and included community leaders, along with a mix of stakeholders from the community, government, and other partners [Citation23,Citation31,Citation32,Citation41].
3.3.4. Communication strategies and sensitization
Timely and accurate information dissemination about the safety and efficacy of the vaccines, importance of uptake, and availability of other prevention measures and treatment options, were essential for building confidence and trust in the vaccines in all studies assessing communication methods. Sensitization for communities to learn and become aware of the vaccine and vaccination program through these communication strategies is therefore pivotal. Elements of community engagement, communication strategies, and sensitization efforts are often closely linked.
Six studies mentioned the use of the press and a multi-media social mobilization campaign prior to delivery of the vaccines as part of sensitization efforts [Citation23,Citation26,Citation28,Citation34,Citation37,Citation40]. The use of trained journalists and bloggers, newspapers, radio, and TV ads to raise awareness and disseminate campaign details was common [Citation22,Citation26,Citation27,Citation31,Citation34]. To increase the acceptability for completing the full course of OCV vaccines being rolled out, Bangladesh maintained communication with news media regarding the program’s objectives [Citation37]. However, a study in Guinea also emphasized the importance of oral dissemination for areas without access to TVs and radios. In this case, the Guinea campaign did not utilize modern media for its communication strategy and instead had health promoters and village leaders visit each community 2 days prior to the vaccination day to provide educational and awareness information, with more populated regions being visited by local outreach workers through door-to-door mobilization [Citation30].
Advocacy campaigns were also conducted in many communities through door-to-door canvassing, use of mobile loudspeakers and megaphones, and vehicles with sound systems to advertise the vaccinations [Citation21,Citation23,Citation28,Citation30,Citation40]. Several studies briefly mentioned the use of communication materials to increase campaign visibility, including flyers, posters, banners, leaflets, and badges [Citation21,Citation22,Citation26,Citation28,Citation30,Citation32]. In two papers assessing Bangladesh’s OCV rollout, communication strategies were supplemented with the use of cell phone reminders via text or call – a tactic found particularly helpful for reminding recipients of their second dose [Citation21,Citation32]. ‘Miking’ or local announcements on loudspeakers were utilized in Bangladesh in addition to banners and interpersonal communication, to generate awareness and encourage uptake [Citation32]. In Mozambique’s OCV campaign, the use of megaphones was found to be the most effective tool in disseminating information on the vaccination plan as well as mobilizing the community [Citation40].
While short-term sensitization was often the reality, several studies – Bangladesh, Cameroon, Zambia, Guinea and Somalia for OCV, Mali for MenA, and Zimbabwe for typhoid – noted the benefit of intensive sensitization campaigns, with some emphasizing efforts should be conducted several weeks prior to vaccination launch and sustained throughout in order to raise sufficient awareness [Citation22,Citation23,Citation26,Citation27,Citation29–32,Citation34,Citation41]. One of the factors negatively associated with Uganda’s OCV campaign was the lack of community sensitization that was likely due to the urgency of the rapid response not allowing for much preparation time [Citation25]. Efforts to tailor sensitization and communication efforts to specific groups within the population, such as different religious groups like the social mobilizers previously described from churches in Zimbabwe’s TCV campaign [Citation26], mobile working men [Citation31,Citation32,Citation34,Citation37–39], and other hard to reach populations such as the fisherman population of Lake Chilwa Region heavily targeted during a Malawi OCV campaign [Citation33], was noted as an important way to increase coverage.
4. Discussion
The scoping review encapsulates a decade of experiences in adult novel vaccine introductions in LMICs, shedding light on the multi-dimensional factors influencing vaccine availability, accessibility, and acceptance. Vaccines included in the studies were MenA, TTV, OCV, TCV and EBOV. Reviewing and synthesizing these articles allowed us to glean lessons learned from a diverse range of adult vaccine introductions, providing valuable insights for forthcoming global-, regional- and national- level decision-making concerning the prospective introduction and implementation of new adult vaccines including the novel TB vaccine candidates among adults. depicts some of the key lessons learned and implications for future TB (and other novel) vaccine introductions for adults.
Figure 2. Key lessons learned for new adult vaccines.
4.1. Availability
In relation to availability, several key themes emerged that significantly impact the introduction and implementation of vaccines. Among these, engaging a broad spectrum of stakeholders, including government bodies, international organizations, community leaders, and healthcare workers, was pivotal. This multi-sectoral collaboration creates a conducive environment for policy formulation, resource allocation, and community acceptance, aligning vaccine introduction endeavors with overarching public health goals. As a new TB vaccine may not be situated within National TB Programs, forging such collaborations that potentially include new vaccination partners and implementers will be crucial for successful rollout.
Additionally, understanding local disease burden is pivotal for vaccine prioritization and tailoring vaccine introduction strategies to the prevailing epidemiological conditions. This underscores the necessity for robust epidemiological surveillance. Often, the success of vaccine campaigns is a reflection of policy adaptations made in response to local needs. Furthermore, country-specific data on vaccine efficacy, safety, and cost-effectiveness significantly enhances the prioritization process. The intertwining of vaccine prioritization with both perceived and actual disease burden facilitates the crafting of demand-generation initiatives that align with the community’s health beliefs and practices, engendering a more tailored and effective approach to vaccine introduction.
Resource planning emerged as a cornerstone for ensuring vaccine availability. The narratives identified surrounding vaccine supply shortages and the meticulous planning required to circumvent such challenges underscore the complex coordination of logistics and resources entailed in vaccine introductions. The importance of timely vaccine arrival, efficient resource utilization, and strategic resource allocation, including health workers, in sync with local context and health system capacities, are accentuated across various vaccine introduction experiences. The timelines for resource planning and resource allocation are heavily impacted in emergency and outbreak settings compared to routine or campaign vaccine introductions. Whereas campaigns have the benefit of monitoring progress and adapting strategies based on feedback loops, outbreak settings necessitate an immediate strategy for the deployment of resources. However, the feasibility of alternative vaccination strategies in response to resource shortages elucidates the potential for flexible operational frameworks in vaccine programs. Such flexibility like the single-dose approach used in OCV campaigns in South Sudan and Bangladesh notably increased delivery efficiency during supply constraints. By minimizing the need for multiple doses, these strategies simplify logistics, often improve acceptability, reduce costs, and quickly reach high-risk populations, crucial for outbreaks and remote hard to reach settings. Though not always feasible depending on the setting and specific vaccine, a single dose strategy can be implemented for other vaccination efforts, such as HPV, provided it meets all safety standards and it does not compromise the vaccine’s efficacy [Citation45].
4.2. Accessibility
Several themes concerning the accessibility of vaccines were identified. Notably, an array of vaccine delivery models, each with its unique set of merits and challenges, were identified. Mass campaigns were predominantly employed, albeit innovative strategies such as the community-led self-administered second dose strategy and door-to-door campaigns also showcased promise in enhancing accessibility. The diversity in delivery strategies echoes the necessity of a contextually nuanced approach to vaccine delivery, tailored to the socio-cultural and logistical landscape of the target population(s). To address the vulnerability of populations at risk of outbreaks, innovative strategies were employed, utilizing communal religious venues and popular neighborhood meeting spots as proactive vaccination delivery points. This approach effectively shifted the onus from individuals seeking vaccines to healthcare providers proactively bringing vaccines to the community and exemplifies a strategy that could be extended to routine vaccinations to improve access to and uptake of vaccines, thus ensuring broader immunization coverage. Furthermore, highly targeted campaigns focusing on vulnerable and hard to reach populations, such as the documented examples of fishermen in Lake Chilwa, Malawi, or factory workers in Bangladesh, optimize the use of limited supply and restrained resources. Targeted campaigns can enhance public health interventions by prioritizing areas with high transmission rates or vulnerable populations, thereby averting infections and reducing disease spread more efficiently than broader, generalized campaigns. However, limited examples of targeted vaccine delivery aimed at reaching high-risk individuals were found, which could potentially inform future TB or other novel vaccine implementations. This suggests a need for more research into such strategies. For instance, cocooning – vaccinating close contacts to shield vulnerable populations – has been effectively used with the Tdap vaccine to protect infants from pertussis and with the COVID-19 vaccine to protect adults at high risk for severe disease [Citation46,Citation47]. This strategy, though difficult to achieve in resource constrained settings, could be further researched to potentially benefit high-risk groups in future vaccination efforts, although it presents significant challenges in LMICs due to extensive resource needs and accessibility issues.
One notable challenge under the ‘accessibility’ theme was the difficulty in reaching working men – a group considered a key driver in the TB pandemic – through mass vaccination or door-to-door delivery models. This underscores the necessity for flexible and adaptable vaccination campaigns to cater to working men and other hard-to-reach sub-groups. Strategies like extending vaccination hours and orchestrating vaccination drives on non-working days, in addition to convenient vaccination locations, emerged as pragmatic approaches to improve uptake for this demographic. This strategy could be adapted for future vaccination programs, such as those targeting TB among men, who comprise most of TB cases and face similar challenges as the working men often missed by regular vaccination hours as noted in the literature.
This review also underscores the importance of utilizing existing health infrastructure and ensuring the preparedness of healthcare workers through pre-campaign training and education for a successful vaccine introduction. Insights from different vaccine introductions demonstrated that leveraging the established Expanded Program on Immunization (EPI) infrastructure, along with equipping healthcare workers with the necessary knowledge and skills, are pivotal strategies for improving accessibility. Additionally, while not extensively covered in the literature identified, expanding the use of electronic immunization registries should be considered to support the tailoring of access strategies. These registries allow for improved and real-time monitoring of campaign progress and help adapt implementation efforts according to care seeking and access patterns, enhancing the overall effectiveness of vaccination programs [Citation48]. Combined, these elements not only facilitate the vaccine introduction process but also contribute to tailoring the approach to meet the unique needs of different communities, thus emphasizing a context-driven approach to health campaigns.
4.3. Acceptability
Several key themes emerged concerning the acceptance of vaccines, each illuminating the complex interplay of factors that dictate community receptivity toward novel vaccine introductions. The degree of community awareness and understanding about the disease – its risk, transmission, consequences – and the vaccine – how it works and why it’s important – played a quintessential role in fostering acceptance. Where communities were well-informed, the uptake of vaccines was notably higher. The variance in community-level knowledge underscores the necessity for extensive sensitization campaigns to foster a conducive understanding and acceptance of new vaccines as a precursor to successful vaccine introduction and represents an important opportunity for leveraging partnerships with stakeholders.
The detrimental impact of rumors and misconceptions contributing to vaccine hesitancy was a recurring theme across various vaccine introductions. Real-time monitoring and countering of these rumors proved instrumental in mitigating vaccine hesitancy, showcasing the necessity for proactive measures in dispelling misinformation. The emergence of misconceptions for several different vaccines underscores the critical importance of clear and transparent communication strategies to alleviate unfounded fears and foster a climate of trust surrounding vaccine introductions. Additionally, to adequately address concerns and alleviate fears related to vaccine safety, real-time monitoring of safety surveillance will be crucial for future vaccination programs [Citation49]. This approach will help build confidence in a vaccine’s safety profile and enhance overall acceptance, while directly informing strategies to mitigate vaccine hesitancy.
The effectiveness of community engagement and sensitization activities in fostering vaccine acceptance was prominent across the reviewed introductions. The role of community leaders, especially religious leaders, in mobilizing community acceptance underscores the need for an inclusive, community-centric approach to vaccination campaigns. Furthermore, the utility of diverse communication channels, ranging from traditional media to community meetings, was accentuated in engendering a positive disposition toward the vaccines. Initiating the planning and sensitization processes early, even before a vaccine is made available, can immensely benefit future vaccination programs in establishing a trusting and transparent relationship with stakeholders, thereby ensuring rapid deployment and acceptance once the vaccine becomes available.
4.4. Limitations
This review has limitations. Our review was restricted to introductions within the last 10 years and excluded non-English articles for feasibility considerations. Notably, most of the introductions detailed in these selected papers were carried out prior to the advent of the COVID-19 pandemic. This global event has subsequently significantly impacted the immunization landscape, including various aspects of vaccine trust and hesitancy, healthcare system infrastructures, and health expenditure priorities. Additionally, due to an ongoing WHO-commissioned review of which the data has not yet been made available, we intentionally refrained from including COVID-19 vaccines, which might have led to the omission of pertinent lessons learned. The influenza vaccine was excluded from our review due to the rarity of national influenza vaccination policies and its limited inclusion in the EPI of LMICs, which are the primary focus of our study. Consequently, this analysis does not cover valuable insights that could be gained from the implementation of the influenza vaccine in upper-income settings. Considering the distinctive attributes and delivery modalities associated with oral vaccines, it is noteworthy that the predominance of papers focused on OCV, as included in our review, somewhat constrains our capacity to generalize the insights garnered from these experiences to the domain of injectable vaccines, notably a novel TB vaccine.
5. Conclusions
In conclusion, this review sheds light on the nuanced and multi-faceted elements that shape the introduction of new adult vaccines in LMICs, encompassing availability, accessibility, and acceptance. As we move closer to the reality of introducing a safe and effective novel adult TB vaccine, the insights gleaned from this review offer a practical roadmap. By embracing the lessons learned, stakeholders can better navigate the complex terrain of adult vaccine introduction, moving a step closer to the collective goal of ending the global TB pandemic by equitably reaching adults with a new vaccine [Citation50].
6. Expert Opinion
Attempting to design, implement, and evaluate vaccine introductions in a manner that is sensitive to the complicated confluence of factors outlined in this paper can help to avoid longer-term challenges that vaccines might face, such as national health policy de-prioritization, community resistance, and wasted resources (e.g. polio, COVID-19, etc.) [Citation51,Citation52]. The value of this paper is to establish the commonalities and differences between the introduction of different vaccines among adult populations across diverse resource-constrained settings and highlight barriers and facilitators of implementation. Some commonalities that we identified include the need for local information, which could inform policies; this information extends well beyond surveillance data and includes information about current socio-cultural and socio-political landscapes – contributing to our understanding of the landscape of powerbrokers and decision-makers. This holistic information was found to contribute to the implementation and introduction in some contexts. Importantly, conversations about prioritization should take into consideration this information in conjunction with local stakeholders as well as international stakeholders since potential new vaccines will be made available through a variety of factors at the global level. For example, the introduction of a successful TB vaccine candidate will necessarily involve discussions with enablers and drivers of the research and implementation (i.e. funders), and national level policy makers.
Research in this field should focus on refining our understanding of the existing vaccine delivery models and assessing the impact of different strategies on vaccine uptake. Our findings showed an extensive and diverse set of delivery models used in different contexts, which were responsive to their specific and unique needs. Diverse mechanisms were further used to reach high-risk populations that were otherwise challenging to reach. In some contexts, reaching working men during vaccine introduction was complicated and required strategies such as engaging with them during holidays, or days off. For populations with a high risk for TB, which predominantly includes men, innovative strategies will likely be required to ensure equitable access [Citation53]. However, much research in this space has attempted to gauge the implementational success as independent from the implementing bodies. While this research has value for producing some useful evidence (such as ex-post community receptiveness), it fails to provide a holistic assessment of efforts to introduce new vaccines. Implementational processes include push factors which are led by implementing bodies (e.g. communication and engagement strategies), and a variety of pull factors such as structural aspects of community readiness (e.g. existing interactions with vaccination programs or health systems) [Citation54]. Both implementational processes inform each other – making their collective study essential to fully understand the vaccine introduction landscape. Put differently, future research at different points in the introduction process (e.g. before, during, and after) when cohesively synthesized together, could provide substantial insights to our understanding of the entire cycle of an introduction.
The real-world performances of vaccines influence chosen delivery mechanisms. Integration of new adult vaccines into local Expanded Programs on Immunization (EPI) depends on the frequency and training burden of existing healthcare workers. Some vaccine introductions were successfully able to leverage existing delivery systems through appropriate and timely dialogue with national level stakeholders (e.g. ministries of health (MOH), public and private health system stakeholders). However, with newer vaccines in the development pipeline, the real-world efficacy is yet unknown and only has a hypothetical efficacy that are challenging to communicate with key stakeholders. Yet, from our research, we found that it remains critical that the benefits of upcoming vaccine candidate(s) (upon approval) are communicated to the appropriate stakeholders, to initiate conversations about prioritization of the vaccine – backed up by evidence generated through robust research. We found that such conversations build momentum and alignment at an early stage of the introduction process.
Transparent communication with target communities in the process of vaccine rollout, along with deep engagement with stakeholders (including national and local actors), was also found to be a requisite for success. Rumors and conspiracy theories exist at the nexus of informational voids, as well as perceived and lived systemic inequities that go unaddressed while new interventions (e.g. vaccines) are pursued. Early transparency, as well as continuous and meaningful engagement, become important tools to counter both. As highlighted in this review, informational voids can be addressed by national stakeholders and international partners, responding to the specific emergent configurations in the local settings where the vaccine may be likely to be resisted. Formative research in this space of vaccine introductions can explore idiosyncratic factors relevant to each setting, which might facilitate achieving local, national, and international goals. Vaccine communities, or communities that are the products of vaccination programs and initiatives chosen partially due to their potential risk or existing disease burden, may not understand the process(es) that led to their selection, opening spaces for uncertainty. Examining the creation of vaccine communities with the purpose of communicating that creation to relevant communities is essential for future research to build trust and confidence.
Finally, with one or more potential new candidate vaccines for TB on the horizon – after nearly a century (since the introduction of BCG) – understanding the successes and failures of past vaccine introductions gains renewed importance. Reducing the burden of TB within local and national health systems will have important implications for resource allocations. Many persons with TB remain without timely access to life-saving therapy, and even those who do may choose to forego further treatment under the weight of the substantial side effects, costs, and social stigmatization. The introduction and widespread uptake of a safe and effective TB vaccine in high burden settings could help avert these substantial challenges for millions. The lessons taken from the heterogenous vaccine introductions covered in this paper offer starting points for different country contexts.
Article highlights
Learnings from past adult vaccine implementation experiences in LMICs can inform future new vaccine programs, such as for novel adult TB vaccines currently in development.
Leveraging existing infrastructure to integrate new adult vaccines into the Expanded Program on Immunization (EPI) can offer several benefits.
Various innovative strategies such as extended vaccination hours and convenient community accessible delivery points can improve vaccine uptake among hard-to-reach groups like working men.
The role of community engagement, especially through leaders and diverse context specific communication channels, is crucial in building trust and acceptance of new vaccines.
Engaging a broad spectrum of stakeholders, including government bodies, international organizations, community leaders, and healthcare workers, along with meticulous resource planning, aids vaccine availability.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
ierv_a_2375329_sm3724.docx
Download MS Word (17.8 KB)Acknowledgments
The contents are the sole responsibility of (authors) and do not necessarily reflect the views of USAID, the United States Government, or consortium collaborators or members.
Additional information
Funding
References
- Centers for Disease Control and Prevention. Fast Facts on Global Immunization. CDC. 2023 [cited 2024 Jan 4]. Available from: https://www.cdc.gov/globalhealth/immunization/data/fast-facts.html
- World Health Organization. Essential Programme on Immunization. WHO. [cited 2023 Oct 13]. Available from: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization
- Guignard A, Praet N, Jusot V, et al. Introducing new vaccines in low- and middle-income countries: challenges and approaches. Expert Rev Vaccines. 2019;18(2):119–131. doi: 10.1080/14760584.2019.1574224
- World Health Organization. Table 1: Summary of WHO Position Papers - Recommendations for Routine Immunization. 2023 Mar [cited 2023 Oct 13]. Available from: https://cdn.who.int/media/docs/default-source/immunization/immunization_schedules/table_1_feb_2023_english.pdf?sfvrsn=c7de0e97_11&download=true
- Nanni A, Meredith S, Gati S, et al. Strengthening global vaccine access for adolescents and adults. Vaccine. 2017;35(49, Part B):6823–6827. doi: 10.1016/j.vaccine.2017.10.023
- Frick M. Pipeline Report: Tuberculosis Vaccines. Treatment Action Group. 2023. 2023 [cited 2024 Jan 10]. Available from: https://www.treatmentactiongroup.org/wp-content/uploads/2023/10/2023_pipeline_TB_vaccines_final.pdf
- Lydon P, Levine R, Makinen M, et al. Introducing new vaccines in the poorest countries: What did we learn from the GAVI experience with financial sustainability? Vaccine. 2008;26(51):6706–6716. doi: 10.1016/j.vaccine.2008.10.015
- Makinen M, Kaddar M, Molldrem V, et al. New vaccine adoption in lower-middle-income countries. Health Policy Plann. 2012;27(suppl_2):ii39–ii49. doi: 10.1093/heapol/czs036
- Burchett HED, Mounier-Jack S, Torres-Rueda S, et al. The impact of introducing new vaccines on the health system: case studies from six low- and middle-income countries. Vaccine. 2014;32(48):6505–6512. doi: 10.1016/j.vaccine.2014.09.031
- Lindstrand A, Cherian T, Chang-Blanc D, et al. The world of immunization: achievements, challenges, and strategic vision for the Next Decade. J Infect Dis. 2021;224(Supplement_4):S452–7. doi: 10.1093/infdis/jiab284
- Donadel M, Panero MS, Ametewee L, et al. National decision-making for the introduction of new vaccines: a systematic review, 2010–2020. Vaccine. 2021;39(14):1897–1909. doi: 10.1016/j.vaccine.2021.02.059
- World Health Organization. Principles and considerations for adding a vaccine to a national immunization program: from decision to implementation and monitoring. 2014. Available from: https://iris.who.int/bitstream/handle/10665/111548/9789241506892_eng.pdf?sequence=1
- The World Bank. World Bank Country and Lending Groups. World Bank data. 2023 [cited 2023 Oct 13]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- World Health Organization Immunization. Vaccines and Biologicals, Product & Delivery Research. WHO Global Framework to prepare for Country Introduction of New TB Vaccines for Adults and Adolescents. [cited 2023 Jul 25]. Available from: https://www.who.int/publications/m/item/who-global-framework-to-prepare-for-country-introduction-of-new-tb-vaccines-for-adults-and-adolescents
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. [2021 Mar 29]:n71. doi: 10.1136/bmj.n71
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850
- Ortiz, Perut M, Dumolard L, et al. A global review of national influenza immunization policies: analysis of the 2014 WHO/UNICEF Joint Reporting Form on immunization. Vaccine. 2016;34(45):5400–5405. doi: 10.1016/j.vaccine.2016.07.045
- Morales KF, Brown DW, Dumolard L, et al. Seasonal influenza vaccination policies in the 194 WHO Member States: the evolution of global influenza pandemic preparedness and the challenge of sustaining equitable vaccine access. Vaccine: X. 2021;8:100097. doi: 10.1016/j.jvacx.2021.100097
- Otieno NA, Malik FA, Nganga SW, et al. Decision-making process for introduction of maternal vaccines in Kenya, 2017–2018. Implementation Sci. 2021;16(1):39. doi: 10.1186/s13012-021-01101-7
- Abubakar A, Azman AS, Rumunu J, et al. The first use of the global oral cholera vaccine emergency stockpile: lessons from South Sudan. PLOS Med. 2015;12(11):e1001901. doi: 10.1371/journal.pmed.1001901
- Khan IA, Khan AI, Rahman A, et al. Organization and implementation of an oral cholera vaccination campaign in an endemic urban setting in Dhaka, Bangladesh. Glob Health Action. 2019;12(1):1574544. doi: 10.1080/16549716.2019.1574544
- Amani A, Ngo Bama S, Dia M, et al. Challenges, best practices, and lessons learned from oral cholera mass vaccination campaign in urban Cameroon during the COVID-19 era. Vaccine. 2022;40(47):6873–6879. doi: 10.1016/j.vaccine.2022.08.025
- Poncin M, Zulu G, Voute C, et al. Implementation research: reactive mass vaccination with single-dose oral cholera vaccine, Zambia. Bull World Health Organ. 2018;96(2):86–93. doi: 10.2471/BLT.16.189241
- Fleming JA, Munthali A, Ngwira B, et al. Maternal immunization in Malawi: a mixed methods study of community perceptions, programmatic considerations, and recommendations for future planning. Vaccine. 2019;37(32):4568–4575. doi: 10.1016/j.vaccine.2019.06.020
- Bwire G, Roskosky M, Ballard A, et al. Use of surveys to evaluate an integrated oral cholera vaccine campaign in response to a cholera outbreak in Hoima district, Uganda. BMJ Open. 2020;10(12):e038464. doi: 10.1136/bmjopen-2020-038464
- Poncin M, Marembo J, Chitando P, et al. Implementation of an outbreak response vaccination campaign with typhoid conjugate vaccine – Harare, Zimbabwe, 2019. Vaccine X. 2022;12:100201. doi: 10.1016/j.jvacx.2022.100201
- Lubogo M, Mohamed AM, Ali AH, et al. Oral cholera vaccination coverage in an acute emergency setting in Somalia, 2017. Vaccine. 2020;38:A141–A147. doi: 10.1016/j.vaccine.2020.01.015
- Kar SK, Pach A, Sah B, et al. Uptake during an oral cholera vaccine pilot demonstration program, Odisha, India. Hum Vaccin Immunother. 2014;10(10):2834–2842. doi: 10.4161/21645515.2014.971655
- Mounier-Jack S, Burchett HED, Griffiths UK, et al. Meningococcal vaccine introduction in Mali through mass campaigns and its impact on the health system. Glob Health Sci Pract. 2014;2(1):117–129. doi: 10.9745/GHSP-D-13-00130
- Ciglenecki I, Sakoba K, Luquero FJ, et al. Feasibility of Mass vaccination campaign with oral cholera vaccines in response to an Outbreak in Guinea. PLOS Med. 2013;10(9):e1001512. doi: 10.1371/journal.pmed.1001512
- Parker LA, Rumunu J, Jamet C, et al. Neighborhood-targeted and case-triggered use of a single dose of oral cholera vaccine in an urban setting: feasibility and vaccine coverage. Kosek M, ed. PloS Negl Trop Dis. 2017;11(6):e0005652. doi: 10.1371/journal.pntd.0005652
- Khan AI, Islam MS, Islam M, et al. Oral cholera vaccination strategy: self-administration of the second dose in urban Dhaka, Bangladesh. Vaccine. 2019;37(6):827–832. doi: 10.1016/j.vaccine.2018.12.048
- Heyerdahl LW, Ngwira B, Demolis R, et al. Innovative vaccine delivery strategies in response to a cholera outbreak in the challenging context of Lake Chilwa. A rapid qualitative assessment. Vaccine. 2018;36(44):6491–6496. doi: 10.1016/j.vaccine.2017.10.108
- Grandesso F, Rafael F, Chipeta S, et al. Oral cholera vaccination in hard-to-reach communities, Lake Chilwa, Malawi. Bull World Health Organ. 2018;96(12):817–825. doi: 10.2471/BLT.17.206417
- Sharp A, Blake A, Backx J, et al. High cholera vaccination coverage following emergency campaign in Haiti: results from a cluster survey in three rural Communes in the South Department, 2017. Wunder E, ed. PLOS Negl Trop Dis. 2020;14(1):e0007967. doi: 10.1371/journal.pntd.0007967
- Porta MI, Lenglet A, De Weerdt S, et al. Feasibility of a preventive mass vaccination campaign with two doses of oral cholera vaccine during a humanitarian emergency in South Sudan. Trans R Soc Trop Med. 2014;108(12):810–815. doi: 10.1093/trstmh/tru153
- Uddin M, Wahed T, Saha NC, et al. Coverage and acceptability of cholera vaccine among high-risk population of urban Dhaka, Bangladesh. Vaccine. 2014;32(43):5690–5695. doi: 10.1016/j.vaccine.2014.08.021
- Ngwa MC, Alemu W, Okudo I, et al. The reactive vaccination campaign against cholera emergency in camps for internally displaced persons, Borno, Nigeria, 2017: a two-stage cluster survey. BMJ Glob Health. 2020;5(6):e002431. doi: 10.1136/bmjgh-2020-002431
- Msyamboza KP, M’bang’ombe M, Hausi H, et al. Feasibility and acceptability of oral cholera vaccine mass vaccination campaign in response to an outbreak and floods in Malawi. Pan Afr Med J. 2016;23:23. doi: 10.11604/pamj.2016.23.203.8346
- Elias Chitio JJ, Baltazar CS, Langa JP, et al. Pre-emptive oral cholera vaccine (OCV) mass vaccination campaign in Cuamba District, Niassa Province, Mozambique: feasibility, vaccination coverage and delivery costs using CholTool. BMJ Open. 2022;12(9):e053585. doi: 10.1136/bmjopen-2021-053585
- Amani A, Fouda AAB, Nangmo AJ, et al. Reactive mass vaccination campaign against cholera in the COVID-19 context in Cameroon: challenges, best practices and lessons learned. Pan Afr Med J. 2021;38:38. doi: 10.11604/pamj.2021.38.392.27754
- Anikene C, Olowu A, Tagbo BN, et al. Health-care workers’ perspectives on ebola virus vaccine: a focus group and In-depth interview interventional study. Am J Trop Med Hyg. 2016;95(3):654–662. doi: 10.4269/ajtmh.16-0206
- Clinical and Translational Science Awards Consortium, U.S. National Institutes of Health (U.S.), Centers for Disease Control and Prevention (U.S.), and Clinical & Translational Science Awards Consortium. Principles of community engagement. 2011. Available from: http://heinonline.org/HOL/Page?handle=hein.usfed/pcomeng0001&id=1&collection=usfed&index=usfed
- Dutta T, Agley J, Meyerson BE, et al. Perceived enablers and barriers of community engagement for vaccination in India: using socioecological analysis. PLOS ONE. 2021;16(6):e0253318. doi: 10.1371/journal.pone.0253318
- World Health Organization. Human papillomavirus vaccines: WHO position paper, December 2022. Wkly Epidemiol Rec. 2022;97:645–672. Available from: https://iris.who.int/bitstream/handle/10665/365350/WER9750-eng-fre.pdf?sequence=1
- Urwyler P, Heininger U. Protecting newborns from pertussis – the challenge of complete cocooning. BMC Infect Dis. 2014;14(1):397. doi: 10.1186/1471-2334-14-397
- Wang X, Du Z, Huang G, et al. Effects of Cocooning on coronavirus disease rates after relaxing social distancing. Emerg Infect Dis. 2020;26(12):3066–3068. doi: 10.3201/eid2612.201930
- Secor AM, Mtenga H, Richard J, et al. Added value of electronic immunization registries in low- and middle-income countries: observational case study in Tanzania. JMIR Public Health Surveill. 2022;8(1):e32455. doi: 10.2196/32455
- Chandler RE, Balakrishnan MR, Brasseur D, et al. Collaboration within the global vaccine safety surveillance ecosystem during the COVID-19 pandemic: lessons learnt and key recommendations from the COVAX Vaccine Safety Working Group. BMJ Glob Health. 2024;9(3):e014544. doi: 10.1136/bmjgh-2023-014544
- World Health Organization. Implementing the End TB Strategy: the essentials 2022. Who. 2022 [cited 2024 Jan 8]. Available from: https://www.who.int/publications/i/item/9789240065093
- Yarlagadda H, Patel MA, Gupta V, et al. COVID-19 vaccine challenges in developing and developed countries. Cureus. 2022;14(4):e23951. doi: 10.7759/cureus.23951
- Deressa W, Kayembe P, Neel AH, et al. Lessons learned from the polio eradication initiative in the Democratic Republic of Congo and Ethiopia: analysis of implementation barriers and strategies. BMC Public Health. 2020), 1807;20(4). doi: 10.1186/s12889-020-09879-9
- Horton KC, MacPherson P, Houben RM, et al. Sex differences in tuberculosis burden and notifications in low- and middle-income countries: a systematic review and meta-analysis. PLOS Med. 2016;13(9):e1002119. doi: 10.1371/journal.pmed.1002119
- Green LW, Orleans CT, Ottoson JM, et al. Inferring strategies for disseminating physical activity policies, programs, and practices from the successes of tobacco control. Am J Preventive Med. 2006;31(4):66–81. doi: 10.1016/j.amepre.2006.06.023
