Introduction
Recent advances in technology have generated several new types of equipment which can be used within biomechanics to measure motion and inertial forces during human movement (Adesida et al., Citation2019; Aroganam et al., Citation2019; Dian et al., Citation2020; Kiely et al., Citation2019; Lutz et al., Citation2020; De Pasquale & Ruggeri, Citation2019; Ray et al., Citation2019). The more established and used technologies are measurement units based on inertia (Inertial Measurement Units [IMUs]), that are often used in association with magnetic field sensors (MIMUs) (Grand View Research, Citation2018). The domains of application of these technologies span several key areas of sports biomechanics, including performance enhancement (Camomilla et al., Citation2018; Macadam et al., Citation2019; Magalhaes et al., Citation2015), inertial force monitoring (Naughton et al., Citation2020; Paquette et al., Citation2020; Vanwanseele et al., Citation2020), and injury risk mitigation (Patton et al., Citation2020; Sheerin et al., Citation2019). The benefits of these new technologies often include a reduction in cost and improved portability in comparison to more established equipment, allowing for data collection outside of a lab setting which can improve ecological validity (Macadam et al., Citation2020). With increased availability there is increased potential for unsuitable use, therefore, extensive independent testing is required to establish the validity and reliability of these methods (Macadam et al., Citation2019; Naughton et al., Citation2020). This is needed to establish the required levels of accuracy and consistency to measure variables of interest within certain conditions prior to conducting experimental research, and to establish guidelines for obtaining information from sensors that could be reliably used to inform decisions (Camomilla et al., Citation2018). This editorial will address some of the novel technologies being increasingly utilised within sports biomechanics and highlight key factors to be considered in best practice.
Wearable sensor technology: spotlight on inertial and magneto-inertial measurement units
Inertial and magneto-inertial measurement units (also known as inertial sensors) are increasingly prevalent wearable sensor technologies in sports biomechanics. These wireless sensors typically contain tri-dimensional linear accelerometers and gyroscopes, with a working principle based on inertia, and tri-dimensional magnetometers (Fong & Chan, Citation2010). For simplicity, all sensors based on inertia from hereon will be referred to as IMUs, irrespective to the presence/absence of a magnetometer. IMUs are often used as either a standalone tool or within a movement analysis system including multiple IMUs. IMUs can provide linear and angular motion measures of individual segments (e.g. head, thorax, tibia), but state of the art estimates of the centre of mass trajectory are still not considered reliable for energy quantifications (Pavei et al., Citation2020). They can be mounted directly onto the skin, attached to the athlete via a strap/belt, or within tightfitting clothing. Various custom tools using IMUs are also available, which are often designed for a specific sport application, such as in distance running (e.g. mounted onto the lower back, the back of the shoe or in the laces) and in unhelmeted football codes (e.g. mouthguards, behind the ear patches). The variety of IMU technology, data collection protocols and proposed applications of these IMUs are vast, consistent with the abundant range of sports, movements, and skill variations. This affects the accuracy and reliability of the resulting measures.
Several factors are crucial to the accuracy and reliability of the measurements from IMUs. Validity relies on the proper selection of a sensor with appropriate technical specifications, the accuracy of the sensor calibration and the absence of external ferromagnetic disturbances (both to be eventually spot checked). Subsequent sensor placement, fixing and anatomical calibration are of vital importance when determining validity (Camomilla et al., Citation2018; Macadam et al., Citation2019).
The measurements that can be obtained with IMUs can be broadly categorised into: (1) physical activity classification and monitoring, (2) acceleration measurement to estimate dynamics quantities related to external (whole-body) and/or internal (segment) inertial forces (often also referred to as biomechanical loads), (3) acceleration measurement to measure dynamic stability, (4) point or body segment kinematic quantities to assess the technical aspects of the movement (e.g. angular velocity of the body about the centre of gravity or two body segments relative orientation), or (5) a combination of two or more of these categories. When it is crucial to represent and interpret mechanical quantities within the linguistic framework of functional anatomy, as it is the case for category 4, data measured in the sensor reference frame must be represented into an anatomical segment reference frame, through an anatomical calibration procedure (Cereatti et al., Citation2017; Cutti et al., Citation2010; Picerno, Citation2017; Picerno et al., Citation2008). Several anatomical calibration methods have been used in the past; the most direct (but rarely adequately accurate) method is to manually align the IMU case with qualitatively identified anatomical planes and axes of the underlying bony segment, thus aligning sensor and anatomical frames. An alternative solution for anatomical axes identification is based on static and/or functional (dynamic) calibrations which benefit from a similar popularity to manual alignment (Vitali & Perkins, Citation2020) and continuous development (Bessone et al., Citation2019; Yoon et al., Citation2019; Li et al., Citation2020). During functional calibration, functional movements are executed and used to calculate the orientation of anatomically relevant axes with respect to the sensor frame. For example, some commercially available systems use walking gait as a functional movement.
Regardless of the mechanical quantities of interest, there is presently no set of standard protocols that provides adequate accuracy and reliability for the complexity of movements and variety of sensor placement, biomechanical models, and anatomical calibration procedures for specific measurement outputs (Poitras et al., Citation2019). Finally, invalid data can also arise during data processing due to inappropriate selection of cut-off frequencies, and/or from not using ad hoc algorithms to compensate for drift errors or ferromagnetic disturbances (Ligorio & Sabatini, Citation2016; Mendes Jr. et al., Citation2016).
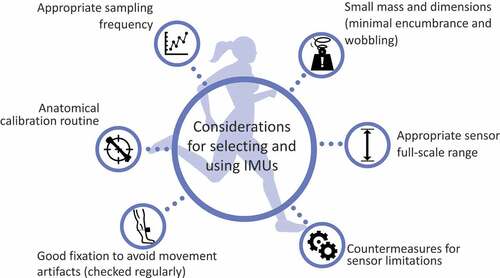
Consensus on the minimal requirements for accurate and reliable outcomes is needed to strengthen the quality of the research that uses IMUs in exercise and sport science. Given the central technical importance of kinetic and kinematic measurement in biomechanics; our discipline is well qualified to guide the initiative to establish standards for their use, given the discipline’s experience in publishing standards in three-dimensional motion analysis and electromyography (e.g. Bishop et al., Citation2012; Camomilla et al., Citation2017; Chin et al., Citation2010; Jackson et al., Citation2012; Kontaxis et al., Citation2009; De Luca, Citation1997; Wu & Cavanagh, Citation1995; Wu et al., Citation2002; Citation2005). In the absence of such standards, Sports Biomechanics recommends that a comprehensive evaluative review is undertaken as a matter of urgency to determine minimum specifications of wearable technologies, and to provide guidelines on accurate and reliable standard measurement protocols. Until this important step can be achieved, some general guidelines are now provided for IMU-based studies, including a checklist of considerations on selecting and using IMUs (), and a table providing points to consider to recognise and minimise potential error sources
().Table 1. Sensors limits, sport assessments more prone to negative effects and error sources to consider.
Checklist
IMU sensor mass and dimensions are small enough to minimise its influence (encumbrance) on the movement, especially when used with children and youth populations, or to limit the sensor wobbling when used to assess kinematics of fast dynamic movements.
Sampling frequency is appropriate for the measured movement and outcome parameters, being at least two times the highest frequency in the signal of interest (according to the Nyquist–Shannon sampling theorem [Hamill et al., Citation1997]).
Sensor capacity (e.g. linear acceleration full-scale range) is appropriate to capture the true biomechanics of the movement, especially for the distal segments during high impact events. It is important to check the quality of the recorded data (e.g. no clipping/capping of the signal).
Fixation on the skin should be as rigid as possible to avoid introducing movement artefacts in the measures from the sensor itself. For that reason, fixing sensors onto clothing, even tight-fitting clothing, or within non-rigid pockets is not recommended. Placing sensors over soft tissue (fat or muscle) should also be avoided, as should encumbering movement through placement too close to a joint. Sensor placement fixation should be checked regularly during athlete testing, as they may loosen over time when used in high impact activities and when exposed to athlete sweat.
Sensor placement for inertial force measures should be based on scaled instead of absolute positions to account for the individual’s anthropometry (e.g. intersection of the middle and distal thirds of the antero-medial aspect of the tibia instead of 8 cm above the transverse plane defined by the centres of medial and lateral malleolus).
An anatomical calibration routine should be implemented to ensure test-retest and inter-athlete reliability. The orientation of the sensor reference frame axes is determined with respect to the anatomical axes of the segment. If manual alignment to anatomical features is selected (e.g. for inertial force measures), sensor placement must follow a set protocol. For any measures that seek to obtain descriptive kinematics of technique (e.g. knee joint angular kinematics), a more reliable approach should be selected which may include static (e.g. anatomical position, T pose) and functional (e.g. unweighted squats, walking) tasks.
Data processing includes countermeasures for sensors limitations, using proper sensor fusion (Ligorio & Sabatini, Citation2016; Mendes Jr. et al., Citation2016), or implementing algorithms that embed a priori knowledge (Camomilla et al., Citation2018).
Smartphone sensors and application (App) software
Modern smartphones possess internal sensors which allow for measurement of the phone’s movement using tri-axial accelerometers and gyroscopes. The notion of using these sensors to monitor human movement during sports has been proposed for a while, but until more recently may not have been fully exploited (Hummel et al., Citation2013; McNab et al., Citation2011; Mitchell et al., Citation2013). Software developers have started creating innovative applications (apps) which allow Biomechanists to use the phone as a wearable technology device to measure motion and estimate forces. Examples of validated apps which use the phone’s gyroscopes as an inclinometer include Dorsiflex, which has been validated to measure ankle dorsiflexion range of motion (Balsalobre-Fernández et al., Citation2019), and TiltMeter©, which has been validated to measure lumbar spine sagittal plane range of motion (Pourahmadi et al., Citation2016). A more detailed critique of validated smartphone apps to measure joint range of motion can be found in a systematic review by Keogh et al. (Citation2019), in which they support the use of smartphone apps to replace goniometers, but recommend the development of more reliable and valid protocols for their use. These apps, however, only measure static range of motion (range of joint motion when held stationary at the limits of its movement) which restricts their possible application for sports activities. While apps do exist for dynamically tracking inclination or direct measures of acceleration and angular velocity (e.g. Phyphox) or estimating force using the phones accelerometer (e.g. ForceData), there is limited validation of these applications to support their accuracy at present. In addition, the specifications of the smartphone’s internal sensors can vary considerably between devices which has been shown to influence the accuracy of some applications when used on different devices (Chen et al., Citation2018). Therefore, these specifications should be checked prior to using an app with a particular smartphone. With continuous rapid advances in mobile phone technology, this type of equipment is likely to become more accessible, accurate and more widely used, since these apps offer opportunities to measure variables that would have previously been beyond the scope of the equipment available to many practitioners. However, they should not be viewed as a replacement for established equipment. Practitioners should be aware of their limitations, so that they can take the steps required to minimise sources of error, as well as having the expertise required to correctly interpret the data generated before using these tools for diagnostic assessments.
From measuring to providing actionable insights
A full awareness of sensor potential and limitations is at the foundation of bridging the disconnect between the capability of these systems to measure movement and providing actionable insights to coaches and athletes. The challenges and trends are to provide more intelligent, real-time, accurate information, making it user friendly (Whelan et al., Citation2016). Aside for adhering to minimum requirements for sensor use, our community should move towards obtaining usable information from sensors to reliably inform decisions through a human or automatic decision-making process. Supporting this process requires being in the position to answer the following questions (adapted from Spiegelhalter, Citation2020):
Does the proposed measure provide practical value when obtained and used in the real world?
Is the system as complex/simple as required for it to be used as a decision-making tool?
Could you, as user, explain how it works (in general) to anyone who is interested?
Are you sure the system is valid and reliable and are you aware of its uncertainty?
Do you use it appropriately, with the right level of scepticism?
Summary
Novel technology is often commercialised for direct sport applications. Researchers and practitioners need to understand the specific technology limits, best protocols for its intended use, as well as the accuracy, reliability, and specificity of the chosen measures before implementing the technologies in practice. In this editorial, two prevalent technologies with biomechanical applications have been discussed due to their relevance to sport biomechanics: the inertial measurement unit(s) and the smartphone sensors/app software. Emerging technological developments that are applicable to movement analysis offer exciting opportunities for biomechanics to bridge the gap between research and practice and allow Biomechanists to increasingly move away from the laboratory and to the field where athletes train and compete. The technologies could therefore provide opportunities to increase the ecological validity of the measurement obtained in sports biomechanics practice (research, applied). This changing operational environment could also assist biomechanics to have greater presence and perceived relevance to sport provided that the measures and interpretations can be trusted. The International Society of Biomechanics in Sport (ISBS) and this Journal are well positioned to guide and advise this evolution, to give the discipline and its members the best chance of success. This can be achieved through establishing standards for best practice, guided by a comprehensive review of what has already been learnt from the foundational research using these emerging technologies. Sports Biomechanics, therefore, encourages the International Society of Biomechanics in Sport (ISBS) to carry out research and provide a more comprehensive position statement on the use these technologies.
References
- Adesida, Y., Papi, E., & McGregor, A. H. (2019). Exploring the role of wearable technology in sport kinematics and kinetics: A systematic review. Sensors, 19(7), 1597. https://doi.org/10.3390/s19071597
- Aroganam, G., Manivannan, N., & Harrison, D. (2019). Review on wearable technology sensors used in consumer sport applications. Sensors, 19(9), 1983. https://doi.org/10.3390/s19091983
- Balsalobre-Fernández, C., Romero-Franco, N., & Jiménez-Reyes, P. (2019). Concurrent validity and reliability of an iPhone app for the measurement of ankle dorsiflexion and inter-limb asymmetries. Journal of Sports Sciences, 37(3), 249–253. https://doi.org/10.1080/02640414.2018.1494908
- Bessone, V., Höschele, N., Schwirtz, A., & Seiberl, W. (2019). Validation of a new inertial measurement unit system based on different dynamic movements for future in-field applications. Sports Biomechanics, https://doi.org/10.1080/14763141.2019.1671486
- Bishop, C., Paul, G., & Thewlis, D. (2012). Recommendations for the reporting of foot and ankle models. Journal of Biomechanics, 45(13), 2185–2194. https://doi.org/10.1016/j.jbiomech.2012.06.019
- Camomilla, V., Cereatti, A., Cutti, A. G., Fantozzi, S., Stagni, R., & Vannozzi, G. (2017). Methodological factors affecting joint moments estimation in clinical gait analysis: A systematic review. Biomedical Engineering Online, 16(1), 106. https://doi.org/10.1186/2Fs12938-017-0396-x
- Camomilla, V., Bergamini, E., Fantozzi, S., & Vannozzi, G. (2018). Trends supporting the in-field use of wearable inertial sensors for sport performance evaluation: A systematic review. Sensors, 18(3), 873. https://doi.org/10.3390/s18030873
- Cereatti, A., Della Croce, U., & Sabatini, A. M. (2017). Three-dimensional human kinematic estimation using magneto-inertial measurement units. In B. Müller, et al. (Ed.), Handbook of human motion, 1-24. Springer. https://doi.org/10.1007/978-3-319-30808-1_162-1
- Chen, K. H., Hsu, Y. W., Yang, J. J., & Jaw, F. S. (2018). Evaluating the specifications of built-in accelerometers in smartphones on fall detection performance. Instrumentation Science & Technology, 46(2), 194–206. https://doi.org/10.1080/10739149.2017.1363054
- Chin, A., Lloyd, D., Alderson, J., Elliott, B., & Mills, P. (2010). A marker-based mean finite helical axis model to determine elbow rotation axes and kinematics in vivo. Journal of Applied Biomechanics, 26(3), 305–315. https://doi.org/10.1123/jab.26.3.305
- Cutti, A. G., Ferrari, A., Garofalo, P., Raggi, M., Cappello, A., & Ferrari, A. (2010). Outwalk: A protocol for clinical gait analysis based on inertial and magnetic sensors. Medical & Biological Engineering & Computing, 48(1), 17–25. https://doi.org/10.1007/s11517-009-0545-x
- De Luca, C. (1997). The use of surface electromyography in biomechanics. Journal of Applied Biomechanics, 13(2), 135–163. https://doi.org/10.1123/jab.13.2.135
- De Pasquale, G., & Ruggeri, V. (2019). Sensing strategies in wearable bio-mechanical systems for medicine and sport: A review. Journal of Micromechanics and Microengineering, 29(10), 103001. https://doi.org/10.1088/1361-6439/ab2f24
- Dian, F. J., Vahidnia, R., & Rahmati, A. (2020). Wearables and the Internet of Things (IoT), applications, opportunities, and challenges: A survey. IEEE Access, 8, 69200–69211. https://doi.org/10.1109/ACCESS.2020.2986329
- Fong, D. T. P., & Chan, Y. Y. (2010). The use of wearable inertial motion sensors in human lower limb biomechanics studies – A systematic review. Sensors, 10(12), 11556–11565. https://doi.org/10.3390/s101211556
- Grand View Research. (2018). Wearable sensors market size, share & trends report wearable sensors market size, share & trends analysis report by sensor type, by device (Smart Watch, Fitness Band, Smart Glasses, Smart Fabric), by vertical, by region, and segment forecast, 2018-2025. Market research report, Grand View Research, Inc., San Francisco, CA. Retrieved December 4, 2020, from https://www.grandviewresearch.com/industry-analysis/global-wearable-sensor-market
- Hamill, J., Caldwell, G. E., & Derrick, T. R. (1997). Reconstructing digital signals using Shannon’s sampling theorem. Journal of Applied Biomechanics, 13(2), 226–238. https://doi.org/10.1123/jab.13.2.226
- Hummel, O., Fehr, U., & Ferger, K. (2013). Beyond ibeer-exploring the potential of smartphone sensors for performance diagnostics in sports. International Journal of Computer Science in Sport, 12, 46–60. https://iacss.org/fileadmin/user_upload/IJCSS_FullPaper/Vol12_2013_Ed1/IJCSS-Volume12_2013_Edition1_Hummel.pdf
- Jackson, M., Michaud, B., Tétreault, P., & Begona, M. (2012). Improvements in measuring shoulder joint kinematics. Journal of Biomechanics, 45(12), 2180–2183. https://doi.org/10.1016/j.jbiomech.2012.05.042
- Keogh, J. W., Cox, A., Anderson, S., Liew, B., Olsen, A., Schram, B., & Furness, J. (2019). Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: A systematic review. PloS One, 14(5), e0215806. https://doi.org/10.1371/journal.pone.0215806
- Kiely, M., Warrington, G., McGoldrick, A., & Cullen, S. (2019). Physiological and performance monitoring in competitive sporting environments: A review for elite individual sports. Strength and Conditioning Journal, 41(6), 62–74. https://doi.org/10.1519/SSC.0000000000000493
- Kontaxis, A., Cutti, A. G., Johnson, G. R., & Veeger, H. E. J. (2009). A framework for the definition of standardized protocols for measuring upper-extremity kinematics. Clinical Biomechanics, 24(3), 246–253. https://doi.org/10.1016/j.clinbiomech.2008.12.009
- Li, Y., Koldenhoven, R. M., Jiwan, N. C., Zhan, J., & Liu, T. (2020). Trunk and shoulder kinematics of rowing displayed by Olympic athletes. Sports Biomechanics, https://doi.org/10.1080/14763141.2020.1781238
- Ligorio, G., & Sabatini, A. M. (2016). Dealing with magnetic disturbances in human motion capture: A survey of techniques. Micromachines, 7(3), 43. https://doi.org/10.3390/mi7030043
- Lutz, J., Memmert, D., Raabe, D., Dornberger, R., & Donath, L. (2020). Wearables for integrative performance and tactic analyses: Opportunities, challenges, and future directions. International Journal of Environmental Research and Public Health, 17(1), 59. https://doi.org/10.3390/ijerph17010059
- Macadam, P., Cronin, J., Neville, J., & Diewald, S. (2019). Quantification of the validity and reliability of sprint performance metrics computed using inertial sensors: A systematic review. Gait & Posture, 73, 26–38. https://doi.org/10.1016/j.gaitpost.2019.07.123
- Macadam, P., Cronin, J. B., Uthoff, A. M., Nagahara, R., Zois, J., Diewald, S., Tinwala, F., & Neville, J. (2020). Thigh loaded wearable resistance increases sagittal plane rotational work of the thigh resulting in slower 50-m sprint times. Sports Biomechanics, 1–12. https://doi.org/10.1080/14763141.2020.1762720
- Magalhaes, F. A. D., Vannozzi, G., Gatta, G., & Fantozzi, S. (2015). Wearable inertial sensors in swimming motion analysis: A systematic review. Journal of Sports Sciences, 33(7), 732–745. https://doi.org/10.1080/02640414.2014.962574
- McNab, T., James, D. A., & Rowlands, D. (2011). iPhone sensor platforms: Applications to sports monitoring. Procedia Engineering, 13, 507–512. https://doi.org/10.1016/j.proeng.2011.05.122
- Mendes Jr., J. J. A., Vieira, M. E. M., Pires, M. B., & Stevan Jr., S. L. (2016). Sensor fusion and smart sensor in sports and biomedical applications. Sensors, 16(10), 1569. https://doi.org/10.3390/s16101569
- Mitchell, E., Monaghan, D., & O’Connor, N. E. (2013). Classification of sporting activities using smartphone accelerometers. Sensors, 13(4), 5317–5337. https://doi.org/10.3390/2Fs130405317
- Naughton, M., Jones, B., Hendricks, S., King, D., Murphy, A., & Cummins, C. (2020). Quantifying the collision dose in rugby league: A systematic review, meta-analysis, and critical analysis. Sports Medicine-Open, 6(1), 6. https://doi.org/10.1186/s40798-019-0233-9
- Paquette, M. R., Napier, C., Willy, R. W., & Stellingwerff, T. (2020). Moving beyond weekly “distance”: Optimizing quantification of training load in runners. Journal of Orthopaedic & Sports Physical Therapy, 50(10), 564–569. https://doi.org/10.2519/jospt.2020.9533
- Patton, D. A., Huber, C. M., Jain, D., Myers, R. K., McDonald, C. C., Margulies, S. S., & Arbogast, K. B. (2020). Head impact sensor studies in sports: A systematic review of exposure confirmation methods. Annals of Biomedical Engineering, 48(1), 1–11. https://doi.org/10.1007/s10439-020-02642-6
- Pavei, G., Salis, F., Cereatti, A., & Bergamini, E. (2020). Body center of mass trajectory and mechanical energy using inertial sensors: A feasible stride? Gait & Posture, 80, 199–205. https://doi.org/10.1016/j.gaitpost.2020.04.012
- Picerno, P., Cereatti, A., & Cappozzo, A. (2008). Joint kinematics estimate using wearable inertial and magnetic sensing modules. Gait & Posture, 28(4), 588–595. https://doi.org/10.1016/j.gaitpost.2008.04.003
- Picerno, P. (2017). 25 years of lower limb joint kinematics by using inertial and magnetic sensors: A review of methodological approaches. Gait & Posture, 51, 239–246. https://doi.org/10.1016/j.gaitpost.2016.11.008
- Poitras, I., Dupuis, F., Bielmann, M., Campeau-Lecours, A., Mercier, C., Bouyer, L., & Roy, J.-S. (2019). Validity and reliability of wearable sensors for joint angle estimation: A systematic review. Sensors, 19(7), 1555. MDPI AG. https://doi.org/10.3390/s19071555
- Pourahmadi, M. R., Taghipour, M., Jannati, E., Mohseni-Bandpei, M. A., Takamjani, I. E., & Rajabzadeh, F. (2016). Reliability and validity of an iPhone® application for the measurement of lumbar spine flexion and extension range of motion. PeerJ, 4, e2355. https://doi.org/10.7717/peerj.2355
- Ray, T., Choi, J., Reeder, J., Lee, S. P., Aranyosi, A. J., Ghaffari, R., & Rogers, J. A. (2019). Soft, skin-interfaced wearable systems for sports science and analytics. Current Opinion in Biomedical Engineering, 9, 47–56. https://doi.org/10.1016/j.cobme.2019.01.003
- Sheerin, K. R., Reid, D., & Besier, T. F. (2019). The measurement of tibial acceleration in runners—A review of the factors that can affect tibial acceleration during running and evidence-based guidelines for its use. Gait & Posture, 67, 12–24. https://doi.org/10.1016/j.gaitpost.2018.09.017
- Spiegelhalter, D. (2020). Should we trust algorithms? Harvard Data Science Review, 2(1). https://doi.org/10.1162/99608f92.cb91a35a
- Vanwanseele, B., Op De Beéck, T., Schütte, K., & Davis, J. (2020). Accelerometer based data can provide a better estimate of cumulative loading during running compared to GPS based parameters. Frontiers in Sports and Active Living, 2, 154. https://doi.org/10.3389/fspor.2020.575596
- Vitali, R. V., & Perkins, N. C. (2020). Determining anatomical frames via inertial motion capture: A survey of methods. Journal of Biomechanics, 106, 109832. https://doi.org/10.1016/j.jbiomech.2020.109832
- Whelan, D., O’Reilly, M., Huang, B., Giggins, O., Kechadi, T., & Caulfield, B. (2016). Leveraging IMU data for accurate exercise performance classification and musculoskeletal injury risk screening. In 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, Florida, USA (pp. 659–662). IEEE. https://doi.org/10.1109/EMBC.2016.7590788
- Wu, G., & Cavanagh, P. R. (1995). ISB recommendations for standardization in the reporting of kinematic data. Journal of Biomechanics, 28(10), 1257–1261. https://doi.org/10.1016/0021-9290(95)00017-c
- Wu, G., Siegler, S., Allard, P., Kirtley, C., Leardini, A., Rosenbaum, D., Whittle, M., D’Lima, D. D., Cristofolini, L., Witte, H., Schmid, O., & Stokes, I. (2002). ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion - Part I: Ankle, hip, and spine. Journal of Biomechanics, 35(4), 543–548. https://doi.org/10.1016/s0021-9290(01)00222-6
- Wu, G., van der Helmb, F., Veegerc, H. E. J., Makhsouse, M., Van Royf, P., Angling, C., Nagelsh, J., Kardunai, A. R., McQuadej, K., Wangk, X., Wernerl, F. W., & Buchholz, B. (2005). ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion - Part II: Shoulder, elbow, wrist and hand. Journal of Biomechanics, 38(5), 981–992. https://doi.org/10.1016/j.jbiomech.2004.05.042
- Yoon, T.-L., Kin, H.-N., & Min, J.-H. (2019). Validity and reliability of an inertial measurement unit–based 3-dimensional angular measurement of cervical range of motion. Journal of Manipulative and Physiological Therapeutics, 42(1), P75–P81. https://doi.org/10.1016/j.jmpt.2018.06.001