ABSTRACT
Conventional treatments for excessive hair are tedious and time consuming. Laser hair removal has become the leading therapy option for long–term results. It works on the principle of selective photothermolysis, whereby photons destroy the hair follicle while sparing the surrounding tissue. As demand increases, there has been an increase in the regulation of these treatments. Laser hair removal is not risk-free and side effects are associated with the treatment. Adequate training is vital to minimise adverse side effects. Certain countries have regulatory boards that laser operators need to register with, as well as the completion of mandatory hours. Others require laser operators to register with a Care Quality Commission (CQC) to ensure that minimum training and safety standards are met. Currently, in South Africa, the lack of regulatory boards and mandatory hours poses a risk to the public as anyone with little or no qualification is allowed to perform laser hair removal treatments, placing patients at risk. This review looks at some of the devices used and basic mechanisms of action of laser hair removal, its associated risks, side effects and current regulation.
Introduction
Unwanted hair is a common complaint that often requires continuous treatment. In many cases, an underlying medical condition is not the cause of unwanted hair, and there is an increased preference for a “neat image” (Citation1). The presence of unwanted hair may cause significant psychological and emotional stress, and may have an adverse impact on their quality of life, resulting in patients resorting to feeling uncomfortable and experiencing low self-esteem (Citation2). Feelings of self-consciousness often arise from what is perceived as the “ideal hair pattern” within our culture and society.
For many years’ temporary hair removal treatment options such as waxing, threading, tweezing and depilatory creams have been utilised, and are still being used. Although these methods are relatively inexpensive, convenient and easily accessible, the results are short-lived, and require regular repetitive treatments. Permanent hair removal can be attained through electrolysis and light based treatments. The use of electricity to damage the hair follicle can be painful and time consuming, and frequently leads to pigmentary disorders and scarring with poor application (Citation2). Light-based hair removal technologies are grounded on either high-intensity, coherent, monochromatic, narrow-waveband lasers, or high-intensity, incoherent and polychromatic pulsed light (intense pulsed light, IPL). Along with significant advances in technology, laser hair removal, otherwise known as photo-epilation, has become a popular choice for the permanent reduction and removal of unwanted hairs. The concept of selectively targeting chromophores, known as selective photothermolysis, is an important concept in efforts to eradicate unwanted hairs, and relies on selectively targeting and destroying hair follicles through exposure to pulses of light, while causing minimal damage to surrounding tissue.
The breakthrough in selective photothermolysis and the application of this concept for efficient and lasting hair removal has provided the cosmetic industry and medical practitioners with several highly effective laser and IPL devices (Citation3). According to the American Society for Aesthetic Plastic Surgery, laser hair removal was in the top three non-surgical procedures performed in 2016, coming below botulinum toxin treatments and hyaluronic acid treatments, and accounted for 1,035,783 procedures (Citation4). Ideal candidates for light-based treatments mostly still consists of light-skinned patients with dark, thick hair (Citation5). A variety of lasers and pulsed light sources are available for the purpose of hair removal, with efficacy and safety differing from wavelength to wavelength, and include neodymium-doped yttrium aluminium garnet (Nd:YAG) lasers (1064 nm), ruby lasers (694 nm), alexandrite lasers (755 nm), diode lasers (810 nm), and although technically not a laser, a variety of IPL devices. The untrained use of these high-powered devices is coupled with unfavourable side effects and can cause severe complications. Therefore, sufficient regulations are necessary. This review article looks at the mechanism of action behind laser hair removal, as well as some of the devices used, associated hazards and regulations.
Mechanism of action of laser hair removal
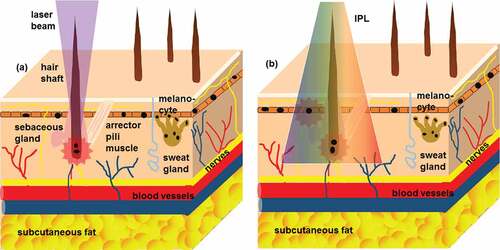
Any light-based therapy relies on the absorption of the photons by specific chromophores (targets). In the skin, these chromophores can include tattoo ink, haemoglobin, melanin, water and collagen. In the case of laser hair removal, the chromophore is melanin located within the hair bulb and hair shaft. During laser hair removal, a high-intensity pulsed laser beam (or broad-spectrum light source in the case of IPL) is directed at the target. The emitted light is primarily absorbed by melanin in the hair, and converts the light energy into an intense heat energy that diffuses into and destroys the hair follicle. While stem cells located in the hair bulge do not contain melanin, they are also targeted and destroyed by thermal damage through the diffusion of the heat energy from the hair follicle () (Citation6). This damage to the stem cells prevents future hair regrowth (Citation7). In patients with dark skin, melanin located in the epidermis interferes with this mechanism of action. Epidermal melanin competes with melanin within the hair follicle, and the epidermis absorbs the photons. Thus, these patients experience poorer clinical outcomes and a higher rate of thermally induced adverse effects (Citation7).
Epidermal melanin affects the optical properties of human skin. According to Karsten and Singh the absorption coefficient of the epidermis varies with the volume fraction of melanosomes and epidermal eumelanin concentration (Citation8). Wavelengths between 700 and 1000 nm are selectively absorbed by melanin, whereas competing chromophores such as oxyhemoglobin and water absorb less energy at these wavelengths (Citation9). Because of the high absorption of light by melanin, ruby and alexandrite lasers are not recommended for darker skin types as this could result in injury to the skin (Citation8). Recent technological advances now allow for a more inclusive customisation of settings that has paved the way for the safe reduction in hair regrowth in darker skinned patients (Citation7).
Laser hair removal relies on three paramount parameters: the proper selection of wavelength in the recommended visible to near-infrared (NIR) region up to about 1100–1200 nm; pulse duration (in milliseconds, ms); and the energy density or fluence (in joules per square centimetre, J/cm2) administered, which is related to total exposure time (Citation10). Thermal injury can be restricted to the target chromophore through the selection of the correct parameters. One other important concept is the thermal relaxation time (TRT). TRT is defined as the time required by an object to cool down to 50% of the initial temperature achieved (Citation11). For targeted tissue damage to occur, photons at the correct wavelength need to be absorbed by the chromophore and not the adjacent tissue. In order to achieve this, the pulse duration should be less than the TRT of the target. If the pulse duration exceeds the TRT, not only will the target be damaged, but the heat energy will also dissipate to the adjacent tissue resulting in injury to the surrounding area. Additionally, the stage of hair growth also plays an important factor. The ideal stage in the hair growth cycle is the active anagen phase, as there is an abundance of melanin and the follicles are located deep within the skin and are still attached to the papilla for nourishment. It is estimated that a 20% reduction may be observed with each treatment if hair growth is in the anagen phase and if the correct laser/light parameters are used.
Hair removal devices
Light sources that destroy hair photothermally includes the ruby laser (694 nm), alexandrite laser (755 nm), diode lasers (800 or 810 nm), Nd:YAG laser (1064 nm), and IPL devices ().
Table 1. Distinguishing types of light based treatments and recommended Fitzpatrick skin types.
Ruby laser
Due to the high melanin absorption at 694 nm, ruby lasers are best suited for individuals with light skin types, Fitzpatrick I to III, and dark hair. Because of this limitation and its high power consumption, ruby lasers have become less popular over the years. A study conducted by Campos et al. (Citation15) showed a reduction of hair growth in 63% of 51 patients; however, pigmentary changes occurred most frequently in patients with Fitzpatrick skin type IV.
Alexandrite laser
The alexandrite laser is a solid state laser that emits at 755 nm. This wavelength allows for a greater depth of penetration, but with less melanin absorption as opposed to the ruby laser. To minimise the risk of complications in darker skin types, longer wavelengths and pulse durations combined with effective skin cooling devices should be considered. The use of cooling devices can allow the laser operator to deliver effective energy to the dermal target whilst protecting the epidermis from thermal injury. A study conducted by Moon et al. (Citation16), compared the reduction of hair growth using an alexandrite laser versus an IPL device. The results showed a 96% reduction in hair growth following treatments with the alexandrite laser as opposed to IPL at 86%.
Diode lasers
Over the last few years, diode lasers have become the gold standard for laser hair removal globally (Citation5). To surmount the limitations of darker skin types, 810 nm diode lasers have been propositioned as a solution. Positive results have been shown through the use of a low fluence, which decreases side effects whilst maintaining efficacy, coupled with a high repetition rate, which ensures applicable amounts of accumulative energy in the hair bulb and bulge (Citation17). A six-month follow-up multi-center prospective study was conducted on 368 patients (Fitzpatrick skin types III to V) using an 810 nm diode laser (Citation17). Patients received five treatments to the face and various other body areas. Results revealed a high degree of patient approval and satisfaction, high efficiency in hair removal and elimination, and a low index of adverse events. In order to attain the required deposition of high-energy to the target, whilst avoiding the risk of burning, the movement of the hand-piece had to be adjusted to a constant speed (in-motion technique) (Citation17). In another study conducted by Agarwal and colleagues, 71 patients with Fitzpatrick skin types IV to VI were treated for hair removal with an 810 nm diode laser on various body parts, making use of the in-motion technique (Citation5). Patients received 5 to 6 treatments at 1 to 3 month intervals. A high degree of patient approval and satisfaction was obtained, with 58 (82%) patients rating the treatment as excellent, five as good (7%), five as average (7%), and three as poor (4%). Discomfort experienced during treatments was minor, with 69 (95.8%) patients experiencing very low to no discomfort, two (1.44%) patients experienced average discomfort, and one (0.72%) patient experienced high discomfort (upper lip region). Treatments were complication-free, and there was no reporting of any adverse effects during or after treatments (Citation5).
Nd:YAG laser
Nd:YAG lasers emit at a wavelength of 1064 nm. Together with diode lasers at 810 nm, Nd:YAG lasers are highly recommended for darker skin types as the penetration of the laser beam is much deeper as opposed to ruby and alexandrite lasers, therefore lowering the risk of epidermal interference. However, increased fluence is required to damage the follicular growth centres, as these wavelengths are not readily absorbed by melanin. Effective cooling of the epidermis is also essential, as higher energy is required. In the United Kingdom, a comparison of the overall incidence of side effects in Fitzpatrick skin types IV to VI (in 109 patients) treated with a ruby laser (29.9%) or the long-pulsed Nd:YAG laser (9.4%) was made. This study recommended that the ruby laser should not be used for dark skin types, and alternatives such as the Nd:YAG laser should be used instead (Citation18).
Intense pulsed light (IPL)
The IPL system delivers a broad range of non-coherent light in the spectrum of 400 nm to 1400 nm. The larger spot sizes associated with most IPL hand pieces allows for a larger target area, and thus a large amount of hair to be treated simultaneously. The light beam is delivered to the skin through a quartz or sapphire light guide and a translucent cooling gel is topically applied prior to the treatment. Szima et al. (Citation19), conducted a study on 38 untanned volunteers with Fitzpatrick skin types II to III, and brown or black terminal hair. Patients underwent seven treatment sessions on the leg at 4- to 6-week intervals, with a 6- and 18-month follow-up. Unwanted leg hair was decreased safely and efficiently by both systems; however, IPL had less side effects and higher satisfaction scores.
Hazards
Lasers are classified according to the potential harm that the laser beam can cause, namely Class one to Class four. Typically, when using a laser device for hair removal, class three or four lasers are used. The incorrect use of these devices can give rise to a number of complications. The most common skin complications include folliculitis, post-treatment transient and reticulate erythema, perifollicular oedema, ocular complications, pain, crusting and purpura (Citation20–Citation22). More severe side effects can also occur, which include thermal burns resulting in permanent scarring, blisters and pigmentary changes (hyper-and hypopigmentation) (Citation23). Other uncommon side effects include the induction or aggravation of acne, rosacea-like rash, premature greying of hair, tunnelling of hair under the skin, prolonged diffuse redness and oedema of the face, and inflammatory and pigmentary changes of pre-existing nevi (Citation24). Some of the reported ocular complications include cataracts, iritis, iris atrophy, pupillary distortion, uveitis, photophobia, posterior synechiae, and visual field defects. These have all been reported despite the use of metal protective lenses (Citation25).
Improper wavelength selection or improper fluencies are common errors that occur. The Canadian Dermatology Association states that “73 per cent of dermatologists surveyed have treated patients for burns, scars or other wounds sustained after seeking laser treatments“ (Citation26). Nowdays, most high power laser systems have cooling devices integrated into the system, with a view of protecting the epidermis, reducing pain and erythema, and improving the efficacy of the laser treatment (Citation27). Cooling mechanisms make use of cold air, liquid nitrogen (cryogen spray), aqueous gels, and water encased in a sapphire window (Citation28). The aim of these devices is to get the most out of the thermal damage to the target chromophores while reducing injury to the normal surrounding tissue (Citation27).
A voluntary, anonymous study conducted by the Radiation Health Committee Working Group in Australia investigated the use of laser and IPL devices for cosmetic purposes. The survey was conducted from 15 November 2012 to 13 December 2012 (the 2012 survey) in registered health practitioners and non-medical practitioners. The aim of the study was to seek data on accidents and incidents caused by the use of laser and IPL devices (Citation29). The survey attracted 430 responses from five medical practitioner groups (38%) and six other health and beauty practitioner groups (62%). Responses by medical practitioners revealed that there were 62 cases in which the diagnosis of skin cancer was missed or delayed, and was incorrectly treated with IPL or laser in a 12-month period, which represents a significant health risk with devastating outcomes for the patients. Other results showed that there were 416 injuries in the preceding 12 months. Of these, 268 injuries were labelled as severe and included burns, blistering, skin discolouring and scarring. It was reported that more than 50% of the 268 severe injuries was due to inadequate training. There was also the reporting of one case of eye injury (Citation29).
Another national survey conducted in Germany was conducted from October 2009 to January 2010 (Citation30). This retrospective analysis assessed 50 patients who reported treatment errors by laypersons. Data from seven patients were excluded due to missing, uncertain, or unspecific data. Of the laypersons administering treatment, 2.3% were tattoo artists, 13.9% were trained assistants, 32.6% had unidentified qualifications and 51.2% were cosmetologists. The following devices were used: 62.8% were treated with IPL, 18.6% were treated with a laser, and in 18.6% the modality was uncertain. The survey reported the following complications: 81.4% ensued pigmentary changes; 25.6% had scarring; 14% had textural changes; and 4.6% had non-clearance. The following treatment errors were reported to have occurred: excessive energy application (62.8%); incorrect selection of treatment device (39.5%); inadequate skin cooling resulting in over heating of the area (7%); and inadequate information (4.6%) (Citation30).
Between the period of 01 January 2009 to 31 December 2011, a total of 61 adverse incident reports involving laser hair removal were reported in the United States, in which 88 patients were reportedly injured by laser hair removal devices (Citation31). In 2009 a total of 22 reports were filed in which 37 patients were reported as injured. In 2010 a total of 25 reports were filed in which 31 patients were reported as injured, and in 2011 a total of 14 reports were filed by 20 patients. Out of the 88 patients, three were removed as one involved a laser purchased for home use, one was determined to have a psychiatric condition with no actual injury, and one was reported injured in a non-hair removal procedure. Of the remaining 85 patients, the following treatment errors were reported: eight were as of the result of the inadequate conduct of a patch test; seven were as of the result of overtreatment; eight were as of the result of incorrect settings or exercising poor technique with the hand device; 26 were due to poor equipment maintenance; two were due to treating patients who had recently achieved tans; one was due to failure to calibrate the device correctly; one was due to failure to shave the area prior to treatment; one was due to the treatment of a patient who had been taking medication that caused hyper-photosensitivity; and in 31 of patients, the cause of injury could not be determined. The following complications were reported: 58 patients were reported as having burns (four having third-degree burns, and 54 having first or second degree burns); nine reported scarring; seven reported having blisters; two reported having redness or inflammation; six reported having hypopigmentation; two reported having swelling; and one reported an “adverse reaction” which was not specified (Citation31).
The Food and Drug Administration (FDA) requires that manufacturers and device users submit medical device reports (MDRs) for suspected injuries from device use or malfunction. A study conducted by Tremaine and Avram, between 1991 and December 2013 has shown diode lasers to be the second most frequently reported technology, with 252 MDRs (Citation32). Blisters and burns were the most common adverse events. In many cases the complications were thought to occur secondary to operator error; either inadequate device maintenance or improper settings. IPL had 158 MDRs and broadband light (BBL) had 22 MDRs. The most commonly reported adverse events included burns, dyschromia and scarring. There was a total of 246 MDRs associated alexandrite (118 MDRs) and Nd:YAG (99 MDRs) lasers. The most common adverse events observed included burns, blisters and dyschromia (Citation32).
Hazards not only exist for the patients, but also include occupational risks for the operator. These include exposure to the laser plume which consists of the particulate debris, vapours, and smoke produced during a laser hair removal treatment. The laser plume is known to be carcinogenic as well as being a teratogen. There is an increase in published literature on the adverse health effects of ambient exposures to ultrafine particles (UFP), however little is known regarding occupational exposures while performing a laser hair removal treatment. During a laser hair removal procedure, Chuang et al. (Citation33), indicated that burning-hair plume present during laser hair removal should be considered a biohazard. They tested discarded terminal hairs from two adult volunteers, which was sealed in glass gas chromatography chambers and treated with a laser. The laser plume was analyzed by gas chromatography–mass spectrometry (GC-MS), with the identification of 377 chemical compounds, of which 13 are known or suspected carcinogens and more than 20 are known environmental toxins. They also tested UFPs during a laser hair removal procedure using a portable condensation particle counter (CPC) in the waiting room, and in the treatment room at baseline, during, and after treatment. The results showed a considerable increase in UFPs, with between 69 976 and 129 376 particles per cubic centimeter at the level of the laser practitioner (Citation33). Eshleman and colleagues (Citation34) measured the concentrations of UFPs in the procedure and waiting rooms before, during and after laser hair removal procedures. Twelve procedures were sampled over a period of 4 days. As expected, the mean UFP concentration in the procedure rooms was higher than levels in the waiting room. UFP levels increased swiftly in the procedure room during treatment, peaked at the end of the procedure, and decreased after procedures. Levels did not return to pre-treatment concentrations. UFP levels were directly related to the duration of the procedures, and interestingly there was a decrease in UFPs when a pre-laser lotion was used (Citation34).
Regulation
Leading up to October 2010, healthcare professional and non-healthcare professional treatment providers performing treatments with lasers and intense light sources (which includes IPL and light emitting diodes) in England were regulated by the Care Quality Commission (CQC). The CQC regulated facilities providing either non-surgical cosmetic interventions or treatments of disorder, disease, injury or both. The Care Standards Act 2000 included standards for various providers. These standards comprised of ‘Prescribed Techniques and Prescribed Technologies’ (‘P’ standards) for laser and intense light sources (ILS). The ‘P’ standards form the basis for the IHAS Essential Standard which was updated in 2015/2016. It was then re-launched by the British Medical Laser Association (BMLA) in October 2016. The UK government however deregulated the cosmetic sector (non-surgical cosmetic intervention) in England with the repeal of the Care Standard Act 2000, which means anyone may legally purchase a laser and ILS device and perform treatments with little to no training. Non-healthcare professional treatment providers are no longer required to register with the CQC to perform cosmetic laser or IPL treatments which include hair removal. In addition to this, there are few restrictions on enforcement of holding suitable insurance or working from appreciated premises (Citation35). Despite the repeal of the Care Standards Act 2000 that took place in England, the provision of the ‘P’ standards still applies in Wales and Northern Ireland. The ‘P’ standards are enforced by the Health Inspectorate Wales (HIW) (Citation36) and the Regulation and Quality Improvement Authority (RQIA) in Northern Ireland (Citation37). In certain regional areas of England, namely Nottingham, London, Birmingham and some areas in Essex boroughs, a licensing scheme exists for establishments that performs ‘special therapies’ which include laser and ILS therapy. In Scotland, registration is a requirement to perform laser and ILS treatments but this currently only applies to medical healthcare practitioners (Citation35).
In the United States, the first state to instate mandatory training hours for light based treatments and laser hair removal was Arizona. In the case of laser hair removal, the candidate is required to complete 40 hours of theoretical education, as well as 24 hours hands on practical training in laser hair removal, with an additional 24 hours on other light based treatments, i.e. IPL. All training is to be completed at state approved facilities under the supervision of a health professional or laser technician who has a minimum of 100 hours practical experience (Citation38). In Texas, for a candidate to obtain a laser hair removal professional certificate, he/she is required to be certified by a recognised certifying agency, including the Society for Clinical and Medical Hair Removal or another certification entity approved by the department. In addition, the candidate would need to meet the requirements for a senior laser hair removal technician certificate as well as pass an examination (Citation39). In order to receive a certificate as a Senior Laser Technician, applicants must observe 100 laser hair removal treatments on approved body parts performed by a registered apprentice (Citation39). In the state of Florida, applicants are required to complete a 30 hour continuing education course approved by the council, Florida Administrative Code (F.A.C), followed by a minimum of five hours practical experience in laser and light based devices (Citation40). National certification is conferred by the Electrolysis Council and the Board of Medicine, which is part of the Society of Clinical & Medical Hair Removal (Citation41).
In Australia, only Tasmania, Queensland and Western Australia regulate Class 3B and Class 4 laser operators. The remaining states have not yet introduced a regulatory framework for the operation and use of laser and IPL devices. Non-medical professionals in Queensland are required to be licensed in order to use a laser device, but not in the case of IPL therapy. However, in Tasmania a licence is required by non-medical professionals to operate both laser and IPL devices. Operators must also be supervised by a registered medical practitioner. In Western Australia, the use of lasers must be operated under direct supervision, this however does not apply to IPL users. The users of both laser and IPL needs to be licenced (Citation29).
In South Africa, the opposite exists. Currently there is no regulation governing who is allowed to perform laser treatments and what qualification/s are required. There are no systems in place to ensure that operators are competent to perform these treatments, particularly laser hair removal. In addition to this concern, there is no legislation regarding the supply and purchase of laser devices. Anyone, without the official appropriate qualification or experience, with a sufficient amount of capital, can purchase a laser device. Most suppliers of devices in South Africa may offer informal, non-accredited training for a period of two to four days. This does not meet the standards as set out by the South African Association of Health and Skincare Professional (SAAHSP), which states that in order to obtain accredited training the duration of the course should be a minimum of 100 hours (Citation12).
Conclusion
The unwanted presence and growth of hair on certain body parts is an everyday concern for many women, and even some men, with the increased preference for a “neat image” and what society perceives as acceptable (Citation1). The occurrence of excessive hair, especially facial hair in women, can lead to emotional distress and decreased quality of life. A number of treatments are available for their removal. Temporary methods are relatively inexpensive and convenient; however, they only offer interim results and treatments must to be repeated on a regular basis. An alternative option is permanent removal that makes use of lasers and IPL devices.
Laser hair removal and IPL treatments are one of the most widely performed, minimally invasive cosmetic procedures performed, highlighting the popularity of this treatment. It relies on photothermal destruction, through the principles of selective photothermolysis, to induce damage to hair. However, epidermal melanin also competes for photon absorption, which poses a risk for burns. Thus, dark skin types pose further complications for laser hair removal. In spite of this, advances in technology and the proper protocol does allow for these procedures in such individuals, however great care should be taken. A number of other risks are also associated with the treatment; however, all of these can be reduced through the proper theoretical understanding and adequate training. Not only do risks exist for patients, but there are also occupational risks associated with laser operators. High levels of UFPs have been identified, and levels remain high even with the use of a smoke extractor. Further research into long term repeated exposure to these UFPs is necessary and warranted.
Approximately 30% of all complications associated with laser therapy can be attributed to non-medical personnel (Citation3). In certain parts of the world, strict guidelines exist for operators, as well as clinics or salons performing laser and light based therapies, including laser hair removal. While in South Africa, the lack of any form of regulation and qualification is problematic. The absence of formal training and regulation poses a large risk to the public. Lack of regulation also leads to individuals creating their own job titles such as “medical aesthetician”, which are not recognised credentials. No specific accreditation is currently required for aestheticians to work in medical spas or laser clinics in South Africa. The regulation of such procedures will enforce the required knowledge and skills under a standardised licencing board exam administered by an established government recognised tertiary institution, which would substantially lower the risk to the public.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the manuscript.
Additional information
Funding
References
- Jo S, Kim J, Ban J, Lee Y, Kwon O, Koh W. Efficacy and safety of hair removal with a long-pulsed diode laser depending on the spot size: a randomized, evaluators-blinded, left-right study. Ann Dermatol. 2015;27:517–22. doi:10.5021/ad.2015.27.5.517.
- Thacker P, Kumar P. Near infrared pulsed light for permanent hair reduction in fitzpatrick skin types IV and V. J Cutan Aesthet Surg. 2016;9:249–53. doi:10.4103/0974-2077.197078.
- Paasch U, Schwandt A, Seeber N, Kautz G, Grunewald S, Haedersdal M. New lasers and light sources - old and new risks? J Dtsch Dermatol Ges. 2017;15:487–96.
- American Society for Aesthetic Plastic Surgery. Cosmetic surgery national data bank statistics; 2016 [accessed 2017 Dec 3]. http://www.surgery.org/sites/default/files/.
- Agarwal M, Velaskar S, Gold MH. Efficacy of a low fluence, high repetition rate 810nm diode laser for permanent hair reduction in indian patients with skin types IV–VI. J Clin Aesthet Dermatol. 2016;9:29–33.
- Altshuler GB, Anderson RR, Manstein D, Zenzie HH, Smirnov MZ. Extended theory of selective photothermolysis. Lasers Surg Med. 2001;29:416–32. doi:10.1002/(ISSN)1096-9101.
- Fayne RA, Perper M, Eber AE, Aldahan AS, Nouri K. Laser and light treatments for hair reduction in fitzpatrick skin types IV–VI: a comprehensive review of the literature. Am J Clin Dermatol. 2017. doi:10.1007/s40257-017-0316-7.
- Karsten A, Singh A. Quantifying the influence of the epidermal optical properties on laser treatment parameters. European Conferences on Biomedical Optics: International Society for Optics and Photonics; 2013. doi:10.1117/12.2032511.
- Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg. 2013;39:823–38. doi:10.1111/dsu.12116.
- Martella A, Raichi M. Photoepilation and skin photorejuvenation: an update. Dermatol Rep. 2017;9:7116. doi:10.4081/dr.2017.7116.
- Patil U, Dhami L. Overview of lasers. Indian J Plast Surg. 2008;41 Suppl S1:101–13.
- Crichton P. Informative articles laser or IPL treatments; 2012 [accessed 2016 May 28]. http://www.saahsp.co.za/info_laser_IPL_treatments.ph.
- Lepselter J, Elman M. Biological and clinical aspects in laser hair removal. J Dermatol Treat. 2004;15:72–83. doi:10.1080/09546630310023152.
- Courtney E, Goldberg D. Clinical evaluation of hair removal using an 810 nm diode laser with a novel scanning device. J Drugs Dermatol. 2016;15:1330–33.
- Campos VB, Dierickx CC, Farinelli WA, Lin TY, Manuskiatti W, Anderson RR. Ruby laser hair removal: evaluation of long-term efficacy and side effects. Laser Surg Med. 2000;26:177–85. doi:10.1002/(SICI)1096-9101(2000)26:2<177::AID-LSM8>3.0.CO;2-J.
- Moon H-R, Lee J-H, Lee G, Rhee D-Y, Park G, Won CH, Chang S-E, Lee M-W, Choi J-H, Moon K-C, et al. Long-pulsed Alexandrite Laser vs. Intense pulsed light for axillary hair removal in Korean women. Med Laser. 2012;1:11–15.
- Royo J, Urdiales F, Moreno J, Al-Zarouni M, Cornejo P, Trelles MA. Six-month follow-up multicentre prospective study of 368 patients, phototypes III to V, on epilation efficacy using an 810-nm diode laser at low fluence. Lasers Med Sci. 2011;26:247–55. doi:10.1007/s10103-010-0846-1.
- Lanigan SW. Incidence of side effects after laser hair removal. JAAD. 2003;49:882–86. doi:10.1067/S0190.
- Szima GZ, Janka EA, Kovács A, Bortély B, Bodnár E, Sawhney I, Ė S, Remenyik Ė. Comparison of hair removal efficacy and side effect of neodymium: yttrium-aluminum-garnetlaser and intense pulsed light systems (18-month follow-up). J Cosmet Dermatol. 2017;16:193–98. doi:10.1111/jocd.12312.
- Lapidoth M, Shafirstein G, Ben Amitai D, Hodak E, Waner M, David M. Reticulate erythema following diode laser-assisted hair removal: a new side effect of a common procedure. J Am Acad Dermatol. 2004;51:774–77. doi:10.1016/j.jaad.2004.04.017.
- Nanni CA, Alster TS. Long-pulsed alexandrite laser-assisted hair removal at 5, 10, and 20 millisecond pulse durations. Lasers Surg Med. 1999;24:332–37. doi:10.1002/(ISSN)1096-9101.
- Vano-Galvan S, Jaen P. Complications of nonphysician-supervised laser hair removal. Case report and literature review. Can Fam Physician. 2009;55:50–52.
- Alster TS, Khoury RR. Treatment of laser complications. Facial Plast Surg. 2009;25:316–23. doi:10.1055/s-0029-1243080.
- Rasheed AI. Uncommonly reported side effects of hair removal by long pulsed-alexandrite laser. J Cosmet Dermatol. 2009;8:267–74. doi:10.1111/j.1473-2165.2009.00465.x.
- Brilakis HS, Holland EJ. Diode-laser-induced cataract and iris atrophy as a complication of eyelid hair removal. Am J Ophthalmol. 2004;137:762–63. doi:10.1016/j.ajo.2003.11.009.
- Sourtzis L. W5 investigation: the painful side to laser skin treatments. CTV News. 2012 [accessed 2017 Nov 11]. https://www.ctvnews.ca/w5-investigation-the-painful-side-to-laser-skin-treatments-1.759779.
- Das A, Sarda A, De A. Cooling devices in laser therapy. J Cutan Aesthet Surg. 2016;9:215–19. doi:10.4103/0974-2077.197028.
- Gold MH. Lasers and light sources for the removal of unwanted hair. Clin Dermatol. 2007;25:443–53. doi:10.1016/j.clindermatol.2007.05.017.
- Australian Radiation Protection and Nuclear Safety Agency (ARPANSA). Regulatory Impact Statement. Intense Pulsed Light sources (IPLs) and lasers for cosmetic or beauty therapy; 2015 accessed 2017 Aug 22]. https://www.arpansa.gov.au/consultation-regulatory-impact-statement-intense-pulsed-light-sources-ipls-and-lasers-cosmetic.
- Hammes S, Karsai S, Metelmann HR, Pohl L, Kaiser K, Park BH, Raulin C. Treatment errors resulting from use of lasers and IPL by medical laypersons: results of a nationwide survey. J Dtsch Dermatol Ges. 2013;11:149–56.
- Food and Drug Administration. Reporting adverse events (Medical Devices); 2011 [accessed 21 September 2017]. http://www.fda.gov/MedicaiDevices/DeviceRegulationandGuidance/PostmarketRequirements/ReportingAdverseEvents/default.htm.
- Tremaine A, Avram M. FDA MAUDE data on complications with lasers, light sources, and energy-based devices. Lasers Surg Med. 2015;47:133–40. doi:10.1002/lsm.22328.
- Chuang GS, Farinelli W, Christiani DC, Herrick RF, Lee NC, Avram MM. Gaseous and particulate content of laser hair removal plume. JAMA Derm. 2016;152:1320–26. doi:10.1001/jamadermatol.2016.2097.
- Eshleman EJ, LeBlanc M, Rokoff LB, Xu Y, Hu R, Lee K, Chuang GS, Adamkiewicz G, Hart JE. Occupational exposures and determinants of ultrafine particle concentrations during laser hair removal procedures. Environ Health. 2017;16:30. doi:10.1186/s12940-017-0239-z.
- Town G, Brown ER. Laser and light intervention standards. Aesthetics J. 2017;5(1):30–35.
- Healthcare Inspectorate Wales. Welcome to Healthcare Inspectorate Wales; 2017 [accessed 2018 Aug 10]. http://hiw.org.uk/?skip=1&lang=en.
- Nidirect government services. Regulation and quality improvement authority (RQIA). RQIA Provider Guidance 2017–2018 - Independent Hospital - Cosmetic Laser/Intense Pulse Light Services; [accessed 2018 Aug 10]. https://www.nidirect.gov.uk/contacts/contacts-az/regulation-and-quality-improvement-authority-rqia.
- Arizona Revised Statutes. Professions and occupation. Title 32, Article 2; 2014 [accessed 2018 Jan 25]. https://boc.az.gov/sites/default/files/documents/files/Arizona%20Revised%20Statutes%207-2014.pdf.
- Texas Department of Licensing and Regulation. Laser hair removal. Health and safety code; 2017 [accessed 2017 Nov 18]. https://www.tdlr.texas.gov/las/laslaw090117.pdf.
- Silberman L. The lowdown on hair removal; 2012 [accessed 2016 Apr 28]. http://nationallaserinstitute.com/laser-laws-lowdown-hair-removal/.
- Florida Health. Laser information; 2014 [accessed 2017 Dec 20]. http://www.floridahealth.gov/licensing-and-regulation/electrolysis/laser/index.html.