Abstract
Objective
To evaluate the cumulative amount of iatrogenic blood loss in extreme preterm infants during the first month of life.
Study design
We performed an observational cohort study in 20 extreme preterm infants (gestational age <28 weeks). We recorded the amount of blood drawn for laboratory testing during the first 4 weeks of life, the number of punctures for phlebotomy and intravenous access and the amount of blood loss associated with these procedures. We compared the cumulative blood loss to the estimated total blood volume (85 ml/kg body weight) and to the total volume of red blood cell (RBC) transfusions administered during the same study period.
Results
The median cumulative iatrogenic blood loss was 24.2 ml/kg (interquartile range (IQR) 15.8–30.3 ml/kg) per patient, which equals a median of 28.5% (IQR 18.6–35.6%) of the total blood volume. Blood loss was higher in the most extreme preterm infants (30.2 ml/kg at 24 weeks versus 15.9 ml/kg at 27 weeks). The median number of punctures per infant was 47 (IQR 26–56) during the first 4 weeks of life. The median volume of RBC transfusions administered during the study period was 30 ml/kg, slightly more than the cumulative blood loss (24.2 ml/kg).
Conclusions
Extreme preterm infants lose almost one-third of their total blood volume in the first month of life as a result of blood loss due to multiple blood draws for laboratory investigations, and procedures.
Introduction
Anemia of prematurity (AoP) is a common hematologic finding in preterm infants admitted to neonatal intensive care units (NICUs). Nearly all extremely preterm infants develop AoP and up to 90% require at least one red blood cell (RBC) transfusion during their NICU stay [Citation1,Citation2]. AoP is partly due to normal physiological processes such as increasing body weight, shorter life span, and clearance of neonatal RBCs and relative insufficient erythropoiesis. However, another important cause of AoP seems to be related to iatrogenic blood loss due to frequent laboratory investigations. Recently, several small studies reported that preterm infants may lose more than half of their blood volume due to cumulative laboratory blood sampling in the first weeks after birth [Citation3–5]. Not surprisingly, a direct correlation was found between the volume of phlebotomy blood loss and volume of RBC transfusions, emphasizing the necessity of reducing blood loss in order to reduce the need of transfusions [Citation6]. Importantly, transfusions of blood products are increasingly being reported to be associated with an increased risk of inflammatory responses, neonatal morbidity, and mortality [Citation1]. Reducing iatrogenic blood loss in preterm infants could therefore not only reduce the need for transfusions but simultaneously also reduce the associated risk of mortality and morbidity [Citation7].
Despite the importance of AoP and the association with iatrogenic blood loss, detailed information on the cumulative amount of phlebotomy blood loss in extremely preterm infants remains limited. In addition, not much is known on the cumulative number of punctures and the relation with timing after birth and gestational age in this high-risk group of patients.
The aim of our study is to evaluate the amount of iatrogenic blood loss and number of punctures in extreme preterm infants during the first month of life and to use this as a baseline for comparison after implementing blood-saving strategies in the future.
Materials and methods
This retrospective observational cohort study was conducted at the Leiden University Medical Center (LUMC), a tertiary care center in the Netherlands. Extreme preterm infants admitted to our NICU between February and December 2016, with gestational age at birth between 24 + 0 and 28 + 0 weeks were included in the study. Infants that were admitted less than 21 days or that died in the first 21 days of life were excluded from analysis. The study was approved by the Leiden Medical Ethics Committee (institutional review board) (G17.127).
We collected data from the medical records on the amount of blood drawn for laboratory testing, the number of punctures for phlebotomy and intravenous access and the amount of blood loss associated with these procedures during the first 28 days of life. During the study period, the amount of blood drawn for laboratory tests and the exact number of punctures was recorded in the medical record by the caretaker performing each procedure. If several punctures were needed to obtain one lab, these were counted separately. A capillary tube used for a blood gas was defined to contain 85 µl, a capillary tube for bedside glucose or bilirubin both contain 10 µl of blood. At our NICU, an in-line point of care is routinely used for the analysis of blood gas, glucose, and bilirubin. Blood volume for other laboratory tests and blood cultures was measured in a syringe before transferring it to the blood collection containers. A strict protocol is routinely used to determine the exact amount of blood needed for each specific laboratory test; if more blood was drawn this was defined as blood overdraw. This overdrawn blood loss in the needle for a venepuncture was defined as 100 µl. Blood loss in gauze pads was estimated by noting the number of blood drops, one blood drop was defined to be 62.5 µl. The mean iatrogenic blood loss was reported in ml per kg birth weight.
We recorded the following neonatal parameters: gestational age at birth, birth weight, gender, mode of delivery, use of antenatal steroids, days of mechanical ventilation, and use of an arterial line.
We recorded the number of RBC transfusions administered in the same 28-day period. The criteria for RBC transfusions used are based on a Cochrane systematic review from 2011 [Citation8]. The volume used for an RBC transfusion was 15 ml/kg. We compared the cumulative blood loss to the total blood volume (estimated at 85 ml/kg body weight) [Citation9,Citation10] and to the total volume of received RBC transfusions.
The primary outcome was the cumulative amount of iatrogenic blood loss in the first 28 days of life. Secondary outcomes are iatrogenic blood loss compared to RBC transfusions, the amount of blood overdraw and the number of punctures.
Statistical analysis
Results for the non-normally distributed values are expressed as median with interquartile range (IQR). The Mann–Whitney U test was used for non-normally distributed continuous variables. A p value <.05 was considered to indicate statistical significance. Statistical analyses were performed using SPSS version 23.0 (IBM, Chicago, IL, USA).
Results
A total of 25 preterm infants born between 24 + 0 and 28 + 0 weeks admitted during the study period were eligible in the study. Five infants were excluded: one neonate died on the second day of life and four others were transferred to another hospital within the first 21 days of life. Data of the remaining 20 infants were collected for analysis.
Baseline characteristics are described in . presents the median amounts of blood loss, punctures, blood overdraw, and RBC transfusions.
Table 1. Baseline characteristics.
Table 2. Results of cumulative iatrogenic blood loss, punctures, and RBC transfusions.
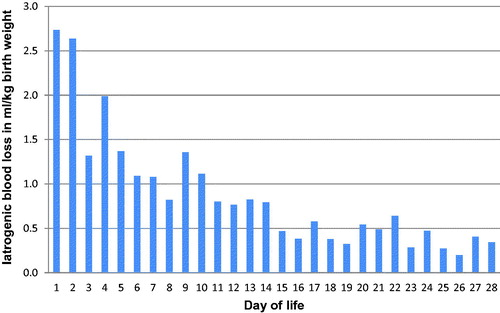
The median cumulative iatrogenic blood loss in the first 4 weeks of life was 19.6 ml (IQR 16.5–25), which equals 24.2 ml/kg (IQR 15.8–30.3 ml/kg) (i.e. 0.9 ml/kg/day). When compared to the total blood volume (estimated at 85 ml/kg), this translates to a median blood loss of 28.5% (IQR 18.6–35.6%) of the total blood volume. The amount of iatrogenic blood loss was the greatest in the first days of life and showed a gradual decline afterward ().
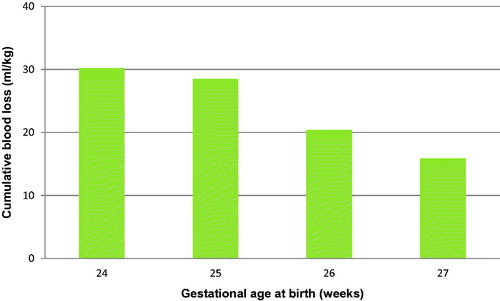
The median cumulative iatrogenic blood loss showed a gradual decline with increasing gestational age at birth, from 30.2 ml/kg at 24 weeks to 15.9 ml/kg at 27 weeks (). The total volume of blood overdraw was 0.9 ml (IQR 0.7–1.4), which is 4.7% of the total blood loss.
Figure 2. Median cumulative iatrogenic blood loss in ml/kg birth weight during the first 28 days of life per week of gestational age.
The median blood loss during the days with mechanical ventilation was 1.1 ml/kg/day (IQR 0.4–2.0) versus 0.15 ml/kg/day (IQR 0.1–1.0) for the days without mechanical ventilation (p < .001). The median blood loss during the days with an arterial line was 1.5 ml/kg/day (IQR 0.8–2.5) versus 0.2 ml/kg/day (IQR 0.1–0.7) for the days without an arterial line (p < .001).
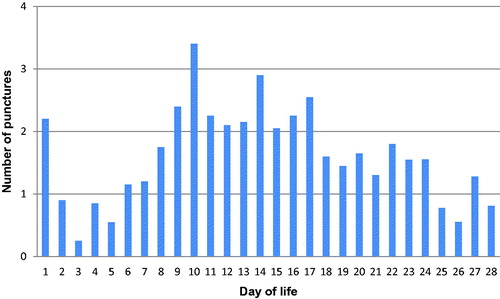
The median number of punctures was 47 in 28 days (range 13–102 punctures per patient). The mean number of punctures was lower in the first week after birth compared to the second and third week ().
Eighteen infants (90%) received one or more RBC transfusions, with a median of 2 (IQR 1–3) transfusions per patient or 30 ml/kg (IQR 15–45) ().
Discussion
Several findings can be deducted from this observational cohort study. First, the study shows that the cumulative iatrogenic blood loss in extreme preterm infants in the first 28 days of life is high and is approximately 24 ml/kg, which equals to almost a third of the total blood volume. Second, this blood loss occurs primarily in the first week of life. This can partly be explained by the fact that most days of mechanical ventilation (and the associated need for frequent testing of blood gases) occur during the first week of life. Importantly, blood loss was almost twice higher in extreme preterms born at 24-week gestation compared to preterm infants born at 27 weeks, 30.2 versus 15.9 ml/kg. Finally, the amount of iatrogenic blood loss was almost equal to the volume of RBC transfusions required in the first month of life, confirming that blood loss is one the major causes of the high need of RBC transfusions in preterm infants.
Several small studies previously reported on the cumulative blood loss due to iatrogenic blood loss but found varying results. In 2005, Widness et al. reported an estimated cumulative blood loss of 70 ml/kg in 2 weeks’ time in 47 preterm infants [Citation5]. More recently in 2013, Rosebraugh et al. studied cumulative blood loss in 26 preterm infants and reported a loss of around 60 ml/kg in 30 days [Citation3]. Christensen et al. compared phlebotomy blood losses in multiple small studies. They found a wide range in cumulative phlebotomy blood loss of 14.2–98.5 ml/kg, with study periods varying from 7 to 70 days [Citation4].
These large variations in reported total blood loss can be due to various reasons, including differences in the studied population, in particular, the gestational age at birth, but also the type of included measurements. Other explanations include differences in clinical practice between caregivers concerning the frequency of blood testing and differences in the amount of blood needed depending on the type of testing devices.
Overall, the percentage of blood loss in our observational study was significantly lower than reported in the previous, albeit limited literature, even after accounting for the fact that we also measured blood loss while requiring intravenous access and in gauze pads. In most studies, only phlebotomy blood loss was measured.
The lower amount of blood loss reported in our study (compared to the literature) could be due to the routine use of a strict protocol for labs, the use of in-line point of care, and a continuous attention within our team on the importance of minimization of laboratory tests and procedures. Decreasing the frequency and amount of phlebotomy loss is probably the area in the field of neonatology that can be changed the quickest. This will automatically decrease the risk of neonatal anemia and save substantial transfusions and complications.
In agreement with other studies [Citation3–5,Citation11,Citation12], the cumulative iatrogenic blood loss is directly associated to the volume of RBC transfusions, suggesting that iatrogenic blood loss is the main cause of AoP and RBC transfusions. In adults, RBC transfusions are associated with an increased risk of typical transfusion-related side effects such as TRALI (transfusion-associated lung injury). In preterm infants, also other inflammatory responses may occur such as TANEC (transfusion-associated necrotizing enterocolitis). This phenomenon is not fully understood and is not only confined to RBC products. Notwithstanding that, a recent randomized trial comparing liberal versus restrictive platelet transfusions in preterm infants showed that the group with more liberal transfusions had an increased risk of mortality and morbidity, including chronic lung disease [Citation7]. Reducing iatrogenic blood loss in preterm infants could therefore reduce both the need for transfusions as well as the associated risk of mortality and morbidity [Citation1,Citation13].
This study also showed that extreme preterm infants are exposed to an impressive number of punctures in the first month of life. The median number of punctures per infant was 47 (IQR 26–56), including punctures for intravenous access. The mean number of punctures was lower in the first week after birth compared to the second and third week. This is probably due to the more frequent use of arterial lines in the first week of life, reducing the need for frequent phlebotomies and intravenous access. In a similar group of preterm infants also born before 28 weeks of age, Rosebraugh et al. reported a strikingly higher cumulative number of punctures (138 ± 21.2 phlebotomies during the first month of life) [Citation3]. Discrepancies between these and our findings could be due to differences in clinical practices, such as lower frequency of laboratory tests, lower duration of mechanical ventilation, and higher use of arterial lines in our cohort. Unfortunately, these factors were not described in the study from Rosebraugh et al. Reducing the number of punctures in preterm neonates is not only important to improve the care for this specific group of high-risk infants, but also in the context of the evolving literature on the long-term effects of noxious stimuli in the newborn.
In general, any strategy to avoid the development and persistence of anemia in preterm infants by limiting iatrogenic blood loss will always be beneficial and is of crucial importance. Our current strategies include drawing first complete blood count, type and screen, and C-reactive protein (CRP) from umbilical cord blood and placental blood at birth, strict adherence to protocols on the amount of blood that is needed for every specific test and bedside point-of-care testing with the lowest volumes needed. To minimalize the need for RBC transfusions, we use a strict transfusion protocol [Citation8], we give supplemental iron and our local guideline underscores the importance of delayed cord clamping.
In addition, reduction of blood loss could particularly be achieved by reducing laboratory blood testing particularly in the first days of life. On day 1, reduction of iatrogenic blood loss can be achieved by sampling blood cultures from the placenta instead of from the neonate. Furthermore, in-line point-of-care testing through arterial catheters or more reliable end-tidal or transcutaneous CO2 measurement might help to reduce the high blood loss associated with mechanical ventilation or arterial line use [Citation14]. After finishing this study, we adopted the use of transcutaneous CO2 monitors at our NICU to further reduce the frequency of blood gases. Lastly, reduction of blood loss could be achieved by increased awareness in caregivers on the importance of reducing the frequency of laboratory tests and the impact of frequent testing on blood loss and iatrogenic anemia.
Strength and limitations of the study
The strength of this study is that we measured the amount of blood drawn instead of estimating the blood loss and we also included blood loss in gauze pads. As we use standardized volumes for each blood test, we could calculate the amount of blood overdraw quite precisely. Limitations are the small study population and that the amount of blood lost in the gauze pads was estimated by the amount of drops instead of weighed.
In conclusion, our study shows that the cumulative amount of iatrogenic blood loss in the first month of life in extreme preterm infants was almost one third of the total blood volume. Implementing blood saving strategies and creating increased awareness about iatrogenic blood loss with the team of caregivers within each NICU is necessary in order to improve the management and outcome in extreme preterm infants and reduce the use of compensating RBC transfusions and potential complications.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Howarth C, Banerjee J, Aladangady N. Red blood cell transfusion in preterm infants: current evidence and controversies. Neonatology. 2018;114(1):7–16.
- Heeger LE, Counsilman CE, Bekker V, et al. Restrictive guideline for red blood cell transfusions in preterm neonates: effect of a protocol change. Vox Sang. 2019;114(1):57–62.
- Rosebraugh MR, Widness JA, Nalbant D, et al. A mathematical modeling approach to quantify the role of phlebotomy losses and need for transfusions in neonatal anemia. Transfusion. 2013;53(6):1353–1360.
- Christensen RD, Carroll PD, Josephson CD. Evidence-based advances in transfusion practice in neonatal intensive care units. Neonatology. 2014;106(3):245–253.
- Widness JA, Madan A, Grindeanu LA, et al. Reduction in red blood cell transfusions among preterm infants: results of a randomized trial with an in-line blood gas and chemistry monitor. Pediatrics. 2005;115(5):1299–1306.
- Carroll PD, Widness JA. Nonpharmacological, blood conservation techniques for preventing neonatal anemia – effective and promising strategies for reducing transfusion. Semin Perinatol. 2012;36(4):232–243.
- Curley A, Stanworth SJ, Willoughby K, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380(3):242–251.
- Whyte R, Kirpalani H. Low versus high haemoglobin concentration threshold for blood transfusion for preventing morbidity and mortality in very low birth weight infants. Cochrane Database Syst Rev. 2011;11(11):CD000512.
- Bauer K, Linderkamp O, Versmold HT. Systolic blood pressure and blood volume in preterm infants. Arch Dis Child. 1993;69(5 Spec. No.):521–522.
- Wright IMR, Goodall SR. Blood pressure and blood volume in preterm infants. Arch Dis Child Fetal Neonatal Ed. 1994;70(3):F230–F231.
- Becquet O, Guyot D, Kuo P, et al. Respective effects of phlebotomy losses and erythropoietin treatment on the need for blood transfusion in very premature infants. BMC Pediatr. 2013;13(1):176.
- Kling PJ, Sullivan TM, Leftwich ME, et al. Score for neonatal acute physiology and phlebotomy blood loss predict erythrocyte transfusions in premature infants. Arch Pediatr Adolesc Med. 1997;151(1):27–31.
- Rabe H, Alvarez JR, Lawn C, et al. A management guideline to reduce the frequency of blood transfusion in very-low-birth-weight infants. Am J Perinatol. 2009;26(03):179–183.
- Alves-Dunkerson JA, Hilsenrath PE, Cress GA, et al. Cost analysis of a neonatal point-of-care monitor. Am J Clin Pathol. 2002;117(5):809–818.