Abstract
Background
The use of non-prescribed drugs are common to pregnant women. It may lead to undesirable effects, such as birth defects. Study results on the occurrence and predictor of non-prescribed drug use among pregnant women throughout Ethiopia are highly variable and inconsistent. Therefore, the objective of this systematic review and meta-analysis was to estimate the pooled prevalence of non-prescribed drug use and predictors among pregnant women in Ethiopia.
Methods
We systematically searched studies from the international databases, including PubMed, EMBASE, Web of Science, Science Direct, Google Scholar, the Cochrane Library and others. The meta-analysis was conducted using Stata15. I2 test and Egger’s test were used to assess the heterogeneity and publication bias respectively. The random-effect model was used to estimate the pooled prevalence of non-prescribed drug use at a 95% CI.
Results
Eleven studies with a total of 4492 pregnant women fulfilled the inclusion criteria and were included. The pooled national level non-prescribed drug use among pregnant women was 30.38% (95% CI: 20.28, 40.48). The highest use of non-prescribed drug among pregnant women was observed in Amhara region 36.71%, while the lowest was in Tigray region 9.67%, respectively. The most frequently consumed non prescribed drugs by pregnant mothers were paracetamol 34.38%, amoxicillin 14.73%, aspirin 4.25%, metronidazole 2.81% and ciprofloxacin 2.80%. Maternal previous history of self-medication, maternal illness during pregnancy and maternal marital status were significantly associated with women non-prescribed drug use during pregnancy.
Conclusions
The overall prevalence of non- prescribed drug use among pregnant women in Ethiopia is relatively high, and varies across different regions. The most frequently consumed non- prescribed drug by pregnant mothers was paracetamol. Maternal; previous history of self-medication, illness during pregnancy and marital status were significantly associated with pregnant women non-prescribed drug use. Awareness of the possible side effects of taking non-prescribed drugs for all pregnant women is very relevant in the media and in the maternity ward. In particular, it is important to make clear to mothers who have a history of self-medication, to those who have a history of illness during pregnancy and to those who are pregnant, unmarried or divorced.
Backgrounds
Self-medication is described as the use of pharmaceutical or home-made medicinal products without medical prescription to treat symptoms or self-diagnosed health issues [Citation1,Citation2]. It has been reported worldwide and among different age groups, although the magnitude reveals an inconsistency [Citation3–6]. Anti-malarial drugs, antidepressants, antibiotics and cough syrup are prone to self-medication in many developing countries where medications are not well-regulated [Citation7,Citation8].
The magnitude of non-prescribed drug use in developing countries such as Egypt was 86% [Citation9], while in developed countries such as Europe; the magnitude is 68% [Citation10], which differs considerably due to inherent cultural and socio-economic dissimilarities, differences in health services and availability to healthcare and drug delivery policies [Citation11].
People in developing countries, particularly pregnant women, use non-prescribed drugs without constant surveillance [Citation7,Citation12]. People with low socioeconomic status are using medicines suggested by parents who have used the same medicine beforehand [Citation12]. Non-prescribed drug use habits differ across populations [Citation13].
Several reports have suggested that women use non-prescribed drug to treat their menstrual irregularities, hormonal problems, psychological distress, osteoporosis, and pregnancy and breastfeeding problems [Citation14,Citation15]. The overall magnitude of non-prescribed drug use by pregnant women in low-and middle-income countries was 31.5% [Citation16]. In addition, the magnitude of non-prescribed drug use among pregnant women in Ethiopia also ranged from 7.8% in Tigray region [Citation17] to 69.7% in Harar town [Citation18]. While some drugs are intended for non-prescribed drug use and have proven efficacy and protection, they have severe presumptions due to improper use and lack of awareness of their side effects and interactions, particularly in certain groups such as adolescents, elders, pregnant women and breast-feeding women [Citation19,Citation20].
Pregnancy is a rare medical condition where the treatment of drugs raises questions regarding a particular problem. non-prescribed drug use during pregnancy may trigger significant structural as well as physiological adverse effects on the woman's health and the newborn's development [Citation21]. Although it is not a direct cause of maternal and infant mortality, it can lead to abortion, congenital anomalies, disability and death [Citation22–24].
Evidence of safe use has not been established in pregnant women for many commonly used medicines. This is because research on medication efficacy for pregnant women is scarce because pregnant women are frequently excluded from clinical drug studies [Citation25–27]. Limited knowledge on medical products has a major contribution to maternal and neonatal mortality and morbidity and fetal death [Citation21]. Despite this, studies have shown that there is a high amount of self-medication in pregnant women [Citation26].
Maternal and child health is one of the main priorities of the Government of Ethiopia [Citation28] While, a significant achievement has been observed in the reduction of under-five mortality rates. However, the decline in mortality and morbidity in neonatal age groups is not remarkable. Prematurity is the most common cause of neonatal mortality [Citation28]. The avoidance of pregnancy and childbirth complications associated with the practice of self-medication helps protect the health of the mother and fetus [Citation21,Citation29].
Studies have shown that most districts in Ethiopia have an incoherent prevalence of non-prescribed drug use in pregnant mothers. In addition, the risk factors associated with the use of non-prescribed drug use in pregnant mothers and the type of drug they use vary from district to district. Although the evidence in this field is insufficient, the results of the analysis are variable, so it is appropriate to work toward the synthesis of the data. The objective of this systematic review and meta-analysis was to evaluate the pooled use of non-prescribed drug among pregnant women in Ethiopia and identify predictors associated with non-prescribed drug use among pregnant mothers in Ethiopia. The findings of this meta-analysis will help policy makers and other stakeholders in the planning and implementation of strategies to raise awareness of the potential side-effects of non-prescribed drug use on the fetus; some drugs may be teratogenic to humans [Citation30]. The research might also be used as a basis for researchers conducting confirmatory investigations. The question posed was: What are the pooled magnitude and non-prescribed drug use predictors among pregnant women in Ethiopia?
Methods
Identification and study selection
The protocol of this systematic review and meta-analysis has been registered on an international prospective register of a systematic review (PROSPERO), university of York center for reviews and disseminations https://www.crd.york.ac.uk/prospero/. The registration number is CRD42020187704. Three authors (FA, GS & YM) identified both published articles and unpublished research reporting the prevalence and predictors of non-prescribed drug use among pregnant mothers in Ethiopia. All published articles have been searched for major international databases such as PubMed, Cochrane Library, Web of science, science direct, Google Scholar, EMBASE, African Journals Online databases and Google's hand searching mainly for unpublished articles. Besides, a search of the reference list of already identified studies to retrieve additional articles was done (). The search was conducted from 1 February 2020 to 30 April 2020, and it was limited to English language. Unpublished studies have also been searched through Google and Google Scholar. The search terms were determined to include all fields in documents, as well as medical subject headings (MeSH terms) to extend the search in an advanced PubMed search. Within each axis, we merged keywords with the “OR” in the Boolean operator and then linked the search strategies for the two axes to the “AND” operator. The key terms used for the search were “pregnancy,” “gravidity,” “self- treatment,” “self- medication,” “non-prescribed,” “over-the-counter,” “self-administered,” “self-reported,” Ethiopia,” “prevalence,” “occurrence,” “frequency,” “predictors,” Associated factors” and “epidemiology.” All literature accessible until April 2020 was included in the systematic review and meta-analysis. The systematic review and meta-analysis was conducted in agreement with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [Citation31].
Table 1. Example of MEDLINE/PubMed and Google Scholar database searches to analyze the magnitude and predictors of non-prescribed drug use among pregnant women in Ethiopia, 2020.
Study selection
Retrieved studies have been exported to Endnote version 8 reference manager programs to delete duplicate studies. The title and the abstract were screened by three independent reviewers (FA, YM and GS). Based on the defined article selection criteria, the disagreement was controlled. The abstract and whole-text review was performed by three independent authors (FA, YM and GS).
Eligibility criteria
Inclusion criteria
Articles included were those reporting the prevalence of non-prescribed drug use and/or at least one type predictors among pregnant mothers in Ethiopia.
Study area: Only articles conducted in Ethiopia.
Study design: All observational studies (cross-sectional, case controls, and cohort) that contain original data reporting the prevalence and/or at least one type predictors of non-prescribed drug use among pregnant mothers in Ethiopia were considered.
Publication year: no year of limitation of publication or any other restriction has been considered.
Language: Literatures written in English language
Population: Studies that have been conducted among pregnant mothers in Ethiopia.
Publication condition: A consideration was given to both published articles and unpublished research.
Exclusion criteria: Non-accessible studies which are unpublished, irretrievable from the internet or which has not received an email reply from the corresponding authors have been excluded. In addition, a study that did not disclose our outcome of interest has been omitted after a review of the full documents by three authors (FA, GS and YM). Finally, non-full text articles or secondary studies, review types were also removed from this study.
Data abstraction
All the data required were extracted using a clear data extraction format prepared by three authors (FA, GS and YM) in Microsoft Excel TM. For the prevalence of non-prescribed drug use, the data extraction format prepared based on first author, the region where the study was carried out, publication year, sample size, and prevalence of non-prescribed drug use stated for the target group.
The data extraction format for each specific predictor was prepared for predictors based on first author, publication year and variables name (maternal marital status, maternal illness during pregnancy, and previous history of self-medication, maternal education and maternal residence). The researchers selected these variables as the most commonly reported associated risk factors in the studies included in this meta-analysis. In this systematic review and meta-analysis, authors found additional variables as risk factors when two or more studies examined them as risk factors. For each associated risk factor, the data from the primary studies were collected by three authors (FA, GS and YM) in the form of two by two tables to calculate the odds ratio ().
Outcome measurements
This systematic review and meta-analysis have two main outcomes. The primary outcome was the prevalence of non-prescribed drug use among pregnant women in Ethiopia. The second outcome of the study was predictor of non-prescribed drug use among pregnant women in Ethiopia. The prevalence was computed by dividing the number of pregnant mothers who use non-prescribed drugs by the total number of pregnant mothers participating the study (sample size) multiplied by 100.
Quality assessment and data collection
The Newcastle-Ottawa Scale(NOS) quality assessment tool was used to assess the quality of the included studies based on the three components [Citation32]. The primary elements of the tool were evaluated from five stars and the main focus was on the methodological consistency of each primary study. The other component of the tool graded from two stars and mainly concerned with the comparability of each study and the last component of the tool graded from three stars and used to evaluate the results and statistical analysis of each original study. The NOS included three categorical criteria with a maximum score of 10 points. The quality of each study was assessed using the following score algorithms: ≥7 points were considered as “good,” 2–6 points were considered as “fair,” and ≤1 point was considered as “poor” quality studies. Consequently, in order to improve the validity of this systematic review result, only primary studies of fair to good quality have been included. The three reviewers (FA, GS and YM) independently assessed or extracted articles for overall study quality and/or included in the review using a standardized data extraction format. The data extraction format included primary author, year of publication, and region of the study, sample size, and prevalence, and the selected predictors of non-prescribed drug use.
Publication bias and, statistical analysis
The publication bias was assessed using Egger’s [Citation33] and Begg’s [Citation34] tests with a p-value of less than .05. The I2 statistic was used to assess heterogeneity between studies and a p-value of less than .05 was used to detect heterogeneity. As a result of the presence of heterogeneity, a random-effects model was used as a method of analysis [Citation35] resulting in the use of a random-effects meta-analysis model was used to estimate the pooled effect of DerSimonian and Laird [Citation36]. Data were extracted in Microsoft Excel and exported to Stata version 15 for analysis. Sub-group analysis was conducted by region. Besides, a meta-regression model based on sample size and year of publication was used to identify the sources of random variations in the included studies. The effect of selected determinant variables was analyzed using separate categories of meta-analysis [Citation37]. The findings of the meta-analysis were presented using forest plot and Odds Ratio (OR) with its 95% CI. In addition, we conducted a sensitivity analysis to assess whether the pooled prevalence estimates were influenced by individual studies.
Results
Study identification and characteristics of included studies
This systematic review and meta-analysis included published studies of non-prescribed drug use and predictors among pregnant women in Ethiopia using international electronic databases. A total of 439 published articles were found in the review. Of these, 350 duplicated records were deleted and 71 articles were excluded by the screening of titles and abstracts. Subsequently, a total of 18 full-text papers were assessed for eligibility on the basis of the inclusion and exclusion criteria. Thus, seven studies were excluded due to population difference [Citation38–44].
Finally, 11 studies were included in the final quantitative and qualitative meta-analysis (). As regards the design of the included studies, all were cross-sectional, of which nine were cross-sectional institution-based studies (IBCS) and two were cross-sectional community-based studies (CBCS). The review was conducted among 4492 pregnant women in order to estimate the pooled prevalence of non-prescribed drug use. The study was conducted with a maximum sample size of 652 in Amhara region [Citation45] and a minimum sample size of 195 in Oromia region [Citation3]. All the studies were conducted in the four regions of Ethiopia. Of these studies, five were from Oromia region [Citation3,Citation18,Citation46–48], two were from Amhara region [Citation45,Citation49], two were from Tigray region [Citation17,Citation50], and two were from Addis Ababa [Citation51,Citation52] ().
Figure 1. Flow chart describing the selection of studies for the systematic review and meta-analysis of prevalence and use non prescribed drugs and predictors among pregnant women in Ethiopia (showing how articles were identified, screened, and included in the studies).
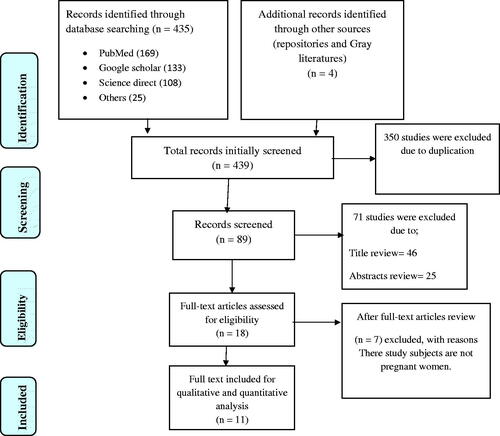
Table 2. Characteristics of included studies in the systematic review and meta-analysis, Ethiopia, 2020.
Meta-analysis of non-prescribed drug use among pregnant women in Ethiopia
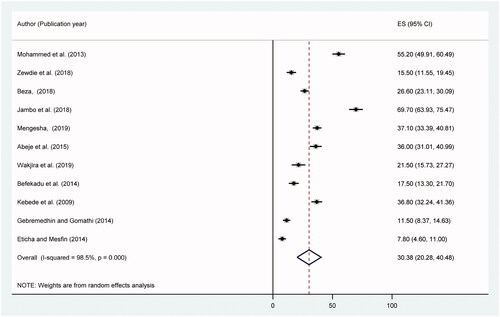
The meta-analysis of eleven studies showed a pooled national level magnitude of non-prescribed drug use among pregnant women in Ethiopia was 30.38% (95% CI: 20.28, 40.48). A random-effect model was used due to significant heterogeneity (I2 = 98.5%, p-value < .001) (). Publication bias was based on the Eggers test with a p-value of .0001 and a trim and fill full analysis was performed. The univariate meta-regression model was used to identify possible sources of heterogeneity based on year of publication and sample size, but none of these variables were found to be statistically significant, p-value >.05. Sensitivity analyzes using a random-effects model showed that no single study had unduly influenced the overall estimate of the non-prescribed drug use among pregnant women in Ethiopia (S1 Figure). Funnel plot symmetry was assessed using Egger’s weighted regression test to examine the presence of publication bias (S2 Figure).
Figure 2. Forest plot of the pooled prevalence of non-prescribed drug use among pregnant women in Ethiopia, 2020.
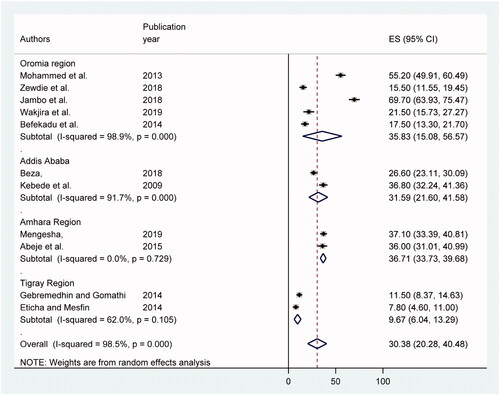
The sub-group analysis of this meta-analysis revealed that the high levels of non-prescribed drug use among pregnant women were observed in Amhara region, 36.71% (95%CI: 33.73, 39.68) followed by Oromia region, 35.83% (95%CI: 15.08, 56.57), Addis Ababa, 31.59% (95%CI: 21.60, 41.58), and lowest was in Tigray region, 9.67% (95%CI: 6.04, 13.29) respectively ().
Predictors of non-prescribed drug use among pregnant women in Ethiopia
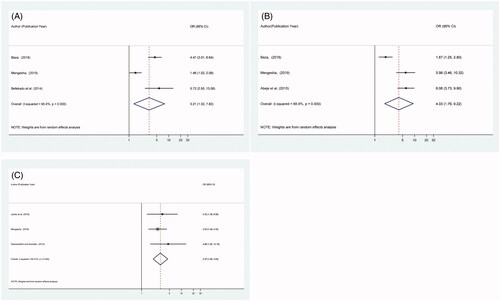
Among the predictor variables described in , those who fulfill the criteria were evaluated; maternal previous history of self-medication (95% CI: 1.32, 7.82), maternal illness during pregnancy (95% CI: 1.76, 9.22) and maternal marital status (95% CI: 1.95, 4.53) were significantly associated with pregnant women non-prescribed drug use during pregnancy while, maternal education (95% CI: 0.55, 2.08) and maternal residency (95% CI: 0.63, 1.71) were not significantly associated with non-prescribed drug use among pregnant women.
In this study, the probability of non-prescribed drug use among pregnant mothers who have the previous history of self-medication was about 3.21 times higher than mothers who have no history of self-medication (OR = 3.21 [95% CI: 1.32, 7.82]). Also, pregnant mothers who reported a history illness during pregnancy were 4.03 times more likely to use drugs by themselves when compared with those who had no history of illness (OR = 4.03, [95% CI: 1.76, 9.22]). Finally, pregnant women who were single or divorced (no husband) were 2.97 times more likely to use non prescribed drugs than those who are married (lives with husband) (OR = 2.97, [95% CI: 1.95, 4.53]) () ().
Table 3. Descriptive summary of studies reporting the predictor variables of non-prescribed drug use among pregnant women in Ethiopia included in the systematic review and meta-analysis, 2020.
Types of drugs used by pregnant women in Ethiopia
The most frequently consumed non- prescribed drugs by pregnant mothers were paracetamol 34.38% (95% CI: 16.46, 52.31), amoxicillin14.73% (95% CI: 1.54, 30.99), aspirin 4.25% (95% CI: 1.13, 8.64), metronidazole 2.81% (95% CI: 1.29, 5.34) and ciprofloxacin 2.80% (95% CI: 1.28, 5.35) ().
Table 4. A type of frequently consumed non-prescribed drug among pregnant women’s in Ethiopia, 2020.
Discussion
This study attempted to determine the pooled prevalence of non-prescribed drug use and predictors among pregnant women in Ethiopia. The study found that the overall prevalence of non-prescribed drug use among pregnant women in Ethiopia was 30.38%. This result is similar to a study conducted in low-and middle-income countries [Citation16] that reported a prevalence of 31.4% non-prescribed drug use among pregnant mothers. On the other hand, the prevalence of non-prescribed drug use observed in this study is slightly lower than the prevalence reported 38.46% in the systematic review and meta-analysis conducted in Iran [Citation53], 40% of the prevalence reported in the United Arab Emirates [Citation54] and 44% of the prevalence reported in Epidemiology of self-medication in Ethiopia: systematic review and meta-analysis of observational studies subgroup analysis [Citation55]. However, some studies reported a lower prevalence of non-prescribed drug use compared to the rate in our study. For example, in Nigeria [Citation56] the prevalence of non-prescribed drug use was found to be 19.6% and in Mexico [Citation57] 21.9%. Finally, the findings of the present study were higher than those of study on the prevalence of non-prescribed drugs use among pregnant women in developed countries, such as Portugal (26.2%) [Citation58], the Netherlands (12.5%) [Citation59] and Brazil (16.4%) [Citation60]. The potential reason for this disparity between the magnitudes of non-prescribed drug use prevalence in different areas of the world may be due to variations in over-the-counter drug practices and prescription policies in various countries. In some African countries, for example, all drugs can be obtained without a medical prescription [Citation16]. On the other hand, the other possible explanation for this disparity may be in developed countries and in some middle-income countries, there is a strict rule that no citizen can buy pharmacies without a physician’s prescription. Although most countries have legislation that states that they cannot buy medicines without a physician’s prescription, in countries such as Ethiopia, due to poor performance, it is common for pregnant mothers to buy medicines from pharmacies for any pregnancy-related illness. Finally, the reason for the current study prevalence is lower than the magnitude previously reported by a systematic review and Meta-analysis subgroup analysis portion in Ethiopia may be the difference in sample size. The prevalence of the current study has been reported by including 11 studies conducted among pregnant mothers. However, in the previous study, the magnitude of self-medication indicated in the subgroup analysis portion by including only three articles. As a result, there could be a big difference in sample size.
The sub-group analysis of this study reveals that the prevalence of non-prescribed drug use among pregnant women varies considerably across regions. The highest prevalence of non-prescribed drug use was observed in the Amhara Region, followed by the Oromia region, and the lowest prevalence was observed in the Addis Ababa and Tigray region. The reason for this is likely to be since Addis Ababa is the capital city of Ethiopia and the population of Tigray is smaller, mothers are more educated than others in Amhara and Oromia, and standard of maternal follow-up care is more available to regions that do not have a large number of mothers. They have a better understanding of the side effects of drugs taken during pregnancy, and mothers living in the capital are better off in terms of community wellbeing [Citation61]. Another reason for the relatively small amount of non-prescribed drug usage by pregnant mothers in the Tigray region is the small amount of research from the Tigray region included in this research. For the reasons described above, the number of pregnant women in the Amhara and Oromia regions who use non-prescribed drugs is higher than in Addis Ababa and Tigray.
In our study, the non-prescribed drugs commonly taken by women during pregnancy were paracetamol, amoxicillin, aspirin, metronidazole and ciprofloxacin. Studies in the Democratic Republic of Congo [Citation62] and Peru [Citation63] have reported similar findings, with paracetamol and amoxicillin being the most frequently used modern medicines among pregnant mothers. The possible explanation for this could be that these medicines have been obtained from pharmacies or drugstores. The use of over-the-counter painkillers is easy without prescription, as most pregnancy-related pain is associated with headaches and the cost of medicines is cheap [Citation61].
The current study demonstrated that there are important associations between non-prescribed drug use and previous maternal history of self-medication, maternal illness during pregnancy, and maternal marital status. In this study, the probability of non-prescribed drug use among pregnant mothers with a previous history of self-medication was approximately 3.21 times higher than among mothers with no history of non-prescribed drug use. This finding was consistent with previous studies in the Democratic Republic of Congo [Citation62], Iran [Citation64] and Nigeria [Citation65]. This may be due to the occurrence of maternal chronic illnesses, habitual drug use, pregnancy and childbirth complications, and poor awareness of non- prescribed drug use developmental risks [Citation51]. Another potential explanation may be that drugs are often used before pregnancy gives the illusion that over-the-counter medications can be used safely during pregnancy. A woman who has used medicine for mild illness can also take non prescribed medicine during pregnancy for any discomfort [Citation65].
The results of this study found that pregnant mothers who had a history of disease were 4.03 times more likely to use non-prescribed drugs than those who had no history of the disease. This is similar to other studies conducted in the Democratic Republic of Congo [Citation62]. This suggests that women who have any kind of health problems during pregnancy may have chosen non-prescribed drug use to save time and other related factors.
Finally, pregnant women who were single or divorced (no husband) were 2.97 times more likely to use non prescribed drugs than those who are married. The result of this finding is similar to that of previous research done in Nigeria [Citation56]. The possible justification for this may be that unmarried mothers may take drugs most of the time before they know they are pregnant due to increased symptoms of pregnancy-related pain. Another potential explanation why unmarried pregnant women often take non-prescribed drugs is that they do not interact with the public or physicians begin pregnancy and do not have adequate knowledge of the impact of non-prescription drugs during pregnancy.
Limitations of systematic review and meta-analysis
The results of this review should be interpreted with some limitations. All articles included in this systematic review and meta-analysis were cross-sectional in design. As a result, it is not possible to establish temporal associations between the factors and the outcome variables and may also be subject to recall biases. The high heterogeneity in the characteristics of the studies might lead to insufficient statistical power to detect significant association. Thus, a meta-regression analysis revealed that there was no variation due to sample size and publication year. Furthermore, given that this meta-analysis included accessible research from a small area in Ethiopia, the different regions of the country may be under-represented and some studies have small sample size, may affect the estimation.
Conclusions
The overall prevalence of non-prescribed drug use among pregnant Ethiopian women is relatively high and varies across different regions of Ethiopia. The non-prescribed drug commonly taken by women during pregnancy was paracetamol. Previous maternal history of self-medication, maternal illness during pregnancy, and maternal marital status were the predictors variable of non-prescribed drug use during pregnancy. It is therefore important to make pregnant women aware of the risks of non-prescribed drug use and to train health care providers on how to help pregnant women stay safe from non-prescribed drug use. In addition, coordinated efforts need to be made to enhance regulatory enforcement and identify early pregnant women. It is also essential to develop and/or update maternal and child health including policies, recommendations and ANC charts or forms relevant to the ANC system to resolve the risk of non-prescribed drug use activities. Finally, it is also suggested that the confirmatory investigation should be explored extensively on the specific types of drugs identified in this study, particularly on those most commonly consumed during pregnancy.
Authors’ contributions
FA: conceived and designed the study protocol, literature review, data extraction, data analysis, interpretation and wrote up the manuscript. FA, YM, & GS have extracted and analyzed the data, review and edit the manuscript. All authors read and approved the final manuscript.
| Abbreviations | ||
| ANC | = | Ante-natal Care |
| ADHD | = | attention-deficient hyperactive disorder |
| WHO | = | World Health Organization |
| IBCS | = | institution-based correctional studies and |
| CBCS | = | community based cross sectional study. |
Supplemental Material
Download MS Word (100 KB)Supplemental Material
Download MS Word (20 KB)Acknowledgements
We would like to express our gratitude and appreciation to all the staff of the Debre Markos University College of Medicine and Health Sciences who helped us in this study. We would like to acknowledge Pammla Petrucka (PhD, Professor), College of Nursing, University of Saskatchewan, Saskatoon) who helped in reviewing English and grammatical parts.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data are available from the manuscript.
References
- Organization WH. Guidelines for the regulatory assessment of medicinal products for use in self-medication. Geneva: World Health Organization; 2000.
- Souza LAF, Silva CDd, Ferraz GC, et al. The prevalence and characterization of self-medication for obtaining pain relief among undergraduate nursing students. Rev Latino-Am Enfermagem. 2011;19(2):245–251.
- Wakjira GB, Boru BG, Labata BG. Prevalence of self-medication and its associated factors among pregnant women attending antenatal care at Nekemte Referral Hospital, Oromia Regional State, West Ethiopia. J Bioanal Biomed. 2019;11:160–165.
- Domingues PHF, Galvão TF, Andrade KRCd, et al. Prevalence and associated factors of self-medication in adults living in the Federal District, Brazil: a cross-sectional, population-based study. Epidemiol Serv Saude. 2017;26(2):319–330.
- Sunny TP, Jacob R, Krishnakumar K, et al. Self-medication: is a serious challenge to control antibiotic resistance? Natl J Physiol Pharm Pharmacol. 2019;9(0):1–7.
- Seam M, Bhatta R, Saha B, et al. Assessing the perceptions and practice of self-medication among Bangladeshi undergraduate pharmacy students. Pharmacy. 2018;6(1):6.
- Afolabi A. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7(3):120–127.
- Fox J. Use of analgesics in self-medication. Therapie. 2002;57(2):115–118.
- Rizk MA, Abdel-Aziz F, Ashmawy A, et al. Knowledge and practices of pregnant women in relation to the intake of drugs during pregnancy. J Egypt Public Health Assoc. 1993;68(5–6):567–591.
- Bretagne J-F, Richard-Molard B, Honnorat C, et al. Gastroesophageal reflux in the French general population: national survey of 8000 adults. Presse Medicale. 2006;35(1):23–31.
- Branthwaite A, Pechère J-C. Pan-European survey of patients' attitudes to antibiotics and antibiotic use. J Int Med Res. 1996;24(3):229–238.
- Omolase C, Adeleke O, Afolabi A, et al. Self medication amongst general outpatients in a Nigerian community hospital. Ann Ibadan Postgrad Med. 2007;5(2):64–67.
- Almasdy D, Sharrif A. Self-medication practice with nonprescription medication among university students: a review of the literature. Arch Pharm Pract. 2011;2(3):95.
- Tesch BJ. Herbs commonly used by women: an evidence-based review. Am J Obstet Gynecol. 2003;188(5 Suppl):S44–S55.
- Sado E, Kassahun E, Bayisa G, et al. Epidemiology of self-medication with modern medicines among health care professionals in Nekemte town, western Ethiopia. BMC Res Notes. 2017;10(1):533.
- Adanikin AI, Awoleke JO. Antenatal drug consumption: the burden of self-medication in a developing world setting. Trop Doct. 2017;47(3):193–197.
- Eticha T, Mesfin K. Self-medication practices in Mekelle, Ethiopia. PLoS One. 2014;9(5):e97464.
- Jambo A, Mengistu G, Sisay M, et al. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar town. Front. Pharmacol. 2018;9:1063.
- Murray MD, Callahan CM. Improving medication use for older adults: an integrated research agenda. Ann Intern Med. 2003;139(5 Pt 2):425–429.
- Organization WH. How to develop and implement a national drug policy. Geneva: World Health Organization; 2001.
- Creanga AA, Sabel JC, Ko JY, Wasserman CR, et al. Maternal drug use and its effect on neonates: a population-based study in Washington State. Obstet Gynecol. 2012;119(5):924–933.
- Benjamin DM. Reducing medication errors and increasing patient safety: case studies in clinical pharmacology. J Clin Pharmacol. 2003;43(7):768–783.
- Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med. 1998;338(16):1128–1137.
- Nakhai-Pour HR, Broy P, Sheehy O, et al. Use of nonaspirin nonsteroidal anti-inflammatory drugs during pregnancy and the risk of spontaneous abortion. CMAJ. 2011;183(15):1713–1720.
- Yang T, Walker MC, Krewski D, et al. Maternal characteristics associated with pregnancy exposure to FDA category C, D, and X drugs in a Canadian population. Pharmacoepidemiol Drug Saf. 2008;17(3):270–277.
- Kureshee NI, Dhande PP. Awareness of mothers and doctors about drug utilization pattern for illnesses encountered during pregnancy. J Clin Diagn Res. 2013;7(11):2470.
- Irvine L, Flynn RW, Libby G, et al. Drugs dispensed in primary care during pregnancy: a record-linkage analysis in Tayside, Scotland. Drug Saf. 2010;33(7):593–604.
- Manyazewal T, Matlakala MC. Beyond patient care: the impact of healthcare reform on job satisfaction in the Ethiopian public healthcare sector. Hum Resour Health. 2017;15(1):10.
- Smolina K, Hanley GE, Mintzes B, et al. Trends and determinants of prescription drug use during pregnancy and postpartum in British Columbia, 2002-2011: a population-based cohort study. PLoS One. 2015;10(5):e0128312.
- Wilson JG. Present status of drugs as teratogens in man. Teratology. 1973;7(1):3–15.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–e34.
- Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011.
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634.
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101.
- Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560.
- Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39.
- Deeks JJ, Higgins JP, Altman DG. Analysing data and undertaking meta‐analyses. In: Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Hoboken (NJ): Wiley-Blackwell; 2008. p. 241–284.
- Fekadu G, Dugassa D, Negera GZ, et al. Self-medication practices and associated factors among health-care professionals in selected hospitals of western Ethiopia. PPA. 2020;14(353):353–361.
- Jember E, Feleke A, Debie A, et al. Self-medication practices and associated factors among households at Gondar town, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):153.
- Amaha MH, Alemu BM, Atomsa GE. Self-medication practice and associated factors among adult community members of Jigjiga town, Eastern Ethiopia. PLoS One. 2019;14(6):e0218772.
- Abay S, Amelo W. Assessment of self-medication practices among medical, pharmacy, and health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2(3):306–310.
- Gelayee DA. Self-medication pattern among social science university students in Northwest Ethiopia. J Pharm. 2017;2017:1–5.
- Abula T, Worku A. Self-medication in three towns of North West Ethiopia. Ethiopian J Health Dev. 2001;15(1):25–30.
- Abrha S, Molla F, Melkam W. Self-medication practice: the case of Kolladiba town, north West Ethiopia. Int J Pharma Sci Res. 2014;5(10):670–676.
- Mengesha E. Drug use and its associated factors among pregnant women in Bahir Dar city administration, northwest Ethiopia. Int J Sex Reprod Health Care. 2019;2(1):021–026.
- Mohammed MA, Ahmed JH, Bushra AW, et al. Medications use among pregnant women in Ethiopia: a cross sectional study. J Appl Pharm Sci. 2013;3(4):116.
- Zewdie T, Azale T, Shimeka A, et al. Self-medication during pregnancy and associated factors among pregnant women in Goba town, southeast Ethiopia: a community based cross sectional study. BMC Res Notes. 2018;11(1):1–6.
- Befekadu A, Dhekama NH, Mohammed MA. Self-medication and contributing factors among pregnant women attending antenatal care in Ethiopia: the case of Jimma University specialized hospital. Med Sci. 2014;3(1):969–981.
- Abeje G, Admasie C, Wasie B. Factors associated with self medication practice among pregnant mothers attending antenatal care at governmental health centers in Bahir Dar city administration, Northwest Ethiopia, a cross sectional study. Pan Afr Med J. 2015;20:276.
- Gebremedhin GL, Gomathi P. Assessment of drug use and effect in pregnant women attending antenatal care in hospitals of Mekelle, Tigray, Ethiopia. J Drug Delivery Ther. 2014;4(6):75–82.
- Beyene KG/M, Beza SW. Self-medication practice and associated factors among pregnant women in Addis Ababa, Ethiopia. Trop Med Health. 2018;46(1):10
- Kebede B, Gedif T, Getachew A. Assessment of drug use among pregnant women in Addis Ababa, Ethiopia. Pharmacoepidemiol Drug Saf. 2009;18(6):462–468.
- Rahmani A, Hamanajm SA, Fallahi A, et al. Prevalence of self-medication among pregnant women: a systematic review and meta-analysis. Nurs Midwifery Stud. 2019;8(4):169–175.
- Abduelkarem AR, Mustafa H. Use of over-the-counter medication among pregnant women in Sharjah, United Arab Emirates. J Pregnancy. 2017;2017:4503793.
- Sisay M, Mengistu G, Edessa D. Epidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studies. BMC Pharmacol Toxicol. 2018;19(1):56
- Bello FA, Morhason-Bello IO, Olayemi O, et al. Patterns and predictors of self-medication amongst antenatal clients in Ibadan, Nigeria. Niger Med J. 2011;52(3):153–157.
- Alonso-Castro AJ, Ruiz-Padilla AJ, Ruiz-Noa Y, et al. Self-medication practice in pregnant women from central Mexico. Saudi Pharm J. 2018;26(6):886–890.
- Paula Martins A, da Costa Miranda A, Mendes Z, et al. Self‐medication in a Portuguese urban population: a prevalence study. Pharmacoepidemiol Drug Saf. 2002;11(5):409–414.
- Verstappen GM, Smolders EJ, Munster JM, Aarnoudse JG, et al. Prevalence and predictors of over-the-counter medication use among pregnant women: a cross-sectional study in the Netherlands. BMC Public Health. 2013;13(1):185.
- Brum LFdS, Pereira P, Felicetti LL, et al. Utilização de medicamentos por gestantes usuárias do Sistema Único de Saúde no município de Santa Rosa (RS, Brasil). Ciência Saúde Coletiva. 2011;16:2435–2442.
- Adane F, Seyoum G, Alamneh YM, et al. Herbal medicine use and predictors among pregnant women attending antenatal care in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):1–11.
- Mbarambara PM, Songa PB, Wansubi LM, et al. Self-medication practice among pregnant women attending antenatal care at health centers in Bukavu, Eastern DR Congo. Int J Innov Appl Stud. 2016;16(1):38.
- Miní E. Self-medication in pregnant women attending the Maternal Perinatal Institute, Peru 201. Peru Rev Exp Med Public Health. 2012;29(2):212–217.
- Afshary P, Mohammadi S, Najar S, et al. Prevalence and causes of self-medication in pregnant women referring to health centers in southern of Iran. Int J Pharm Sci Res. 2015;6(2):612.
- Emmanuel A, Achema G, Afoi BB, et al. Self medication practice among pregnant women attending antenatal clinic in selected hospitals in Jos, Nigeria. Int J Nurs Health Sci. 2014;1(6):55–59.