Abstract
Objectives
The objectives of this study were to determine in a population-based cohort study the association between cesarean section (CS) during the second stage of labor and the risk for preterm birth and/or cervical insufficiency in the subsequent pregnancy; to identify maternal and neonatal risk factors for long-term complications following CS due to prolonged second stage of labor.
Methods
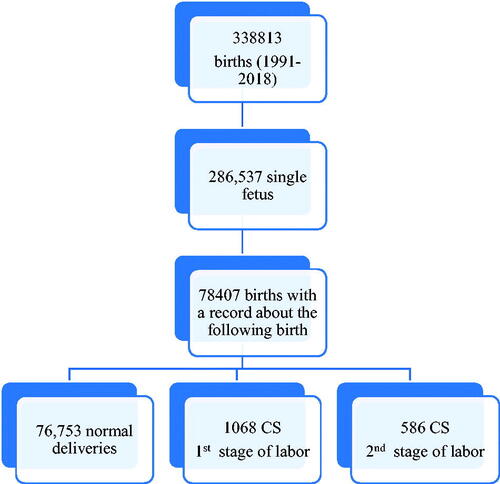
We conducted a retrospective population-based cohort study including women who had at least one consecutive delivery following a CS at our institution from 1991 to 2018, provided that the first delivery was at term. We divided the study cohort into two groups: (1) women who delivered by CS due to failure to progress during the first stage of labor (n = 1068); and (2) those who delivered by CS due to arrest of descent at the second stage of labor (n = 603).
Results
Of the 120,147 women who met the inclusion criteria, 78,407 had a subsequent delivery during the study period. Women of group 1 were significantly older than those of group 2 (p = .018), and had a higher rate of assisted reproductive technology [61 (5.7%) vs. 18 (3.1%), p < .022,]. Additionally, their hospitalization period was significantly longer (p < .001). The rate of preterm birth in the subsequent delivery was higher among women who had a CS due to arrest of descent than those who had a CS due to arrest in dilatation [43 (7.3%) vs 49 (4.6%), p < .026]. This was confirmed after adjusting for confounding factors In a multivariable regression analysis (OR 1.78, 95% CI 1.14–2.76, p value = .011) A Cox regression analysis implying gestational age at delivery at the time factor identifies CS due to arrest of descent as a risk factor for subsequent preterm birth (Hazard ratio 1.19 95% CI 1.07–1.31).
Conclusion
CS due to arrest of descent is an independent risk factor for subsequent preterm birth. The exact mechanisms contributing to this association are yet to be determined.
Synopsis
Cesarean section during the second stage of labor is an independent risk factor for late preterm birth in the subsequent pregnancy when compared to cesarean section in the first stage of labor.
Introduction
The second stage of labor is defined as the duration between complete cervical dilation and delivery of the neonate. Several factors are shown to affect the length of the second stage, such as parity, epidural anesthesia, maternal body mass index (BMI), and fetal head position [Citation1].
The duration of the second stage of labor regarded as within normal limits has become less stringent in recent years. The World Health Organization (WHO) recommended an upper limit of 2 h for parous women and 3 h in cases of nulliparous [Citation2]. As a part of a global effort to avoid the first CS, the American College of Obstetricians and Gynecologists (ACOG) stated that at least 2 and 3 h of pushing should be allowed in multiparous and nulliparous women, respectively, to define a second stage labor arrest [Citation3]. It should be noted that a prolonged second stage of labor does not stand alone as an indication for CS. Once the second stage becomes prolonged, clinical assessment of the women, fetus, and uterine contractile forces should also be considered to decide whether a CS is required [Citation4]. Nonetheless, CS rates are rising worldwide, despite the intent to reduce them, including those at full dilation (FDCS) [Citation5,Citation6].
Women delivered by CS due to arrest of descent are at higher risk of failure in a trail of labor in subsequent pregnancy and repeated CS due to this indication. However, recent evidence may suggest that cesarean delivery during the second stage carries an increased risk for other complications in subsequent pregnancies, such as preterm birth [Citation7,Citation8]. During the second stage of labor, it is hard to distinguish between the cervix and the lower uterine segment, increasing the risk that the uterine incision will be performed through the cervix rather than through the lower uterine segment [Citation9]. Thus, potential damage to the proximal vagina or uterine cervix may result in different degrees of cervical insufficiency in subsequent pregnancies. It has been previously reported that cervical injury during CS for the arrest of the second stage of labor may manifest in higher rates of spontaneous preterm delivery in subsequent pregnancies [Citation10–12]. Moreover, the rate of subsequent spontaneous preterm birth among women who had CS due to arrest at the second stage of labor was higher than the overall national USA spontaneous preterm rate and that of women who had CS due to arrest at the first stage of labor [Citation13].
The objectives of this study were to determine in a population-based cohort study the association between CS during the second stage of labor and the risk for preterm birth and/or cervical insufficiency in the subsequent pregnancy; to identify maternal and neonatal risk factors for long-term complications following CS due to prolonged second stage of labor.
Methods
We conducted between 1991 and 2018a retrospective population-based cohort study including all women who had at least one consecutive delivery following a primary CS at term, at the Soroka University Medical Center (SUMC). The SUMC is a tertiary referral hospital in which almost all the deliveries of the region takes place, reaching up to 17,000 deliveries annually in recent years.
Singleton live births were included in the study population. Women with a history of cervical manipulation (e.g. cone biopsy, cerclage), multiple gestations, elective CS, as well as cases of fetuses with chromosomal abnormalities and anatomical malformations were excluded from the study.
Exposure definition and study groups
Exposed study patients included women who were delivered by CS during labor in their index pregnancy (n = 1654). These patients were divided into two subgroups according to the stage in which CS was performed in the index pregnancy. Common indications for CS included labor dystocia, non reassuring fetal heart rate tracing, fetal malpresentation, and suspected fetal macrosomia. First-stage CS group (comparison) included women who were delivered by CS due to failure of progress at the first stage of labor (cesarean delivery at less than 10 cm dilation of the uterine cervix)(n = 1068). Second-stage CS group (study) included women who were delivered by CS due to arrest of descent at the second stage of labor (defined as cesarian delivery at 10 cm dilation of cervix) (n = 586). Arrest of descent of the second stage of labor was diagnosed in nulliparous women after 3 h without epidural anesthesia and 4 h with epidural anesthesia, while in multiparous women, it was diagnosed after 2 and 3 h, respectively (Gabbe’s Obstetrics: Normal and Problem Pregnancies 8th citation, Table 11.3). Deliveries are typically conducted with the help of a midwife under the supervision of an obstetrician, which intervenes under specific indications. Elective CS was defined as those scheduled in advance, as opposed to emergent CS indicated during labor.
Data regarding the subsequent pregnancy and labor were compared and analyzed. Alongside preterm births, we presented clinically meaningful maternal and neonatal outcomes.
Cervical insufficiency was defined as transvaginally cervical length ≤25 mm before 24 weeks of gestation [Citation14]. Gestational hypertension was diagnosed when blood pressure readings were higher than 140/90 mm\Hg in a woman who had normal blood pressure prior to 20 weeks of gestation. A body mass index (BMI) over 30 was considered obese. Cases with no recorded information about subsequent pregnancy and/or labor were also excluded. The institutional Helsinki committee of SUMC approved the study (IRB number is 0012-21-SOR).
Statistical analysis
Quantitative variables were described by mean ± standard deviation (SD) for normally distributed variables; medians, and interquartile range (IQR) for other distributions. Categorical variables were summarized by frequencies out of available cases. T-test was used for the comparison of normally distributed continuous variables and Mann–Whitney test for those not normally distributed; Chi-Square or Fisher Exact tests were used for the comparison of dichotomous variables. We performed a multivariable regression analysis to adjust for confounding factors. The regression analysis model included all factors found to be statistically significant in the univariate analysis and clinically relevant.
Results
Of the 120,147 women who met the inclusion criteria, 78,407 had subsequent births during the study period and included in the study cohort (), of them 76,753 (97.9%) women delivered vaginally or by elective CS, while 1068 (1.36%) had CS during first stage of labor, and 586 (0.74%) had CS during second stage of labor. Demographics, clinical and historical characteristics are presented in . Women delivered by CS due to labor dystocia at the first stage of labor had a higher mean maternal age than those who had a CS at the second stage of labor (p = .018). Parity-wise, at index labor, the vast majority were primiparous (given birth to one live baby), with more than 90% in both groups. The Multiparity rate was higher in the comparison group than in the study group (96, 9% and 36, 6%, respectively. p = .041). A higher rate of assisted reproductive technology (ART) pregnancies was recorded among the women of the comparison group compared to the study group (61, 5.7% vs 18, 3.1%, p < .022).
Table 1. Demographics, clinical, and historical characteristics.
presents information about subsequent pregnancy and labor. Pregnancy-related hypertension was more frequent in the first stage CS group; the rate of gestational hypertension and preeclampsia were higher in the comparison group than in the study group (p = .01 and p = .02, respectively). The mean hospitalization period was significantly longer (p < .001) in the comparison group (5.3 ± 2 days) than study group (5 ± 1.9 days). The subsequent preterm birth rate in the overall cohort was 5.5%. The rate of preterm birth in the second stage CS group was higher than that in the first stage CS group [43 (7.3%) vs. 49 (4.6%), p < .026]. Preterm premature rupture of the membranes (PPROM) rate did not differ between the two groups.
Table 2. Pregnancy and labor information.
The rate of repeated CS was higher among women who had the primary CS at the first stage than in those who had it during the second stage of labor [67.6% (722/1068) vs. 63.7% (367/586), p = .038 respectively], most of them were elective. repeated CS during the first stage of labor was more common among those who had CS at the first stage of labor in the index pregnancy (p < .001), and during the second stage of labor among those who had CS at the index pregnancy during the second stage (p < .001).
Date of neonatal outcomes in subsequent pregnancies are presented in . Mean birth weight, and rates of appropriate, large, and small for gestational age (AGA, LGA, SGA, respectively) were similar in the two study groups. The rate of persistent hypoglycemia was higher among neonates of women in the second stage CS group than those in first stage CS group [1.3% (8/586) vs. 0.4% (4/1068), p = .023]. Other neonatal outcomes such as Apgar score, cord PH, birth asphyxia, hypotonia and post-partum death during the first month of life did not differ between the study groups.
Table 3. Neonatal outcomes in subsequent labor.
We conducted a multivariable regression analysis including all factors which differ significantly between women who underwent CS during the first stage of labor and those who underwent CS in the second stage of labor (). The following factors were included- Age, LMS Social State Score, multiparous in index pregnancy, nulliparous in index pregnancy, infertility treatment, gestational hypertension, preeclampsia, CS in the following pregnancy. CS during the second stage of labor in the index pregnancy was independently associated with preterm labor in the subsequent pregnancy. The rate of cervical incompetency was higher among women who underwent CS during the second stage of labor. However, this variable is an outcome variable that supports our findings. Therefore, cervical incompetency was not included in the logistic regression model.
Table 4. Multivariable logistic regression—preterm birth in the following pregnancy adjusted for confounding factors.
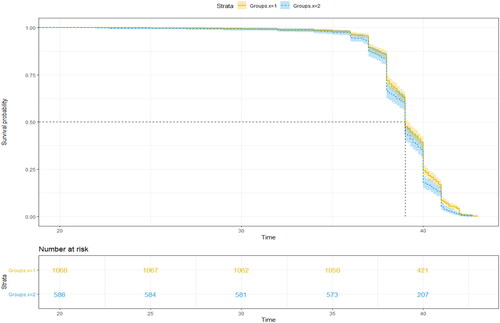
A Cox regression analysis was made with the purpose of evaluating the risk of subsequent preterm birth in women who underwent CS during the first stage of labor compared to those in the second stage. A Kaplan–Meier curve representing the survival analysis of preterm birth by the stage of labor in which CS was performed in the previous pregnancy is presented in . The curve implies that CS during the second stage of labor is a risk factor for subsequent preterm birth with a hazard ratio of 1.19 (95% CI 1.07–1.31). higher rates of preterm birth were observed in the study group after 34 weeks of gestation, suggesting that CS performed during the second stage of labor increases the risk of late preterm birth.
Discussion
Principal findings of the study
(1) Women who underwent CS during the second stage of labor are at higher risk of having late preterm delivery in the subsequent pregnancy. (2) Women who delivered by CS at the first stage of labor were older, with a history of ARTs, and suffered more in subsequent pregnancies from gestational HTN and preeclampsia compared to women in the second stage CS group. (3) Neonates of the study group had more persistence of hypoglycemia.
Cesarean delivery increases the risk for subsequent preterm birth. A meta-analysis by Zhang et al. included Ten cohort studies involving 10,333,501 women reported that a CS has an adjusted relative risk of 1.12 (95%CI 1.01–1.24) for preterm birth in the subsequent pregnancy [Citation15]. However, the authors did not differentiate between the stage of labor in which CS was performed and whether the premature birth was spontaneous or indicated. Studies hypothesized that CS during the second stage of labor might damage the cervix and the formation of uterine scar, causing permanent cervical insufficiency, manifested by preterm birth in following pregnancies [Citation9]. A recently published study examined subsequent pregnancy preterm birth rates in women who had a CS during the second stage of labor and compared it to a combined group of women who had a CS during the first stage of labor plus those who had a vaginal delivery [Citation16]. The adjusted odds ratio of spontaneous preterm birth before 37 weeks of gestation after second stage cesarean section was 2.4 (95%CI 1.2–4.8, p value = .01).
Our results demonstrate higher rates of late preterm birth in subsequent pregnancies following CS during the second stage than those performed during the first stage of labor. Prior reports suggested that CS during the second stage of labor was associated with an increased risk of subsequent preterm birth compared to vaginal delivery [Citation7,Citation8]. However, these studies demonstrated higher rates of very early preterm birth (before 32 gestational weeks). In the current study, this increase was attributed to higher rates of late preterm birth (34–36 + 6 gestational weeks). A possible explanation for this finding may be the tendency of clinicians to be more aggressive when managing an ART labor in order to monitor the delivery closely. Moreover, in our study, the index labor was not defined as the first labor of the women but could be the first, second, or, less commonly, third.
Cesarean birth is increasingly used for operative birth in the second stage of labor, with an accompanying reduction in attempted and successful assisted vaginal births [Citation17]. According to Wang et al. the risk of preterm birth in the subsequent pregnancy following second stage CS or mid-cavity instrumental delivery is 5.7% and 3.2%, respectively [Citation18]. The future consequences of CS during the second stage of labor should be considered when intervention is required during the second stage of labor.
In this retrospective study, we demonstrated that women who had pregnancies due to infertility treatments were more likely to undergo CS during the first stage of labor than in the second stage of labor. In the subsequent pregnancy, rate of elective CS, was similar within the groups. It has been previously demonstrated that pregnancies following ART are at higher risk of CS than pregnancies following spontaneous conceptions [Citation19]. This is true in both elective surgeries and those that are emergent and unplanned [Citation20,Citation21]. A possible explanation is that clinicians tend to deliver these women surgically in order to monitor the delivery process more closely.
Aligned with a study by Betgella et al. we found that neonates of mothers undergoing CS in the second stage of labor had a higher rate of neonatal hypoglycemia [Citation7]. This can be explained due to the higher rate of late preterm birth in this group. A study conducted in our center regarding the maternal and neonatal outcomes of patients with late preterm birth showed higher rates of composite neonatal outcomes among women delivering at late preterm [Citation22]. An additional explanation to the findings regarding the increased neonatal morbidity of neonatal hypoglycemia is our novel finding that women who had CS during the second stage also have a higher rate of early-term deliveries than those delivered by CS during the first stage of labor. Indeed, early-term delivery (37–38 + 6 weeks) carries higher neonatal morbidity compared with full-term (39–41 weeks) deliveries, including hypoglycemia, NICU admission, and need for respiratory support [Citation23,Citation24].
Our study carries several limitations, most of which are related to its retrospective nature. Firstly, preterm birth induced medically could not be excluded from the study’s database. This pitfall is shared by many large retrospectively collected databases, as pointed out by lam’s editorial suggesting [Citation25]. However, higher rates of preeclampsia and gestational HTN, both common indications for labor induction in preterm, were observed in women who underwent CS during the first stage of labor. These unexpected findings indicate that the difference in preterm birth rates between the study groups was masked; hence CS during the second stage of the labor may play an even more significant role than that suggested by the results in inducing preterm birth in subsequent pregnancies. Secondly, the study population includes nulliparous women as well as multiparous women, which may cause a potential selection bias [Citation26]. Lastly, we cannot rule out the possibility that a part of the cohort delivered subsequent pregnancies in other hospitals, thus not included in our study.
The study’s strengths include its large cohort of patients and the meticulous data collection on a comprehensive set of variables. Additionally, we present the possible impact of CS during the second stage of labor and higher rates of early-term births in subsequent pregnancies. Furthermore, while previous studies compared the preterm births rate of women who had CS during the second stage of labor to those who had vaginal deliveries, this study compares subsequent pregnancies’ preterm births rate of women who had CS during the first stage to those who had CS in the second stage of labor. We believe that this comparison methodology better addresses the hypothesis that CS at full cervical dilation and effacement, as opposed to CS at the first stage of labor, may be the cause of cervical damage and futural preterm births.
Conclusion
Term cesarean in the sconed stage of labor is associated with both higher rates of late preterm birth and early term birth in a subsequent pregnancy when compared to those performed in the first stage of labor. These findings may prompt further investigation to inform management of operative delivery in the second stage.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Piper JM, Bolling DR, Newton ER. The second stage of labor: factors influencing duration. Am J Obstet Gynecol. 1991;165(4 Pt 1):976–979.
- World Health Organization. WHO recommendations on intrapartum care for a positive childbirth experience. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO.
- American College of Obstetricians and Gynecologists. Dystocia and augmentation of labor. Obstet Gynecol. 2003;102:1445.
- Caughey AB, Cahill AG, Guise JM, et al. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Vousden N, Cargill Z, Briley A, et al. Caesarean section at full dilatation: incidence, impact and current management. Obstet Gynaecol. 2014;16(3):199–205.
- Unterscheider J, McMenamin M, Cullinane F. Rising rates of caesarean deliveries at full cervical dilatation: a concerning trend. Eur J Obstet Gynecol Reprod Biol. 2011;157(2):141–144.
- Berghella V, Gimovsky AC, Levine LD, et al. Cesarean in the second stage: a possible risk factor for subsequent spontaneous preterm birth. Am J Obstet Gynecol. 2017;217(1):1–3.
- Williams C, Fong R, Murray SM, et al. Caesarean birth and risk of subsequent preterm birth: a retrospective cohort study. BJOG. 2021;128(6):1020–1028.
- Koyama S, Tomimatsu T, Kanagawa T, et al. Cervical insufficiency following cesarean delivery after prolonged second stage of labor: experiences of two cases. J Obstet Gynaecol Res. 2010;36(2):411–413.
- Arbyn M, Kyrgiou M, Simoens C, et al. Perinatal mortality and other severe adverse pregnancy outcomes associated with treatment of cervical intraepithelial neoplasia: meta-analysis. BMJ. 2008;337:a1284.
- Wood SL, Tang S, Crawford S. Cesarean delivery in the second stage of labor and the risk of subsequent premature birth. Am J Obstet Gynecol. 2017;217(1):63–e1.
- Watson HA, Carter J, David AL, et al. Full dilation cesarean section: a risk factor for recurrent second‐trimester loss and preterm birth. Acta Obstet Gynecol Scand. 2017;96(9):1100–1105.
- Levine LD, Sammel MD, Hirshberg A, et al. Does stage of labor at time of cesarean delivery affect risk of subsequent preterm birth? Am J Obstet Gynecol. 2015;212(3):360.e1.
- American College of Obstetricians and Gynecologists and ACOG Practice Bulletin No. 142. Cerclage for the management of cervical insufficiency. Obstet Gynecol. 2014;123(2 Pt 1):372–379.
- Zhang Y, Zhou J, Ma Y, et al. Mode of delivery and preterm birth in subsequent births: a systematic review and meta-analysis. PLoS One. 2019;14(3):e0213784.
- Offringa Y, Paret L, Vayssiere C, et al. Second stage cesarean section and the risk of preterm birth in subsequent pregnancies. Int J Gynecol Obstet. 2022;159(3):783–789.
- Loudon JAZ, Groom KM, Hinkson L, et al. Changing trends in operative delivery performed at full dilatation over a 10-year period. J Obstet Gynaecol. 2010;30(4):370–375.
- Wang M, Kirby A, Gibbs E, et al. Risk of preterm birth in the subsequent pregnancy following caesarean section at full cervical dilatation compared with mid‐cavity instrumental delivery. Aust N Z J Obstet Gynaecol. 2020;60(3):382–388.
- Lodge-Tulloch NA, Elias FTS, Pudwell J, et al. Caesarean section in pregnancies conceived by assisted reproductive technology: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2021;21(1):1–13.
- Stojnic J, Radunovic N, Jeremic K, et al. Perinatal outcome of singleton pregnancies following in vitro fertilization. Clin Exp Obstet Gynecol. 2013;40(2):277–283.
- Tomic V, Tomic J. Neonatal outcome of IVF singletons versus naturally conceived in women aged 35 years and over. Arch Gynecol Obstet. 2011;284(6):1411–1416.
- Besser L, Sabag-Shaviv L, Yitshak-Sade M, et al. Medically indicated late preterm delivery and its impact on perinatal morbidity and mortality: a retrospective population-based cohort study. J Matern Fetal Neonatal Med. 2019;32(19):3278–3287.
- Sengupta S, Carrion V, Shelton J, et al. Adverse neonatal outcomes associated with early-term birth. JAMA Pediatr. 2013;167(11):1053–1059.
- Parikh LI, Reddy UM, Männistö T, et al. Neonatal outcomes in early term birth. Am J Obstet Gynecol. 2014;211(3):265–2e1.
- Iams JD. Late preterm birth: more and better data needed. Am J Obstet Gynecol. 2011;205(5):395.
- Israeli Centre Bureau of Statistics. Characterization and Classification of Geographical Units by the Socio-Economic Level of the Population; 2013.