Abstract
Objective
This study aimed to analyze the ultrasound characteristics of fetal congenital vertical talus (CVT) to provide a detailed basis for the prenatal diagnosis of CVT.
Methods
We retrospectively analyzed the ultrasonographic findings of fetuses with CVT confirmed by X-ray, surgery, or autopsy from 2010 to 2020. Clinical characteristics and ultrasonographic findings of CVT, including foot morphology, ossification center of the calcaneus and talus, associated deformities, and chromosomal test results, were recorded.
Results
Thirteen patients diagnosed with CVT by prenatal ultrasound were confirmed postpartum. Nine cases were bilateral, and four were unilateral. Under two-dimensional ultrasound, 13/13 cases had abnormal foot morphology, and 10 of 13 cases (76.9%) showed that the ossification center of the talus moved downward, and the calcaneus moved laterally. Under three-dimensional ultrasound, 11 cases (84.6%) presented a “rocking chair” appearance, and two cases did not obtain satisfactory three-dimensional image due to oligohydramnios and fetal position. In this group of cases, two cases (15.4%) were isolated CVT, and the other 11 cases (84.6%) were complicated with other abnormalities. Eleven cases of non-isolated CVT and 1 case of isolated CVT were induced, and another patient with isolated CVT had undergone postnatal surgery, which had been followed up for 8 years and recovered well.
Conclusions
The combination of fetal foot morphology, ossification center position of the calcaneus and talus, and three-dimensional ultrasound can provide a reliable diagnosis of CVT. Furthermore, we should pay more attention to the evaluation of other systemic and chromosomal abnormalities in CVT cases.
Introduction
Congenital vertical talus (CVT), commonly known as rocker bottom foot, is a relatively rare congenital foot deformity, with an incidence of 1 in 10,000 [Citation1,Citation2]. CVT is a rigid deformity with fixed vertical positioning of the talus, dorsal dislocation of the navicular bone with respect to the head and neck of the talus, midfoot dorsiflexion and forefoot abduction, resulting in the plantar convexity that earned the deformity its moniker [Citation3–5]. Approximately half of the CVT cases are often associated with malformations of other systems and chromosomal abnormalities. In particular, CVT is recognized as a marker for Trisomy 18 [Citation6,Citation7].
For prenatal ultrasound diagnosis of CVT, the current diagnostic approach is based on morphological changes in plantar prominence and forefoot dorsiflexion in a standard lateral view of the foot, partial or skewed images can lead to incorrect features or may even be misdiagnosed as clubfoot deformity [Citation8]. Thus, the judgment of foot morphology is subjective, and it is easy to be misdiagnosed. The postnatal standard of CVT diagnosis mainly relies on the observation of the position of the talus by radiography [Citation2,Citation9,Citation10]. However, whether prenatal ultrasound could be used to observe and assess the position of fetal talus has not been reported. Therefore, this study aimed to summarize the sonographic features of CVT to provide a detailed and objective basis for prenatal diagnosis of CVT.
Materials and methods
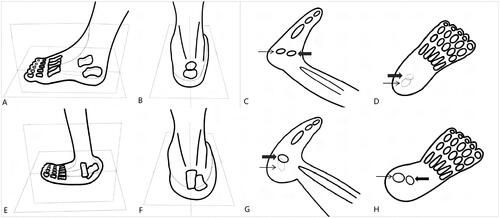
A retrospective study was performed in CVT cases retrieved from the picture archiving and communication system (PACS) database of our hospital from January 2010 to December 2020. The CVT cases diagnosed by ultrasound prenatally and confirmed by X-ray, surgery, or autopsy postnatally were included in our study. The ultrasonographic findings of CVT, including two-dimensional ultrasound foot morphology and ossification center of calcaneus and talus, as well as three-dimensional ultrasound images, were recorded. We further evaluated the location of the ossification center of the talus and the calcaneus in the sagittal and axial section when there was a suspicion of fetal foot anomalies, especially when abnormal fetal foot morphology was detected by two-dimensional ultrasound. The specific ultrasound examination method is shown in . In addition to the ultrasound images of fetal feet, maternal age, gestational age at the time of diagnosis, prenatally ultrasonic diagnosed associated anomalies, and genetic abnormalities were also retrieved. This retrospective study was approved by the Clinical Research Ethics Committee of our hospital.
Figure 1. Diagrams show the method to obtain detailed feet anatomic structures in sagital and axial sections in normal and CVT fetuses. (A, B) These figures show diagrams of ultrasound views of the talus and calcaneus ossification centers observed in the normal fetal foot, with sagittal and axial sections. (C, D) These figures respectively show the position of the talar and calcaneus ossification centers on the ultrasound image when a normal fetal foot is viewed in sagittal (C) and axial (D) views. (E, F) These figures show diagrams of ultrasound views of the talus and calcaneus ossification centers observed in the foot of a CVT fetus, with sagittal and axial views. (G, H) These figures respectively show the position of the talar and calcaneus ossification centers on the ultrasound image when a CVT fetal foot is viewed in sagittal (G) and axial (H) views (The ossification centers of the talus and calcaneus that cannot be shown on the ultrasound image section are indicated in light color, and those that can be observed are indicated in black. Bold arrow points to the talus, slim arrow points to the calcaneus).
Patients were scanned by two trained maternal-fetal medicine specialists with more than 10 years of experience in prenatal ultrasound. Ultrasound scans were performed using the Volusion E8/E10 Ultrasound Diagnostic Instrument (GE, Boston, MA, USA) with 4.0–8.0-MHz transabdominal transducers. Quantitative data are presented as median and range, and counting data are presented as percentage.
Results
Thirteen cases of 138,317 scanned fetuses were diagnosed with CVT by prenatal ultrasound in the second and third trimesters (median gestational age, 24.5 weeks; range, 20–29 weeks) and were confirmed postnatally over the study period between January 2010 and December 2020. Therefore, within our study population, the incidence was about 1 in 10,640. The clinical details of the 13 CVT cases are shown in . The median age of pregnant women was 31.5 years, with the oldest aged 42, and the youngest aged 21. Seven of these cases were male fetuses, and six were female, resulting in a male: female ratio of 7:6. All 13 fetuses were followed up, one case was liveborn, and 12 were terminated. The liveborn fetus with isolated CVT underwent X-ray examination and surgery after birth, and the others terminated were confirmed by autopsy.
Table 1. Clinical characteristics of the 13 CVT cases included in this study.
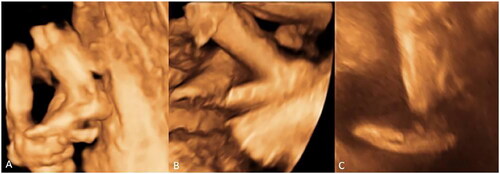
Observation of the foot, including the sagittal and axial sections, to observe the shape of the foot and the ossification center of the talus and calcaneus. As for the shape of the foot (), the sagittal section showed protuberant heel, convex plantar surface, and distal foot dorsiflexion; the axial section demonstrated obvious valgus heel. The calcaneus and talus were visible on two-dimensional ultrasound images in 10 cases, with a minimum gestational age of 23 weeks and 4 days. In these cases, the ossification center of the calcaneus and talus had lost the normal above and below parallel position relationship. As the calcaneus is valgus, we can only observe the talus in the mid-sagittal section. In the axial view, due to the downward movement of the talus, the calcaneus and talus can be displayed on the same section (). In the other three cases, the ossification center of the bone was not observed due to the small gestational age. Additionally, 11/13 cases had undergone three-dimensional ultrasound foot morphology imaging, which showed the plantar bulging, the heel protruding, the arch missing, and a shape like a rocking chair morphology (). For the other two cases, satisfactory three-dimensional images were not obtained due to oligohydramnios or fetal position.
Figure 2. A morphological comparison of normal foot and foot of a fetus with CVT by prenatal ultrasound. (A, B) The prenatal ultrasound images of the foot of a fetus with CVT in the sagittal (A) and axial (B) sections. (A) A longitudinal scan of the foot sagittal section shows protuberant heel, convex plantar surface, and distal foot dorsiflexion; (B) A transverse scan of the foot axial section shows obvious valgus heel. (C, D) The prenatal ultrasound images shows the normal fetal foot of a normal fetus in the sagittal (C) and axial (D) sections.
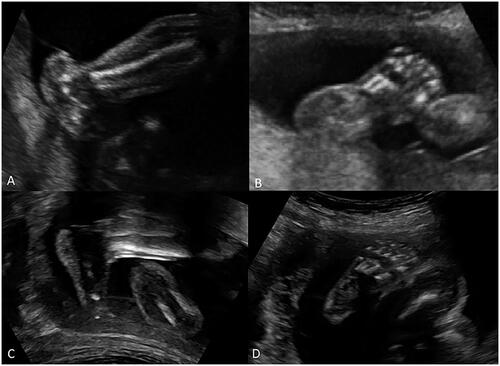
Figure 3. Comparison of normal foot and foot of a fetus with CVT in the location of calcaneus and talus ossification center by prenatal ultrasound. (A, B) The images show abnormal prenatal ultrasound images of the foot location of the calcaneus and talus ossification center with CVT in the sagittal (A) and axial (B) sections. (A) A longitudinal scan of the foot sagittal section shows the calcaneus is valgus, only the talus is shown in the image. (B) A transverse scan of the foot axial section shows the calcaneus and talus are shown on the same section due to the downward movement of the talus. (C, D) The images show normal prenatal ultrasound images of the foot location of calcaneus and talus ossification center in the sagittal section (C) and axial section (D). (C) A longitudinal scan of the foot sagittal section shows the talus is located above the calcaneus. (D) A transverse scan of the foot axial section shows the sole of normal foot only presented soft tissue echoes, due to the presence of normal arch structure (Bold arrow points to the talus, slim arrow points to the calcaneus).
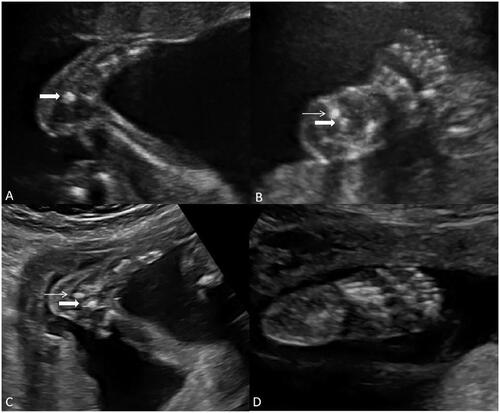
Figure 4. Comparison of the normal foot and foot of a fetus with CVT by three-dimensional ultrasound. (A) The image shows the normal foot of a fetus using three-dimensional ultrasound. (B, C) The images show “rocking chair” morphology in fetuses with CVT under three-dimensional ultrasound.
There were nine cases of bipedal CVT (69.2%) and four unilateral CVT (30.8%). Among these unilateral CVT cases, three had contralateral foot abnormalities, including two cases with congenital talipes equinovarus and one with absence of foot. Additionally, the only twins in 13 cases showed only one fetus with CVT, whereas the other had normal feet. In this group of cases, two (15.4% CVT cases) were isolated CVT, and the other 11 (84.6% CVT cases) were complicated with other abnormalities. The associated malformations included nervous system anomalies (46.2% of CVT cases), skeletal anomalies (53.8% of CVT cases), cardiac defects (30.8% of CVT cases), facial abnormalities (23.1% of CVT cases), other major anomalies (23.1% of CVT cases), chromosomal anomalies (33.3% of CVT cases), and other findings (38.5% of CVT cases) (). The combined malformations of CVT are summarized in .
Figure 5. The ultrasound images of associated malformations in CVT fetuses. (A) The image shows arthrogryposis multiplex congenita. The lower limbs of the fetus were crossed, and the knee joints were stiff and cannot be bent. (B) The image shows hooks (ulnar radius dysplasia). (C) The image shows Dandy–Walker syndrome. (D) The image shows a congenital cataract.

Table 2. The associated malformations observed in the CVT cases.
We obtained chromosomal results in 6/13 cases, of which two were abnormal (33.3%), including one case of Trisomy 13 and one of Trisomy 18. There was no family history of the disease in the two cases. Both cases of chromosomal abnormalities combined with other structural abnormalities.
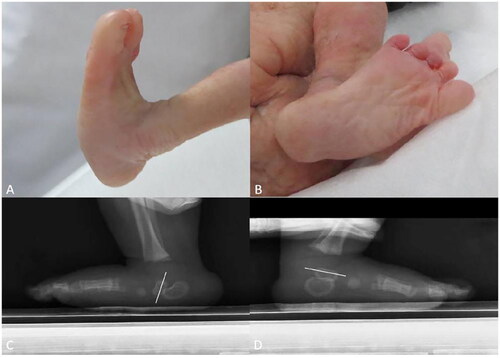
In 12 cases of induced labor, each foot of fetuses with CVT had rigid convex plantar surface, creating a rocker-bottom deformity. Additionally, the forefoot was abducted in dorsiflexion at the midtarsal joint, and the hindfoot was in fixed equinovalgus (). One case with isolated CVT received operation after birth. Lateral X-ray showed that the long axis of the talus of the affected foot was almost perpendicular to the ground, and the talus of the contralateral normal foot was located above the calcaneus, with the long axis nearly parallel to the ground (). The operation was performed 4 months after birth. The patient was followed up to 8 years after birth and recovered well.
Figure 6. Foot images of a fetus with bilateral CVT, and X-ray images of a fetus feet with unilateral isolated CVT. (A, B) The images show the gross specimen of a fetus with bilateral CVT after induction. (A) The image shows CVT fetus with convex plantar surface, and the hindfoot was in fixed equinovalgus, forming a rocker-bottom foot deformity. (B) The image shows the forefoot was abducted in dorsiflexion. (C, D) The images show bipedal X-ray comparison of a three-month-old child with unilateral CVT. (C) The long axis of the left talus is almost perpendicular to the ground. (D) The long axis of the right talus is almost parallel to the ground (The white line shows the long axis of the talus).
Discussion
CVT is a rare bone condition characterized by unusual congenital foot deformity. The etiology of CVT is unclear, but some studies suggested that it is caused by an incomplete explicit autosomal dominant gene or mutations of the genes HOXD10 or GDF5, which are associated with early limb development [Citation11,Citation12]. The deletion of the TSHZ1 gene has also been related to an isolated CVT [Citation11–14]. There are also other theories such as vascular defects of the lower limbs, muscle force imbalance due to increased intrauterine pressure or fetal growth arrest occurring during the 7th–12th weeks of gestation [Citation14–17]. As the literature reported, isolated CVT accounts for approximately half of the CVT cases, while the rest are associated with neuromuscular abnormalities and genetic diseases [Citation8,Citation18,Citation19]. In our study, there were only two cases of isolated CVT, accounting for approximately 15.4% of CVT cases, which is much lower than the prevalence reported in the previous literature [Citation9,Citation19]. There is no consensus on gender distribution, and the gender ratio of cases in our study is close to 1:1 [Citation2,Citation3,Citation20].
Currently, the prenatal diagnosis of CVT was based on the foot morphology on two-dimensional and three-dimensional ultrasound images. So far, Rubio EI et al.’s study, which is the largest sample size of published study for prenatal diagnosis of CVT, was also based on fetal foot morphology abnormalities [Citation8]. This method of diagnosis is too subjective to be accurate and difficult to use in distinguishing from other foot deformities, such as calcaneovalgus foot, flexible flatfoot, congenital talipes equinovarus, and metatarsus adductus. The diagnosis of CVT postnatally mainly depends on clinical diagnosis and radiological evaluation. The clinical diagnosis was mainly based on rigid hind foot valgus and forefoot dorsiflexion abduction. On the neutral lateral view, the long axis of the talus is vertical in relation to the first metatarsal, and the calcaneus is in significant equinus () [Citation2,Citation9,Citation10]. However, the use of ultrasound in evaluating the fetal foot bone ossification for the prenatal diagnosis of CVT has not been reported. To the best of our knowledge, this is the first study to use ultrasound to evaluate the location of fetal talus and calcaneus ossification centers in different planes for the prenatal diagnosis of CVT. Moreover, the observation of the calcaneus and talus in fetuses with abnormal foot morphology is helpful to distinguish it from other diseases.
The calcaneovalgus foot and most flexible flatfoot do not have significant skeletal deformities but mainly soft tissue abnormalities; therefore, there are no abnormalities in the position of the talus and calcaneus. Although there are skeletal deformities in congenital talipes equinovarus and metatarsal adductus, there are no abnormalities in the position of the talus and calcaneus. Therefore, the observation of the calcaneus and talus ossification center using two-dimensional ultrasound to diagnose CVT is theoretically-based and feasible. This anatomic position-based method of prenatal ultrasound diagnosis is closer to the standard of postpartum CVT diagnosis to avoid prenatal misdiagnosis. In previous study, Goldstein et al. [Citation21] found that the calcaneus ossification center could be shown in ultrasound images after 18 weeks and the talus ossification center could be shown after 22 weeks in 223 healthy pregnant women who underwent routine ultrasound examinations, which is consistent with our study. It also suggested that the use of ossification centers for the diagnosis of CVT in earlier gestational weeks is limited.
Three-dimensional ultrasound also plays an important role in auxiliary diagnosis. We used three-dimensional surface imaging technology to vividly display the unique shape of the fetal foot, which is conducive to enhancing the diagnostic confidence and facilitating better communication with the patient.
Because of the high probability of CVT merging with other related anomalies, it is important to examine other systems. Compared with previous reports on prenatal diagnosis of CVT, most associated abnormalities discovered by ultrasound were nearly similar. Our study differs slightly from previous studies in several respects. Fetal intracranial nervous system malformations are the most severe combined malformations, with an incidence of 46.2% in this study, which was slightly lower than that reported in the literature (62.5%) [Citation8]. Both studies demonstrated that brain abnormalities are the most severe finding associated with CVT. Moreover, skeletal malformations (53.8%) also account for a high proportion, with the highest percentage in our study. Some common associated malformations, such as clubfoot, arthrogryposis multiplex congenita, Dandy–Walker syndrome, and spina bifida, were also found in our study () [Citation8]. We also found many other combined malformations that had not been previously reported in the literature, such as congenital cataract, microtia and low-set ears, unilateral hydronephrosis, congenital cystic adenomatoid malformation, and esophageal atresia [Citation1,Citation3,Citation8,Citation18,Citation22–25]. CVT is usually associated with chromosomal abnormalities, such as trisomy 13, trisomy 15, and trisomy 18, which is consistent with our study results [Citation8,Citation18,Citation25]. The fetuses with chromosomal abnormalities in this study all had other structural abnormalities.
The prognosis of CVT depends on whether it has other structural abnormalities and chromosomal abnormalities. For isolated CVT, a combination of plaster and surgery is often required after birth, and most children can obtain imaging reduction and flexible ankle function [Citation26–30]. The early diagnosis and timely treatment allowed most patients to achieve restoration of flexibility in the foot and ankle. In this study, one case of chromosomal normal isolated CVT fetus had undergone surgical treatment when the patient was 4 months old and recovered well until now.
The advantage of this study is that we first proposed the use of prenatal ultrasound in determining the location of the fetal calcaneus and talus ossification center to diagnose CVT, which is of great significance for accurate prenatal diagnosis. This method is close to the diagnosis criteria of radiological examination postnatally, which is very helpful for the differential diagnosis of fetal foot abnormalities. Our study also has some limitations. Since this is a retrospective study, we only included cases of CVT diagnosed prenatally and confirmed after birth. Therefore, no further statistical analysis of diagnostic experiments can be performed. Additionally, we cannot assess whether a fetus with CVT that has not formed a calcaneus and talar ossification center before 23 weeks of pregnancy through the location of the ossification center, and observation is also limited in late-trimester fetuses because the ossification center forms an acoustic shadow.
Conclusions
CVT can be diagnosed by combining the observation of the fetal foot shape and the positional relationship between the calcaneus and the talus ossification center. In addition, attention should be paid to other structure malformations and chromosome abnormalities in the prenatal detection of CVT.
Ethics approval and consent to participate
This study was approved by the Clinical Research Ethics Committee of our hospital, and written informed consent was obtained.
Authors’ contributions
YX was responsible for the original draft preparation and editing. YQW, FJH, YXZ, YTW and WS participated in collecting the data and were major contributors during the writing of the manuscript. BW and LZC were responsible for conceptualization, manuscript editing, and reviewing the manuscript. All authors read and approved the final manuscript.
Acknowledgments
We thank the patients and their family for providing medical records and allowing us to report this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Availability of data and materials
The data analyzed during this study are included in the tables in this published article. The datasets used during the current study are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Benard MA. Congenital vertical talus. Clin Podiatr Med Surg. 2000;17:471–480.
- Miller M, Dobbs MB. Congenital vertical talus: etiology and management. J Am Acad Orthop Surg. 2015;23:604–611.
- Hamanishi C. Congenital vertical talus: classification with 69 cases and new measurement system. J Pediatr Orthop. 1984;4:318–326.
- Thometz JG, Zhu H, Liu XC, et al. MRI pathoanatomy study of congenital vertical talus. J Pediatr Orthop. 2010;30:460–464.
- Violas P, Chapuis M, Tréguier C, et al. Ultrasound: a helpful technique in the analysis of congenital vertical talus: a case report. J Pediatr Orthop B. 2006;15:70–72.
- Kruse L, Gurnett CA, Hootnick D, et al. Magnetic resonance angiography in clubfoot and vertical talus: a feasibility study. Clin Orthop Relat Res. 2009;467(5):1250–1255.
- Yassir WK, Grottkau BE, Goldberg MJ. Costello syndrome: orthopaedic manifestations and functional health. J Pediatr Orthop. 2003;23:94–98.
- Rubio EI, Mehta N, Blask AR, et al. Prenatal congenital vertical talus (rocker bottom foot): a marker for multisystem anomalies. Pediatr Radiol. 2017;47:1793–1799.
- Arbab D, Rath B, Quack V, et al. Vertical talus: current diagnostic and therapy options. ]. Orthopade. 2013;42:402–408.
- Alaee F, Boehm S, Dobbs MB. A new approach to the treatment of congenital vertical talus. J Child Orthop. 2007;1:165–174.
- Dobbs MB, Gurnett CA, Pierce B, et al. HOXD10 M319K mutation in a family with isolated congenital vertical talus. J Orthop Res. 2006;24:448–453.
- Dobbs MB, Gurnett CA, Robarge J, et al. Variable hand and foot abnormalities in family with congenital vertical talus and CDMP-1 gene mutation. J Orthop Res. 2005;23:1490–1494.
- Coré N, Caubit X, Metchat A, et al. Tshz1 is required for axial skeleton, soft palate and Middle ear development in mice. Dev Biol. 2007;308(2):407–420.
- Alvarado DM, McCall K, Hecht JT, et al. Deletions of 5’ HOXC genes are associated with lower extremity malformations, including clubfoot and vertical talus. J Med Genet. 2016;53:250–255.
- Drennan JC, Sharrard WJ. The pathological anatomy of convex pes valgus. J Bone Joint Surg Br. 1971;53(3):455–461.
- Silvani SH. Congenital convex pes valgus. The condition and its treatment. Clin Podiatr Med Surg. 1987;4:163–173.
- Wirth T, Schuler P, Griss P. Early surgical treatment for congenital vertical talus. Arch Orthop Trauma Surg. 1994;113:248–253.
- Merrill LJ, Gurnett CA, Connolly AM, et al. Skeletal muscle abnormalities and genetic factors related to vertical talus. Clin Orthop Relat Res. 2011;469:1167–1174.
- McKie J, Radomisli T. Congenital vertical talus: a review. Clin Podiatr Med Surg. 2010;27:145–156.
- Wirth T. Congenital vertical talus. Foot Ankle Clin. 2021;26:903–913.
- Goldstein I, Reece EA, Hobbins JC. Sonographic appearance of the fetal heel ossification centers and foot length measurements provide independent markers for gestational age estimation. Am J Obstet Gynecol. 1988;159(4):923–926.
- Angsanuntsukh C, Oto M, Holmes L, et al. Congenital vertical talus in multiple pterygium syndrome. J Pediatr Orthop. 2011;31:564–569.
- Fornaciari P, Gilgen A, Zwicky L, et al. Isolated talonavicular fusion with tension band for Müller-Weiss syndrome. Foot Ankle Int. 2014;35:1316–1322.
- Dodge LD, Ashley RK, Gilbert RJ. Treatment of the congenital vertical talus: a retrospective review of 36 feet with long-term follow-up. Foot Ankle. 1987;7:326–332.
- Cho BC, Lee IH, Chung CY, et al. Undercorrection of planovalgus deformity after calcaneal lengthening in patients with cerebral palsy. J Pediatr Orthop B. 2018;27:206–213.
- Dobbs MB, Purcell DB, Nunley R, et al. Early results of a new method of treatment for idiopathic congenital vertical talus. J Bone Joint Surg Am. 2006;88:1192–1200.
- Aydın A, Atmaca H, Müezzinoğlu ÜS. Bilateral congenital vertical talus with severe lower extremity external rotational deformity: treated by reverse Ponseti technique. Foot. 2012;22:252–254.
- Eberhardt O, Fernandez FF, Wirth T. The talar axis-first metatarsal base angle in CVT treatment: a comparison of idiopathic and non-idiopathic cases treated with the Dobbs method. J Child Orthop. 2012;6:491–496.
- Eberhardt O, Wirth T, Fernandez FF. Minimally invasive treatment of congenital foot deformities in infants: new findings and midterm-results. Orthopade. 2013;42:1001–1007.
- Aslani H, Sadigi A, Tabrizi A, et al. Primary outcomes of the congenital vertical talus correction using the Dobbs method of serial casting and limited surgery. J Child Orthop. 2012;6:307–311.
