Abstract
Introduction
Prenatal diagnosis and counseling of isolated ventriculomegaly (VM) represent a considerable challenge. We aimed to analyze the intrauterine evolution, associated anomalies, and neurodevelopmental outcome using the Battelle Development Inventory (BDI) of fetuses with an initial diagnosis of isolated mild VM.
Material and methods
Retrospective cohort study of fetuses diagnosed with mild isolated VM (10 -12 mm) between 2012 and 2016 in a tertiary hospital. In 2018, parents were invited to complete the structured BDI test for the neurodevelopmental evaluation of their children in five domains (personal-social skills, adaptive behavior, psychomotor ability, communication, and cognition). Results exceeding two standard deviations were considered abnormal and referred to an expert neuropediatrician.
Results
We identified 43 cases of mild isolated VM. In 5 (11%), structural abnormalities were detected during prenatal follow-up, being related to non-regressive forms (p = .01) and bilateral VM (p = .04). The BDI test was completed by 19/43 (44%). The global score was abnormal in 10/19 (53%). Of them, the neuropediatrician confirmed a neurodevelopmental delay solely in 3 cases that had already been diagnosed with neurological disorders. The most affected domains were gross motor skills (63%), personal-social (63%), and adaptive domains (47%). Communicative and cognitive areas were abnormal in 26% of cases.
Conclusion
In fetuses with isolated mild VM detected in the second half of pregnancy, 53% had an abnormal BDI test at 2–6 years, but a neurological disorder was only confirmed in the 30% of them.
Introduction
Ventriculomegaly (VM) is the most common central nervous system anomaly diagnosed in fetal life. Its prevalence varies between 0.3 and 1.5 per 1,000 births [Citation1,Citation2]. VM can appear isolated or associated with other congenital abnormalities such as structural malformations (33–61%), chromosomal aberrations (3–9%), or congenital infections (5%). Non-isolated cases tend to have a poorer prognosis [Citation3,Citation4].
Prenatal diagnosis of isolated VM represents a considerable challenge when counseling about the impact of this anomaly on the neurodevelopment of the newborn [Citation5,Citation6]. Firstly, parents should be warned that this is a provisional diagnosis, and in about 13% of cases, other major brain defects cannot be initially identified. In addition, ventricular dilatation progression occurs in 16% of cases, which may worsen the postnatal prognosis [Citation7]. Secondly, the natural history of isolated VM is poorly understood, with very little information on long-term neurological outcomes [Citation8–10]. Finally, few studies have assessed which prenatal and postnatal ultrasound parameters are associated with adverse outcomes [Citation11–13].
Therefore, there is a need to better understand which fetuses have a higher risk of presenting associated abnormalities or worse neurological outcomes using prenatal parameters to provide adequate prenatal management and accurate prognostic information. This could help provide better postnatal follow-up and early interventions to improve the neurodevelopment of these children.
The objectives of this article are to analyze the natural history, the rate of associated anomalies, and the postnatal neurodevelopmental outcomes using the Battelle Development Inventory (BDI) of fetuses with an initial prenatal diagnosis of isolated mild fetal VM.
Materials and methods
Study population
This was a retrospective study undertaken at a tertiary care referral center. Our database was queried for cases of prenatally diagnosed VM between 2012 and 2016.
We selected all cases which fulfilled the following inclusion criteria: (a) ultrasound measurement of one or both lateral ventricles between 10–12 mm at initial diagnosis, (b) absence of fetal abnormalities at the initial assessment, (c) normal karyotype confirmed either prenatally or postnatally, and (d) no evidence of maternal or fetal infections ().
Figure 1. Flow chart of the study population. TOP: termination of pregnancy; IUFD: intrauterine fetal death; CNS:central nervous system.
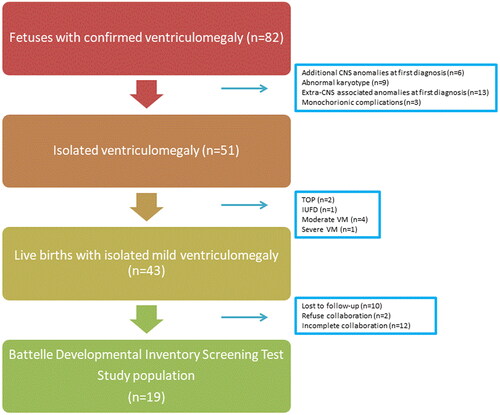
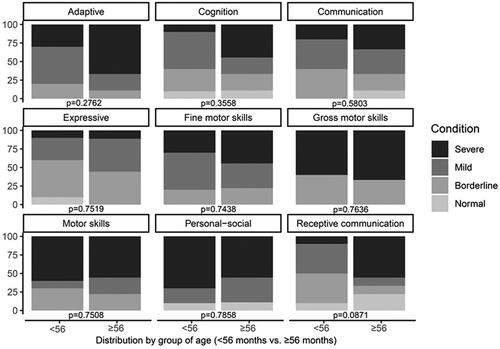
Figure 2. Distribution of neurodevelopmental outcomes assessed by the Battelle Development Inventory (BDI) by group of age (< 56 months vs. ≥ 56 months).
Exclusion criteria were moderate and severe ventriculomegaly at the initial assessment, stillbirths, terminated pregnancies, multiple pregnancies complicated by twin-to-twin-transfusion syndrome, or selective intrauterine growth restriction and loss to follow-up.
Maternal clinical data were obtained from medical records. Socioeconomic status was established according to the income level of each patient as reflected by their economic contribution to pharmaceutical benefits. The study was approved by the local ethics committee (ref. N°18/405). Parents were contacted and invited to participate in the postnatal follow-up, for which there was a separate informed consent form.
Fetal ultrasound
Mild ventriculomegaly was defined as a transverse diameter of one or both ventricular atria between 10–12 mm. According to current recommendations, sonographic measurements of lateral ventricles were obtained in the axial plane [Citation14]. Additionally, an advanced neurosonographic exam and a thorough sonographic evaluation of the rest of the fetal morphology were performed. Ongoing pregnancies underwent serial fetal sonographic examinations every 4–6 weeks to detect the progression of ventricular dilation and/or additional structural abnormalities. Fetal medicine specialists performed each of the examinations. VM was defined as resolved if the ventricular diameter returned to less than 10 mm during the ultrasound follow-up, persistent if it remained stable within 2 mm from the initial assessment, and progressive if it increased by ≥ 2 mm. Karyotype analysis and TORCH analysis were offered.
Fetal magnetic resonance imaging (MRI)
Fetal MRI was offered in those cases in which the presence of associated CNS abnormalities was suspected, or persistence or progression of VM on ultrasound was noted. A fetal MRI was performed using a 1.5-Tesla system (Philips Achieva). Measurements were obtained at the level of the atrium, on the axial plane, where both the posterior aspects of the basal ganglia and the third ventricle were visible [Citation15].
Postnatal outcome
A general clinical and neurological evaluation was carried out by a neonatologist and a pediatric neurologist in the first week of life, as well as a cerebral transfontanellar ultrasound (TF-US) performed by a pediatric radiologist, to confirm the prenatal diagnosis regardless of the intrauterine evolution of the VM. This protocol was similar for all centers.
In our center, the outpatient follow-up protocol was made by a specialized neuropediatrician. It consisted of, first, a clinical evaluation including a complete physical and neurological examination, measurement of head circumference, and evaluation of psychomotor development by exploring the acquisition of the main neurological landmarks at 1, 3, 6, 12, 18 and 24 months of age. Second, the completion of a TF-US on each visit provided that the fontanels remained open. Finally, MRI was requested whenever there was progression of VM or when the clinical examination revealed either psychomotor delay or neurological deficits. If each of these tests revealed normal results, the infant was discharged. Otherwise, the patient remained under specialized surveillance. For children that were referred from distant areas of our country, delivery took place at their local centers and a similar follow up was undertaken.
Neurodevelopmental evaluation
Information on the neurological development of the patients included in the study was obtained by consulting their medical records and by applying validated developmental tests.
Thus, psychomotor development was examined by using the BDI. The complete BDI has three administration formats (structured administration, observation, and interviews with parents) and can be used either as a standalone test or as an additional tool to acquire information [Citation16]. Since most of our patients were referred from distant areas of our country, we obtained all data from telephone interviews with the parents and the completion of a questionnaire sent by ordinary mail.
Briefly, complete BDI is a widely used clinical tool for assessing critical developmental skills in children from 6 months to 8 years of age. It is comprised of 341 age-specific items to evaluate the following five domains: personal-social skills, adaptive behavior, psychomotor ability (including fine motor and gross motor skills), communication (including receptive communication and expressive communication), and cognition. Mean and standard deviations (SD) from the scores in each domain are calculated to classify patients either as normal, borderline (<1 SD below the mean), mild delay (1–2 SD), or severe delay (< 2 SD) [Citation17]. This questionnaire has been validated to be applied in Spanish [Citation18].
BDI was applied at the end of 2018 when all were at least 24 months of age. The mean age of the infants at the time of the neurodevelopment evaluation with BDI was 56 months, so the study population was subclassified into two homogenous groups according to the age at which BDI was applied (<56 months vs.≥56 months) for further comparisons.
All patients that completed the BDI were contacted by the neuropediatrician and neuropsychologist, who made a structured telephone consultation to evaluate the veracity of the data, the current status of the patient, the functionality in terms of school performance, and personal autonomy according to their age. Those with high neurological risk were asked for in-person consultations to conduct a more specific neurological and neurocognitive examination. A follow-up consultation was scheduled when necessary.
We analyzed the neurological impact of prenatal variables which might be associated with the outcome of isolated mild VM, such as gestational age at diagnosis, fetal sex, unilateral or bilateral ventricular dilatation, intrauterine evolution of VM, and associated abnormalities.
Statistical analysis
A descriptive study of the different pre- and postnatal variables, as well as a univariate analytical analysis of the relationship of the gestational age at diagnosis, fetal sex, unilateral or bilateral ventricular dilatation, intrauterine evolution of VM and associated abnormalities with the neurodevelopmental outcome, was carried out. Continuous variables were presented as mean (SD) or median (interquartile range) when non-normally distributed. Categorical variables were presented as n (%). Statistical significance (p < .05) was determined by Kruskal-Wallis test for continuous variables and by Fisher’s exact tests for categorical variables. Data were analyzed using SPSS software, version 20.0 (SPSS, Chicago, Ill., USA).
Results
During the study period, there were 82 cases of VM. Of them, 39 were excluded due to: additional CNS anomalies (n = 6) or extra-CNS associated anomalies (n = 13) already present at the first diagnosis, abnormal genetic testing (n = 9), monochorionic complications (n = 3), termination of pregnancy (n = 2), intrauterine fetal death (n = 1), moderate VM (n = 4) and severe VM (n = 1). A flow chart is shown ().
The study sample comprised 43 fetuses with mild isolated VM at the initial assessment (). Of them, BDI was obtained in 19 (44%), belonging to upper-middle socioeconomic status families in 9/19, middle class in 5/19 and low class in 5/19. Their prenatal characteristics are shown (). No significant differences were found between the cases with or without completion of BDI.
Table 1. Summary of the characteristics of the cases with prenatally diagnosed isolated mild ventriculomegaly.
Natural history
The median (range) gestational age at the initial ultrasound was 26 weeks (20–37 weeks). Serial prenatal ultrasounds were available in 39/43 (91%) cases. The occurrence of additional findings is presented in Supplement Table S1. In 5/43 (11.6%) cases, structural abnormalities were detected during ultrasound follow-up. The prenatal detection of additional anomalies was associated with non-regressive forms (p = .01) and the presence of bilateral VM (p = .04).
Prenatal MRI was performed in 15/43 cases. The median (range) gestational age at prenatal MRI was 28 weeks (22–36 weeks). In 14/15 patients, a diagnostic concordance with the last ultrasound examination before the MRI in terms of the severity of VM was observed, and additional information was found in 2/15 cases, one case with subependymal grey matter heterotopia, and another case with subependymal nodular heterotopia and bilateral colobomas.
Neurodevelopmental outcome
Of the 19 cases with complete follow-up who undertook the BDI test, in 11 (57.9%), there was an in utero resolution of VM; in 5 (26.3%) it remained stable, and in 3 (15.8%), there was a progression of the VM. In 2/19 (10.5%) cases, there were additional brain anomalies diagnosed during pregnancy which were postnatally confirmed. These two cases included one of megacisterna magna and one of subependymal heterotopia, cortical atrophy, and delayed myelination.
The mean age of the infants at the time of the neurodevelopment evaluation with BDI was 56 months (range 24–86). BDI results are depicted in .
Table 2. Distribution of the results of the Battelle Developmental Inventory Screening Test in our series of 19 infants prenatally diagnosed with isolated mild ventriculomegaly.
We found lower scores in males (p = .006). The global score of the test was abnormal (< 2SD) in 10/19 (52.6%) cases, but only in 3 of them (19.2%) the neuropediatrician and neuropsychologist confirmed the neurodevelopmental delay. Of the abnormal patients, 3/10 (30%) had been previously diagnosed with neurological disorders, including one case of progressive VM, which required a ventriculoperitoneal shunt and presented mild motor and mild intellectual delay requiring early supportive measures, one with mild-to-moderate language, lecture, and attention impairment that requires a speech therapist; and one who suffers from severe intellectual delay requiring supportive measures due to a neuronal migration disorder. In the remaining 7 cases, no neurological disorders were identified.
Disabilities affecting social-personal skills were reported in 17/19 (89.5%), and in 12/19 (63.2%) of the cases, such delay was severe (<2SD). The ‘gross motor skills’ section was the second most compromised domain, affecting 12/19 (63.2%) of them, but only two children were receiving physiotherapy sessions. The ‘adaptative behavior’ domain which includes attention, eating, dressing, toileting, and personal responsibility, was the third most affected area with 11/19 (57.9%). ‘Fine motor skills’ disabilities were slightly less common (9/19, 47.4%). Communicative and cognitive areas were the least affected domains, and scores <2 SD were reported in 5 (26.3%) and 5 (26.3%) of our patients, respectively.
We compared the BDI global scores between the group with spontaneous in utero resolution of VM and the group with stable or progressive VM, and we found that scores of < 2SD were obtained in 7/11 (63.6%) and 3/8 (37.5%), respectively (p = .37). We also compared the BDI results between those in which the test was performed early (<56 months) and late (≥56 months). We found almost statistically significant differences in global scores (p = .05) with a trend toward poorer outcomes in the group of ≥ 56 months. However, we were not able to detect significant differences in any of the specific domains ().
Discussion
Main findings
Our prenatal series of “apparently” isolated mild VM shows first that the presence of associated abnormalities in the CNS in the follow-up is relatively common (11%). Second, these additional anomalies are associated with persistent and progressive VM and bilateral VM. Third, in those patients with VM regression (58%), there are no associated neurological malformations. And fourth, the postnatal application of the BDI scale demonstrates that the results are abnormal in the majority of these infants. The personal-social skills, gross motor skills, and adaptative behavior domains accumulate more disabilities. Communicative and cognitive areas are less affected. However, expert reevaluation of cases with altered BDI only found a neurodevelopmental delay in 30% (3/10). Of them, 2/3 had other structural brain abnormalities. This reflects that BDI scale should be used exclusively as a screening tool. Nevertheless, it could also indicate that, even in the absence of neurodevelopmental delay, these children may have neurological soft signs that are likely to be enhanced with early stimulation programs.
Interpretation of the results
In this study, we have followed a practical approach by setting our starting point for inclusion at the initial diagnosis of apparently isolated mild VM, even if additional abnormalities are discovered later, as this is a critical moment for parental assessment and decision-making. Several studies have attempted to identify factors correlated with the outcome of isolated mild VM. Some experts recommend the routine use of prenatal MRI in all cases of mild VM, as it could add relevant information in 6–10% of cases [Citation14,Citation19,Citation20]. Others, including ourselves, advocate that MRI should only be used when ultrasound imaging is inadequate or if there is a suspicion of an associated brain abnormality or VM progression [Citation12,Citation21–23]. In our study, fetal MRI was performed in 15/43 cases, and we obtained additional information in 13.3%. In the remaining cases, no clinical data suggesting additional CNS anomalies were postnatally detected, although we cannot completely rule them out, since MRI was not performed.
There is insufficient evidence about the mid-term postnatal outcome of infants with a prenatal diagnosis of mild VM. It is believed that more than 90% of them have a favorable prognosis. However, there is a need for a more refined neurodevelopmental assessment of these children. A quick and effective way for this assessment is the application of developmental questionnaires and scales within the family and school environment. Thus, we selected the complete BDI, a scale that explores in-depth five domains of development (personal-social skills, adaptive behavior, psychomotor ability, communication, and cognitive), to detect the presence of subtle alterations which may be otherwise unnoticed. Furthermore, this is a widely validated screening test to be used in children with an ample range of ages between 6 months and eight years, which fitted well with our patients. The high sensitivity of the extended BDI is helpful to avoid the risk of overlooking slight deficits but can also lead to overdiagnosis [Citation8]. The clinical significance of this information should be established with the aid of an expert.
We found that the most common disabilities in these patients affected the gross motor skills, personal-social, and behavior domains, in accordance with previous reports [Citation4,Citation8,Citation10,Citation24,Citation25]. Therefore, these are the areas where early interventions should focus. However, there is less affectation of other areas with a more significant impact on the child’s daily life, such as communicative and cognitive skills. We were unable to assess the bearing of additional abnormalities on the outcomes since only two of these cases completed the BDI (showing severe and moderate affectation of the global score, respectively). Interestingly, we found that 63.6% of cases with resolution of the in utero VM had abnormal BDI global scores. It could be argued that fetal VM is a marker of neurological risk and its recognition, regardless of its subsequent resolution, should be interpreted as an alarm signal that leads us to a more detailed study.
Another interesting finding was that children evaluated before 56 months had a trend toward better BDI than those assessed at a later age. Therefore a longitudinal study with serial follow-up would be necessary to corroborate if poorer BDI results are observed with advancing age. If so, this would have clinical relevance since the prognosis of many children could improve with the use of early interventions.
Strengths and limitations
The strengths of our study include our selection of only mild isolated cases of VM and our performance of a profound neurodevelopment assessment of the children by the administration of the full scale of the BDI test.
This test, together with a longer follow-up, has allowed us to broaden the knowledge of the impact of this anomaly on the neurodevelopment of the newborn and expand the conclusions of our previous research [Citation8], thereby confirming that the prenatal diagnosis of mild isolated VM implies a higher neurodevelopmental impact than previously believed. These findings could help provide adequate postnatal follow-up and early interventions to improve neurodevelopment in these children.
We acknowledge some limitations. First, the retrospective design of the study although it was based on careful data collection. Second, the sample size was small for drawing more solid conclusions, although it is challenging to recruit cases of isolated mild VM willing to complete the BDI test. Third, there may have been a response bias since we have not obtained a response from more than half of the patients in our sample. It could be speculated that parents who filled out the BDI test are more concerned about their child’s development. However, we did not find significant differences in the prenatal characteristics of the cases that completed the BDI test and those that did not. Finally, more studies are needed to prove the usefulness of early interventions on these infants.
In conclusion, this study opens a door to broadening the knowledge of the impact of VM on neurodevelopment, although our modest sample size precludes us from drawing more solid conclusions. The implementation of screening strategies, such as the BDI test, may help to recognize mild delays in different areas of neurological development during the infant period in children with a prenatal diagnosis of mild VM. However, in our series, expert neuropediatricians only confirmed a neurodevelopmental delay in 30% of the positive-screening cases.
Ethics approval and consent to participate
Ethical clearance was obtained from the research ethics committee of the Hospital Universitario 12 de Octubre (ref. N° 18/405).
The need for informed consent was officially waived by the ethics committee of the Institutional Review Board of the Faculty of Health Sciences due to the retrospective design of the study and the anonymous nature of the data collection process. Parents were contacted and invited to participate in the prospective postnatal follow-up test. Those who agreed were included after they signed an informed consent form.
All methods were performed in accordance with the ethical guidelines stipulated in the Declaration of Helsinki.
Author contributions
all authors have accepted responsibility for the entire content of this manuscript and approved its submission. All authors read and approved the final manuscript.
Supplemental Material
Download MS Word (15 KB)Acknowledgments
The authors are grateful to the mothers who have selflessly contributed to the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
the datasets used and/or analyses performed during the study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Pilu G, Hobbins JC. Sonography of fetal cerebrospinal anomalies. Prenat Diagn. 2002;22(4):321–330.
- Sethna F, Tennant PWG, Rankin J, et al. Prevalence, natural history, and clinical outcome of mild to moderate ventriculomegaly. Obstet Gynecol. 2011;117(4):867–876.
- Kelly EN, Allen VM, Seaward G, et al. Mild ventriculomegaly in the fetus, natural history, associated findings and outcome of isolated mild ventriculomegaly: a literature review. Prenat Diagn. 2001;21(8):697–700.
- Beeghly M, Ware J, Soul J, et al. Neurodevelopmental outcome of fetuses referred for ventriculomegaly. Ultrasound Obstet Gynecol. 2010;35(4):405–416.
- Melchiorre K, Bhide A, Gika AD, et al. Counseling in isolated mild fetal ventriculomegaly. Ultrasound Obstet Gynecol. 2009;34(2):212–224.
- Pisapia JM, Sinha S, Zarnow DM, et al. Fetal ventriculomegaly: diagnosis, treatment, and future directions. Childs Nerv Syst. 2017;33(7):1113–1123.
- Fox NS, Monteagudo A, Kuller JA, Society for Maternal-Fetal Medicine (SMFM), et al. Mild fetal ventriculomegaly: diagnosis, evaluation, and management. Am J Obstet Gynecol. 2018;219(1):B2–B9.
- Gómez-Arriaga P, Herraiz I, Puente JM, et al. Mid-term neurodevelopmental outcome in isolated mild ventriculomegaly diagnosed in fetal life. Fetal Diagn Ther. 2012;31(1):12–18.
- Pagani G, Thilaganathan B, Prefumo F. Neurodevelopmental outcome in isolated mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2014;44(3):254–260.
- Thorup E, Jensen LN, Bak GS, et al. Neurodevelopmental disorder in children believed to have isolated mild ventriculomegaly prenatally. Ultrasound Obstet Gynecol. 2019;54(2):182–189.
- Perlman S, Bar-Yosef O, Jacobson JM, et al. Natural history of fetal isolated ventriculomegaly: comparison between pre- and post-natal imaging. J Matern Fetal Neonatal Med. 2018;31(13):1762–1767.
- Baffero GM, Crovetto F, Fabietti I, et al. Prenatal ultrasound predictors of postnatal major cerebral abnormalities in fetuses with apparently isolated mild ventriculomegaly. Prenat Diagn. 2015;35(8):783–788.
- Kheiri G, Naderian N, Karami S, et al. Prenatal ventriculomegaly: natural course, survival, and neurodevelopmental status. J Neurosurg Pediatr. 2021;5:1–6.
- Malinger G, Paladini D, Haratz KK, et al. ISUOG practice guidelines (updated): sonographic examination of the fetal Central nervous system. Part 1: performance of screening examination and indications for targeted neurosonography. Ultrasound Obstet Gynecol. 2020;56(3):476–484.
- Kyriakopoulou V, Vatansever D, Davidson A, et al. Normative biometry of the fetal brain using magnetic resonance imaging. Brain Struct Funct. 2017;222(5):2295–2307.
- Berls AT, McEwen IR. Battelle developmental inventory. Phys Ther. 1999;79(8):776–783.
- Newborg J, Stock JR, Wnek L, et al. The battelle developmental inventory. Allen (TX): DLM Teaching Resources; 1988.
- Newborg J, Stock JR, Batelle WK. Inventario de desarrollo. Madrid: TEA; 2004.
- Di Mascio D, Sileo FG, Khalil A, et al. Role of magnetic resonance imaging in fetuses with mild or moderate ventriculomegaly in the era of fetal neurosonography: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019;54(2):164–171.
- Prayer D, Paladini D, Deprest J. Current controversies in prenatal diagnosis 1: should MRI be performed on all fetuses with mild ventriculomegaly? Prenat Diagn. 2019;39(5):331–338.
- Doğan Durdağ G, Yılmaz Baran Ş, Kalaycı H, et al. Is fetal magnetic resonance imaging indicated in patients with isolated ventriculomegaly? Eur J Obstet Gynecol Reprod Biol. 2019;240:52–56.
- Parazzini C, Righini A, Doneda C, et al. Is fetal magnetic resonance imaging indicated when ultrasound isolated mild ventriculomegaly is present in pregnancies with no risk factors? Prenat Diagn. 2012;32(8):752–757.
- Rydz D, Srour M, Oskoui M, et al. Screening for developmental delay in the setting of a community pediatric clinic: a prospective assessment of parent-report questionnaires. Pediatrics. 2006;118(4):e1178–e1186.
- Bloom SL, Bloom DD, DellaNebbia C, et al. The developmental outcome of children with antenatal mild isolated ventriculomegaly. Obstet Gynecol. 1997;90(1):93–97.
- Sadan S, Malinger G, Schweiger A, et al. Neuropsychological outcome of children with asymmetric ventricles or unilateral mild ventriculomegaly identified in utero. BJOG. 2007;114(5):596–602.
