The clinician’s concept of mitral stenosis (MS) is often based around the model of rheumatic disease in younger patients. In such rheumatic patients, management is generally clear and current guidelines [Citation1] offer a structured approach to investigation and treatment. However, as in many other cardiovascular diseases, the patient profile in countries with advanced economies has changed. Patients with MS today are older and suffer from multiple diseases that effect cardiac function. With advancing age the pathology also becomes more complex, and there is an increasing shift from rheumatic to degenerative MS caused by mitral annular calcification (MAC) encroaching on valve leaflet function [Citation2]. Conventional imaging approaches (usually by echocardiography) have involved understanding obstruction at the level of the valve. The mitral valve area reduces which impedes flow resulting in an atrioventricular pressure gradient, raised LA pressure and ultimately pulmonary hypertension. This is an oversimplification which becomes more clinically relevant as the disease process and the clinical profile of the patients become more complicated. All of these factors mean our current approaches to medical, surgical and percutaneous management may not deliver equivalent outcomes compared with more conventional rheumatic patients.
MS remains a relatively rare disease which in a recent large analysis of public health records in Sweden was found in only 1917 (0.02%) individuals [Citation3]. For comparison overall, the rates for valvular heart disease in this study were 0.65% across all age groups with a dramatic increase from the fifth decade onwards. In a recent UK cohorts the MS was found in 0.1% in healthy screened subjects over 65 years [Citation4], while in the US, a prevalence of 0.2% in those over 75 undergoing population screening has been noted [Citation5]. Surprisingly, mitral stenosis seems to be following the same age trajectory as other valve diseases, and, although patients with prior rheumatic fever are still 3.5 times more likely to suffer from MS, many cases have no antecedent rheumatic history nor clear rheumatic changes on echocardiography. In the EuroHeart survey (limited to moderate and severe disease) which is now more than 15 years old, the proportion of cases with degenerative disease was 12.5% [Citation6]. This trend suggests a shift from rheumatic to degenerative valvular pathology with advancing age. There is a female preponderance for both degenerative and rheumatic MS [Citation3,Citation7–Citation9]. Why women are more likely to develop stenosis is not known.
Current European Society of Cardiology/European Association of Cardiothoracic Surgery (ESC/EACTS) [Citation1] suggest balloon valvotomy or surgery for patients with symptomatic moderate or severe MS defined as a mitral valve area (MVA) of less than 1.5cm2. In those with significant MS and no symptoms, intervention may be offered in line with a very narrow set of indications to prevent thromboembolism or pulmonary hypertension. Although the guidelines also allude to intervention with those with mitral valve areas greater than 1.5cm2 no real guidance about how to assess this situation is provided. A major weakness in the guidance is that it does not specifically differentiate between rheumatic and degenerative mitral stenosis, despite the latter having a different pathology, different patient profile and very different outcomes to intervention.
A frequent clinical scenario is a breathless patient with MSan MVA > 1.5 cm2 who has either no other apparent cause in the case of rheumatic disease, or multiple possible causes in the case of degenerative disease. Pregnancy can act as a biological model because cardiac output involuntarily rises to meet increased metabolic demand. Cardiac events and mortality are frequent in women with a mitral valve orifice greater than 1.5 cm2. Up to 20% of women with mild MS develop pulmonary edema [Citation10]. MS therefore must still be considered the likely cause of breathlessness in patients with mild disease and no other reason for symptoms. Augmenting flow across the mitral valve assessed either by exercise or by dobutamine infusion may reveal important hemodynamic findings. The valve resistance, a measure which incorporates both gradients and flow, is an important predictor of pulmonary vascular changes [Citation11] and although not used in routine practice may better describe the obstructive character of the valve than gradient or valve area alone.
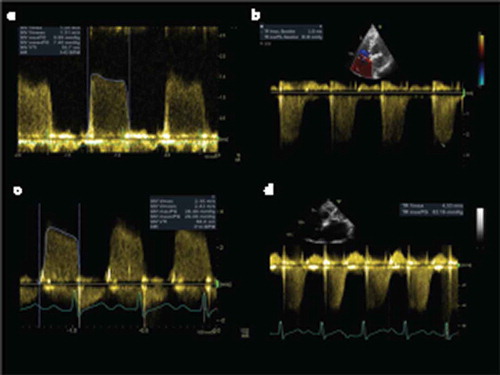
Bicycle or dobutamine stress echocardiography can be particularly clinically useful in this situation, giving the opportunity to augment flow and measure the resultant change in hemodynamics non-invasively. The test allows an objective measure of exercise performance, it also permits a measure of the heart rate response to exercise (excessive tachycardia causes a disproportionate increase in gradient) as well as allowing a comprehensive assessment of change in transmitral gradient, mitral valve area and the pulmonary artery systolic pressure () [Citation12]. Grimiladi et al. undertook stress echo in patients with MS and a valve area of 1.0–1.5 cm (above the indication for surgery at the time of study design) and found that 75% had either symptoms or high gradients with or without important elevations in PA systolic pressure [Citation13]. Fifty percent had an exercise tolerance less than 50 W, and most importantly, all those with symptoms underwent intervention with a response rate of more than 80% (defined as NYHA 1 at 6 months). Laufer-Perl demonstrated that a range of complex cardiac parameters (stroke volume reserve and chronotropic incompetence) as well as abnormalities of lung function predicted effort intolerance in a group of patients with mild MS, effort intolerance being observed in all cases when compared to control [Citation14].
Figure 1. Increasing transmitral gradients (a-c) and tricuspid peak velocity (related directly to PA systolic pressure) (B & D) during exercise stress echocardiography.
Obstruction at the level of valve is a key evaluation parameter, but how the left atrium and the left ventricle deal with the pressure is also an important determinant of pulmonary hypertension and symptoms. Understanding the physical properties of both the atrium and the ventricle is especially important when symptoms and valve area are discordant. At its most extreme the atrial wall can be almost completely replaced by fibrosis [Citation15,Citation16] thus unable to accommodate the higher pressures generated when heart rate and flow rates increase. The total net compliance of the atrium and ventricle provides a more comprehensive assessment of the hemodynamic consequences of MS and can be non-invasively estimated from transmitral Doppler echocardiography using a directly measured MVA and the downslope of the transmitral Doppler trace [Citation17,Citation18]; it can also be measured invasively during valvuloplasty procedures. A low combined net compliance of ventricle and atrium appears to track well to disproportionate pulmonary hypertension, symptoms, response to treatment and morbid cardiac events [Citation17]. Compliance is however not a fixed phenomenon; some, but not all, patients see a significant increase in compliance atrial after valvoplasty suggesting the pressure/function relationship is to some extent load dependent. Those who cannot modulate compliance after treatment get the worst symptomatic response to improving the balloon valvotomy [Citation19].
Classically MS is considered a disease in which the ventricle is spared the effects of excessive loading conditions. Recent evidence from deformation imaging echocardiography [Citation20,Citation21] has demonstrated significant ventricular dysfunction although with a preserved ejection fraction, the pattern of dysfunction favoring the basal and mid segments. This has prompted the hypothesis that the rheumatic pancarditis may also result in long-term ventricular fibrosis which may limit the benefits of treatments to the mitral valve. Sengupata et al. recently noted that ventricular abnormalities resolve after relief of mitral stenosis, suggesting that ventricular loading due to the very abnormal profile of trans mitral flow may be the cause of some of ventricular dysfunction [Citation22] and hence be reversible. This remains an area of uncertainty.
Low flow aortic stenosis is a well recognized clinical entity and much has been written about how best to investigate and manage the condition [Citation1]. It is increasingly recognized that gradients across the mitral valve also fall as transmitral flow reduces leading to an analogous syndrome of low flow low gradient mitral stenosis [Citation23]. This is conventionally defined as a mean MVA of less than 1.5 cm2, measured directly from planimetry of the echocardiogram, and mean gradient of less than 10 mmHg and a transmittal flow less than 35 mls/m2, estimated from transmitral doppler. As with low flow aortic stenosis, it is often ambiguous if the valve or other factors in the circulation are limiting flow and valve opening. Recent evidence has suggested that these patients are very different being older, more ill, with more atrial fibrillation and more subvalvular disease. After valvotomy, they have a lower reduction in LA pressure, and most importantly a worse symptomatic response. Measured directly in this study, the main limitation of flow was at the level of the vasculature with significantly elevated after-load, rather than intrinsic contractile abnormalities of the left ventricle. Similar disappointing results in this group have been observed with mitral valve surgery [Citation23].
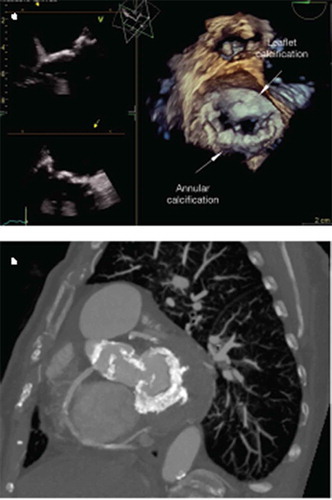
Degenerative MS because of mitral annular calcification is an increasingly common diagnosis (). In the original EuroHeart survey, 12% of mitral stenosis was degenerative and is likely to have risen in the intervening decade [Citation6]. It is a complex disease to evaluate for most of the reasons outlined above. It tends to be a disease of the elderly, who suffer from more comorbidities, reduced atrial and ventricular compliance as well as abnormal vascular function. Diastolic LV dysfunction is common and sometimes challenging to differentiate clinically. Detailed morphological evaluation of the valve, with TOE if necessary, is required. Balloon valvoplasty has no role in this disease as the pathology does not involve commissural fusion and surgery comes at a significant risk of complications [Citation24,Citation25]. In recent years the deployment of TAVI valves within the ring of annular calcification has emerged as a less invasive alternative to surgery. The outcomes hemodynamic and symptomatic results of valve in MAC are good but at the penalty of very significant mortality, in the largest series to date this was 25% at 20 days and 54% at 12 months [Citation26]. This field is moving very fast with a constant pipeline of new devices and approaches in development. It seems likely that by the middle of the next decade percutaneous treatments will be the mainstay of treatment.
Figure 2. (a) 2 and 3D transoesophageal echocardiography demonstrating extensive severe annular and leaflet calcification resulting in degenerative MS. (b) Circumferential annular calcification demonstrated by multislice computerised tomography.
Although the current international consensus guidance does not satisfactory cover many of the scenarios outlined above, some common themes emerge. Firstly, the outcomes of intervention, whether surgical or percutaneous are much less certain. It is therefore reasonable to offer medical therapy in all instances as a first approach. Heart rate control with prolongation of diastole is effective in reducing transmitral gradients and improve exercise tolerance. Beta blockers are the mainstay of therapy [Citation27], while rate-limiting calcium antagonists or digoxin provide alternatives in atrial fibrillation. For patients in sinus rhythm, ivabradine is an emerging effective alternative [Citation28]. If medical therapy fails, then exercise stress echocardiography is useful to assess the consequences of increase demand on transmittal gradients. Anatomical information from transesophageal echocardiography and gated computer tomography (for degenerative) disease is invaluable before difficult interventional decisions are made by the heart team. We propose a specific management algorithm ()
Figure 3. Proposed algorithm for the evaluation and treatment of patients presenting with symptomatic mitral stenosis in circumstances not covered by ESC/EACTS guideline [Citation1].
![Figure 3. Proposed algorithm for the evaluation and treatment of patients presenting with symptomatic mitral stenosis in circumstances not covered by ESC/EACTS guideline [Citation1].](/cms/asset/ed7c6035-f0dc-4452-a641-993a0e4d43ac/ierk_a_1632190_f0003_oc.jpg)
Mitral stenosis is relatively rare, and its management complexity is easy to overlook, often being reduced to a binary decision between balloon valvotomy or surgery. Too often clinicians are faced with a patient with rather modest mitral stenosis but significant symptoms. This may occur in younger patients because of either reduced mitral valve compliance or loss of atrial compliance to buffer atrial pressure changes. In the more elderly patent with more co-morbidities which effect trans valvular flow, the relative contribution of valve stenosis, atrial or ventricular compliance and vascular adaption, as well as other confounders such as atrial fibrillation, become more important. The most extreme examples of this are calcific degenerative mitral stenosis and the increasingly recognized syndrome of low gradient severe mitral stenosis. In these groups, the outcomes of intervention are uncertain at best and hazardous at worst, so very meticulous evaluation of each aspect of the anatomy and physiology is indicated to make best interest clinical decisions. Stress echocardiography plays a pivotal role in establishing changes in trans valvular gradient and pulmonary artery systolic pressure, thus refining the opportunities for therapy. Current guidelines help little with the management of these patients so careful multidisciplinary evaluation is required to achieve the best clinical outcomes.
Declaration of interest
G Lloyd holds research awards from Medtronic; grants from the Edwards foundation; and honoraria from Edwards Lifesciences in the field of heart valve disease. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Baumgartner H, Falk V, Bax JJ, et al. ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739–2791.
- Sud K, Agarwal S, Parashar A, et al. Degenerative mitral stenosis: unmet need for percutaneous interventions. Circulation. 2016;133(16):1594–1604.
- Andell P, Li X, Martinsson A, et al. Epidemiology of valvular heart disease in a Swedish nationwide hospital-based register study. Heart. 2017;103(21):1696–1703.
- d’Arcy JL, Coffey S, Loudon MA, et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE population cohort study. Eur Heart J. 2016;37(47):3515–3522.
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005–1011.
- Lung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: the Euro heart survey on valvular heart disease. Eur Heart J. 2003;24(13):1231–1243.
- Oktay AA, Gilliland YE, Lavie CJ, et al. Echocardiographic assessment of degenerative mitral stenosis: a diagnostic challenge of an emerging cardiac disease. Curr Probl Cardiol. 2017;42(3):71–100.
- Manjunath CN, Srinivas P, Ravindranath KS, et al. Incidence and patterns of valvular heart disease in a tertiary care high-volume cardiac center: a single center experience. Indian Heart J. 2014;66(3):320–326.
- Chiang CW, Kuo CT, Chen WJ, et al. Comparisons between female and male patients with mitral stenosis. Br Heart J. 2994;72(6):567–570.
- Tsiaras S, Poppas A. Mitral valve disease in pregnancy: outcomes and management. Obstet Med. 2009;2(1):6–10.
- Izgi C, Ozdemir N, Cevik C, et al. Mitral valve resistance as a determinant of resting and stress pulmonary artery pressure in patients with mitral stenosis: a dobutamine stress study. J Am Soc Echocardiogr. 2007;20(10):1160–1166.
- Badiani S, Waddingham P, Lloyd G. Bhattacharyya S.Stress echocardiography in valvular heart disease. Expert Rev Cardiovasc Ther. 2018;16(11):795–804.
- Grimaldi A, Olivotto I, Figini F, et al. Dynamic assessment of ‘valvular reserve capacity’ in patients with rheumatic mitral stenosis. Eur Heart J Cardiovasc Imaging. 2012;13(6):476–482.
- Laufer-Perl M, Gura Y, Shimiaie J, et al. Mechanisms of effort intolerance in patients with rheumatic mitral stenosis: combined echocardiography and cardiopulmonary stress protocol. JACC Cardiovasc Imaging. 2017;10(6):622–633.
- Zhu D, Wu Z, van der Geest RJ, et al. Accuracy of late gadolinium enhancement - Magnetic resonance imaging in the measurement of left atrial substrate remodeling in patients with rheumatic mitral valve disease and persistent atrial fibrillation. Int Heart J. 2015;56(5):505–510.
- Shriki J, Talkin B, Thomas IC, et al. Delayed gadolinium enhancement in the atrial wall: a novel finding in 3 patients with rheumatic heart disease. Tex Heart Inst J. 2011;38(1):56–60.
- Nunes MCP, Tan TC, Elmariah S, et al. Net atrioventricular compliance is an independent predictor of cardiovascular death in mitral stenosis. Heart. 2017;103(23):189–1891.
- Athayde GRS, Nascimento BR, Elmariah S, et al. Impact of left atrial compliance improvement on functional status after percutaneous mitral valvuloplasty. Catheter Cardiovasc Interv. 2019;93(1):156–163.
- Mahfouz RA, Elawady W, Hossein E, et al. Impact of atrioventricular compliance on clinical outcome of patients undergoing successful percutaneous balloon mitral valvuloplasty. Echocardiography. 2013;30(10):1187–1193.
- Dogan S, Aydin M, Gursurer M, et al. Prediction of subclinical left ventricular dysfunction with strain rate imaging in patients with mild to moderate rheumatic mitral stenosis. J Am Soc Echocardiogr. 2006;19(3):243–248.
- Ozdemir AO, Kaya CT, Ozcan OU, et al. Prediction of subclinical left ventricular dysfunction with longitudinal two-dimensional strain and strain rate imaging in patients with mitral stenosis. Int J Cardiovasc Imaging. 2010;26(4):397–404.
- Sengupta SP, Amaki M, Bansal M, et al. Effects of percutaneous balloon mitral valvuloplasty on left ventricular deformation in patients with isolated severe mitral stenosis: a speckle-tracking strain echocardiographic study. J Am Soc Echocardiogr. 2014;27(6):639–647.
- El Sabbagh A, Reddy YNV, Barros-Gomes S, et al. Low-gradient severe mitral stenosis: hemodynamic profiles, clinical characteristics, and outcomes. J Am Heart Assoc. 2019;8(5):e01073624.
- Cho IJ, Hong GR, Lee SH, et al. Differences in characteristics, left atrial reverse remodeling, and functional outcomes after mitral valve replacement in patients with low-gradient very severe mitral stenosis. J Am Soc Echocardiogr. 2016;29(8):759–767.
- Okada Y. Surgical management of mitral annular calcification. Gen Thorac Cardiovasc Surg. 2013;61(11):619–625.
- Guerrero M, Urena M, Himbert D, et al. 1-Year outcomes of transcatheter mitral valve replacement in patients with severe mitral annular calcification. J Am Coll Cardiol. 2018;71(17):1841–1853.
- Klein HO, Sareli P, Schamroth CL, et al. Effects of atenolol on exercise capacity in patients with mitral stenosis with sinus rhythm. Am J Cardiol. 1985;56(10):598–601.
- Rajesh GN, Sajeer K, Sajeev CG, et al. A comparative study of ivabradine and atenolol in patients with moderate mitral stenosis in sinus rhythm. Indian Heart J. 2016;68(3):311–315.
