1. Introduction
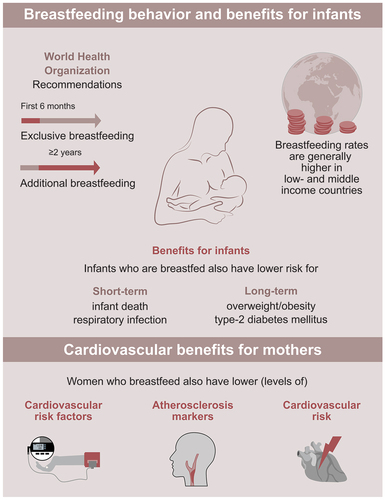
The benefits of breastfeeding on infants are widely known, and include both short- and long-term benefits such as a reduced risk for infant death and respiratory infections as well as a reduced risk for adiposity and type 2 diabetes mellitus [Citation1]. Consequently, the World Health Organization recommends breastfeeding children exclusively for the first 6 months after birth and continuing breastfeeding for up to 2 years or longer while combining it with complementary feeding. Although rates of breastfeeding initiation are high at global level, the duration of lactation differs significantly across countries [Citation1]. In low- and middle-income countries, only one in three infants is breastfed exclusively during the first 6 months after birth and 37% of children aged 6–23 months do not receive any breast milk [Citation1]. Lactation rates are even lower in high-income countries, albeit with large between-countries variabilities [Citation1]. For instance, at 1 year of age, less than 1% of infants receive breast milk in the United Kingdom compared to 27% in the United States and 95% in Oman [Citation1].
Several reproductive and pregnancy-related factors have been associated with maternal cardiovascular health [Citation2]. For instance, it has been demonstrated that having more children is related to a higher risk for future maternal coronary heart disease [Citation3]. Moreover, a higher number of pregnancies and a history of miscarriage, induced abortion, or stillbirth were related to an elevated risk of developing maternal cardiovascular disease [Citation4]. In addition to these pregnancy-related factors, a variety of studies have investigated whether breastfeeding could also impact a mother’s risk for cardiovascular disease later in life.
2. Benefits of lactation on breastfeeding mothers
While the advantages of breastfeeding on infants are commonly known, the benefits for mothers who have lactated are less well known. However, breastfeeding also has various beneficial short- and long-term impacts on mothers [Citation1,Citation5]. For instance, it supports birth spacing as it has been demonstrated to be related to longer duration of postpartum amenorrhea [Citation5]. Furthermore, breastfeeding has been associated with a lower risk of future maternal breast and ovarian carcinoma [Citation5]. Breastfeeding might also confer several cardiovascular benefits [Citation6], including positive effects on maternal cardiovascular risk factors, markers for subclinical atherosclerosis, and risk of cardiovascular events such as coronary heart disease or stroke.
2.1. Cardiovascular risk factors
Breastfeeding has been shown to be associated with an advantageous profile of various major cardiovascular risk factors, including diabetes, hypertension, and the metabolic syndrome.
In a systematic review and meta-analysis of 22 studies, women who ever lactated had a 27% lower risk of maternal type 2 diabetes mellitus compared to women who never lactated (relative risk [RR] 0.73 [95% confidence interval [CI] 0.65, 0.83]) [Citation7]. Moreover, each additional month of lactation was associated with a 1% lower risk of type 2 diabetes (RR 0.990 [95% CI 0.984, 0.996]) [Citation7]. Studies included in these meta-analyses adjusted relative risks for several potential confounding factors including age, body mass index, ethnicity, education, smoking, and parity, among others.
Furthermore, it has been shown that breastfeeding is related to a lower risk of hypertension [Citation6]. A meta-analysis of seven studies and 444,759 participants reported that women who had breastfed had a 7% lower risk for hypertension (odds ratio 0.93 [95% CI 0.91, 0.95]) in comparison to women that did not breastfeed [Citation8]. Notably, studies reported odds ratios adjusted for multiple potential confounders such as age, body mass index, and smoking. Furthermore, compared to mothers who had not breastfed, women who had breastfed for >0-6, >6–12, or >12 months had a reduced risk of hypertension of 8%, 11%, or 12%, respectively [Citation8].
It has also been suggested that breastfeeding is associated with postpartum weight loss [Citation9]. As outlined in a systematic review of 45 observational studies, results on the role of breastfeeding in weight change after pregnancy were conflicting across prior studies; however, evidence from studies of high methodological quality (i.e. studies that objectively measured postpartum weight change and adjusted for important covariates) indicated that lactation is indeed associated with postpartum weight change [Citation10].
In addition, lactation plays a role in the development of metabolic syndrome, a cluster of conditions favoring risk for cardiovascular disease [Citation6]. For instance, an analysis of the Coronary Artery Risk Development in Young Adults Study, including 704 parous women, reported an inverse association between longer duration of lactation and incidence of metabolic syndrome in both women with and without gestational diabetes mellitus when adjusting for several potential confounding characteristics such as race, age, education, smoking, and time-dependent parity, among others [Citation11].
2.2. Subclinical atherosclerosis
Breastfeeding has also been associated with markers for subclinical atherosclerosis in mothers, including coronary, aortic, and carotid vasculature [Citation6]. A recent meta-analysis of three studies found that the carotid intima-media thickness was significantly lower in women who breastfed for 6 months or longer compared to women who breastfed for a shorter duration or not at all [Citation12]. Similarly, the Study of Women Across the Nation found a higher risk for aortic or coronary artery calcification for mothers who had not breastfed compared to those who had breastfed all children for at least 3 months after adjusting for variables on socioeconomic status, lifestyle, and family history [Citation13].
2.3. Cardiovascular events
Multiple studies have also demonstrated a positive association between breastfeeding and the incidence of cardiovascular disease events, including coronary heart disease, stroke, and cardiovascular mortality [Citation14]. A recent systematic review and meta-analysis combined the results of eight studies on over 1 million parous women in order to investigate the relationship between lactation and risk of cardiovascular disease [Citation15]. Over a weighted median follow-up of 10.3 years, >50,000 cardiovascular disease events, >25,000 coronary heart disease events, >30,000 strokes, and >10,000 deaths from cardiovascular disease were reported by the studies. The meta-analysis revealed a reduced risk of 11% for maternal cardiovascular disease (hazard ratio 0.89 [95% CI 0.83, 0.95]), 14% for maternal coronary heart disease (0.86 [95% CI 0.78, 0.95]), 12% for maternal stroke (0.88 [95% CI 0.79, 0.99]), and 17% for maternal fatal cardiovascular disease (0.83 [95% CI 0.76, 0.92]) for women who ever breastfed compared to parous women who never breastfed [Citation15]. The majority of studies included in these meta-analyses adjusted for a variety of potential confounders (i.e. demographics, cardiovascular risk factors, and reproductive- and pregnancy-related factors). Moreover, progressive reductions of cardiovascular risk were reported for lifetime durations of breastfeeding for up to approximately 12 months with uncertainties in shapes of association for longer durations of breastfeeding [Citation15].
3. Causality
The results of a variety of studies point toward a significant role of breastfeeding in the path of developing cardiovascular disease. However, those studies were of observational nature, and it cannot be concluded that there is a causal relationship between lactation and cardiovascular risk. Indeed, while the majority of studies adjusted for a variety of potential confounding factors, including demographics, cardiovascular risk factors, and reproductive- and pregnancy-related factors, residual confounding cannot be ruled out. This is also underpinned by the fact that multiple factors that are considered related to increased cardiovascular risk, such as pre-pregnancy obesity or smoking, have also been associated with a lower chance to initiate breastfeeding [Citation16]. Another important factor that influences both breastfeeding behavior and risk for cardiovascular disease is socioeconomic status [Citation1,Citation17]. Consequently, it is important to control for socioeconomic status when investigating the relationship between breastfeeding initiation and duration and cardiovascular risk. On the contrary, Stuebe and Rich-Edwards suggested that breastfeeding could be responsible for resetting the pregnancy-related disturbed metabolism of mothers after birth (‘reset-hypothesis’) [Citation9]. Nevertheless, whether or not breastfeeding is causally linked to cardiovascular risk in the mother, it is unlikely to harm and the benefits for infants are undisputable.
4. Implications
The benefits of breastfeeding for infants are widely known. However, the positive impacts of lactation on breastfeeding mothers are communicated to a lesser extent. A recent national survey in the United States revealed that only 38.5% of women are aware that breastfeeding is related to a decreased risk for breast cancer [Citation18]. Improving communication strategies of beneficial aspects of breastfeeding not only for the child but also for the mother may increase rates of breastfeeding initiation and improve duration of breastfeeding. However, the reason why many mothers decide not to breastfeed or discontinue breastfeeding is not always intertwined with not willing to breastfeed [Citation19]. In fact, many other determinants are linked to lactation behavior. For instance, opinions of close persons influence breastfeeding behavior such as experiences of relatives or attitudes of the mother’s partner [Citation19]. Moreover, some women encounter negative experiences while breastfeeding in public places [Citation19]. Another important factor is a woman’s work situation. No or short maternity leave and multifaceted pressure often lead to non-initiation or early discontinuation of breastfeeding [Citation19].
Several interventions on improvement of lactation behavior have been suggested that target different parameters. Measures that positively affect breastfeeding behavior include adequate maternity leave and possibilities for mothers to continue breastfeeding after returning to work, such as lactation breaks and separate rooms for breastfeeding and pumping of breast milk [Citation19]. Furthermore, support for mothers, fathers, and other family members had positive impacts on breastfeeding behavior. For instance, home- and family-based as well as community-based interventions comprising counseling and education were demonstrated to significantly improve lactation initiation and continuation [Citation19]. It is essential that governments, health-care providers, and employers are aware of such interventions and facilitate women that want to lactate in a breastfeeding-friendly environment.
Breastfeeding behavior is related to socioeconomic status. In general, breastfeeding is more prevalent in low- and middle-income countries than in high-income countries [Citation1]. Moreover, also within low- and middle-income countries, breastfeeding durations for poorer women are on average higher than for richer women [Citation1]. Contrarily, within high-income countries, well-educated women tend to breastfeed more commonly [Citation1]. This fact also highlights the importance of breastfeeding being ‘one of few positive health-related behaviors in low- and middle-income countries that is less frequent in rich people, both between and within countries’ as stated by Victora et al. [Citation1].
5. Conclusion
Several benefits of breastfeeding along the pathway to maternal cardiovascular disease development have been reported (). These range from associations of lactation with reduced cardiovascular risk factors, markers for subclinical atherosclerosis, and incidence of maternal cardiovascular events. Beneficial aspects of breastfeeding need to be better communicated. Moreover, measures that enable women to breastfeed, also as they return to work, need to be implemented and strengthened such that mothers who are willing to breastfeed also have the possibilities to do so.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Victora CG, Bahl R, Barros AJD, et al., Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490.
- O’Kelly AC, Michos ED, Shufelt CL, et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res. 2022;130(4):652–672.
- Peters SA, van der Schouw YT, Wood AM, et al. Parity, breastfeeding and risk of coronary heart disease: a pan-European case-cohort study. Eur J Prev Cardiol. 2016;23(16):1755–1765.
- Peters SAE, Yang L, Guo Y, et al. Pregnancy, pregnancy loss, and the risk of cardiovascular disease in Chinese women: findings from the China Kadoorie biobank. BMC Med. 2017;15(1):148.
- Chowdhury R, Sinha B, Sankar MJ, et al., Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):96–113.
- Nguyen B, Jin K, Ding D. Breastfeeding and maternal cardiovascular risk factors and outcomes: a systematic review. PLoS One. 2017;12(11):e0187923.
- Pinho-Gomes A-C, Morelli G, Jones A, et al. Association of lactation with maternal risk of type 2 diabetes: a systematic review and meta-analysis of observational studies. Diabetes Obes Metab. 2021;23(8):1902–1916.
- Qu G, Wang L, Tang X, et al. Association between duration of breastfeeding and maternal hypertension: a systematic review and meta-analysis. Breastfeed Med. 2018;13(5):318–326.
- Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009;26(1):81–88.
- Neville CE, McKinley MC, Holmes VA, et al. The relationship between breastfeeding and postpartum weight change—a systematic review and critical evaluation. Int J Obes (Lond). 2014;38(4):577–590.
- Gunderson EP, Jacobs DR, Chiang V, et al. Duration of lactation and incidence of the metabolic syndrome in women of reproductive age according to gestational diabetes mellitus status: a 20-year prospective study in CARDIA (Coronary artery risk development in young adults). Diabetes. 2010;59(2):495–504.
- Pérez-Roncero GR, López-Baena MT, Sánchez-Prieto M, et al. Association of breastfeeding duration with carotid intima-media thickness in later life: a systematic review and meta-analysis. Gynecol Endocrinol. 2021;37(9):778–784.
- Schwarz EB, McClure CK, Tepper PG, et al. Lactation and maternal measures of subclinical cardiovascular disease. Obstet Gynecol. 2010;115(1):41–48.
- Peters SAE, Yang L, Guo Y, et al. Breastfeeding and the risk of maternal cardiovascular disease: a prospective study of 300 000 Chinese women. J Am Heart Assoc. 2017;6(6). DOI:10.1161/JAHA.117.006081.
- Tschiderer L, Seekircher L, Kunutsor SK, et al. Breastfeeding is associated with a reduced maternal cardiovascular risk: systematic review and meta-analysis involving data from 8 studies and 1,192,700 parous women. J Am Heart Assoc. 2022;11(2):e022746.
- Stuebe AM. Does breastfeeding prevent the metabolic syndrome, or does the metabolic syndrome prevent breastfeeding? Semin Perinatol. 2015;39(4):290–295.
- Rosengren A, Smyth A, Rangarajan S, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. 2019;7(6):e748–e760.
- Hoyt-Austin A, Dove MS, Abrahão R, et al. Awareness that breastfeeding reduces breast cancer risk: 2015-2017 National Survey of Family Growth. Obstet Gynecol. 2020;136(6):1154–1156.
- Rollins NC, Bhandari N, Hajeebhoy N, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387(10017):491–504.