ABSTRACT
Introduction: Ceftobiprole is a fifth-generation cephalosporin with a broad spectrum of antimicrobial activity, including also methicillin-resistant Staphylococcus aureus (MRSA). Ceftobiprole is approved for the treatment of community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP), excluding ventilator-associated pneumonia, in several European and non-European countries.
Areas covered: In this narrative review, we discuss the current place in therapy of ceftobiprole, both within and outside approved indications. An inductive MEDLINE/PubMed search of the available literature was conducted.
Expert opinion: There are three main reasons which render ceftobiprole an attractive option for the empirical and targeted treatment of CAP and HAP: (i) its broad spectrum of activity; (ii) its activity against MRSA; (iii) its good safety profile. For these indications, ceftobiprole should be employed thoughtfully, in those scenarios in which its intrinsic advantages could be maximized. The use of ceftobiprole outside approved indications could be justified in specific scenarios, such as when other approved alternatives are ineffective, when the risk of toxicity due to other agents is unacceptable, and for salvage therapy. In the near future, ongoing phase 3 studies and further observational experiences could both enlarge the current panel of approved indications and enrich our knowledge on the use of ceftobiprole for off-label indications.
1. Introduction
Ceftobiprole is a fifth-generation cephalosporin with a wide spectrum of antimicrobial activity, including various Gram-positive and Gram-negative bacteria [Citation1,Citation2]. One of the preeminent features of ceftobiprole is its activity against methicillin-resistant Staphylococcus aureus (MRSA) [Citation3], a peculiarity of a very few β-lactams, that could represent an important advantage in specific scenarios.
Ceftobiprole is approved for the treatment of community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP), excluding ventilator-associated pneumonia (VAP), in several European and non-European countries [Citation4–Citation6]. In this narrative review, we discuss its current place in therapy in light of the available literature, both within and outside approved indications.
2. Methods
During a remote meeting on December 2018, the structure of the present narrative review was decided, and divided in the following main chapters: (i) antimicrobial properties of ceftobiprole; (ii) pharmacological properties of ceftobiprole; (iii) use of ceftobiprole for pneumonia; (iv) use of ceftobiprole for other indications; (v) safety and tolerability of ceftobiprole. Subsequently, an inductive MEDLINE/PubMed search for relevant publications was conducted, using various combinations of dedicated keywords for each topic. Then, different teams of authors produced separated drafts addressing the different topics, that were later merged in a final manuscript reviewed and approved by all authors.
3. Antimicrobial properties of ceftobiprole
Ceftobiprole is an expanded-spectrum cephalosporin which, like other β-lactams, exerts its antibacterial activity by inhibition of the transpeptidase moiety of the penicillin binding proteins (PBPs). It exhibits tight binding to several different PBPs of Gram-positive and Gram-negative pathogens, and a most notable feature is the ability to inhibit also the PBPs that are resistant or poorly susceptible to conventional β-lactams, including PBP2a of methicillin-resistant Staphylococcus aureus (MRSA) and PBP2x of penicillin-resistant pneumococci (PRP) [Citation1–Citation3].
Concerning β-lactamases, ceftobiprole is stable to the PC1 staphylococcal penicillinase, to the class A broad-spectrum β-lactamases of the TEM type (less so to those of the SHV type and to the K1 β-lactamase of Klebsiella oxytoca), and to the chromosomal AmpC-type β-lactamases of Enterobacterales and P. aeruginosa. Similar to third- and fourth generation cephalosporins, ceftobiprole is degraded by class A extended-spectrum β-lactamases (ESBLs) (e. g. CTX-M-15) and by carbapenemases (both serine-carbapenemases, such as KPC-2, and metallo-carbapenemases, such as IMP-1 and VIM-2), and is also degraded by some class D enzymes (e. g. OXA-10) [Citation7].
Altogether, these features account for a broad spectrum of antimicrobial activity which covers staphylococci (including methicillin-resistant strains of S. aureus and of coagulase-negative staphylococci), streptococci (including PRP strains), Haemophilus influenzae, Moraxella catarrhalis, most members of the order Enterobacterales, and also P. aeruginosa and Enterococcus faecalis. On the other hand, ceftobiprole has reduced or no activity against Enterococcus faecium, Acinetobacter baumannii, Burkholderia cepacia complex, Stenotrophomonas maltophilia, Proteus vulgaris, most Gram-negative anaerobes (e. g. Bacteroides fragilis group and Prevotella spp.), and strains of Enterobacterales producing acquired ESBLs or carbapenemases [Citation2,Citation8–Citation10]. The activity against methicillin-resistant staphylococci and PRP, which is outstanding compared to that of conventional β-lactams, has led to classification of ceftobiprole among the fifth generation of cephalosporins [Citation11].
Large surveillance studies carried out during the past decade on clinical isolates from different geographic regions have shown a remarkable activity of ceftobiprole against staphylococci and pneumococci, including methicillin-resistant and penicillin-resistant isolates, respectively. In particular, for MRSA and pneumococci, MIC90 values of 2 and 0.5 mg/L, respectively, have been reported, with susceptibility rates consistently exceeding 95% and 99%, respectively (). Strains of MRSA resistant to ceftobiprole are uncommon, and usually exhibit an MIC of 4 mg/L, i. e. only two-fold higher than the EUCAST breakpoint for susceptibility (European Committee on Antimicrobial Susceptibility Testing [EUCAST] clinical breakpoint tables, version 9.0, 2019; http://www.eucast.org) [Citation12–Citation16]. Against Enterobacterales, MIC90 values ≥16 mg/L have been reported, with variable susceptibility rates () [Citation12–Citation18], depending on the prevalence of ESBL and carbapenemase producers. No clinical breakpoints are yet available for CoNS, streptococci other than pneumococci, E. faecalis, H. influenzae, M. catarrhalis, and P. aeruginosa. However, considering the EUCAST PK/PD breakpoint for susceptibility of 4 mg/L and the MIC90 values of these pathogens () [Citation12–Citation18], also these species could be considered among the potential targets for this antibiotic.
Table 1. Ceftobiprole activity against clinical isolates of various bacterial species, from large surveillance studies.
In vitro studies have shown that ceftobiprole can be synergistic with daptomycin against MSSA, MRSA and methicillin-resistant Staphylococcus epidermidis strains [Citation19,Citation20] and with amikacin and levofloxacin against P. aeruginosa [Citation21].
Ceftobiprole was also shown to have notable activity against methicillin-susceptible and methicillin-resistant strains of S. aureus and S. epidermidis grown as biofilms, alone and in combination with rifampin or vancomycin [Citation22], suggesting potential activity against infections associated with biofilm growth (e.g. infections of devices). Indeed, ceftobiprole showed remarkable activity against staphylococcal isolates from foreign body-associated infections and prosthetic joint infections [Citation23,Citation24].
4. Pharmacological properties of ceftobiprole
Ceftobiprole is the active moiety of the water-soluble prodrug ceftobiprole medocaril, which is rapidly activated in plasma by type A esterases [Citation25,Citation26].
Similar to other cephalosporins, ceftobiprole exhibits time-dependent antibacterial activity. It has been shown in experimental infection models that maintenance of plasma concentrations above the MIC for 30% to 60% of the dosing interval (t> MIC) may guarantee effective bactericidal activity, in terms of >2–3 log10 decrease in CFU over 24 h, against S. aureus, S. pneumoniae and wild-type Enterobacterales [Citation27]. Noteworthy, the pharmacodynamic target of ceftobiprole against S. aureus in experimental pneumonia models was very similar (t> MIC of 40%) among phenotypically diverse strains (methicillin-susceptible S. aureus, community-associated (CA)-MRSA and healthcare-acquired (HA)-MRSA) [Citation28].
Ceftobiprole is administered intravenously at the dosage of 500 mg q8h infused over 2 h. The pharmacokinetic parameters of ceftobiprole in healthy volunteers are summarized in [Citation25,Citation29]. Similar to several other beta-lactams, ceftobiprole is poorly bound to plasma protein (16%) and has a Vd which is similar to the extracellular compartment. Penetration of ceftobiprole was evaluated into the epithelial lining fluid (ELF) and into soft tissues of healthy volunteers. Mean penetration (calculated as tissue-to-plasma AUCs ratio) was 25.5% into the ELF [Citation30], 69% and 49% into skeletal muscle and adipose tissue, respectively [Citation31]. Ceftobiprole has a low potential for drug–drug interaction, a short elimination half-life and is excreted almost completely as unmodified moiety by the renal route. Dosage adjustments are needed in patients with renal impairment (500 mg q12h over 2 h, 250 mg q12h over 2 h, 250 q24h over 2 h in presence of CLCr 30–50 mL/min, <30 mL/min and end stage renal disease or intermittent hemodialysis, respectively) [Citation32]. A recent PK analysis carried out in a single case of critically ill patient undergoing continuous-veno-venous-hemodiafiltration (CVVHDF) suggested that a ceftobiprole dosage of 250 mg q12h over 2 h may allow appropriate target attainment in terms of maintenance of 100% t> MIC [Citation33]. In patients with augmented renal clearance (>130 mL/min/1.73 m2), the infusion time of ceftobiprole must be extended up to 4 h for optimizing drug exposure [Citation29,Citation32].
Table 2. Pharmacokinetic (PK) parameters of ceftobiprole after single 500 mg intravenous dose over 2 h infusion in healthy volunteers [Citation25,Citation29].
The relationship between ceftobiprole exposure and microbiological and/or clinical outcomes was analyzed in patients with nosocomial pneumonia by using data from a randomized double-blind phase 3 clinical trial [Citation34]. Multiple logistic regression analysis showed a strong correlation, and CART analysis determined that the percentage of t> MIC needed for obtaining favorable clinical outcome was of 51% of the dosing interval, a value which is in line with those found in preclinical models [Citation34]. A Monte Carlo simulation showed that at this percentage of t> MIC, pharmacokinetic data coming from phase 1 study in healthy volunteers accurately predicted the actual clinical exposure to ceftobiprole in patients who were enrolled in the phase 3 nosocomial pneumonia study, the difference being very small (3.5% for PK-sampled patients) [Citation35].
A recent population pharmacokinetic/pharmacodynamic analysis demonstrated that at the standard ceftobiprole dose of 500 mg every 8 h as a 2-h infusion no pharmacokinetic or pharmacodynamic differences existed between Asian and non-Asian subjects, considering that, at a pharmacodynamic target of 60% t> MIC of the dosing interval, more than 90% of the population was adequately exposed in both subgroups [Citation36].
5. Use of ceftobiprole in patients with pneumonia
Within in-label indications, ceftobiprole is an important option for the empirical treatment of patients with CAP and HAP, given its activity against MRSA, Enterobacterales, and P. aeruginosa.
The approval of ceftobiprole for CAP and HAP is based on two phase 3 randomized controlled trials (RCT) [Citation37,Citation38]. The first one, published in 2011, was a non-inferiority, double-blind RCT comparing ceftobiprole vs. ceftriaxone (plus optional linezolid, based on investigators’ suspicion of MRSA involvement) for the treatment of severe CAP requiring hospitalization and intravenous treatment [Citation38]. Ceftobiprole was administered q8h at 500 mg over a 120-min infusion, whereas ceftriaxone was administered once-daily at 2 g over a 30-min infusion. The minimum target duration of therapy was 7 days in both arms, with optional stepdown to oral cefuroxime at day 3 in case of significant improvement. The primary efficacy endpoint was clinical cure (defined either as resolution of signs and symptoms of infection or as sufficient improvement rendering continuation of antibacterial therapy unnecessary) at the test-of-cure (TOC) visit (7–14 days after the end of treatment) in the intention-to-treat (ITT) and the clinically evaluable (CE) populations. Overall, 706 patients were enrolled, 638 of whom were included in the ITT population. The CE population consisted of 469 patients. Clinical cure was achieved in 76.4% (240/314) and 79.3% (257/324) of ITT patients treated with ceftobiprole and with ceftriaxone ± linezolid, respectively (difference −2.9%, 95% confidence interval [CI] −9.3 to 3.6), and in 86.6% (200/231) and 87.4% (208/238) of CE patients treated with ceftobiprole and with ceftriaxone ± linezolid, respectively (difference −0.8%, 95% CI −6.9 to 5.3), meeting non-inferiority in both populations according to the pre-fixed 10% non-inferiority margin [Citation38].
The second registrative study, published in 2014, was a non-inferiority, double-blind, RCT comparing ceftobiprole vs. ceftazidime plus linezolid for the treatment of HAP and VAP [Citation37]. Ceftobiprole was administered q8h at 500 mg over a 120-min infusion, ceftazidime was administered q8h at 2 g over a 120-min infusion, and linezolid was administered q12h at 600 mg over a 60-min infusion. The planned treatment duration was 7 days, with a maximum of 14 days. The primary efficacy endpoint was clinical cure (defined either as resolution of signs and symptoms of infection or as sufficient improvement rendering continuation of antibacterial therapy unnecessary) at the TOC visit (7–14 days after the end of treatment) in the ITT and in the CE populations. The ITT and CE populations consisted of 781 (571 HAP and 210 VAP) and 495 (383 HAP and 112 VAP) patients, respectively. Clinical cure was achieved in 59.6% (171/287) and 58.8% (167/284) of ITT patients with HAP treated with ceftobiprole and with ceftazidime plus linezolid, respectively (difference 0.8%, 95% CI −7.3 to 8.8), and in 77.8% (154/198) and 76.2% (141/185) of CE patients treated with ceftobiprole and with ceftazidime plus linezolid, respectively (difference 1.6, 95% CI −6.9 to 10.0), meeting non-inferiority in both populations according to the pre-fixed 15% non-inferiority margin. Of note, in the CE population HAP patients treated with ceftobiprole showed a higher rate of early improvement (assessed at day 4 after the onset of therapy) than HAP patients treated with ceftazidime plus linezolid (86.9% [172/198] vs. 78.4% [145/185], respectively, difference 8.5%, 95% CI 0.9 to 16.1), with the largest difference being observed in patients with MRSA-positive cultures at baseline (94.7% [18/19] vs. 52.6% [10/19], respectively, difference 42.1%, 95% CI 17.5 to 66.7) [Citation37].
With regard to VAP patients, clinical cure rates were 23.1% (24/104) and 36.8% (39/106) in ITT patients treated with ceftobiprole and with ceftazidime plus linezolid, respectively (difference −13.7%, 95% CI −26.0 to −1.0), and in 37.7% (20/53) and 55.9% (33/59) in CE patients treated with ceftobiprole and with ceftazidime plus linezolid, respectively (difference −18.2%, 95% CI −36.4 to 0.0), failing to demonstrate non-inferiority [Citation37].
The reasons underlying failure in demonstrating non-inferiority of ceftobiprole vs. ceftazidime plus linezolid in patients with VAP are not perfectly clear. A possible unfavorable effect due to the presence biofilm-embedded organisms has been hypothesized, which is nonetheless in contrast with the higher rates of clinical cure observed in ceftobiprole-treated patients than in ceftazidime plus linezolid-treated patients in the subgroup of mechanically ventilated HAP (30.4% [21/69] vs. 27.1% [19/70] in the ITT population, difference 3.3%, 95% CI −11.8 to 18.3, and 55.3% [21/38] vs. 40.5% [15/37] in the CE population, difference 14.7%, 95% CI −7.6 to 37.1) [Citation37]. In addition, ceftobiprole demonstrated activity in an experimental model of foreign-body infection [Citation39]. An alternative explanation is the possibly insufficient attainment of therapeutic concentrations of ceftobiprole in patients with CLCr ≥150 ml/min, a condition encountered in as many as 29% of ceftobiprole-treated patients with VAP, and that might require higher dosages and prolonged infusions to achieve adequate therapeutic levels [Citation29,Citation32].
As regards post-hoc analyzes of patients with CAP or HAP in the two major trials, higher rates of early clinical improvement in patients treated with ceftobiprole than in those treated with comparators were observed overall and especially in CAP patients aged ≥75 years (difference 16.3%, 95% CI 1.8 to 30.8), CAP patients with chronic obstructive pulmonary disease (difference 20.1%, 95% CI 8.8 to 31.1), HAP patients considered to be at higher risk of poor outcomes according to previous literature (difference 12.5%, 95% CI 3.5 to 21.4), and HAP patients with >10 baseline comorbidities (difference 15.3%, 95% CI 0.3 to 30.4) [Citation40].
The main findings of the two registrative studies are also summarized in . Overall, on the basis of the high-level evidence provided by RCT, ceftobiprole is an effective β-lactam option for the treatment of patients with CAP or HAP, with the notable advantage of anti-MRSA and anti-PRP activity [Citation41]. Conversely, without further high-level evidence from dedicated RCT, the use of ceftobiprole for VAP cannot be supported.
Table 3. Efficacy data from phase 3, non-inferiority, randomized clinical trials in patients with CAP and HAP/VAP.
6. Use of ceftobiprole for other indications
The use of ceftobiprole outside approved indications could be justified in specific, non-mutually exclusive scenarios: (i) when other approved alternatives are ineffective (e.g. resistance); (ii) when the risk of toxicity or allergic reactions is unacceptable; (iii) for salvage therapy. In the literature, the use of ceftobiprole for indications other than pneumonia has been reported in patients with skin and soft tissue infections, bloodstream infections, infective endocarditis, mediastinitis, and osteomyelitis [Citation42–Citation47].
6.1. Skin and soft tissue infections
In a mouse subcutaneous abscess model, ceftobiprole showed a more potent activity than vancomycin or linezolid against MRSA and VISA [Citation2]. In healthy volunteers, in vivo microdialysis techniques have evidenced adequate penetration of ceftobiprole in soft tissues, with prediction of optimal activity against organisms with MIC up to 2 mg/L [Citation31].
From 2004 to 2005, a phase 3, non-inferiority, double-blind RCT was conducted in 129 sites worldwide, in patients with suspected or documented Gram-positive complicated skin and soft tissue infections (cSSTI) [Citation46]. Patients were randomized to receive either ceftobiprole at 500 mg q12h or vancomycin at 1 g q12h. The duration of treatment was 7–14 days. Diabetic foot infections, bite wound infection, and osteomyelitis were excluded. The primary endpoint was clinical cure at the TOC visit (7–14 days after the end of treatment). The non-inferiority margin was set at 10%. In the ITT population, clinical cure was achieved in 77.8% (309/397) and 77.5% (300/387) of patients treated with ceftobiprole and vancomycin, respectively (difference 0.3%, 95% CI −5.5 to 6.1). In the CE population, clinical cure was achieved in 93.3% (263/282) and 93.5% (259/277) of patients treated with ceftobiprole and vancomycin, respectively (difference −0.2%, 95% CI −4.4 to 3.9) [Citation46].
From 2005 to 2006 another phase 3, double-blind, RCT was conducted in patients with cSSTI caused by either Gram-positive or Gram-negative bacteria, comparing ceftobiprole vs. vancomycin plus ceftazidime [Citation45]. Ceftobiprole was administered at 500 mg q8h, vancomycin was administered at 1 g q12h, and ceftazidime was administered at 1 g q8h. The primary endpoint was clinical cure at the TOC visit (7–14 days after the end of treatment). The non-inferiority margin was set at 10%. In the ITT population, clinical cure was achieved in 81.9% (448/547) and 80.8% (227/281) of patients treated with ceftobiprole and vancomycin plus ceftazidime, respectively (difference 1.1%, 95% CI −4.5 to 6.7). In the CE population, clinical cure was achieved in 90.5% (439/485) and 90.2% (220/244) of patients treated with ceftobiprole and vancomycin plus ceftazidime, respectively (difference 0.3%, 95% CI −4.2 to 4.9) [Citation45].
However, despite the results of these two RCT suggested that ceftobiprole was beneficial to patients, it should be noted that authorization for SSTI was ultimately not granted. This decision was based on the lack of compliance with good clinical practice (GCP) recommendations registered in some participating sites in the United States [Citation48]. A novel phase 3, non-inferiority, double-blind RCT comparing ceftobiprole vs. vancomycin plus aztreonam for the treatment of acute bacterial skin and skin structure infections (ABSSSI) has been initiated and is currently ongoing (NCT03137173).
6.2. Bacteremia, endocarditis, and mediastinitis
The interest in using ceftobiprole for the treatment of bacteremia and endocarditis is increased by the results of rat and rabbit models of infective endocarditis (IE) due to MRSA, which showed a bactericidal effect possibly higher than that of linezolid and daptomycin [Citation49,Citation50]. Therapy with ceftobiprole was also successful in a rat model of mediastinitis, induced by the injection of MRSA into the sternal bone [Citation51]. A higher reduction in MRSA load after 5 days of therapy was observed in rats receiving ceftobiprole in comparison with rats receiving vancomycin. At day 14 of treatment, there was evidence of complete/most complete MRSA sternal clearance in both ceftobiprole-treated and vancomycin-treated rats [Citation51].
Regarding the available evidence in humans, some information about the efficacy of ceftobiprole for the treatment of staphylococcal bacteremia can be extrapolated from existent RCT. In a post-hoc pooled analysis of four phase 3 double-blind RCT (two in patients with cSSTI, one in patients with CAP, and one in patients with HAP/VAP) [Citation37,Citation38,Citation45,Citation46], which was presented at the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) congress in 2016, clinical cure rates and 30-day all-cause mortality were compared between patients with staphylococcal bacteremia treated with ceftobiprole and patients with staphylococcal bacteremia treated with the different comparators (vancomycin and vancomycin plus ceftazidime in cSSTI trials, ceftriaxone ± linezolid in the CAP trial, and ceftazidime plus linezolid in the HAP/VAP trial) [Citation52]. Cumulatively, 95 patients had staphylococcal bacteremia in the four RCT. With the limitation of the small sample size, both clinical cure rates and 30-day all-cause mortality were similar between patients treated with ceftobiprole and patients treated with the comparators (for clinical cure, 48.9% [22/45] vs. 44.0% [22/50], respectively, difference 4.9%, 95% CI −12.2 to 25.0; for 30-day all-cause mortality, 8.9% [4/45] vs. 16.0% [8/50], respectively, difference −7.1%, 95% CI −20.2 to 6.0). Of note, a trend toward higher rates of favorable outcomes was observed in ceftobiprole-treated vs. comparator/s-treated patients in the subgroup of patients with MRSA bacteremia, although the very small denominator (n = 18) precludes generalization (for clinical cure, 55.6% [5/9] vs. 22.2% [2/9], respectively, difference 33.3%, 95% CI −9.0 to 77.7; for 30-day all-cause mortality, 0.0% [0/9] vs. 22.2% [2/9], respectively, difference −22.2%, 95% CI −49.4 to 4.9) [Citation52].
No evidence from RCT is available regarding the efficacy of ceftobiprole for the treatment of infective endocarditis. However, a non-inferiority, double-blind, RCT comparing ceftobiprole vs. daptomycin for the treatment of S. aureus bacteremia, including right-sided infective endocarditis, is currently being conducted in adult patients (NCT03138733), and could open the door to the future approval of ceftobiprole for these indications should non-inferiority be demonstrated.
With regard to observational studies, 10 episodes of severe MRSA infection treated with ceftobiprole (of which 7/10 were bacteremia and 3/10 were pneumonia) were reported in a single-center retrospective case series in Canada [Citation42]. Microbiological eradication was observed in 9/10 patients treated with ceftobiprole, including two bacteremic cases of salvage therapy following previous treatment failure with vancomycin, and one bacteremic case of salvage therapy following previous treatment failure with linezolid. Of note, breakthrough bacteremia was observed in a patient in whom ceftobiprole was underdosed due to a medication error. Overall, a favorable outcome was observed in 8/10 episodes (80%) [Citation42].
Two case reports describing the successful treatment with ceftobiprole of patients with IE have also been published [Citation43,Citation47]. The first case involved a patient with severe pancytopenia after autologous hematopoietic stem cells transplantation (HSCT) for Burkitt lymphoma and recurrent bacteremia due to methicillin-resistant Staphylococcus epidermidis (MRSE) in presence of a prosthetic endovascular infection of the aortic valve and the ascending aorta, which responded favorably to ceftobiprole monotherapy [Citation43]. After blood cultures turned negative, the patient underwent halogenic HSCT without episodes of breakthrough bacteremia in the postoperative period. Ceftobiprole was discontinued 3 months after allogeneic HSCT, and no radiological or clinical signs of infection were detected during a 1-year follow-up [Citation43].
The second case involved a patient with renal insufficiency and aortic valve replacement complicated by MRSA mediastinitis [Citation47]. After several failed courses of antimicrobials, a combination regimen of daptomycin plus ceftobiprole was initiated, with favorable response (the patient became afebrile) and subsequent valve surgery [Citation47]. The use of combination therapy (ceftobiprole plus daptomycin) was in line with in vitro studies reporting a potent synergy between ceftobiprole and daptomycin [Citation19,Citation20]. This is an intriguing possibility to be further investigated in clinical studies, since it could represent an important option for salvage therapy of MRSA bacteremia and/or endocarditis. Of note, synergy between ceftobiprole and daptomycin has also been demonstrated against enterococci, including vancomycin-resistant isolates [Citation20,Citation53]. However, the related evidence is currently limited to in vitro studies, and further evidence from either animal models or clinical studies is needed regarding the possible use of ceftobiprole/daptomycin combinations for severe enterococcal infections in humans.
6.3. Osteomyelitis
Ceftobiprole showed potent activity against MRSA and methicillin-resistant coagulase-negative staphylococci isolates from bone and joint infections in an in vitro study, as well as in a rabbit model of CA-MRSA osteomyelitis [Citation54,Citation55]. The interest in using ceftobiprole for osteomyelitis and prosthetic joint infections also relies of its synergy with rifampin observed against biofilms [Citation22].
An experience about the use of ceftobiprole for osteomyelitis was reported in 2010 [Citation44]. A diabetic patient with a septic arthritis and bone destruction, with MRSA and Peptostreptococcus prevotii isolation and involving both the second and third metatarsophalangeal joints at the right foot, was initially treated with vancomycin and piperacillin/tazobactam, later replaced by ceftobiprole monotherapy due to kidney failure [Citation44]. The patient underwent excision of the second and third metatarsal heads and was successfully treated with intravenous ceftobiprole for a total duration of 42 days including the postoperative period, with no evidence of relapsed osteomyelitis after a 1-year follow-up [Citation44]. However, there could have been a major role of infected tissue removal in favorably influencing clinical cure, thus more supportive clinical evidence is warranted.
7. Safety and tolerability of ceftobiprole
Safety and tolerability of ceftobiprole were first assessed in phase 1 trials [Citation26,Citation56]. In a single dose-increasing study, caramel-like dysgeusia, attributable to a diacetyl product of conversion, was the only relevant mild adverse event (AE) observed [Citation26]. In two subsequent phase 1 trials, nausea, vomiting and headache were reported as dose-related events [Citation57].
Data from phase 2 and phase 3 studies involved a total of 3037 patients (1668 receiving ceftobiprole and 1369 receiving the comparator/s) [Citation58]. Pooled data from pneumonia studies included a total of 1404 patients (696 receiving ceftobiprole and 708 the comparator/s). Ceftobiprole was generally well tolerated with a low discontinuation rate due to AE drug-related, similar to that observed with the comparator/s (10.3% vs. 7.3% for ceftobiprole vs. comparator/s, overall; 14.0% vs. 10.4% in the HAP/VAP phase 3 trial and 5.8% vs. 3.7% in the CAP phase 3 trials). Most patients reported at least one AE (74.1% in the ceftobiprole and 71.8% comparator arm, respectively), with rates being 77.5% in the ceftobiprole arm vs. 77.7% in the comparators arm in the HAP/VAP trial, and 70.0% in the ceftobiprole arm vs. 64.6% in the comparator/s arm in the CAP trial [Citation58].
Overall, the most common AEs (≥3% of patients) reported with ceftobiprole from the pooled analysis of HAP, CAP or cSSTI studies were nausea, vomiting, diarrhea, infusion site reactions, dysgeusia and drug-related hypersensitivity (urticaria, pruritus, and rash) [Citation58].
In the phase 3 CAP RCT, the overall AE rate was 36% in the ceftobiprole group vs. 26% in the ceftriaxone ± linezolid comparator group [Citation38]. This difference was mainly related to higher occurrence of nausea (7% vs. 2%) and vomiting (5% vs. 2%) in the ceftobiprole group, whereas occurrence of injection-site AEs (7% vs. 5%), hyponatremia (1% vs. 3%) and hepatic AEs (7% vs. 7%) were similar in both groups.
In the phase 3 HAP/VAP RCT the overall AE rate was 24.9% in the ceftobiprole group vs. 25.4% in the ceftazidime plus linezolid group [Citation37]. Diarrhea was less frequently reported in the ceftobiprole arm (3.1% and 6.5%), whereas hyponatremia was more frequent in patients treated with ceftobiprole than in those receiving the comparators (4.4% and 2.6%, respectively). In patients treated with ceftobiprole, dysgeusia occurred only in 1.3% of cases. No other clinically relevant differences in laboratory values, vital signs, physical examinations, or electrocardiograms were observed between the treatment arms.
Overall, Clostridioides difficile colitis was rare in ceftobiprole-treated patients in RCT. This is possibly related to the valid inhibitory activity that ceftobiprole exhibits against C. difficile [Citation59]. This hypothesis is supported by the fact that ceftobiprole was shown to have no significant ecological impact on the human intestinal microflora of healthy volunteers [Citation60]. Additionally, in experimental models, ceftobiprole did not promote neither growth of nor toxin production by C. difficile in mouse cecal contents, differently from what occurred with other cephalosporins (ceftazidime, cefoxitin, ceftriaxone, cefotaxime) and with carbapenems (ertapenem) [Citation59].
8. Conclusion
Ceftobiprole is an important option for the treatment of CAP and HAP when MRSA is suspected or involved. In the near future, ongoing RCT and further observational experiences could both enlarge the current panel of approved indications and enrich our knowledge on its use for off-label indications.
9. Expert opinion
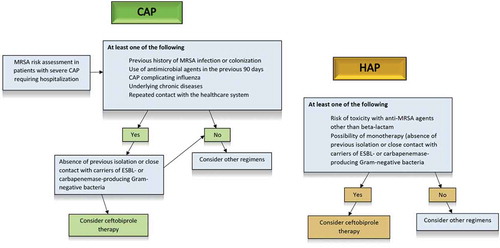
There are three main and non-mutually exclusive reasons which render ceftobiprole an attractive option for the empirical and targeted treatment of CAP and HAP: (i) its broad spectrum of activity; (ii) its activity against MRSA; (iii) its good safety profile. For example, these advantages should be taken into account when dealing with HAP in hospitalized patients with multiple comorbidities and at risk both of MRSA infection and of adverse events due non-β-lactam anti-MRSA agents. Another suitable scenario for ceftobiprole therapy could be that of severe CAP complicating influenza, in which empirical coverage of CA-MRSA should be guaranteed [Citation61]. On the other hand, costs and antimicrobial stewardship principles (which dictate against the use of anti-MRSA agents in absence of substantial risk, in order to avoid useless selective pressure) indicate that ceftobiprole should not be overused, but rather employed thoughtfully in those scenarios in which its intrinsic advantages could be maximized. Based on these premises, a potential treatment algorithm for guiding clinicians’ decisions regarding the use of ceftobiprole in CAP and HAP is depicted in .
Figure 1. Algorithm illustrating the possible use of ceftobiprole for empirical therapy in patients with CAP and HAP (non-VAP).
CAP, community-acquired pneumonia; ESBL, extended-spectrum β-lactamases; HAP, hospital-acquired pneumonia; MRSA, methicillin-resistant Staphylococcus aureus; VAP, ventilator-associated pneumonia.
Another framework in which ceftobiprole could represent a reasonable choice at the present time is the salvage therapy of bacteremia and endocarditis (despite not approved) due to MRSA after failure of vancomycin or daptomycin therapy. In such a case, the possible advantage of a salvage combination of ceftobiprole plus either daptomycin or vancomycin lies in the synergy observed in vitro studies [Citation11], for which several possible mechanisms have been described. Amongst others are the reduced expression of the mecA gene and the inhibitory effect on the early stages of the peptidoglycan synthesis by daptomycin [Citation62], the reduction in the cell surface charge by β-lactams that might favor daptomycin binding [Citation63], and the seesaw effect enhancing activity of β-lactams in case of isolates with increased daptomycin or vancomycin MIC [Citation11,Citation64]. It should nonetheless be noted that, despite the use this strategy could be considered after failure of standard therapy, the related evidence from clinical studies remains limited, and further experience is thus warranted to determine its true efficacy. Notably, also the use of ceftobiprole monotherapy may be considered in the future for the treatment of MRSA bacteremia, not only as salvage therapy but also possibly as a primary therapeutic approach, in case of favorable results from ongoing RCT (NCT03138733). The possible synergistic activity of ceftobiprole and daptomycin against some strains of vancomycin-resistant enterococci, suggested in a preliminary in vitro study, deserves further investigation [Citation65].
In the next five years, we expect to witness an increasing number of observational studies and case reports about the use of ceftobiprole for currently off-label indications such as bacteremia, endocarditis, osteomyelitis, and mediastinitis. In addition, results of phase 3 RCT on ABSSSI and S. aureus bacteremia (NCT03137173 and NCT03138733) are much awaited and may provide important high-evidence efficacy data regarding the use of ceftobiprole for these potential, additional indications.
Article highlights
Ceftobiprole is a fifth-generation cephalosporin with a broad spectrum of antimicrobial activity, including also MRSA, and is approved for the treatment of CAP and HAP, excluding VAP, in several European and non-European countries.
On the basis of the high-level evidence provided by RCT, ceftobiprole is an effective β-lactam option for the treatment of patients with CAP or HAP, with the notable advantage of anti-MRSA activity.
In the literature, the use of ceftobiprole for indications other than pneumonia has been reported in patients with skin and soft tissue infections, bloodstream infections, infective endocarditis, mediastinitis, and osteomyelitis.
In the near future, ongoing RCT and further observational experiences could both enlarge the current panel of approved indications and enrich our knowledge on its use for off-label indications...
Declaration of interest
Outside the submitted work, DR Giacobbe reports honoraria from Stepstone Pharma GmbH and an unconditioned grant from MSD Italia. Outside the submitted work, FG De Rosa has received speaker grant and has participated in advisory board for Correvio and Basilea. Outside the submitted work, V Del Bono has received funding for scientific advisory boards, travel, and speaker honoraria from MSD, Pfizer, Basilea, Hikma, Gilead. Outside of the submitted work, PA Glossi has served as a speaker for Merck Sharp and Dohme, Biotest, Pfizer, Angelini. Novartis, Gilead and as a consultant in Advisory Boards for Merck Sharp and Dohme, Biotest, Becton Dickinson, Angelini, Gilead, Paratek and Shire. Outside the submitted work, F Pea participated in advisory boards and/or received speaker honoraria from Angelini, Basilea Pharmaceutica, Correvio, Gilead, Hikma, Merck Sharp & Dohme, Nordic Pharma, Pfizer, Sanofi Aventis, and Shionogi. Outside the submitted work, N Petrosillo received fees as speaker from Merck Sharp and Dohme, Pfizer, Cepheid. Angelini, Zambon, Gilead, Accelerate, Johnson & Johnson, Becton & Dickinson, Takeda, Shionogi, and participated in advisory boards for MSD, Shionogi, Pfizer. Outside of the submitted work, GM Rossolini has received honoraria for scientific advisory boards, and/or travel and/or speakers bureau from Accelerate, Achaogen, Angelini, AstraZeneca, Basilea, Beckman Coulter, Becton-Dickinson, bioMérieux, Biotest, Cepheid, Copan, Cubist, Curetis, Elitech, Menarini, Merck, Nordic Pharma, Novartis, Pfizer, Qpex, Rempex, Roche, Shionogi, ThermoFisher, VenatorX, Zambon; and research grants to the laboratory from Accelerate, Alifax, Angelini, Arrow, AstraZeneca, Basilea, Becton-Dickinson, bioMérieux, Biotest, Cepheid, Checkpoints, DID, Elitech, Estor, GenePoc, Hain Lifesciences, Liofilchem, Menarini, Merck, Nordic Pharma, Novartis, Pfizer Rempex, Seegene, Shionogi, Symcel, VenatorX, Zambon. Outside the submitted work, C Tascini has received funding for scientific advisory boards, travel and speaker honoraria from Angelini. Basilea, BioMérieux. Biotest, Correvio, MSD, Pfizer, ThermoFisher, and Zambon. Outside the submitted work, M Tumbarello has been scientific advisor/consultant for Angelini, MSD, Nordic Pharma and Roche, and speaker/chairman at accredited educational courses funded by unrestricted grants from Astellas, Gilead, MSD and Pfizer. For activities outside of the submitted work, P Viale has served as a consultant for MSD, Pfizer, VenatoRx, Nabriva, Gilead, ThermoFisher, and BioMérieux, and received payment for serving on the speaker’s bureau for MSD, Pfizer, Correvio, and Gilead. Outside the submitted work, M Bassetti has received funding for scientific advisory boards, travel and speaker honoraria from Angelini, Astellas, AstraZeneca, Basilea, Bayer, BioMerieux, Cidara, Correvio, Cubist, Menarini, Molteni, MSD, Nabriva, Paratek, Pfizer, Roche, Shionogi, Tetraphase, Thermo Fisher, and The Medicine Company. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
A peer reviewer on this manuscript has disclosed that they are a member of the AVIR Pharma advisory board. AVIR distributes ceftobiprole for Basilea in Canada. They have also received honoraria from AVIR Pharma for educational sessions.
Additional information
Funding
References
- Davies TA, Page MG, Shang W, et al. Binding of ceftobiprole and comparators to the penicillin-binding proteins of Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, and Streptococcus pneumoniae. Antimicrob Agents Chemother. 2007;51(7):2621–2624.
- Hebeisen P, Heinze-Krauss I, Angehrn P, et al. In vitro and in vivo properties of Ro 63-9141, a novel broad-spectrum cephalosporin with activity against methicillin-resistant staphylococci. Antimicrob Agents Chemother. 2001;45(3):825–836.
- Lovering AL, Gretes MC, Safadi SS, et al. Structural insights into the anti-methicillin-resistant Staphylococcus aureus (MRSA) activity of ceftobiprole. J Biol Chem. 2012;287(38):32096–32102.
- Basilea reports launch of antibiotic Zevtera (ceftobiprole) in Argentina by Grupo Biotoscana. [cited 2019 Apr 26]. Available from: https://globenewswire.com/news-release/2018/03/06/1415442/0/en/Basilea-reports-launch-of-antibiotic-Zevtera-ceftobiprole-in-Argentina-by-Grupo-Biotoscana.html
- CISION. News. Cardiome announces agreement with Basilea for distribution of Zevtera®/Mabelio® (Ceftobiprole) in Europe and Israel. [ cited 2019 Apr 26]. Available from: https://www.newswire.ca/news-releases/cardiome-announces-agreement-with-basilea-fordistribution-of-zevteramabelio-ceftobiprole-in-europe-and-israel-643915603.html
- Falco V, Burgos J, Almirante B. Ceftobiprole medocaril for the treatment of community-acquired pneumonia. Expert Opin Pharmacother. 2018;19(13):1503–1509.
- Queenan AM, Shang W, Kania M, et al. Interactions of ceftobiprole with beta-lactamases from molecular classes A to D. Antimicrob Agents Chemother. 2007;51(9):3089–3095.
- Ednie L, Shapiro S, Appelbaum PC. Antianaerobe activity of ceftobiprole, a new broad-spectrum cephalosporin. Diagn Microbiol Infect Dis. 2007;58(1):133–136.
- Jones RN, Deshpande LM, Mutnick AH, et al. In vitro evaluation of BAL9141, a novel parenteral cephalosporin active against oxacillin-resistant staphylococci. J Antimicrob Chemother. 2002;50(6):915–932.
- Zbinden R, Punter V, von Graevenitz A. In vitro activities of BAL9141, a novel broad-spectrum pyrrolidinone cephalosporin, against gram-negative nonfermenters. Antimicrob Agents Chemother. 2002;46(3):871–874.
- Bal AM, David MZ, Garau J, et al. Future trends in the treatment of methicillin-resistant Staphylococcus aureus (MRSA) infection: an in-depth review of newer antibiotics active against an enduring pathogen. J Glob Antimicrob Resist. 2017;10:295–303.
- Farrell DJ, Flamm RK, Sader HS, et al. Ceftobiprole activity against over 60,000 clinical bacterial pathogens isolated in Europe, Turkey, and Israel from 2005 to 2010. Antimicrob Agents Chemother. 2014;58(7):3882–3888.
- Pfaller MA, Flamm RK, Duncan LR, et al. Antimicrobial activity of ceftobiprole and comparator agents when tested against contemporary Gram-positive and -negative organisms collected from Europe (2015). Diagn Microbiol Infect Dis. 2018;91(1):77–84.
- Pfaller MA, Flamm RK, Mendes RE, et al. Ceftobiprole activity against Gram-positive and -negative pathogens collected from the United States in 2006 and 2016. Antimicrob Agents Chemother. 2019;63:1.
- Rossolini GM, Dryden MS, Kozlov RS, et al. Comparative activity of ceftobiprole against Gram-positive and Gram-negative isolates from Europe and the Middle East: the CLASS study. J Antimicrob Chemother. 2011;66(1):151–159.
- Santerre Henriksen A, Smart JI, Hamed K. Susceptibility to ceftobiprole of respiratory-tract pathogens collected in the United Kingdom and Ireland during 2014-2015. Infect Drug Resist. 2018;11:1309–1320.
- Pillar CM, Aranza MK, Shah D, et al. In vitro activity profile of ceftobiprole, an anti-MRSA cephalosporin, against recent Gram-positive and gram-negative isolates of European origin. J Antimicrob Chemother. 2008;61(3):595–602.
- Walkty A, Adam HJ, Laverdiere M, et al. In vitro activity of ceftobiprole against frequently encountered aerobic and facultative Gram-positive and Gram-negative bacterial pathogens: results of the CANWARD 2007-2009 study. Diagn Microbiol Infect Dis. 2011;69(3):348–355.
- Barber KE, Werth BJ, Ireland CE, et al. Potent synergy of ceftobiprole plus daptomycin against multiple strains of Staphylococcus aureus with various resistance phenotypes. J Antimicrob Chemother. 2014;69(11):3006–3010.
- Campanile F, Bongiorno D, Mongelli G, et al. Bactericidal activity of ceftobiprole combined with different antibiotics against selected Gram-positive isolates. Diagn Microbiol Infect Dis. 2019;93(1):77–81.
- Kresken M, Korber-Irrgang B, Lauffer J, et al. In vitro activities of ceftobiprole combined with amikacin or levofloxacin against Pseudomonas aeruginosa: evidence of a synergistic effect using time-kill methodology. Int J Antimicrob Agents. 2011;38(1):70–75.
- Abbanat D, Shang W, Amsler K, et al. Evaluation of the in vitro activities of ceftobiprole and comparators in staphylococcal colony or microtitre plate biofilm assays. Int J Antimicrob Agents. 2014;43(1):32–39.
- Hischebeth GTR, Gravius S, Molitor E, et al. Activity of ceftobiprole against Staphylococcus spec. isolates derived from foreign body associated infections. Diagn Microbiol Infect Dis. 2018;91(2):175–178.
- Isnard C, Dhalluin A, Malandain D, et al. In vitro activity of novel anti-MRSA cephalosporins and comparator antimicrobial agents against staphylococci involved in prosthetic joint infections. J Glob Antimicrob Resist. 2018;13:221–225.
- Murthy B, Schmitt-Hoffmann A. Pharmacokinetics and pharmacodynamics of ceftobiprole, an anti-MRSA cephalosporin with broad-spectrum activity. Clin Pharmacokinet. 2008;47(1):21–33.
- Schmitt-Hoffmann A, Roos B, Schleimer M, et al. Single-dose pharmacokinetics and safety of a novel broad-spectrum cephalosporin (BAL5788) in healthy volunteers. Antimicrob Agents Chemother. 2004;48(7):2570–2575.
- Craig WA, Andes DR. In vivo pharmacodynamics of ceftobiprole against multiple bacterial pathogens in murine thigh and lung infection models. Antimicrob Agents Chemother. 2008;52(10):3492–3496.
- Laohavaleeson S, Tessier PR, Nicolau DP. Pharmacodynamic characterization of ceftobiprole in experimental pneumonia caused by phenotypically diverse Staphylococcus aureus strains. Antimicrob Agents Chemother. 2008;52(7):2389–2394.
- Torres A, Mouton JW, Pea F. Pharmacokinetics and dosing of ceftobiprole medocaril for the treatment of hospital- and community-acquired pneumonia in different patient populations. Clin Pharmacokinet. 2016;55(12):1507–1520.
- Rodvold KA, Nicolau DP, Lodise TP, et al. Identifying exposure targets for treatment of staphylococcal pneumonia with ceftobiprole. Antimicrob Agents Chemother. 2009;53(8):3294–3301.
- Barbour A, Schmidt S, Sabarinath SN, et al. Soft-tissue penetration of ceftobiprole in healthy volunteers determined by in vivo microdialysis. Antimicrob Agents Chemother. 2009;53(7):2773–2776.
- Syed YY. Ceftobiprole medocaril: a review of its use in patients with hospital- or community-acquired pneumonia. Drugs. 2014;74(13):1523–1542.
- Cojutti PG, Merelli M, De Stefanis P, et al. Disposition of ceftobiprole during continuous venous-venous hemodiafiltration (CVVHDF) in a single critically ill patient. Eur J Clin Pharmacol. 2018;74(12):1671–1672.
- Muller AE, Punt N, Mouton JW. Exposure to ceftobiprole is associated with microbiological eradication and clinical cure in patients with nosocomial pneumonia. Antimicrob Agents Chemother. 2014;58(5):2512–2519.
- Muller AE, Schmitt-Hoffmann AH, Punt N, et al. Monte Carlo simulations based on phase 1 studies predict target attainment of ceftobiprole in nosocomial pneumonia patients: a validation study. Antimicrob Agents Chemother. 2013;57(5):2047–2053.
- Muller AE, Punt N, Engelhardt M, et al. Pharmacokinetics and Target Attainment of Ceftobiprole in Asian and Non-Asian Subjects. Clin Pharmacol Drug Dev. 2018;7(7):781–787.
- Awad SS, Rodriguez AH, Chuang YC, et al. A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia. Clin Infect Dis. 2014;59(1):51–61.
- Nicholson SC, Welte T, File TM Jr., et al. A randomised, double-blind trial comparing ceftobiprole medocaril with ceftriaxone with or without linezolid for the treatment of patients with community-acquired pneumonia requiring hospitalisation. Int J Antimicrob Agents. 2012;39(3):240–246.
- Vaudaux P, Gjinovci A, Bento M, et al. Intensive therapy with ceftobiprole medocaril of experimental foreign-body infection by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2005;49(9):3789–3793.
- Scheeren TWL, Welte T, Saulay M, et al. Early improvement in severely ill patients with pneumonia treated with ceftobiprole: a retrospective analysis of two major trials. BMC Infect Dis. 2019;19(1):195.
- Bassetti M, Righi E, Vena A, et al. Risk stratification and treatment of ICU-acquired pneumonia caused by multidrug- resistant/extensively drug-resistant/pandrug-resistant bacteria. Curr Opin Crit Care. 2018;24(5):385–393.
- Chaubey V, Dalton B, Sabuda D, et al. Abstract SP26: Ceftobiprole use in methicillin resistant Staphylococcus aureus (MRSA) bacteremia and pneumonia. CACMID-AMMI Canada 2010).
- Esposito F, Efthymiou A, Van Delden C, et al. Ceftobiprole as an ultimate successful therapy for MRSE prosthetic endovascular infection judged to be medically untreatable in a profound immunocompromised patient: a case report. Joint annual meeting 2018. Swiss Societies for Infectious Diseases (SSI), Hospital Hygiene (SSHH), Tropical Medicine and Parasitology (SSTMP) and Tropical and Travel Medicine (SSTTM); September 13-14, 2018; Interlaken, Switzerland. Poster P88.
- Macdonald A, Dow G. Ceftobiprole: first reported experience in osteomyelitis. Can J Infect Dis Med Microbiol. 2010;21(3):138–140.
- Noel GJ, Bush K, Bagchi P, et al. A randomized, double-blind trial comparing ceftobiprole medocaril with vancomycin plus ceftazidime for the treatment of patients with complicated skin and skin-structure infections. Clin Infect Dis. 2008;46(5):647–655.
- Noel GJ, Strauss RS, Amsler K, et al. Results of a double-blind, randomized trial of ceftobiprole treatment of complicated skin and skin structure infections caused by gram-positive bacteria. Antimicrob Agents Chemother. 2008;52(1):37–44.
- Oltolini C, Castiglioni B, Tassan Din C, et al. Meticillin-resistant Staphylococcus aureus endocarditis: first report of daptomycin plus ceftobiprole combination as salvage therapy. Int J Antimicrob Agents. 2016;47(6):502–504.
- European Medicines Agency, 2010 [cited 2019 Apr 26]. Available from: https://www.ema.europa.eu/en/documents/smop-initial/questions-answers-recommendation-refusal-marketing-authorisation-zeftera_en-0.pdf
- Entenza JM, Veloso TR, Vouillamoz J, et al. In vivo synergism of ceftobiprole and vancomycin against experimental endocarditis due to vancomycin-intermediate Staphylococcus aureus. Antimicrob Agents Chemother. 2011;55(9):3977–3984.
- Tattevin P, Basuino L, Bauer D, et al. Ceftobiprole is superior to vancomycin, daptomycin, and linezolid for treatment of experimental endocarditis in rabbits caused by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2010;54(2):610–613.
- Barnea Y, Navon-Venezia S, Kuzmenko B, et al. Ceftobiprole medocaril is an effective treatment against methicillin-resistant Staphylococcus aureus (MRSA) mediastinitis in a rat model. Eur J Clin Microbiol Infect Dis. 2014;33(3):325–329.
- Rello J, Rahav G, Scheeran T, et al. A pooled analysis of clinical cure and mortality with ceftobiprole medocaril versus comparators in staphylococcal bacteraemia in complicated skin infections, and community- and hospital-acquired pneumonia. ECCMID 2016: O-318).
- Werth BJ, Barber KE, Tran KN, et al. Ceftobiprole and ampicillin increase daptomycin susceptibility of daptomycin-susceptible and -resistant VRE. J Antimicrob Chemother. 2015;70(2):489–493.
- Rouse MS, Steckelberg JM, Patel R. In vitro activity of ceftobiprole, daptomycin, linezolid, and vancomycin against methicillin-resistant staphylococci associated with endocarditis and bone and joint infection. Diagn Microbiol Infect Dis. 2007;58(3):363–365.
- Saleh-Mghir A, Dumitrescu O, Dinh A, et al. Ceftobiprole efficacy in vitro against Panton-Valentine leukocidin production and in vivo against community-associated methicillin-resistant Staphylococcus aureus osteomyelitis in rabbits. Antimicrob Agents Chemother. 2012;56(12):6291–6297.
- Schmitt-Hoffmann A, Nyman L, Roos B, et al. Multiple-dose pharmacokinetics and safety of a novel broad-spectrum cephalosporin (BAL5788) in healthy volunteers. Antimicrob Agents Chemother. 2004;48(7):2576–2580.
- European Medicines Agency. Refusal assessment report for Zeftera (previously known as Zevtera). European Medicines Agency; 2010. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-Public_assessment_report/human/000883/WC500096883.pdf
- Basilea Medical Ltd. Public assessment report, Zevtera 500mg powder for concentrate for solution for infusion. Medicines and Healthcare Products Regulatory Agency.
- Nerandzic MM, Donskey CJ. Effect of ceftobiprole treatment on growth of and toxin production by Clostridium difficile in cecal contents of mice. Antimicrob Agents Chemother. 2011;55(5):2174–2177.
- Backstrom T, Panagiotidis G, Beck O, et al. Effect of ceftobiprole on the normal human intestinal microflora. Int J Antimicrob Agents. 2010;36(6):537–541.
- Hageman JC, Uyeki TM, Francis JS, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg Infect Dis. 2006;12(6):894–899.
- Rand KH, Houck HJ. Synergy of daptomycin with oxacillin and other beta-lactams against methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2004;48(8):2871–2875.
- Dhand A, Bayer AS, Pogliano J, et al. Use of antistaphylococcal beta-lactams to increase daptomycin activity in eradicating persistent bacteremia due to methicillin-resistant Staphylococcus aureus: role of enhanced daptomycin binding. Clin Infect Dis. 2011;53(2):158–163.
- Mehta S, Singh C, Plata KB, et al. beta-Lactams increase the antibacterial activity of daptomycin against clinical methicillin-resistant Staphylococcus aureus strains and prevent selection of daptomycin-resistant derivatives. Antimicrob Agents Chemother. 2012;56(12):6192–6200.
- Werth BJ, Barber KE, Kieu-Nhi TT, et al. Ceftobiprole and ampicillin increase daptomycin susceptibility of daptomycin-susceptible and -resistant VRE. J Antimicrob Chemother. 2015;70(2):489–493.
