 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective: The objective of this study is to quantify the effect of the Bone Conduction Implant (BCI) on sound localisation accuracy in subjects with conductive hearing loss (CHL).
Design: The subjects were tested in a horizontal sound localisation task in which localisation responses were objectively obtained by eye-tracking, in a prospective, cross-sectional design. The tests were performed unaided and unilaterally aided. The stimulus used had a spectrum similar to female speech and was presented at 63 and 73 dB SPL. The main outcome measure was the error index (EI), ranging from 0 to 1 (perfect to random performance).
Study sample: Eleven subjects (aged 21–75 years, five females) with BCI participated in the study. Their mixed/conductive hearing loss was either unilateral (n = 5) or bilateral (n = 6).
Results: Three of five subjects (60%) with unilateral CHL, and four of six subjects (67%) with bilateral CHL showed significantly improved sound localisation when using a unilateral BCI (p < .05). For the subjects with bilateral CHL, a distinct linear relation between aided sound localisation and hearing thresholds in the non-implant ear existed at 73 dB SPL (18% decrease in the EI per 10 dB decrease in pure-tone average, r = 0.98, p < .001).
Conclusions: Individuals with mixed/conductive hearing loss may benefit from a unilateral BCI in sound localisation.
Introduction
Sound localisation accuracy (SLA) refers to the ability of identifying the direction of a sound. In the frontal horizontal plane, the main cues used by the auditory system to compute the spatial position of a sound are interaural differences in time and in intensity (Middlebrooks and Green Citation1991). The interaural time difference (ITD) has a dominant role in horizontal sound localisation (Wightman and Kistler Citation1992), and is based on the difference of a sound’s time of arrival at the two ears. The interaural level difference (ILD) cue arises as a consequence of the acoustic shadow of the head resulting in a more intense signal in the ear closest to the sound-source. In addition to the processing of these binaural cues, sound localisation is facilitated by loudness cues and spectral cues, particularly in the vertical plane and to avoid front-back confusions (Middlebrooks and Green Citation1991).
Individuals with conductive hearing loss (CHL), who are unable to use conventional hearing aids, may benefit from intervention with bone conduction devices (BCDs) by virtue of their normal or near-normal inner ear function. With BCDs, the sound is transmitted to the cochleae by vibrations of the skull bone, effectively producing basilar membrane motion (Békésy Citation1932). Taking interaural cues into consideration, one important aspect of the bone conduction (BC) sound path is the transcranial attenuation (TA), which describes to what extent the sound is attenuated contralateral to the stimulus position. TA is highly variable between and within subjects depending on the method of measurement (e.g. subjectively with pure-tones, Stenfelt Citation2012) or objectively with promontory acceleration measurements (Håkansson et al. Citation2010) or ear-canal sound pressure (Reinfeldt, Stenfelt, and Hakansson Citation2013), on the frequency, and on the stimulation position (e.g. mastoid or Bone Anchored Hearing Aid [BAHA] position). Arguably, the most relevant measure of TA is provided by measuring subjective hearing thresholds with ipsilateral and contralateral BC stimulation in individuals with unilateral deafness. While this measure of TA shows great intra-study variability for the mastoid position in adults, the general trend is that TA seems to be higher at high frequencies (up to 4 kHz was measured in all studies) than at low frequencies (Hurley and Berger Citation1970; Snyder Citation1973; Nolan and Lyon Citation1981; Stenfelt Citation2012). Moreover, according to Stenfelt (Citation2012), the TA in the BAHA position is 2-3 dB lower than in the mastoid position (Stenfelt Citation2012).
These findings have implications for binaural processing of signals presented in the sound field in individuals with CHL using BCDs, since the interaural separation of those signals is affected. Specifically, sound localisation could be compromised because ILD and ITD cues are likely to be distorted by the BC sound pathway. Besides the within- and between-subject variability in TA, its effect on the binaural cues likely varies depending on (1) if an individual is unilaterally or bilaterally fitted with BCDs, (2) if the CHL is unilateral (uCHL) or bilateral (bCHL), and (3) on the position of the transducer(s).
In addition to the alleged effect of TA on sound localisation, animal studies suggest that binaural cues are distorted by conductive hearing loss, as both ILD and ITD in chinchillas are altered by simulated middle ear effusion (Thornton et al. Citation2012).
The results of previous studies on horizontal sound localisation in individuals with CHL (data collected using the BAHA) suggest that listeners with uCHL may obtain a sound localisation benefit from a unilateral BCD, but that this benefit is variable and not universal (Kunst et al. Citation2008; Agterberg et al. Citation2011, Citation2012). In individuals with bCHL, bilateral BCD conditions increase SLA as compared to either left or right unilateral BCD conditions on average (Bosman et al. Citation2001; Priwin et al. Citation2004). The benefit of a unilateral BCD in bCHL is unknown to the authors’ knowledge. Despite bilateral hearing loss, a unilateral fitting of a BCD (or a conventional hearing aid) may theoretically improve performance in tasks that require binaural processing of a sound, since the hearing loss may be asymmetric and audibility quite different between the ears.
The present study was partly motivated by the relatively small numbers of studies evaluating the benefit of a unilateral BCD for conductive hearing losses in horizontal sound localisation tasks. Primarily, however, the goal of the study was to quantify any benefit subjects may receive in sound localisation using the Bone Conduction Implant (BCI). The BCI is a novel BCD introduced as an alternative to the BAHA (Håkansson et al. Citation2010; Eeg-Olofsson et al. Citation2014; Reinfeldt et al. Citation2015; Taghavi et al. Citation2015). Briefly, the BCI utilises a tuned inductive link for the transmission of the sound from an external audio processor to an implanted transducer, thereby removing the need for a skin penetrating screw as in BAHAs and leaving the skin intact. The implanted transducer is placed in a shallow (4–5 mm) drilled recess in the mastoid of the temporal bone. The placement of the transducer together with the technical design of the BCI compensate for the loss of gain introduced by the inductive link, resulting in very similar audiological outcomes in matched BCI and BAHA patients (Rigato et al. Citation2016). Spatial hearing with the BCI, for example sound localisation, has so far not been studied. Since the TA is higher when the transducer is placed in the BCI position than for the classic BAHA position, as found measuring the vibration velocity of the cochlear promontory with a Laser Doppler vibrometer in cadaver heads (Håkansson et al. Citation2010), spatial hearing could theoretically be facilitated. However, TA was not measured in the present study.
Aim of study
The aim of the present study was to quantify the effect of a unilateral BCI on sound localisation accuracy in subjects with unilateral and bilateral CHL.
Subjects and methods
Study design
Individuals with uCHL and bCHL were tested in sound-field in an objective sound localisation task, shown to be reliable in children and adults (Asp, Olofsson, and Berninger Citation2016) as well as sensitive to sound localisation deficits for mild-to-moderate unilateral hearing losses (Asp, Jakobsson, and Berninger Citation2018). Tests were performed in unaided and unilaterally aided conditions, using a continuous stimulus with a spectrum similar to female speech presented at two different levels (63 dB SPL (A) and 73 dB SPL (A)). In total, thus, four tests per subject were performed. The test order (aided/unaided) was randomised within uCHL and bCHL groups so that a specific test order had approximately equal probability of occurring. SLA at 63 dB SPL was always tested before 73 dB SPL. The main outcome measure was the error index (EI) (e.g. Gardner and Gardner Citation1973; Asp, Olofsson, and Berninger Citation2016), which is an overall quantification of SLA, ranging from 0 (perfect performance) to 1 (random performance).
Subjects
Eleven subjects (five females), aged 21–75 years, with CHL participated in the study. Subject characteristics and audiometric data are summarised in . Five subjects had an uCHL (air conduction [AC] pure-tone average [0.5, 1, 2 and 4 kHz] ≤25 dB HL and air-bone gap ≤10 dB at each of the frequencies 0.5, 1, 2 and 4 kHz in the non-affected ear). One of the subjects with uCHL had a sensorineural component (BC thresholds >25 dB HL at any of the frequencies 0.5, 1, 2 or 4 kHz). Six subjects had a bCHL, and four of these subjects had a sensorineural component. Prior to the start of the study, they were all unilaterally implanted with the active transcutaneous BCI in a clinical trial investigating the audiometric and quality of life benefits (Eeg-Olofsson et al. Citation2014; Reinfeldt et al. Citation2015). The BCI was individually fitted based on patient feedback. All subjects used omnidirectional microphone settings. Aided hearing thresholds using the BCI were measured as a part of the clinical trial and are also shown in . For subjects with uCHL, the median interaural asymmetry using the BCI was 13 dB, calculated as the difference in pure-tone average (0.5, 1, 2 and 4 kHz; PTA4) between the non-implant ear and the aided thresholds in the implanted ear. Subjects living far from the measurement site were reimbursed for expenses related to travel and accommodation. The study was approved by the regional ethical committee in Gothenburg, Sweden. The subjects received oral and written information about the study before enrolment and written informed consent was obtained for all the participants.
Table 1. Demographics and characteristics of the participating subjects with conductive (CHL) or mixed hearing loss. Five subjects had a unilateral CHL (uCHL) or mixed hearing loss and six subjects had a bilateral CHL (bCHL) or mixed hearing loss. Congenital and acquired hearing losses occurred in both groups. PTA4 is the average of thresholds at 0.5, 1, 2 and 4 kHz. Aided PTA4 is the average of the frequency-modulated thresholds at 0.5, 1, 2 and 4 kHz recorded in sound-field with the non-implant ear plugged and with the Bone Conduction Implant active (Eeg-Olofsson et al. Citation2014; Reinfeldt et al. Citation2015).
Sound localisation accuracy (SLA)
The setup, stimulus and procedure used for SLA measurements have previously been described in Asp et al. (Citation2016).
Setup
SLA was measured in quasi-free sound field in an audiometric test room (4.1 m × 3.3 m × 2.1 m) with low ambient sound level (mean = 25 dB (A) obtained during 15 s measurement), and short reverberation time (T30 = 0.11 s at 500 Hz), as recorded with a B&K 2238 Mediator and a B&K 2260 Investigator (Brüel & Kjaer, Naerum, Denmark), respectively. Twelve active loudspeakers (ARGON 7340A, Argon Audio, Sweden) were placed equidistantly spacing spanning a 110-degree arc in the frontal horizontal plane, resulting in loudspeaker positions at ±55, ±45, ±35, ±25, ±15 and ±5 degrees azimuth with respect to the subject. The approximate distance from the head of the subject to the loudspeakers was 1.2 m. The loudspeakers were at approximate ear level, vertically adjusted to accommodate different heights of the sitting subjects. Seven-inch video-displays were mounted below each loudspeaker, resulting in twelve loudspeaker/display-pairs (LD-pairs). The video-displays were visible, while the loudspeakers and the loudspeaker-stand were covered in black cloth.
An eye tracking system (Smart Eye Pro, Smart Eye AB, Gothenburg, Sweden) was used to record the gaze of the subjects in relation to the LD-pairs (see Asp, Olofsson, and Berninger Citation2016 for details). The coordinates of the video-displays and loudspeakers were defined in three dimensions in the eye-tracking system, resulting in 12 Areas of Interest (AOI) (Gredebäck, Johnson, and von Hofsten Citation2010; Asp, Olofsson, and Berninger Citation2016). Each AOI had width 0.17 m and height 0.55 m, and in total they constituted a continuous array of AOIs in a 3D-model, corresponding to the physical LD-pairs.
Stimulus
An ongoing auditory–visual stimulus (a colourful cartoon movie playing a continuous melody) was used for sound localisation measurements. The stimulus had a long-term frequency spectrum similar the spectrum of a female voice. The rationale for using this stimulus was to allow comparison between the results from the current study with sound localisation results from individuals with normal hearing (Asp, Olofsson, and Berninger Citation2016), and with simulated unilateral hearing loss (Asp, Jakobsson, and Berninger Citation2018).
Test procedure
Immediately prior to the test, a calibration of the subject’s gaze relative to the LD-pairs was performed (for a detailed description of the calibration procedure, see Asp, Olofsson, and Berninger Citation2016).
The test then started by presenting the auditory-visual stimulus from the loudspeaker at −5 degrees azimuth, just to the left of frontal incidence. After an average time interval of 7 s, the visual stimulus was stopped and the sound was instantaneously shifted to a randomised loudspeaker. The visual stimulus was automatically reintroduced after a sound-only period of 1.6 s to allow sustained acquisition of gaze towards the video-screens. During the 1.6 s sound-only period, the subjects were guided by audition only as to where the active sound-source was located. The auditory and visual shifts were repeated 24 times to randomly selected LD-pairs with the constraint that no LD-pair presented the stimuli a second time before each of the 12 LD-pairs had presented once. The subjects were instructed to watch and follow the auditory − visual stimulus and that sound-only periods would occur, and informed that they were allowed to move their heads freely. Beyond the natural amplitude fluctuations in the signal, no roving of the sound level was applied after azimuthal shifts, i.e. level cues were not deliberately minimised.
Subjects’ pupil positions relative to the LD-pairs were sampled at 20 Hz. The resulting gaze/AOI intersections (sample space: ±55, ±45, ±35, ±25, ±15 and ±5 degrees azimuth) were derived from the output of the eye-tracker and stored as a function of time, time-locked with the auditory and visual events. The perceived auditory azimuth was defined as the median of the final 10 gaze/AOI intersection samples of the 1.6 s sound-only period, i.e. a 500 ms sampling period. Medians were calculated if at least three samples were collected. SLA was quantified by the EI (see for example Gardner and Gardner Citation1973; Asp, Eskilsson, and Berninger Citation2011; Asp, Olofsson, and Berninger Citation2016) which was calculated as
(1)
(1)
where P is the number of presentations with a valid response (P ≤ 24 in the current test paradigm), ip is the presenting loudspeaker (1–12) and kp is the perceived loudspeaker (1–12) at the pth presentation, and n is the number of loudspeakers (12). An EI = 0 corresponds to perfect performance. An EI = 1 corresponds to average random performance. A Monte Carlo simulation showed that the 95% confidence interval for random performance using the current procedure was [0.72, 1.28]. Furthermore, the data from the SLA test was analysed as perceived versus presented sound-source azimuth.
Analyses
Non-parametric tests (aided versus unaided, 63 versus 73 dB SPL, and uCHL versus bCHL) were used for group comparisons and differences were considered statistically significant at p < .05. Within-subject differences (aided versus unaided conditions, and 63 dB SPL versus 73 dB SPL) were considered statistically significant (p < .05) if the difference in the EI was >0.054, based on a test-retest analysis of data from normal hearing subjects (Asp, Olofsson, and Berninger Citation2016).
Results
Unilateral conductive hearing loss
The median EIs in the subjects with uCHL was 0.49 (unaided) and 0.33 (aided) at 63 dB SPL. No significant difference existed between aided and unaided conditions (p > .05, Wilcoxon Matched Pairs).
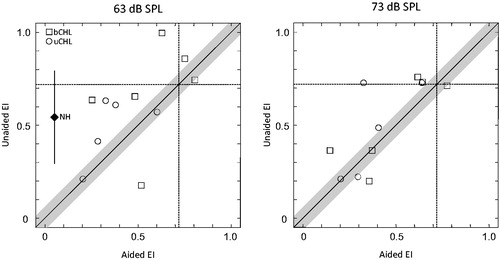
All subjects (n = 5) demonstrated unaided and aided localisation accuracy that was better than chance performance at 63 dB SPL (see individual EIs in the lower left quadrant in ). Three of five subjects (60%) showed a significant and relatively large BCI-benefit at 63 dB SPL (subjects 3, 7 and 202), while the remaining two subjects demonstrated comparable SLA across listening conditions.
Figure 1. Unaided versus aided individual sound localisation accuracy (SLA) at 63 dB SPL (left panel) and 73 dB SPL (right panel), quantified as an error index (EI). Open squares denote subjects with bilateral conductive hearing loss (bCHL) and open circles denote subjects with unilateral conductive hearing loss (uCHL). Markers above the solid diagonal line represent subjects with higher SLA in the aided versus the unaided condition, i.e. an aided benefit. All markers outside the grey area surrounding the diagonal indicates statistically significant within-subject differences >0.054 (aided versus unaided; p < .05), based on a test-retest reliability analysis in previous work (Asp, Olofsson, and Berninger Citation2016). The lower limits of the 95% confidence intervals for random SLA are drawn as dashed straight lines at EI = 0.72, dividing the figure into four quadrants. Each quadrant provides boundaries for the interpretation of SLA in each subject. Thus, subjects in the lower left quadrant reveal SLA better than random performance in both the aided and the unaided condition, subjects in the upper left quadrant can only localise in the aided condition, subjects in the lower right quadrant can only localise in the unaided condition, while subjects in the upper right quadrant cannot localise neither in the aided nor in the unaided condition. The mean EI from normal-hearing (NH) subjects (n = 8, mean EI = 0.054) at 63 dB SPL is provided in the left panel (solid diamond) to facilitate interpretation of data from subjects with CHL (Asp, Olofsson, and Berninger Citation2016). The x-coordinate for the solid diamond reflects the mean EI in normal binaural conditions for NH subjects. The y-coordinate for the solid diamond reflects the mean EI for NH subjects in a simulated unilateral hearing loss condition, and the solid line denote the standard deviation (Asp, Jakobsson, and Berninger Citation2018).
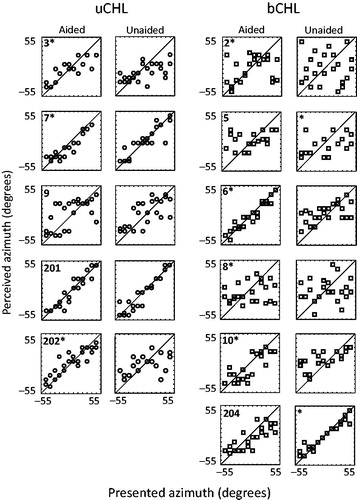
Individual perceived versus presented azimuths are presented in to visualise the difference in sound localisation response variability between aided and unaided conditions at 63 dB SPL. In this figure, responses at the line of equality reflect correct responses. Visual inspection of the localisation responses for the subjects who demonstrated an aided benefit (see panels marked with an Asterisks (*) in the left column in ) revealed that subjects 3 and 202, who both had a uCHL in the right ear, achieved decreasing response variability in the right hemisphere in the aided compared to the unaided condition, while responses in the left hemisphere appeared similar between listening conditions. For subject 7 (left ear uCHL), responses appeared less scattered overall. One of the subjects with no effect of the BCI had good localisation performance in both listening conditions (subject 201) with no clear change in the pattern of responses evident from the visual analysis. The other subject with no aided benefit (subject 9) showed relatively large response variability across spatial positions in both listening conditions, but typically lateralised the stimulus to the left or to the right.
Figure 2. Aided and unaided individual horizontal sound localisation accuracy (SLA) at 63 dB SPL. Open circles (the two left-most columns: unilateral conductive hearing loss; uCHL) and squares (the two right-most columns: bilateral conductive hearing loss; bCHL) represent perceived sound-source azimuth versus presented sound-source azimuth. Markers along the diagonal in each panel denote high SLA, while markers far away from the diagonal denote poor SLA. Each pair of panels (aided and unaided) is labelled with a study-id to facilitate comparison with . Asterisks (*) denote significant differences (p < .05) between aided and unaided conditions, and is placed in the panel with the highest SLA (e.g. subject 6 showed significant aided benefit, while subject 204 revealed significantly higher SLA in the unaided condition).
Effect of increased presentation level
The median EIs at 73 dB SPL (unaided EI = 0.48; aided = 0.31) were very similar to those at 63 dB SPL, and no significant difference existed between presentation levels in neither aided nor unaided listening conditions (p > .05, n = 5, Wilcoxon matched pairs). Furthermore, no significant difference existed between aided and unaided conditions at 73 dB SPL (p > .05, n = 5, Wilcoxon Matched Pairs).
Three of five subjects (60%) showed a statistically significant BCI-benefit (subjects 3, 9 and 202). Subject 201 demonstrated similar SLA across conditions and presentation levels, but the aided EI was statistically significantly higher (i.e. worse SLA) than the unaided EI at 73 dB SPL.
Pooling data from both presentation levels (n = 10) resulted in a statistically significant difference between unaided (median EI = 0.53) and aided (median EI = 0.33) conditions (p < .05, t = 2.3, Student’s t-test for dependent samples), suggesting a benefit of the BCI.
Bilateral conductive hearing loss
In the subjects with bCHL, the median unaided EI (0.70) was higher (i.e. worse SLA) than the median aided EI (0.57) at 63 dB SPL. However, no statistically significant difference existed (p = .25, n = 6, Wilcoxon matched pairs).
At 63 dB SPL, a statistically significant BCI-benefit in SLA (p < .05) existed in four of the six subjects (67%) (subjects 2, 6, 8 and 10) (). However, the EI in subject 8 was at the level of chance performance in both aided and unaided conditions (see upper right quadrant in ). Two of the six subjects (33%) demonstrated significantly higher EIs (i.e. worse SLA) in the aided versus the unaided condition. One of these subjects (subject 5) performed at chance level in both conditions, while the other subject (204) showed quite good localisation in both conditions.
Individual perceived versus presented azimuths are presented in to visualise the difference in sound localisation response variability between aided and unaided conditions at 63 dB SPL. The subjects who showed an aided benefit had variable unaided performance (). Subject 2, who had the highest unaided EI, showed a highly scattered response pattern consistent with guessing, likely because of poor audibility of the stimulus in that listening condition. This subject received a large aided benefit (an increase in EI of 0.37), but still had quite poor aided SLA (EI = 0.63). The responses of subject 204, who showed a significant deterioration in SLA using the BCI, had localisation responses close to the line of equality in the unaided and the aided condition. However, responses were somewhat more scattered in the latter condition, particularly when the sound was presented near frontal incidence.
Effect of increased presentation level
While the increased presentation level of 73 dB SPL decreased the median EI in both the unaided (median EI = 0.50) and the aided (median EI = 0.44) condition, the differences to the aided and the unaided EIs at 63 dB SPL was not statistically significant (p > .05, Wilcoxon matched pairs). Pooling data from both presentation levels (n = 12) resulted in a higher unaided median EI (0.69) than aided EI (0.57), with no statistically significant difference (p = .27, t = 1.2, n = 12, Student’s t-test for dependent samples).
At 73 dB SPL, a statistically significant BCI-benefit (p < .05) existed in three of six subjects (50%) (see individual EIs in ). One subject revealed no change in EI using the BCI, while two of six subjects (33%) showed a significant increase in the EI (i.e. worse SLA).
Individually, the increase in presentation level to 73 dB SPL resulted in either significantly lower EIs compared to 63 dB SPL (p < .05, four of six subjects, 67%) or unchanged EIs (two of six subjects, 33%) in the unaided condition. In the aided condition, five of six subjects (83%) showed a statistically significantly lower EI compared to the EI at 63 dB SPL (p < .05), while one of six subjects (17%) demonstrated a significantly higher EI (p < .05).
Comparison of sound localisation accuracy between bCHL and uCHL
The median EI in uCHL subjects was lower than the median EI in bCHL subjects across listening conditions and presentation levels, but this difference was not statistically significant (p > .05, Mann–Whitney U test).
A majority of both the uCHL and bCHL subjects showed a benefit with the BCI (see specifics above). On a group level, the BCI-benefit was comparable between uCHL (median BCI-benefit = 0.13) and bCHL (median BCI-benefit = 0.14) at 63 dB SPL (p = .92, Mann–Whitney U test). The BCI-benefit was smaller at 73 dB SPL in both uCHL (median BCI-benefit = 0.08) and bCHL (median BCI-benefit = 0.04), with no statistical difference between the groups (p = .78, Mann–Whitney U test). Subject 6, with bCHL, revealed the lowest EI in the entire study population at 73 dB SPL in the aided condition (EI = 0.15).
The pooled data across presentation levels did not reveal statistically significant differences between uCHL and bCHL in neither unaided (p = .25, t = 1.2) nor aided (p = .06, t = 2.0) conditions (Student’s t-test).
Effect of air conduction thresholds in the non-implant ear on SLA
Sound-field hearing thresholds with the BCI, as recorded 6 months after fitting the audio processor (Reinfeldt et al. Citation2015), together with analyses of audibility of the current sound localisation stimulus (Asp, Jakobsson, and Berninger Citation2018) indicated that the sound localisation stimulus used in the present study was audible in the aided condition (aided sound-field hearing thresholds ranged 13–34 dB HL) for all patients. Thus, the assumption was made that interaural comparisons of the BC signal in the implant ear and the AC signal contralaterally should be possible. Based on that assumption, increasing pure tone thresholds (i.e. decreasing audibility of the sound localisation stimulus), in the non-implant ear should result in an increased aided EI, since binaural processing of the stimulus would be affected. Linear regression analyses of the aided EI as a function of the PTA4 in the non-implant ear were performed to study any such relationships (). The aided EI was predicted by the PTA4 at both 63 dB SPL (EI = 0.26 + 0.006 × PTA4, r = 0.75, p = .008, n = 11) and 73 dB SPL (EI = 0.25 + 0.005 × PTA4, r = 0.65, p = .031, n = 11), indicating a decrease in the aided EI of 5–6 percentage points per 10 dB decrease in PTA4 (see top row in ).
Figure 3. Linear regression analyses of the aided Error Index as a function of pure-tone average (0.5, 1, 2 and 4 kHz; PTA4 [dB HL]) in the non-implant ear.
![Figure 3. Linear regression analyses of the aided Error Index as a function of pure-tone average (0.5, 1, 2 and 4 kHz; PTA4 [dB HL]) in the non-implant ear.](/cms/asset/674b29ec-49b4-4074-a86d-fe643c84265d/iija_a_1470337_f0003_b.jpg)
When regression analyses were limited to subjects with bCHL (see middle row in ), a distinct and highly significant correlation existed at 73 dB SPL (EI = −0.048 + 0.018 × PTA4, r = 0.98, p = .0004, n = 6), reflecting a decrease in the aided EI of 18 percentage points per 10 dB decrease in PTA4. The relationship between the aided EI and PTA4 at 63 dB SPL only approached statistical significance (p = .058, n = 6).
No significant relationship between the aided EI and the PTA4 existed in the subjects with uCHL (n = 4) (see bottom row in ).
Discussion
This is the first study to objectively determine sound localisation accuracy in individuals implanted with the BCI, a new rehabilitation option for patients with mild-to-moderate conductive and mixed hearing loss. Horizontal sound localisation accuracy was measured in individuals with unilateral and bilateral mixed or conductive hearing losses, in both unaided and unilaterally aided conditions, by automatic recording of eye-gaze patterns in response to azimuthal shifts of a broadband continuous stimulus. No significant effect of the BCI occurred on group level (probably related to the small study sample). However, at typical conversational level, i.e. 63 dB SPL, the majority of subjects with uCHL as well as with bCHL received a benefit in SLA from the BCI.
Unilateral conductive hearing loss
Objectively obtained sound localisation accuracy data in adults with unilateral conductive or mixed hearing loss are limited, and the reported aided results are exclusively obtained with the BAHA (Snik, Mylanus, and Cremers Citation2002; Hol et al. Citation2005; Agterberg et al. Citation2011, Citation2012). SLA in subjects with uCHL should therefore be of clinical interest and importance, in particular since the aided data are recorded with a transcutaneous bone conduction device with no previously reported results regarding sound localisation. The mean angular error, another measure of sound localisation accuracy, is presented for all subjects in supplemental digital online content (Supplemental Table) to facilitate comparison across studies.
At a typical conversational level of 63 dB SPL, 60% of the uCHL subjects demonstrated a significant BCI-benefit, which is comparable to proportions found for BAHA-benefit in narrow-band noise burst at 0.5 and 2 kHz (63%, Snik, Mylanus, and Cremers Citation2002), and at 0.5 and 3 kHz (67%, Agterberg et al. Citation2011). Lower (38%, narrow-band noise bursts centred around 0.5 kHz, Hol et al. Citation2005) as well as higher (78%, broadband noise bursts, Agterberg et al. Citation2012) proportions for BAHA-benefit have also been reported. A possible explanation to why not all subjects show improved sound localisation in the present study and elsewhere is that they may have adapted to the reduced audibility in the impaired ear, and relearned localisation with abnormal auditory input. Such adaptation is shown in the auditory system for sound localisation in the vertical (Hofman, Van Riswick, and Van Opstal Citation1998) and the horizontal (Kumpik, Kacelnik, and King Citation2010) dimensions in human experimental studies, and in animals (King, Parsons, and Moore Citation2000).
A broad-band sound, as used in the present study, should allow ILD, ITD and spectral cues to be available (if the sound is audible). Also, the stimulus used here was continuous, which potentially allowed subjects to make use of monaural level cues through head-movements during the 1.6 s sound-only period to a greater extent than with a short stimulus. Thus, the sound localisation paradigm and stimulus used in the present study does not provide data to dissociate individual contributions of several sound localisation cues. Instead, the spectrum of the stimulus used together with the measurement paradigm (gaze patterns towards auditory events) should be natural and thus to some extent reflect real-life circumstances. The data presented here support the idea that a sound that is audible in both ears, as it should be in uCHL subjects using a unilateral BCD, is possible to localise in the horizontal plane despite transcranial transmission.
Bilateral conductive hearing loss
Sound localisation accuracy was assessed for a normal conversational presentation level (63 dB SPL) and at 73 dB SPL, despite some rather severe hearing losses in subjects with bilateral CHL (see ). While the 63 dB SPL stimulus was just audible e.g. for subject 8, this presentation level was used to obtain clinically relevant information and to quantify performance in ecologically valid conditions.
The hearing thresholds in the non-implant ear seemed to predict the aided SLA in subjects with bCHL (, middle row), as shown by a highly significant correlation between the aided EI and the PTA4 in the non-implant ear at 73 dB SPL (r = 0.98, p = .0004, n = 6) and a trend at 63 dB SPL (r = 0.80, p = .058, n = 6). We interpret this as the aided audibility in the implanted ear is not enough for aided sound localisation of an ongoing auditory stimulus. Rather, the audibility in the non-implant ear seems essential, which may be important to consider before bilateral BCD implantation (an intervention that is shown to increase SLA in bCHL, e.g. Priwin et al. Citation2004). Decreasing hearing thresholds in the non-implant ear should allow binaural hearing for the unilaterally implanted bCHL subjects, since audibility in both ears should increase the possibility of interaural differences to occur.
In contrast to subjects with uCHL, there were bCHL-subjects for which the BCI had a negative effect on SLA. The subject with the most dramatic negative effect of the BCI on SLA (at 63 dB SPL, see left panel in ) showed a large and distinct increase in the EI from relatively good unaided performance (EI = 0.18) to poor aided performance (EI = 0.52). This subject (204) had quite symmetrical hearing loss (PTA4 = ∼50 dB HL in both ears), suggesting that at least the peaks of the stimulus used was bilaterally audible (Pavlovic Citation1987; Asp, Jakobsson, and Berninger Citation2018). As such, despite allegedly distorted binaural cues in the unaided condition given the bilateral CHL (Thornton et al. Citation2012), the SLA task should be possible to perform for this subject based on ILD. The worse aided SLA may be explained by the fact that the BCI induced an interaural asymmetry in terms of audibility, which might have resulted in distorted ILD cues. It could also be due to limited experience with the changed spatial cues introduced by BCI (∼6 months experience with the device).
Comparison between uCHL and bCHL
The BCI was beneficial both for subjects with uCHL and bCHL, and the magnitude of the benefit was comparable between the two groups. The absolute unaided and aided median EIs, however, were lower (better) in subjects with uCHL. This difference was not statistically significant, possibly due to the relatively small sample size in each group.
The lower unaided median EI in subjects with uCHL was expected, given the relatively severe bilateral hearing loss in subjects with bCHL which resulted in the sound localisation stimulus to be inaudible or just audible for some subjects at 63 dB SPL. By contrast, in the aided condition, three subjects with bCHL showed SLA comparable to that of uCHL (cf. ). As previously indicated, these were the subjects with the lowest PTA4 in the non-implant ear.
Conclusions
Individuals with unilateral conductive hearing loss may benefit from unilateral implantation of the BCI (60% of the subjects showed benefit) in horizontal sound localisation. Subjects with bilateral conductive hearing loss may also improve horizontal sound localisation accuracy using a unilateral BCI (67% of the subjects showed benefit). The aided sound localisation accuracy in bilateral conductive hearing loss patients seems related to the hearing thresholds in the non-implant ear, as localisation accuracy increased when PTA4 decreased.
| Abbreviations | ||
| AOI | = | area of interest |
| BAHA | = | bone anchored hearing aid |
| BC | = | bone conduction |
| BCD | = | bone conduction device |
| BCI | = | bone conduction implant |
| bCHL | = | bilateral conductive hearing loss |
| CHL | = | conductive hearing loss |
| EI | = | error index |
| ILD | = | interaural level difference |
| ITD | = | interaural time difference |
| NH | = | normal hearing |
| PTA4 | = | average of pure tone thresholds at 0.5, 1, 2, and 4 kHz |
| PTT | = | pure tone thresholds |
| SLA | = | sound localisation accuracy |
| TA | = | transcranial attenuation |
| uCHL | = | unilateral conductive hearing loss |
Supplemental Material
Download MS Word (37.5 KB)Acknowledgements
This work was funded by the Hasselblad Foundation. Part of this work was previously presented as a poster at the 6th international congress on bone conduction hearing and related technologies, 17–20 May 2017, Nijmegen, the Netherlands. The authors would like to thank the subjects for participating, and Maria Drott, Kerstin Henricson and Ann-Charlotte Persson for assistance in measurements.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Agterberg, M. J. H., M. K. S. Hol, C. W. R. J. Cremers, E. A. M. Mylanus, J. van Opstal, and A. F. M. Snik. 2011. “Conductive Hearing Loss and Bone Conduction Devices: Restored Binaural Hearing?” Advances in Oto-rhino-laryngology 71: 84–91. doi:10.1159/000323587.
- Agterberg, M. J. H., A. F. M. Snik, M. K. S. Hol, T. E. M. van Esch, C. W. R. J. Cremers, M. M. Van Wanrooij, A. J. Van Opstal, et al. 2011. “Improved Horizontal Directional Hearing in Bone Conduction Device users with Acquired Unilateral Conductive Hearing Loss.” Journal of the Association for Research in Otolaryngology 12 (1): 1–11. doi:10.1007/s10162-010-0235-2.
- Agterberg, M. J., A. F. Snik, M. K. Hol, M. M. Van Wanrooij, and A. J. Van Opstal. 2012. “Contribution of Monaural and Binaural Cues to Sound Localization in Listeners with Acquired Unilateral Conductive Hearing Loss: Improved Directional Hearing with a Bone-conduction Device.” Hearing Research 286 (1–2): 9–18. doi:10.1016/j.heares.2012.02.012.
- Asp, F., A. M. Jakobsson, and E. Berninger. 2018. “The Effect of Simulated Unilateral |Hearing Loss on Horizontal Sound Localization Accuracy and Recognition of Speech in Spatially Separate Competing Speech.” Hearing Research 357: 54–63. doi:10.1016/j.heares.2017.11.008.
- Asp, F., A. Olofsson, and E. Berninger. 2016. “Corneal-Reflection Eye-Tracking Technique for the Assessment of Horizontal Sound Localization Accuracy from 6 Months of Age.” Ear and Hearing 37 (2): e104–e118. doi:10.1097/AUD.0000000000000235.
- Asp, F., G. Eskilsson, and E. Berninger. 2011. “Horizontal Sound Localization in Children With Bilateral Cochlear Implants: Effects of Auditory Experience and Age at Implantation.” Otol Neurotol 32 (4): 558–564. doi:10.1097/MAO.0b013e318218cfbd.
- Békésy, G. V. 1932. “Zur Theorie des Horens bei der Schallaufnahme durch Knochenleitung.” Ann Physik 13: 111–136.
- Bosman, A. J., A. F. Snik, C. T. van der Pouw, E. A. Mylanus, and C. W. Cremers. 2001. “Audiometric Evaluation of Bilaterally Fitted Bone-anchored Hearing Aids.” International Journal of Audiology 40 (3): 158–167. doi:10.3109/00206090109073111.
- Eeg-Olofsson, M., B. Hakansson, S. Reinfeldt, H. Taghavi, H. Lund, K. J. Jansson, E. Håkansson, and J. Stalfors. 2014. “The Bone Conduction Implant–first Implantation, Surgical and Audiologic Aspects.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 35: 679–685. doi:10.1097/MAO.0000000000000203.
- Gardner, M. B., and R. S. Gardner. 1973. “Problem of Localization in the Median Plane: Effect of Pinnae Cavity Occlusion.” The Journal of the Acoustical Society of America 53 (2): 400–408. doi:10.1121/1.1913336.
- Gredebäck, G., S. Johnson, and C. von Hofsten. 2010. “Eye Tracking in Infancy Research.” Developmental Neuropsychology 35 (1): 1–19.
- Håkansson, B., S. Reinfeldt, M. Eeg-Olofsson, P. Ostli, H. Taghavi, J. Adler, J. Gabrielsson, et al. 2010. “A Novel Bone Conduction Implant (BCI): Engineering Aspects and Pre-clinical Studies.” International Journal of Audiology 49 (3): 203–215. doi:10.3109/14992020903264462.
- Hofman, P. M., J. G. Van Riswick, and A. J. Van Opstal. 1998. “Relearning Sound Localization with new Ears.” Nature Neuroscience 1 (5): 417–421. doi:10.1038/1633.
- Hol, M. K., A. F. Snik, E.A. Mylanus, and C. W. Cremers. 2005. “Does the Bone-anchored Hearing Aid have a Complementary Effect on Audiological and Subjective Outcomes in Patients with Unilateral Conductive Hearing Loss?” Audiology & Neuro-otology 10 (3): 159–168. doi:10.1159/000084026.
- Hurley, R., and K. Berger. 1970. “The Relationship Between Vibrator Placement and |Bone Conduction Measurements with Monaurally Deaf Subjects.” Journal of Auditory Research 10: 147–150.
- King, A. J., C. H. Parsons, and D. R. Moore. 2000. “Plasticity in the Neural Coding of Auditory Space in the Mammalian Brain.” Proceedings of the National Academy of Sciences of the United States of America 97 (22): 11821–11828. doi:10.1073/pnas.97.22.11821.
- Kumpik, D. P., O. Kacelnik, and A. J. King. 2010. “Adaptive Reweighting of Auditory Localization Cues in Response to Chronic Unilateral Earplugging in Humans.” Journal of Neuroscience 30 (14): 4883–4894.
- Kunst, S. J. W., J. M. Leijendeckers, E. A. M. Mylanus, M. K. S. Hol, A. F. M. Snik, and C. W. R. J. Cremers. 2008. “Bone-anchored Hearing aid System Application for Unilateral Congenital Conductive Hearing Impairment: Audiometric Results.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 29 (1): 2–7. doi:10.1097/mao.0b013e31815ee29a.
- Middlebrooks, J. C., and D. M. Green. 1991. “Sound Localization by Human Listeners.” Annual Review of Psychology 42: 135–159.
- Nolan, M., and D. J. Lyon. 1981. “Transcranial Attenuation in Bone Conduction Audiometry.” The Journal of Laryngology and Otology 95 (6): 597–608. doi:10.1017/S0022215100091155.
- Pavlovic, C. V. 1987. “Derivation of Primary Parameters and Procedures for use in Speech Intelligibility Predictions.” The Journal of the Acoustical Society of America 82 (2): 413–422. doi:10.1121/1.395442.
- Priwin, C., S. Stenfelt, G. Granstrom, A. Tjellstrom, and B. Hakansson. 2004. “Bilateral Bone-anchored Hearing Aids (BAHAs): An Audiometric Evaluation.” The Laryngoscope 114 (1): 77–84. doi:10.1097/00005537-200401000-00013.
- Reinfeldt, S., B. Hakansson, H. Taghavi, K. J. Freden Jansson, and M. Eeg-Olofsson. 2015. “The Bone Conduction Implant: Clinical Results of the First Six Patients.” International Journal of Audiology 54 (6): 408–416. doi:10.3109/14992027.2014.996826.
- Reinfeldt, S., S. Stenfelt, and B. Hakansson. 2013. “Estimation of Bone Conduction Skull Transmission by Hearing Thresholds and Ear-canal Sound Pressure.” Hearing Research 299: 19–28. doi:10.1016/j.heares.2013.01.023.
- Rigato, C., S. Reinfeldt, B. Håkansson, K.-J. F. Jansson, M. K. S. Hol, and M. Eeg-Olofsson. 2016. “Audiometric Comparison Betwen the First Patients With the Transcutaneous Bone Conduction Implant and Matched Percutaneous Bone Anchored Hearing Device Users.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 37 (9): 1381–1387. doi:10.1097/MAO.0000000000001183.
- Snik, A. F., E. A. Mylanus, and C. W. Cremers. 2002. “The Bone-anchored Hearing Aid in Patients with a Unilateral Air-bone Gap.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 23 (1): 61–66. doi:10.1097/00129492-200201000-00015.
- Snyder, J. M. 1973. “Interaural ttenuation Characteristics in Audiometry.” The Laryngoscope 83 (11): 1847–1855.
- Stenfelt, S. 2012. “Transcranial Attenuation of Bone-conducted Sound when Stimulation is at the Mastoid and at the Bone Conduction Hearing Aid Position.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 33: 105–114. doi:10.1097/MAO.0b013e31823e28ab.
- Taghavi, H., B. Håkansson, S. Reinfeldt, M. Eeg-Olofsson, K.-J. F. Jansson, E. Håkansson, B. Nasri, et al. 2015. “Technical Design of a New Bone Conduction Implant (BCI) System.” International Journal of Audiology 54 (10): 736–744. doi:10.3109/14992027.2015.1051665.
- Thornton, J. L., K. M. Chevallier, K. Koka, J. E. Lupo, and D. J. Tollin. 2012. “The Conductive Hearing Loss due to an Experimentally Induced Middle Ear Effusion Alters the Interaural Level and Time Difference Cues to Sound Location.” Journal of the Association for Research in Otolaryngology 13 (5): 641–654. doi:10.1007/s10162-012-0335-2.
- Wightman, F. L., and D. J. Kistler. 1992. “The Dominant Role of Low-frequency Interaural Time Differences in Sound Localization.” The Journal of the Acoustical Society of America 91 (3): 1648–1661. doi:10.1121/1.402445.
