Abstract
Objective
The purpose of this study was to determine the current prevalence of childhood hearing impairment (HI) in Sweden and to compare our data with previous studies from Sweden and other high-income countries.
Design
This was a cross-sectional study based on a register of children diagnosed with HI. Our results were compared with prevalence data from 18 studies from Sweden and other high-income countries, covering data collected from 1964 to the present.
Study sample
In December 2017, a total of 1911 out of 524,957 children 0–18 years of age and living in Stockholm County were enrolled in the regional programme for HI intervention.
Results
The overall prevalence of unilateral and bilateral HI >20 dB was 3.6/1000. The overall prevalence of bilateral HI >40 dB HL was 1.5/1000, split into age groups the prevalence was 0.4/1000 (<1 year of age), 1/1000 (1–4 years), 1.5/1000 (5–9 years), 1.6/1000 (10–14 years), and 2.14/1000 (15–18 years). From 1 to 18 years of age, the prevalence increased by a factor of 3.5 for moderate to profound HI >40 dB HL (0.7 to 2.4/1000).
Conclusion
The prevalence of HI across childhood in Stockholm County today is not significantly different from previous reports from Sweden and other high-income countries.
Introduction
Definition of paediatric hearing impairment
Reviews, studies, inquiries, and registers demonstrate that the prevalence of hearing impairment (HI) among children and adolescents varies across populations and HI criteria. The criterion for HI used in most studies is a pure tone average (PTA) of 40 dB HL or more in the better ear, but other degrees of HI have also be reported (Parving Citation1983; Davis and Wood Citation1992; Hirsch Citation1988). PTA may be calculated from three frequencies, 0.5, 1, and 2 kHz (PTA3), or four frequencies, 0.5, 1, 2, and 4 kHz (PTA4). The World Health Organization (Citation2019) defines “disabling” hearing impairment as a permanent unaided hearing impairment of more than 40 dB HL in adults and 30 dB HL in children (PTA4 in the better ear). The Global Burden of Disease Hearing Loss Expert Group has proposed a modified definition of hearing impairment that changes the threshold for disabling hearing impairment to 35 dB HL for all age groups (Stevens et al. Citation2013). Despite these recommendations, a standard definition of paediatric hearing impairment remains a matter of debate.
Prevalence of hearing impairment in high-income countries
The prevalence of HI in pre-school and school children varied from 1.7 to 3.2 per 1000 across several studies from Europe, the US, and Australia (Martin et al. Citation1981; Mehra, Eavey, and Keamy Citation2009; Ching et al. Citation2013; Fortnum et al. Citation2001; Ching, Oong, and van Wanrooy Citation2006). In 1977, Childhood Deafness in the European Community (CEC) investigated the prevalence of HI ≥50 dB HL in 8-year-old children in nine European countries (Martin et al. Citation1981) and reported a prevalence of 0.9 per 1000 (range: 0.7–1.5), corresponding to approximately 1.73 per 1000 for ≥40 dB HLFootnote1. Sweden was not included in the study, but in regions of Stockholm, Gothenburg, and northern Sweden prevalence rates of 1.0–1.8 per 1000 have been reported for moderate to severe HI in children born from 1964 to 1983 (Hirsch Citation1988; Kankkunen Citation1982; Sehlin, Holmgren, and Zakrisson Citation1990). In Finland, the prevalence of HI >25 dB HL in the better ear in 10-year-olds has remained unchanged at 2.3 per 1000 across more than three decades, from 1974 to 2002 (Vartiainen, Kemppinen, and Karjalainen Citation1997; Häkli et al. Citation2014; Mäki-Torkko et al. Citation1998). In contrast, a review of several studies and registers of school children in the US showed a higher prevalence rate of 3.2% for HI >20 dB HL and 0.3% for bilateral HI >40 dB HL (Mehra, Eavey, and Keamy Citation2009). However, from an international perspective, the prevalence in high-income countries remains low (Stevens et al. Citation2013).
Furthermore, studies have shown an increase in prevalence with age due to later acquired or progressive HI. In Australia, Ching, Oong, and van Wanrooy (Citation2006) reported a prevalence of 1.1 per 1000 in 3-year-olds compared to 3.17 per 1000 in 9 to 16-year-olds with all degrees of HI (Ching, Oong, and van Wanrooy Citation2006). In the UK, Fortnum et al. (Citation2001) studied cohorts of children born from 1980 to 1995 and found a prevalence of about 1 per 1000 for HI >40 dB at birth, increasing by 50–90% to 1.6 per 1000 by the age of 9 years (Fortnum and Davis Citation1997; Fortnum et al. Citation2001).
Hearing screening protocols in Sweden
Childhood hearing screening has been performed for several decades in Sweden. Pure tone audiometry was implemented in the 1970s for school children, and it is also performed at 4 years of age in many regions. Infant hearing screening at 7–8 months of age was implemented in the child health care programme around 1970. In 1994, infant screening was moved to the neonatal period, and neonatal hearing screening (NHS) is now provided nationally and free of charge to all newborns. It is performed by the maternity hospitals within the first days of life, and the uptake is about 98% of all newborns with very few lost to follow up, as reported regionally. The screening procedure in Stockholm and in most places in Sweden is two or three transient-evoked otoacoustic emission tests followed by an automatic auditory brainstem response (aABR) and, if referred, followed by clinical ABR for diagnostic evaluation. There are no national guidelines for referral and intervention, but an ABR threshold of 35–40 dB nHL is generally accepted as an indication for intervention if there are no signs of secretory otitis media.
Pre-school hearing screening is part of a protocol of general development, hearing, and vision screening and is regulated by national guidelines. Screening should be performed by nurses or audiologists using play audiometry with pure tones of 0.5, 1, 2, 4, and 6 kHz at 25 dB HL. Referral criteria for diagnostic assessment are thresholds of 30 dB HL or worse at two frequencies from 0.5 to 4 kHz, or 40 dB HL or worse at one frequency from 1 to 6 kHz (Stenfeldt Citation2018).
School-age hearing screening at 6 years of age uses a pure-tone screening protocol of 0.5, 1, 2, 4, and 6 kHz at 20 dB HL. The Stockholm criteria for referral to diagnostic assessment are thresholds of 25 dB HL or worse at two frequencies, 30 dB HL or worse at one frequency from 0.5 to 2 kHz, or thresholds of 40 dB HL or worse from 4 to 6 kHz thresholds. However, the exact criteria may vary between communities. Hearing screening for older children is no longer part of the school health care protocol, but hearing tests may be carried out at any time if there are signs of hearing problems, delayed language development, or other behavioural symptoms. Children who are immigrants may not have been previously tested, and they are offered a hearing test as part of the immigration health-screening programme (Swedish Association of Local Authorities and Regions.
From the screening programmes children are referred for diagnostic assessment and, if a permanent HI is established, enrolment in an intervention programme is recommended. All interventions for children with HI are provided by the government in Sweden and are free of charge.
Aim of the study
The aim of this study was to describe the prevalence of childhood HI in a well-documented cohort and to compare the results with those of previous studies. The results of this study will also provide an update of paediatric HI in Sweden, which has not been reported in the last four decades.
Ethical approval
This study was approved by the Swedish Ethical Review Authority (Dnr 2012/354-31/5 and 2013/3012-32).
Methods
The design of the study was a cross-sectional observational registry study. The study sample included all children 0–18 years of age born from 1 January 1999 to 21 December 2017, and living in Stockholm County in December 2017. The data for this study were retrieved from the database Audiohab and Statistics Sweden (CitationSCB). Statistics Sweden provides population statistics on population size and population changes available by county, municipality, sex, and age. Data on the number of inhabitants in Stockholm County for each age from 0 to 18 years were acquired from the most recent update in November 2017.
Audiohab is a database that contains information on the children with HI in Stockholm County, developed and maintained by the Department of Hearing and Balance, Karolinska University Hospital, Stockholm, with the main purpose of supporting the intervention programme for these children and reporting to health care authorities in Stockholm County. The database includes information about the degree and type of HI, the use of hearing devices, special education, and if the child has other disabilities.
The Department of Hearing and Balance, Karolinska University Hospital, is responsible for newborn hearing screening, diagnostic assessment, and intervention for all children in Stockholm County. Children diagnosed with a permanent HI, either bilateral or unilateral, are referred to the hearing intervention programme at Karolinska University Hospital, which is open for all children 0–19 years of age. At enrolment, the parents accept registration in the Audiohab database. Currently, there are no alternative programmes for children with HI, and a vast majority of (if not all) concerned families in the Stockholm County accept enrolment in the intervention programme and, accordingly, registration in Audiohab.
HI is classified in Audiohab as mild (21–40 dB HL), moderate (41–60 dB HL), severe (61–90 dB HL), or profound (>90 dB HL) in the better ear. Unilateral HI is defined as normal hearing (≤20 dB HL) in one ear with HI in the other ear, irrespective of the degree. The criteria for intervention in terms of hearing thresholds are PTA4 ≥ 25 dB HL or a high-frequency loss of ≥40 dB HL in one or both ears, also taking into account other disabilities that might affect speech and language development. HI may be sensorineural or conductive, if permanent or longstanding due to malformation or chronic ear disease. Children with temporary HI due to secretory otitis media are normally not enrolled, but for some children where tube insertion is not possible, hearing aids may be a better choice. Children with mild conductive hearing loss who are at risk for delayed speech development (e.g. children with Down syndrome) may, therefore, be enrolled. The intervention programme covers the fitting of hearing devices, cochlear implants, speech and auditory-verbal therapy, sign language instruction to parents, and psychological and social support to families as well as technical and pedagogical support to preschools and schools.
Prevalence data were compared to data from 18 studies previously performed in Europe, the US, and Australia describing the prevalence of moderate to severe HI in pre-school and school children covering four decades (1964–2003). These studies were selected according to the following criteria. First, each study must represent a population with a socioeconomic structure similar to that in Stockholm County. Second, prevalence data of moderate to profound hearing loss must be presented. Third, comparison to the reference groups must include the same age groups as in the present study. This was the most critical issue because most studies were based on register data of a defined birth cohort, but the age when audiometric data were collected was not always stated.
Statistics
The reference studies have data collected from 1964 to the present, and because the definition of HI in previous studies often differs from present-day conventions, these data have been adjusted to match the definition used by the bulk of modern studies (≥40 dB HL PTA4 in the better ear). To adjust the prevalence rate from PTA3 to PTA4, 3% was added based on hearing levels in children at 0.5, 1, 2, and 4 KHz (Pittman and Stelmachowicz Citation2003). Chi-square analyses were performed in R i386 version 3.5.2 (R Core Team Citation2018).
Results
Data from the Stockholm county birth cohort
In December 2017, a total of 1,911 children 0–18 years of age were registered in the database Audiohab. According to Statistics Sweden update from November 2017, 524,957 children 0–18 years of age were living in Stockholm County. This equates to a total prevalence of 3.6 per1000, including unilateral and bilateral HI >20 dB HL. The prevalence of all categories of HI from 0 to 18 years of age is presented in and . When grouped by age, we found a prevalence of 0.9 per 1000 in infants (<1 year of age), 1.9 per 1000 (1–4 years), 3.4 per 1000 (5–9 years), 4.7 per 1000 (10–14 years), and 5.4 per 1000 (15–18 years). For bilateral HI >40 dB HL, we found an overall prevalence of 1.5 per 1000, and when grouped by age the prevalence rates were 0.4 per 1000 in infants (<1 year), 1 per 1000 (1–4 years), 1.5 per 1000 (5–9 years), 1.6 per 1000 (10–14 years), and 2.14 per 1000 (15–18 years).
Figure 1. There is a clear trend of increasing prevalence rates across age, with significant differences across all types of HI. However, in older children, this increase in prevalence appears to be dominated by unilateral and mild HI.
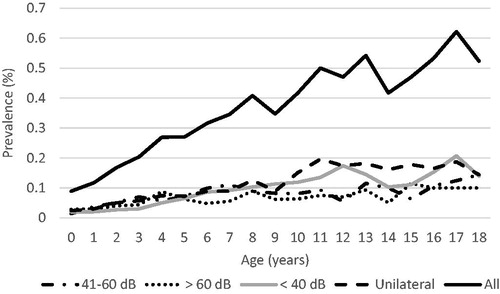
Table 1. Prevalence data from all children and adolescents, 0–18 years old, registered with hearing impairment in the database Audiohab, living in the Stockholm County in December 2017.
There was a clear trend for increasing prevalence rates across age groups as shown in . For example, severe and profound HI (>60 dB HL) was observed in 0.3 per 1000 for infants less than one year of age, and this increased to 1 per 1000 for 15-year-olds. The results of pairwise chi-square analyses performed between age groups are presented in . There were significant differences between all age groups when comparing the prevalence of all hearing loss >25 dB. For type and severity of HI, significant differences were found between 1 and 4-year-olds and older children across all types of HI; however, between 5 and 9-year-olds and older children this increase in prevalence appeared to be dominated by unilateral and mild HI.
Table 2. Chi-square (χ2) analyses comparing prevalence of HI between age-groups.
From 1 to 18 years of age, the prevalence increased by a factor of 4.5 for all HI (1.2 to 5.2/1000) and by a factor of 3.5 for moderate and profound HI (0.7 to 2.4/1000). For younger children from 1 to 7 years of age, the prevalence increased by a factor of 3 for all HI (1.2 to 3.5/1000) and by a factor of 2.5 for moderate and profound HI (0.7 to 1.7/1000). These trends corresponded to a yearly rate of increase of 0.37 per 1000 for all HI and 0.17 per 1000 for moderate and profound HI. The age group of <1 year was excluded from this calculation because some children might still be in the process of diagnostic evaluation and therefore not yet included in the Audiohab register.
For all children in the Audiohab register, 65–70% used hearing aids, and 10–15% had cochlear implants. Bone-conductive devices were worn by 10% of children 1–4 years of age, but only by 4% of children 10–14 years of age. Aetiology was not regularly documented in the Audiohab register, and there were not enough data for analysis.
Comparison with previous studies
Stockholm County data were compared with prevalence data of moderate to profound HI in children from 18 studies previously performed in Sweden and other high-income countries (). The reference studies were register-based with data collected from children born from 1964 to 2003. Reference data were compared with data from corresponding age groups in the Stockholm cohort and corrected for differences in hearing level and PTA criteria. Most studies included pre-school and school children <12 years and reported prevalences from 1.1 to 1.7 per 1000, which is consistent with the Stockholm County data. One study from northern Sweden showed significantly higher prevalence, which might have been because all children born in the county were included, even if they had since moved from the county (Sehlin, Holmgren, and Zakrisson Citation1990). Two studies based on the Metropolitan Atlanta Developmental Disabilities Surveillance Programme (MADDSP) in the US and one study from Austria showed significantly lower prevalence values compared to Stockholm County data (Drews et al. Citation1994; Van Naarden, Decouflé, and Caldwell Citation1999; Nekahm, Weichbold, and Welzl-Müller Citation2001).
Table 3. Comparison of prevalence rate from register-based reference studies of childhood hearing loss and current study data from Stockholm County.
A comparison to Hirsch´s study from the same geographical area in Stockholm County constitutes a birth cohort study, 30–35 years apart (Hirsch Citation1988). Hirsch (Citation1988) calculated the prevalence of HI among 6 to 7-year-olds born from 1976 to 1980, and these data were compared with the present study of children 6 to 7-years-old born from 2010 to 2011. Our study population showed a slightly higher prevalence of HI, but the difference was not significant.
Children with mild and unilateral HI constitute a large population, with increasing prevalence with age, but there was not a sufficient number of studies to make a similar comparison to our data. In the studies that included mild HI, the following prevalence rates were reported for children with HI >25 dB HL: 2.3 per 1000 for children <10 years of age (Häkli et al. Citation2014), 2.1 per 1000 for children <7 years of age (Dietz et al. Citation2009)), 2.15 per 1000 for children 6 years of age (Russ Citation2001; Russ et al. Citation2003), 2.5 per 1000 for children 0–20 years of age (Sehlin, Holmgren, and Zakrisson Citation1990), and 3.1% for children 10 years of age (Mehra, Eavey, and Keamy Citation2009). Data from our study showed prevalence rates of 2.5–4.2 per 1000 across the age groups corresponding to these studies, underpinned by the high coverage of pre-school and school screening in Stockholm.
Summary of the results
The prevalence of moderate to severe HI in this study ranged from 0.5 to 2.14 per 1000 (mean of 1.5/1000) for ages 0–18 years. The prevalence of all HI >25 dB was 3.6 per 1000 (range of 0.9–5.4). These data are consistent with other studies over the last 40 years, suggesting a negligible change in prevalence over time. Most studies including pre-school and young school children <12 years reported a prevalence of 1.0–1.8 per 1000, which is consistent with the prevalence of 1.1–1.7 per 1000 reported in the current study. Significant differences (p < 0.05) were found for three studies. There was a significant increase in prevalence across age groups for all degrees of HI, though this was more pronounced for mild and unilateral HI.
Discussion
Discussion of the results
The prevalence of moderate to profound hearing loss in the present study sample of 1.5 per 1000 from birth to 18 years of age was in accordance with previous studies from Sweden and other high-income countries reporting from 1964 until the present. The reference studies thus covered a time span of almost half a century. During this time period, general health status has improved, and new immunisation programmes have been implemented such that deafness following meningitis due to Haemophilus influenzae or Streptocccus pneumoniae is rarely seen today (Sözen et al. Citation2018). During this same time, however, the ethnicity of the population in Sweden has changed due to immigration from many low-income countries with a documented higher prevalence of HI (Olusanya, Neumann, and Saunders Citation2014; Mulwafu, Kuper, and Ensink Citation2016). Thus it might be speculated that the anticipated positive effects of extended vaccination programmes and improved neonatal care have been levelled out by new risk factors, for example, the increased survival of extremely premature neonates and the immigration of children from socioeconomically less developed countries. The implementation of universal neonatal hearing screening has also increased the awareness of HI in children. The stability in prevalence might also indicate that genetic aetiology dominates over environmental factors.
Mild or unilateral HI is often an overlooked hearing problem if not identified through regular screening. However, hearing screening for mild HI can be challenging in younger children due to temporary middle ear problems, and it is not frequently performed in older children.
As can be expected, the prevalence of all HI increases with age due to later acquired and diagnosed HI, and this is particularly the case for mild and unilateral HI (). In the present study, less than 35% of all HI and about 45% of moderate/severe cases of HI were identified by NHS. Previous studies have shown that the prevalence of HI in 9 to 16-year-olds was almost twice as high as in 3-year-olds (Fortnum et al. Citation2001; Ching et al. Citation2013; Ching, Oong, and van Wanrooy Citation2006), which is consistent with the present findings. Congenital HI missed by NHS, late-onset HI, immigration, and additional mild and unilateral HI might add up to a postnatal diagnosis of >50%, as reported from the UK (Watkin and Baldwin Citation2011). Lower prevalence of postnatal HI from 10 to 30% has also been reported (Van Naarden, Decouflé, and Caldwell Citation1999; Uus and Davis Citation2000; Vartiainen and Karjalainen Citation1997; MacAndie, Kubba, and McFarlane Citation2003; Weichbold, Nekahm-Heis, and Welzl-Müller Citation2005; Dedhia et al. Citation2013), but from the perspective of evaluating the outcome of NHS. To understand differences in prevalence between countries, the protocols for hearing screening and the coverage and uptake for these programmes must be known.
There are known risk factors for later acquired HI, for example, congenital cytomegalovirus infection (Kenna Citation2015; Karltorp et al. Citation2012), large vestibular aqueduct syndrome (Arjmand and Webber Citation2004), ototoxic medication, and head trauma. However, the aetiology of progressive and later acquired HI is still unknown in most cases, and the awareness of hearing problems must never be underestimated.
Interestingly, the large increase in prevalence for mild and unilateral HI in older children and adolescents seen in this study occurred despite the absence of screening programmes for these age groups. Sudden unilateral hearing loss will of course be observed in older children, and hearing may also be checked as part of investigating behavioural and learning problems. Children with mild and unilateral HI thus constitute a significant and increasing number, requiring more attention and demand for intervention.
Discussion of methods
The strength of this study is the high representativeness of the material due to the universal and sequential screening programmes in Sweden in combination with a single provider of hearing care for children in Stockholm County. Consequently, for children up to 6 years of age, the present results represent an epidemiological description, and this part of the sample can, therefore, be regarded to be comparable to a cross-sectional epidemiological study group.
The relevance of a register-based study depends on the uptake from the population studied. In older children who are not regularly screened, the school healthcare system also ensures high coverage in these age groups.
Any suspicion of a hearing problem always results in a referral for audiometry assessment. The implication of the school health programme is that virtually all children and youths with moderate to profound hearing loss are identified, but those with mild or unilateral hearing loss might remain undetected. The same situation is seen for older teenagers, 16 to 18-years-old, attending upper secondary school. In Sweden, 98% of all teenagers continued from elementary school to upper secondary school in 2013 (Swedish National Agency for Education). Accordingly, the prevalence values of moderate to profound hearing loss can be regarded as representative for the general population from birth to 18 years of age.
The recorded prevalence values of mild and unilateral permanent hearing loss are, however, uncertain for several reasons. First, hearing problems might not be observed or might be misinterpreted. Second, pre-school-age hearing screening methods might not be sensitive enough to guarantee the identification of mild and unilateral HI. Permanent HI may also be missed due to middle ear problems often seen in this age group. Finally, in the secondary school health programmes these types of hearing impairments are not given the highest priority and hearing screening is not regularly performed.
Conclusion
This study contributes to the statistics of the prevalence of HI in children in high-income countries. The comparison to the reference studies shows that the prevalence of moderate to profound hearing loss in childhood is similar today as five decades ago. The increase in prevalence with age supports the need for postnatal pathways for the early detection of HI, such as targeted surveillance or universal hearing screening within pre-school and school health cheques.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 The conversion from ≥50 to ≥40 dB HL was achieved by adding half the number of children with a mild hearing loss to the total number of children with hearing loss ≥50 dB HL.
References
- Arjmand, E. M., and A. Webber. 2004. “Audiometric Findings in Children with a Large Vestibular Aqueduct.” Archives of Otolaryngology-Head & Neck Surgery 130 (10): 1169–1174. doi:10.1001/archotol.130.10.1169.
- Ching, T. Y., H. Dillon, V. Marnane, S. Hou, J. Day, M. Seeto, K. Crowe, L. Street, J. Thomson, P. Van Buynder, et al. 2013. “Outcomes of Early- and Late-Identified Children at 3 Years of Age: Findings from a Prospective Population-Based Study.” Ear and Hearing 34 (5): 535–552. doi:10.1097/AUD.0b013e3182857718.
- Ching, T. Y., R. Oong, and E. van Wanrooy. 2006. “The Ages of Intervention in Regions with and without Universal Newborn Hearing Screening and Prevalence of Childhood Hearing Impairment in Australia.” The Australian and New Zealand Journal of Audiology 28 (2): 137–150. doi:10.1375/audi.28.2.137.
- Davis, A., and S. Wood. 1992. “The Epidemiology of Childhood Hearing Impairment: Factor Relevant to Planning of Services.” British Journal of Audiology 26 (2): 77–90. doi:10.3109/03005369209077875.
- Dedhia, K., D. Kitsko, D. Sabo, and D. H. Chi. 2013. “Children with Sensorineural Hearing Loss after Passing the Newborn Hearing Screen.” JAMA Otolaryngology- Head & Neck Surgery 139 (2): 119. doi:10.1001/jamaoto.2013.1229.
- Dietz, A., T. Löppönen, H. Valtonen, A. Hyvärinen, and H. Löppönen. 2009. “Prevalence and Etiology of Congenital or Early Acquired Hearing Impairment in Eastern Finland.” International Journal of Pediatric Otorhinolaryngology 73 (10): 1353–1357. doi:10.1016/j.ijporl.2009.06.009.
- Drews, C. D., M. Yeargin-Allsopp, C. C. Murphy, and P. Decouflé. 1994. “Hearing Impairment among 10-Year-Old Children: Metropolitan Atlanta, 1985 through 1987.” American Journal of Public Health 84 (7): 1164–1166. doi:10.2105/ajph.84.7.1164.
- Fortnum, H., and A. Davis. 1997. “Epidemiology of Permanent Childhood Hearing Impairment in Trent Region, 1985–1993.” British Journal of Audiology 31 (6): 409–446. doi:10.3109/03005364000000037.
- Fortnum, H. M., A. Q. Summerfield, D. H. Marshall, A. C. Davis, and J. M. Bamford. 2001. “Prevalence of Permanent Childhood Hearing Impairment in the United Kingdom and Implications for Universal Neonatal Hearing Screening: Questionnaire Based Ascertainment Study.” BMJ 323 (7312): 536–540. doi:10.1136/bmj.323.7312.536.
- Häkli, S., M. Luotonen, R. Bloigu, K. Majamaa, and M. Sorri. 2014. “Childhood Hearing Impairment in Northern Finland, Etiology and Additional Disabilities.” International Journal of Pediatric Otorhinolaryngology 78 (11): 1852–1856. doi:10.1016/j.ijporl.2014.08.007.
- Hirsch, A. 1988. “Hearing Loss and Associated Handicaps in Preschool Children.” Scandinavian Audiology. Supplementum 30: 61–64.
- Kankkunen, A. 1982. “Preschool Children with Impaired Hearing.” Acta Oto-Laryngologica 94 (391): 1–99. doi:10.3109/00016488209108896.
- Karltorp, E., S. Hellström, I. Lewensohn-Fuchs, E. Carlsson-Hansén, P. I. Carlsson, and M. L. Engman. 2012. “Congenital Cytomegalovirus Infection – A Common Cause of Hearing Loss of Unknown Aetiology.” Acta Paediatrica 101 (8): e357–e362. doi:10.1111/j.1651-2227.2012.02711.x.
- Kenna, M. A. 2015. “Acquired Hearing Loss in Children.” Otolaryngologic Clinics of North America 48 (6): 933–953. doi:10.1016/j.otc.2015.07.011.
- MacAndie, C., H. Kubba, and M. McFarlane. 2003. “Epidemiology of Permanent Childhood Hearing Loss in Glasgow, 1985–1994.” Scottish Medical Journal 48 (4): 117–119. doi:10.1177/003693300304800407.
- Mäki-Torkko, E. M., P. K. Lindholm, M. R. Väyrynen, J. T. Leisti, and M. J. Sorri. 1998. “Epidemiology of Moderate to Profound Childhood Hearing Impairments in Northern Finland. Any Changes in Ten Years?” Scandinavian Audiology 27 (2): 95–103. doi:10.1080/010503998420333.
- Martin, J. A., O. Bentzen, J. R. Colley, D. Hennebert, C. Holm, S. Iurato, G. A. de Jonge, O. McCullen, M. L. Meyer, W. J. Moore, et al. 1981. “Childhood Deafness in the European Community.” Scandinavian Audiology 10 (3): 165–174. doi:10.3109/01050398109076177.
- Mehra, S., R. D. Eavey, and D. G. Keamy, Jr. 2009. “The Epidemiology of Hearing Impairment in the United States: Newborns, Children, and Adolescents.” Otolaryngology-Head and Neck Surgery 140 (4): 461–472. doi:10.1016/j.otohns.2008.12.022.
- Mulwafu, W., H. Kuper, and R. J. Ensink. 2016. “Prevalence and Causes of Hearing Impairment in Africa.” Tropical Medicine & International Health 21 (2): 158–165. doi:10.1111/tmi.12640.
- Nekahm, D., V. Weichbold, and K. Welzl-Müller. 2001. “Epidemiology of Permanent Childhood Hearing Impairment in the Tyrol, 1980–94.” Scandinavian Audiology 30 (3): 197–202. doi:10.1080/010503901316914575.
- Olusanya, B. O., K. J. Neumann, and J. E. Saunders. 2014. “The Global Burden of Disabling Hearing Impairment: A Call to Action.” Bulletin of the World Health Organization 92 (5): 367–373. doi:10.2471/BLT.13.128728.
- Parving, A. 1983. “Epidemiology of Hearing Loss and Aetiological Diagnosis of Hearing Impairment in Childhood.” International Journal of Pediatric Otorhinolaryngology 5 (2): 151–165. doi:10.1016/s0165-5876(83)80020-2.
- Pittman, A. L., and P. G. Stelmachowicz. 2003. “Hearing Loss in Children and Adults: Audiometric Configuration, Asymmetry, and Progression.” Ear and Hearing 24 (3): 198–205. doi:10.1097/01.AUD.0000069226.22983.80.
- R Core Team. 2018. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing.
- Russ, S. 2001. “Measuring the Prevalence of Permanent Childhood Hearing Impairment.” BMJ 323 (7312): 525–526. doi:10.1136/bmj.323.7312.525.
- Russ, S. A., Z. Poulakis, M. Barker, M. Wake, F. Rickards, K. Saunders, and F. Oberklaid. 2003. “Epidemiology of Congenital Hearing Loss in Victoria, Australia.” International Journal of Audiology 42 (7): 385–390. doi:10.3109/14992020309080047.
- SCB Statistics Sweden. Available at: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/population/population-composition/population-statistics/
- Sehlin, P., G. Holmgren, and J. Zakrisson. 1990. “Incidence, Prevalence and Etiology of Hearing Impairment in Children in the County of Västerbotten, Sweden.” Scandinavian Audiology 19 (4): 193–200. doi:10.3109/01050399009070772.
- Sözen, T., M. D. Bajin, A. Kara, and L. Sennaroğlu. 2018. “The Effect of National Pneumococcal Vaccination Program on Incidence of Postmeningitis Sensorineural Hearing Loss and Current Treatment Modalities.” The Journal of International Advanced Otology 14 (3): 443–446. doi:10.5152/iao.2018.6169.
- Stenfeldt, K. 2018. “Preschool Hearing Screening in Sweden. An Evaluation of Current Practices and a Presentation of New National Guidelines.” International Journal of Pediatric Otorhinolaryngology 110: 70–75. doi:10.1016/j.ijporl.2018.04.013.
- Stevens, G., S. Flaxman, E. Brunskill, M. Mascarenhas, C. D. Mathers, and M. Finucane. 2013. “Global and Regional Hearing Impairment Prevalence: An Analysis of 42 Studies in 29 Countries.” European Journal of Public Health 23 (1): 146–152. doi:10.1093/eurpub/ckr176.
- Uus, K., and A. C. Davis. 2000. “Epidemiology of Permanent Childhood Hearing Impairment in Estonia, 1985-1990.” International Journal of Audiology 39 (4): 192–197. doi:10.3109/00206090009073077.
- Van Naarden, K., P. Decouflé, and K. Caldwell. ( 1999. “Prevalence and Characteristics of Children with Serious Hearing Impairment in Metropolitan Atlanta, 1991-1993.” Pediatrics 103 (3): 570–575. doi:10.1542/peds.103.3.570.
- Vartiainen, E., and S. Karjalainen. 1997. “Congenital and Early-Onset Bilateral Hearing Impairment in Children: The Delay in Detection.” The Journal of Laryngology and Otology 111 (11): 1018–1021. doi:10.1017/s0022215100139246.
- Vartiainen, E., P. Kemppinen, and S. Karjalainen. 1997. “Prevalence and Etiology of Bilateral Sensorineural Hearing Impairment in a Finnish Childhood Population.” International Journal of Pediatric Otorhinolaryngology 41 (2): 175–185. doi:10.1016/S0165-5876(97)00080-3.
- Watkin, P. M., and M. Baldwin. 2011. “Identifying Deafness in Early Childhood: Requirements after the Newborn Hearing Screen.” Archives of Disease in Childhood 96 (1): 62–66. doi:10.1136/adc.2010.185819.
- Weichbold, V., D. Nekahm-Heis, and K. Welzl-Müller. 2005. “Evaluation of the Austrian Newborn Hearing Screening Program.” Wiener Klinische Wochenschrift 117 (18): 641–646. doi:10.1007/s00508-005-0414-z.
- World Health Organization. 2019. Grades of hearing impairment. Accessed November 15 2019. https://www.who.int/pbd/deafness/hearing_impairment_grades/en/
