 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
The primary objective of the current study was the validation of a cloud-centralized audiometry system for clinical practice.
Design
A cross-sectional study design was used.
Study sample
A convenience sample of patients (>10 years old) booked for follow-up appointments were invited to participate. Participants completed both conventional and online digital audiometry in a standard sound treated clinic space during a single clinic visit; tests were completed in random order. Data for both ears were included. Patients were from one of three audiological practices.
Results
A total of 41 participants completed both audiometric tests. Validation study results showed that the mean difference between the two audiometric test results remained within 5 dB HL for both air and bone conduction thresholds at all tested frequencies.
Conclusions
Online digital audiometry has been demonstrated as a clinically accurate method for hearing assessment.
1. Introduction
The World Health Organization (WHO) considers hearing impairment to be one of the most important factors in the global burden of disease. Recently the WHO estimated the number of people with this disorder at 466 million world-wide with a projection of 900 million by the year 2050 (World Health Organization, Citation2018). The consequences of hearing loss are numerous and all-encompassing, both from a societal and an individual perspective. In adults, untreated hearing loss tends to lead to isolation and stigmatisation, impacting social participation as evidenced by the significantly higher rates of underemployment and unemployment (Olusanya, Ruben, and Parving Citation2006; Shukla et al. Citation2021; Bott and Saunders Citation2021). Hearing loss is also a leading modifiable risk factor for dementia and cognitive decline (Livingston et al. Citation2017; Loughrey et al. Citation2018; Lin et al. Citation2013).
Today however, the majority of the world’s population does not have access to hearing health services (Swanepoel et al. Citation2010). There are many reasons for this, including the insufficient number of audiologists in most parts of the world (Bhutta et al. Citation2019; Windmill and Freeman Citation2013), the high cost of equipment (e.g. audiometer and transducers) as well as the regular maintenance requirements (e.g. annual calibrations requiring third party vendors and expensive equipment). Differences in hearing healthcare are also noted between urban and rural populations, with a longer time to hearing aid acquisition observed in rural adults (Chan et al. Citation2017).
Recent innovations in the audiometry industry have focussed on different ways to minimise cost and improve access to hearing healthcare. These new approaches are based on the use of mobile devices (e.g. smartphones and tablets) for the practice of clinical audiometry (Yeung et al. Citation2013; Saliba et al. Citation2017; Thompson et al. Citation2015; Bastianelli et al. Citation2019), leveraging the internal, integrated sound card as well as being compatible with common types of audiometric transducers. The complementary integration of hearing test protocols that can be administered by non-specialists (World Health Organization (WHO) Citation2013), has enabled a technology platform, developed in partnership with the University of Pretoria in South Africa, to administer a hearing test on a smartphone to more than 35,000 people over a two-year period (Castillo and Vosloo Citation2015). Reducing costs by 50–70% compared to traditional hearing screening methods, this initiative has demonstrated how new technologies improve hearing screening and early detection among the most underserved communities (Castillo and Vosloo Citation2015).
Synchronous tele-audiology was evaluated by Givens et al. (Citation2003) who compared hearing thresholds measured by conventional systems with those obtained by Internet-based systems (Givens et al. Citation2003). Their study found an average difference in measured hearing thresholds of less than 1.3 dB HL between the two methods. Similarly, Choi et al. (Citation2007) using a standard sound card with a high-quality digital-to-analog converter as a pure tone generator for PC-based tele-audiometry, demonstrated that a hearing assessment was possible with no audiologist present at the measurement site (Choi et al. Citation2007). Finally, Swanepoel et al. (Citation2010) were also able to validate the accuracy of remote tonal audiometry practice by using desktop sharing software to control an audiometer located on another continent and a video conferencing system for clinician-patient communication (Swanepoel, Koekemoer, and Clark Citation2010). Results were clinically equivalent to conventional, face-to-face audiometry; however, the average test duration was longer (around 20%) in tele-audiometry.
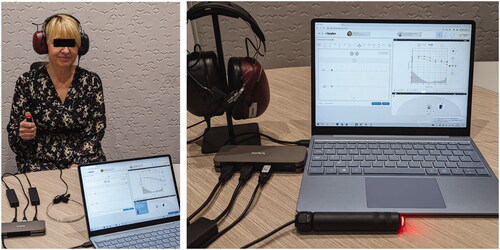
A more recent innovation in the audiology space has a novel design and was originally launched to French hearing health professionals (Clinical Otolaryngologist/Hearing Instrument Specialists). It is now more broadly available. This platform leverages Internet connectivity and digital technologies to bring the functionality of an audiometer to any Windows/Mac connected computer. Testing can be completed either locally at a clinic, or remotely to facilitate tele-audiology practice. Web audio technologies integrated into browsers are used to generate all of the signals required for basic audiometry and fully comply with the specifications established by the ISO 60645 Standard for audiometers. The audiometric transducers are USB-connected, pre-calibrated, and include a sound card with a high-quality digital-to-analog converter, similar to earlier solution by Choi et al (Citation2007). The current approach differs from the previously mentioned solutions as it no longer relies on the computer sound card, but rather the digital-to-analog converter embedded with the transducer (). The digital transducer, as created with the pairing of the audiometric transducer with the digital-to-analog converter, is then able to deliver audiometric signals with identical characteristics over various device platforms to which it is connected. Paving the way for pre-calibration and shipping of annually recalibrated transducers, this solution is already used by several hundred hearing health professionals in France, without the presence of a technician in the field. Accessible on different operating systems, this platform offers unique advantages to facilitate hearing testing access while minimising costs.
Figure 1. Koalys audiometric setup: Headset, bone vibrator and patient response button are connected to the laptop through a regular USB Hub. Software is accessible thanks to a web browser.
The objective of this study is to validate the clinical audiometry solution proposed through this online platform as being clinically equivalent to conventional audiometry. A multicenter clinical study was conducted comparing the audiometric thresholds measured using this new online platform with those obtained by in-person conventional audiometry.
2. Methods
2.1. Population
A convenience sample of patients from three hearing aid practices located in the Lyon area of France were invited to participate. Inclusion criteria were >10 years of age, attending the clinic for follow-up evaluation and able to complete both audiometric testing protocols. Exclusion criteria were unwilling/unable to complete audiometric testing with both systems. The study was conducted simultaneously by hearing healthcare professionals during patients’ annual follow-up visits. Testing took place mid-2017. Approval for this observational study was obtained from the relevant local ethics review board in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
2.2. Audiometric testing procedure
All testing took place in the standard sound treated testing space at each clinic (compliant with ISO 8253-1:2010(E)). Air conduction measurements were started on the better ear, if the patient indicated one, otherwise, the right ear was tested first. The first signal presented was a clearly audible pure pulsed pure tone (1 kHz/60 dB HL or more if necessary). The modified Hughson-Westlake procedure was applied to accurately determine the audiometric thresholds for each of the frequencies tested: 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, 8 kHz, 1 kHz (repeated), 0.5 kHz, 0.25 kHz. For each frequency, the audiometric threshold was confirmed at the level where the participant perceived the signal twice in ascending mode and there was no subjective perception with the same signal reduced by 5 dB. For bone conduction, the same method was applied, except for the 6 kHz and 8 kHz frequencies which were not measured. Masking signals were presented to the untested ear when necessary as per the guidelines below to ensure consistent methodology for both the conventional and the online digital audiometric testing.
Equation 1: Recommended masking levels in air conduction:
Equation 2: Recommended masking levels in bone conduction:
AI: Interaural attenuationABgap: Air-Bone gap
The test order was randomised using a virtual dice roll (http://de.virtuworld.net/) where an even number resulted in the conventional testing first and an odd number resulted in the online digital audiometry testing first. The same instructions were provided for both types of testing and given prior to the series of tests. The instructions included: “You will hear sounds, sometimes very faint. Please raise your hand when you hear a sound, even a very faint one, and point to the ear that heard it. If you hear a sound in the other ear, ignore it”. The test signals (pulsed pure tones) and masking signals (narrow-band noise centred on the frequency of the test signal) were emitted according to IEC 60645-1. The same audiologist completed both tests and was instructed to ignore the results of the first audiogram while performing the second one. Patient information was stored in an approved health data hosting server (French HDS) and in the Noah databases (HIMSA®, Copenhagen, DK) of the three audiology clinics where testing took place. Participants completed testing for both the Online Digital Audiometer and conventional audiometry in the same room.
2.3. Conventional audiometry
Three different models of computer-controlled audiometers were used across the clinical sites: Otometrics Aurical® (Copenhagen, DK), Otometrics Aurical Plus® (Copenhagen, DK) and Interacoustics Affinity® (Copenhagen, DK). On-site calibration of these audiometers was performed for air conduction and bone conduction by an external company in accordance with standardised guidelines for the calibration procedure and application of reference equivalent threshold sound pressure level values (ISO 389-1 for the air conduction transducer, ISO 389-3 for the bone vibrator). Transducers included circumaural (e.g. TDH-39) and bone (e.g. RadioEar B71) for air and bone conduction testing, respectively. Clinic Hearing Instrument Specialists (HISs) conducted hearing assessments at each clinic.
2.4. Online digital audiometer
A Koalys® account was created for each HIS at their respective clinics to allow them access to the online audiometry platform from their web browser (). Each HIS was trained by the Koalys® Support Team before administering their first test. At the time of the study completion a pre-market version of the online digital audiometer platform was used (now CE marked). The online digital audiometer conforms with the IEC 60645-1 Standard for audiometers. A unique set of digital audiometric transducers was prepared and shipped by audiometer manufacturing company Koalys® (formerly Audyx, Jerusalem, IL) to each clinic. Each digital transducer included a Telephonics TDH-39 and a RadioEar B71 bone vibrator coupled with a digital-to-analog converter. Two of the sites received standard air conduction transducers that were fitted with noise-attenuating shells (similar to Audiocups). The noise-attenuating shells were not required given the test environments for the study (i.e. sound-treated clinic space) however they offer additional flexibility to clinicians considering testing in other locations. The digital transducers were connected to the existing computers at each clinic. Bone conduction thresholds were measured using a RadioEar B71 bone vibrator placed on the subject’s mastoid. The Online Digital Audiometer requires a strong (>2 Mbps), stable internet connection to function.
2.5. Statistics
Personal identifiers (e.g. name, date of birth) were removed from the study data using a unique identifier for each participant. Study team members were not permitted access to the identifying information unless within the circle of care. Study data was stored on an HDS (Hébergeur de Données de Santé) certified database. This was a comparative clinical study whose objective was to test equivalency for a continuous response variable, i.e. hearing thresholds. BIAP (Bureau International d’Audiophonologie, https://www.biap.org) hearing loss categories were used to classify hearing ability of participants based on the pure tone average (500, 1000, 2000, 4000 Hz) of the better hearing ear. Clinical equivalence, the primary objective of the study, was evaluated by determining the proportion of thresholds within 5 dB HL and 10 dB HL of conventional (gold-standard) audiometry; 95% confidence intervals were also calculated using the Wilson score method. Mean and standard deviation of the difference between conventional and online digital audiometry were calculated. Statistics were completed using R Studio (version 1.4.1106).
3. Results
A total of 41 participants (82 ears) were recruited (23 women and 18 men) with a mean age of 74.3 years (SD = 14.3). Most participants had mild to moderate hearing loss according to the BIAP categories for hearing loss for their better ear (). The mean Pure Tone Average for ears was 51.4 dB HL (SD = 18.3) and 48.8 (SD = 14.3) dB HL for the right and left ears, respectively.
Table 1. Demographic characteristics of study participants.
The results in show the mean differences in hearing thresholds measured successively by the two systems with a 95% confidence interval for both air and bone conduction. The confidence intervals around the mean difference between the systems at all frequencies for both air and bone conduction are within 3 dB HL for air conduction and within 5 dB HL for bone conduction.
Figure 2. (A) Mean differences in air conduction thresholds by frequency between online digital audiometer and conventional audiometry, with 95% confidence intervals. (B) Mean differences in bone conduction thresholds by frequency between online digital audiometer and conventional audiometry, with 95% confidence intervals.
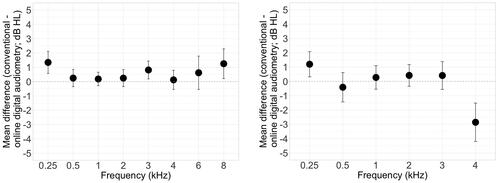
For the speech frequencies (0.5, 1, 2 and 4 kHz) all of the air conduction thresholds from the online digital audiometry were within 5 dB HL of the conventional audiometry values (). The majority of online digital audiometry air and bone conduction thresholds were within 10 dB HL of the conventional audiometry values demonstrating clinical equivalence (). The agreement ranged between 96.3% and 100% for air conduction and between 97.1% and 100% for bone conduction.
Table 2. Percentage agreement between online digital audiometer and conventional audiometer (percent agreement within 5 dBL HL and 10 dB HL, including 95% confidence interval, CI).
4. Discussion
The results from the multi-center clinical equivalence study comparing the air and bone conduction audiometric thresholds measured using the online platform to those obtained using three conventional audiometer models revealed clinically equivalent results. Results comparing the mean difference between the thresholds of online digital audiometry and conventional audiometry demonstrate clinical equivalence. Furthermore, this finding is supported by the high level of percentage agreement of thresholds between online digital audiometry and conventional audiometry. The randomisation of test order helped to control for the potential impact of learning effect or auditory fatigue on the results of the study.
The observed differences are expected considering that the search for audiometric thresholds is affected by intra-subject variability for both physiological and psychological reasons: motivation, fatigue, attention, training effect and change in subjective criteria in the estimation of threshold (Stuart et al. Citation1991). For air conduction, the imperfect reproducibility of the acoustic coupling between the transducer and the eardrum is evoked in the same study as having impacts in the reproducibility of measurements on frequencies below 0.5 kHz (variability of acoustic leakage) and above 2 kHz (variability of the orientation of the transducer axis in relation to that of the eardrum). Landry & Green (Citation1999), referring to previous study (Zwislocki et al. Citation1988) on the use of transducers in audiometry, also indicated that supra-aural transducers may be unreliable for the same reasons and that the variability of the audiometric threshold on successive tests is significantly greater at higher frequencies for people over 65 years of age compared to younger age groups. These studies indicate variations for this age group of at most 6 dB (Upper 95 CI) (Stuart et al. Citation1991) and 8 dB (Upper 95 CI) (Landry and Green Citation1999) for the frequencies 0.5 kHz, 1 kHz, 2 kHz and 4 kHz. In the present study, the measurements were carried out sequentially using a random draw to determine which system to use first and with the same types of transducers (reference, acoustic attenuation mode) used for each of the systems, at each of the measurement sites. These test-retest conditions, identical to those used in previous studies, make it possible to compare our results. Thus, it could be shown that, whatever the frequency tested in air conduction, the absolute differences calculated for this study were always lower than those published for air conduction test-retest conditions for the same patient on a single device (Landry and Green Citation1999; Zwislocki et al. Citation1988).
For bone conduction, Laukli & OddbjØrn (Laukli and Fjermedal Citation1990) and Swanepoel & Biagio (Swanepoel and Biagio Citation2011) independently published clinical data on the variability of measured hearing thresholds. These two studies indicate an absolute difference of up to 10 dB in two successive examinations with the same patient and tester. Such differences can be explained by a number of parameters that are difficult to control and for which there can be no perfect reproducibility: for example, the placement of the bone vibrator, the shape of the mastoid and the application force of the headband (Laukli and Fjermedal Citation1990). The results obtained in our study are in agreement with these previous publications, thus clearly demonstrating that online digital audiometry and conventional audiometry produce, in both air conduction and bone conduction, results that are clinically equivalent.
This study is part of a global effort to validate the use of an online platform for audiometry using digital transducers to perform clinical hearing assessment, locally or remotely, in an effort to expand care delivery potential. The online digital audiometry system configuration offers a range of use cases that allows hearing care professionals to treat significantly more patients both remotely or within their clinic using a single system. The current standard clinical audiometry is most often performed using specific equipment that is not portable, requiring the clinician and patient to be in the same location, limiting access in developing countries and/or isolated communities, two populations for which hearing loss is more common (Tucci, Merson, and Wilson Citation2010). Innovations, such as this online digital audiometer, offer the potential to expand hearing health care delivery to underserved populations. The results from this study provide preliminary evidence that the online digital audiometry can be used to obtain clinically reliable hearing test results. Further research is required to confirm the clinical equivalence in a fully remote configuration leveraging the tele-audiology features of this platform (embedded video conference system, live remote otoscopy). New features, such as remote noise monitoring, would be required to ensure that testing was completed under appropriate conditions. The future appears bright for ubiquitous audiological care. Advances in tele-audiology capabilities, whether synchronous or asynchronous, the increased presence of smartphone equipment in many populations, and the use of low-cost consumer transducers specifically calibrated (Masalski, Grysiński, and Kręcicki Citation2018), are all areas of hope. Reducing costs, these new practice possibilities can significantly increase accessibility to hearing care services and lead to a faster diagnosis of hearing impairment in both low-income areas and richer countries, where needs are also increasing (aging population and increasing number of elderly people living in institutions).
5. Conclusion
The data in this report demonstrate that the air and bone conduction thresholds measured using the online digital audiometer are no different from those obtained using a conventional audiometer. As such, the online digital audiometer is a clinically reliable tool for accurate hearing assessment. This new method is highly sensitive and produces clinically relevant results.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Bastianelli, Mark, Amy E. Mark, Arran McAfee, David Schramm, Renée Lefrançois, and Matthew Bromwich. 2019. “Adult Validation of a Self-Administered Tablet Audiometer.” Journal of Otolaryngology – Head and Neck Surgery 48 (1): 1–9. doi:10.1186/s40463-019-0385-0.
- Bhutta, Mahmood F., Xingkuan Bu, Patricia Castellanos de Muñoz, Suneela Garg, and Kelvin Kong. 2019. “Training for Hearing Care Providers.” Bulletin of the World Health Organization 97 (10): 691–698. doi:10.2471/BLT.18.224659.
- Bott, Anthea, and Gabrielle Saunders. 2021. “A Scoping Review of Studies Investigating Hearing Loss, Social Isolation and/or Loneliness in Adults.” International Journal of Audiology 60 (sup2): 30–46. doi:10.1080/14992027.2021.1915506.
- Castillo, N. M., and S. Vosloo. 2015. “HearScreenTM Case Study by UNESCO-Pearson Initiative for Literacy.” http://www.flexlearnstrategies.net/wp-content/uploads/2017/12/hearScreen.pdf.
- Chan, Stephen, Brian Hixon, Margaret Adkins, Jennifer B. Shinn, and Matthew L. Bush. 2017. “Rurality and Determinants of Hearing Healthcare in Adult Hearing Aid Recipients.” The Laryngoscope 127 (10): 2362–2367. doi:10.1002/lary.26490.Rurality.
- Choi, Jong Min., Haet Bit Lee, Cheol Soo Park, Seung Ha Oh, and Kwang Suk Park. 2007. “PC-Based Tele-Audiometry.” Telemedicine Journal and e-health: The Official Journal of the American Telemedicine Association 13 (5): 501–508. doi:10.1089/tmj.2007.0085.
- Givens, Gregg D., D. Ph, Adrian Blanarovich, Timothy Murphy, Scott Simmons, David Blach, and Saravanan Elangovan. 2003. “Internet-Based Tele-Audiometry System for the assessment of hearing: a pilot study.” Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association 9 (4): 375–378. doi:10.1089/153056203772744707.
- Landry, J. A., and Wb Green. 1999. “Pure-Tone Audiometric Threshold Test-Retest Variability in Young and Elderly Adults.” Journal of Speech-Language Pathology & Audiology 23 (2): 74–80. http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=107215405&site=ehost-live.
- Laukli, Einar, and Oddbj⊘rn Fjermedal. 1990. “Reproducibility of Hearing Threshold Measurements Supplementary Data on Bone-Conduction and Speech Audiometry.” Scandinavian Audiology 19 (3): 187–190. doi:10.3109/01050399009070771.
- Lin, Frank R., Kristine Yaffe, Jin Xia, Qian-Li Xue, Tamara B. Harris, Elizabeth Purchase-Helzner, Suzanne Satterfield, et al. 2013. “Hearing Loss and Cognitive Decline in Older Adults.” JAMA Internal Medicine 173 (4): 293–299. doi:10.1001/jamainternmed.2013.1868.Hearing.
- Livingston, Gill, Andrew Sommerlad, Vasiliki Orgeta, Sergi G. Costafreda, Jonathan Huntley, David Ames, Clive Ballard, et al. 2017. “Dementia Prevention, Intervention, and Care.” The Lancet 390 (10113): 2673–2734. doi:10.1016/S0140-6736(17)31363-6.
- Loughrey, David G., Michelle E. Kelly, George A. Kelley, Sabina Brennan, and Brian A. Lawlor. 2018. “Association of Age-Related Hearing Loss with Cognitive Function, Cognitive Impairment, and Dementia: A Systematic Review and Meta-analysis.” JAMA Otolaryngology- Head & Neck Surgery 144 (2): 115–126. doi:10.1001/jamaoto.2017.2513.
- Masalski, Marcin, Tomasz Grysiński, and Tomasz Kręcicki. 2018. “Hearing Tests Based on Biologically Calibrated Mobile Devices: Comparison with Pure-Tone Audiometry.” JMIR mHealth and uHealth 6 (1): e10–12. doi:10.2196/mhealth.7800.
- Olusanya, Bolajoko O., Robert J. Ruben, and Agnete Parving. 2006. “Reducing the Burden of Communication Disorders in the Developing World: An Opportunity for the Millennium Development Project.” Jama 296 (4): 441–444. doi:10.1001/jama.296.4.441.
- Saliba, Joe, Mahmoud Al-Reefi, Junie S. Carriere, Neil Verma, Christiane Provencal, and Jamie M. Rappaport. 2017. “Accuracy of Mobile-Based Audiometry in the Evaluation of Hearing Loss in Quiet and Noisy Environments.” Otolaryngology-Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery 156 (4): 706–711. doi:10.1177/0194599816683663.
- Shukla, Aishwarya, Michael, Harper, Emily Pedersen, Adele Goman, Jonathan J. Suen, Carrie Price, Jeremy Applebaum, Matthew Hoyer, R. Lin, and Nicholas S. Reed. 2021. “HHS Public Access” 162 (5): 622–633. doi:10.1177/0194599820910377.Hearing.
- Stuart, A., R. Stenstrom, C. Tompkins, and S. Vandenhoff. 1991. “Test-Retest Variability in Audiometric Threshold with Supraaural and Insert Earphones among Children and Adults.” Audiology: Official Organ of the International Society of Audiology 30 (2): 82–90. doi:10.3109/00206099109072873.
- Swanepoel, De Wet., and Leigh Biagio. 2011. “Validity of Diagnostic Computer-Based Air and Forehead Bone Conduction Audiometry.” Journal of Occupational and Environmental Hygiene 8 (4): 210–214. doi:10.1080/15459624.2011.559417.
- Swanepoel, De Wet., Jackie L. Clark, Dirk Koekemoer, James W. Hall, Mark Krumm, Deborah V. Ferrari, Bradley McPherson, et al. 2010. “Telehealth in Audiology: The Need and Potential to Reach Underserved Communities.” International Journal of Audiology 49 (3): 195–202. doi:10.3109/14992020903470783.
- Swanepoel, Wet de., Dirk Koekemoer, and Jackie Clark. 2010. “Intercontinental Hearing Assessment - a Study in Tele-Audiology.” Journal of Telemedicine and Telecare 16 (5): 248–252. doi:10.1258/jtt.2010.090906.
- Thompson, G. P., D. P. Sladen, B. J. H. Borst, and O. L. Still. 2015. “Accuracy of a Tablet Audiometer for Measuring Behavioral Hearing Thresholds in a Clinical Population.” Otolaryngology–Head and Neck Surgery 153 (5): 838–842. doi:10.1177/0194599815593737.
- Tucci, Debara L., Michael H. Merson, and Blake S. Wilson. 2010. “A Summary of the Literature on Global Hearing impairment: current status and priorities for action.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology 31 (1): 31–41. doi:10.1097/mao.0b013e3181c0eaec.
- Windmill, Ian M., and Barry A. Freeman. 2013. “Demand for Audiology Services: 30-Yr Projections and Impact on Academic Programs.” Journal of the American Academy of Audiology 24 (5): 407–416. doi:10.3766/jaaa.24.5.7.
- World Health Organization (WHO) 2013. “Multi-Country Assessment of National Capacity to Provide Hearing Care,” 1–49. http://www.who.int/pbd/deafness/en.
- World Health Organization (WHO) 2018. “Addressing the Rising Prevalence of Hearing Loss”. https://apps.who.int/iris/handle/10665/260336
- Yeung, Jeffrey, Hedyeh Javidnia, Sophie Heley, Yves Beauregard, and Sandra Champagne. 2013. “The New Age of Play Audiometry : Prospective Validation Testing of an IPad-Based Play Audiometer the New Age of Play Audiometry : Prospective Validation Testing of an IPad-Based Play Audiometer.” 42 (1): 1. doi:10.1186/1916-0216-42-21.
- Zwislocki, Jozef, Barbara Kruger, James D. Miller, Arthur F. Niemoeller, Edgar A. Shaw, and Gerald Studebaker. 1988. “Earphones in Audiometry Committee on Hearing, Bioacoustics, and Biomechanics Commission on Behavioral and Social Sciences and Education National Research Council WORKING GROUP.” The Journal of the Acoustical Society of America 83 (4): 1688–1689. doi:10.1121/1.395926.
