Abstract
Objective
The International Classification of Functioning Disability and Health (ICF) is a classification of health and health-related domains created by the World Health Organization and can be used as a standard to evaluate the health and disability of individuals. The ICF Core Set for Hearing Loss (CSHL) refers to the ICF categories found to be relative to Hearing Loss (HL) and the consequences of it on daily life. This study aimed to adapt the content of a database gathered in Hörzentrum Oldenburg gGmbH that included HL medical assessments and audiological data to the ICF.
Design
ICF linking rules were applied to these assessment methods including medical interviews, ear examinations, pure-tone audiometry, Adaptive Categorical Loudness Scaling, and speech intelligibility test.
Study sample
1316 subjects.
Results
In total, 44% of the brief and 18% of the comprehensive CSHL categories were addressed. The hearing functions were broadly evaluated. “Activities and Participation” and “Environmental Factors” were poorly examined (17% and 12% of the comprehensive CSHL categories, respectively).
Conclusions
The HL correlation with day-to-day activities limitation, performance restriction, and environmental conditions were poorly addressed. This study showed the essence of incorporating these methodologies with approaches that assess the daily-life challenges caused by HL in rehabilitation.
Introduction
Hearing impairment can potentially influence an individual's life through a wide range of problems from communication ability to mental disorders; not to mention the day-to-day social life of the person concerned (WHO Citation2021). To enhance the efficiency of hearing rehabilitation processes, it's essential to have a clear perspective of a patient's daily-life challenges originated by Hearing Loss (HL). This also includes the health conditions associated with disability (secondary health conditions such as depression caused by HL), as well as the resulting barriers and limitations in social and environmental living conditions.
Initially, evaluating the HL assessment methods from the research purview to clarify the extent to which they are capable of revealing the daily-life affairs should be considered. These methods may augment a variety of health assessment methods including but not limited to self-assessment methods such as questionnaires or medical interviews, laboratory-based listening experiments, and physical examinations. As a result, the weaknesses and strengths of the above methods in fully screening the health condition and its impact on the patient’s quality of life would be disclosed.
From a research perspective, to ensure by applying these methods, all the necessary aspects of a patient's disability are evaluated, a pre-existing standard is needed where HL is analysed broadly. The World Health Organisation’s (WHO) International Classification of Functioning, Disability, and Health (ICF) is a standard framework, created in 2001, that fully meets this requirement, owing to its biopsychosocial emphasis (WHO Citation2001, Citation2002). The health condition classification follows the WHO’s International Classification of Diseases (ICD) (WHO Citation1992). The ICF framework relates an individual's health condition to functioning and disability as well as the contextual factors (WHO Citation2001, Citation2002).
In 2008, a systematic literature review was performed to evaluate the outcome measures from the ICF perspective. This was to clarify the degree to which these assessment methods targeted functioning and disability in addition to health condition evaluation. These methods were applied in surgeries, rehabilitation, and treatments for injuries. It was found that the majority of the medical assessments did not include social-life aspects to date and that the ICF’s immense scale makes it a powerful tool that can be applied to evaluate the efficiency of the health condition evaluation, diagnostics, and treatment plans (Oltman et al. Citation2008).
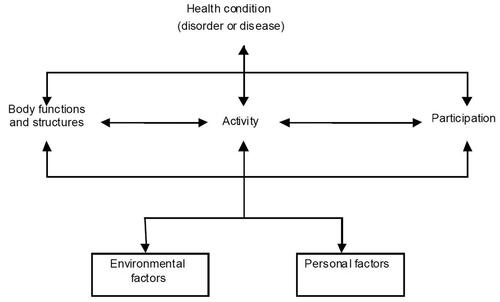
The ICF model includes two parts. Part 1 (functioning and disability) includes two components; “Body Functions and Structures” and “Activities and Participation”. Part 2 (contextual factors) includes two components; “Environmental Factors” and “Personal Factors” (WHO Citation2001, Citation2013). illustrates the interaction between the health condition and the aforementioned components.
Figure 1. The relationship between ICF components representing bio-psycho-social model of Functioning, Disability, and Health (WHO Citation2001).
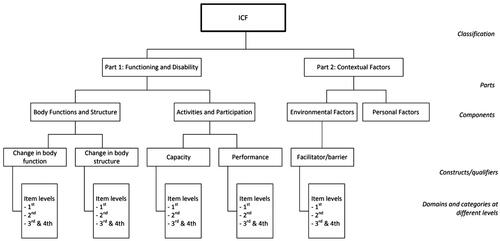
“Personal Factors” (PF) are not classified any further. ICF categorisation continues with classifying “Body Functions” (BF), “Body Structures” (BS), “Activities and Participation” (AP), and “Environmental Factors” (EF) into “chapters”. BF and BS each are divided into eight chapters. AP and EF include nine and five chapters, respectively. Each chapter includes “categories” at different levels. Each ICF category is represented with an ICF “code” (WHO Citation2001, Citation2013).
The categories classification system follows a hierarchical scheme. It means each chapter of a component is considered a “first-level item” which includes a more general concept. The codes used to refer to the categories of each chapter start with a letter (“b” for BF, “s” for BS, “d” for AP, and “e” for EF) followed by a chapter number. Each chapter itself is divided into subsets called “second-level items” which refer to more detailed information. These items are represented using the corresponding component letter and three digits. The classification extends to the “third-level items” (represented with a letter and four numbers) and in some cases to “fourth-level items” (represented with a letter and five numbers) which describe more specified concepts (WHO Citation2001, Citation2013). For instance, the first chapter of EF is “Products and Technology.” Any ICF code that is a subset of this chapter starts with “e1.” This chapter has twelve second-level items (e.g., e110: “Products or substances for personal consumption”). This category itself consists of four third-level items (e.g., e1100: “Food”). summarises the ICF hierarchical scheme.
Figure 2. The hierarchical scheme of the ICF classification (WHO Citation2001).
A user-friendly list of the ICF categories can be accessed through the WHO ICF browser (https://apps.who.int/classifications/icfbrowser/). An ICF core set is a collection of ICF categories, among all, that are found to be the most relevant parameters concerning a specific health condition (Selb et al. Citation2015). In this study, two ICF Core Sets of Hearing Loss (CSHL) were applied which were created and developed in 2010. (1) The comprehensive CSHL includes 117 categories that were found relevant to HL. (2) The brief CSHL includes 27 categories that reflect the minimum requirements to address the HL condition.
The development of these two CSHLs was performed in two major phases. The preparatory and first phase included the creation of the core sets by selecting the HL-related ICF categories. For the detailed procedure, see Danermark et al. (Citation2010, Citation2013), Granberg (Citation2015), Granberg et al. (Citation2014a, Citation2014b, Citation2014c, Citation2014d). Considering this worldwide standard, some studies were conducted in different countries to evaluate the “validity” (Selb et al. Citation2015) of the ICF CSHL, as the second phase. This phase was conducted based on evaluating clinical data and intake documentation in different health facilities. This includes two pilot studies performed by Alfakir, Holmes, and Noreen (Citation2015) and Alfakir, Hall, and Holmes (Citation2015) in the United States, a study carried out by Van Leeuwen et al. (Citation2017) in the Netherlands, a study by Karlsson et al. (Citation2021) using data collected in India, South Africa, Sweden, and the United States. As a result, the ICF CSHL was found to be a valid and reliable tool to be practically applied for outcome measure evaluation. A complete list of the categories of both CSHL can be accessed on the ICF research branch browser (https://www.icf-research-branch.org/icf-core-sets-projects2/other-health-conditions/icf-core-set-for-hearing-loss).
The current study aims to evaluate the audiological assessment methodologies performed during audiological ENT consulting at Hörzentrum Oldenburg gGmbH, Germany according to the ICF standard. This is to substantiate the degree to which the information gathered by virtue of different audiological assessment methodologies could be employed to measure the functioning and health status of a patient with HL according to the ICF framework. The study revealed the ICF categories which were covered by the applied methods as well as those that were previously overlooked and are vital to be included while assessing the patient's HL. As a result, the outcome of this study can be used as guidance in creating a revised rehabilitation process according to the ICF standard.
Materials and methods
In this study, a database, including the information collected from the patient’s record during the first visit of the private ENT consultation hours with an audiological focus at Hörzentrum Oldenburg gGmbH, was analysed. It must be emphasised that this database is not a representative typical German ENT clinical database since the focus of the audiological ENT consultation was rather on advanced audiological procedures. In other words, it partly applied measurement procedures established in audiological research but not in ENT clinics such as speech intelligibility in noise, in this case, Goettingen sentence test (GOESA) (Kollmeier and Wesselkamp Citation1997) or loudness perception, here, Adaptive Categorical Loudness Scaling (ACALOS) (Brand and Hohmann Citation2002; Oetting, Brand, and Ewert Citation2014). In addition, the focus was on diagnostics and not on audiological rehabilitation or psychosocial consequences of HL, therefore the emphasis in this study was on unaided health.
The data were collected for clinical purposes between 2001 and 2012. The anonymous database was converted to an electronic format for research purposes from 2013 to 2016. The database content was the result of the following assessments: medical administration interview, ear examination and otoscopy, pure-tone audiometry, ACALOS, and GOESA.
Medical administration interview/anamnesis
The physician performed the medical administration interview verbally and no paper-based prepared questionnaire was used. Therefore, no list of the exact questions was available and not all the patients were requested to respond to the exact same set of inquiries. Here, the percentage of the missing information for each inquiry was also considered. The physician stored the provided information on paper-based mediums on-site. Later on, the written data were prepared to be used for research purposes. By virtue of this, an optimal data categorisation was reached within a recursive digitising procedure reviewed by the physician who conducted the interviews as the following; patient’s demographic data, health status, and hearing complaints with and without wearing a hearing aid. In the following, the details regarding the above categories are provided. A full list of the categories can be found in the Appendices, see Supplementary Table A1.
Table 1. ICF linking results for the brief and comprehensive Core Set for Hearing Loss (Danermark et al. Citation2013; Granberg Citation2015). The covered (marked as ✔) and non-covered (marked as ✗) categories are provided. GOESA: Goettingen Sentence Test (Kollmeier and Wesselkamp Citation1997), ACALOS: Adaptive Categorical Loudness Scaling (Brand and Hohmann Citation2002; Oetting, Brand, and Ewert Citation2014).
Demographic data
The database includes the information collected from 1316 patients’ records, 750 (57%) male and 566 (43%) female. The age of the patients ranged from 12 to 99 years (M = 63.94, SD = 13.70). Nine patients were below 18 years old (three out of them being under 15 years old). Since no specific paediatric diagnostic was needed for these patients, they were included in the database, but the information collected from them was not included in this study and the ICF linking procedure. Among all, 426 patients had already received hearing aids before their first visit.
The patients were asked about their occupation and occupational or other types of noise exposure. Overall, 9% of the patients reported that they were/are exposed to noise at their workplace (e.g. military service, mining or construction industry, or other similar occupations). Furthermore, 17% of the patients were exposed to noise outside their workplace (e.g. firearms or bombs amid military skirmishes, shooting sports, hunting without ear protection, listening to music with high volume, or playing a musical instrument for an extended period of time). In some cases, the patients reported the time duration of the noise exposure. Moreover, the patients were asked whether they have a family history of HL. In cases where the latter would apply, an inquiry was made as to the side of the family (maternal, paternal, or both) having the impairment.
Health status
The inquiries made regarding the health status were categorised as the information related to general health conditions and ear-related conditions.
General health conditions
The patients were asked to report any existing physical health condition, cognitive disorder, or treatment (e.g. chemotherapy for cancerous or non-cancerous conditions). This information was later categorised during the digitalisation procedure. The most commonly reported health condition was cardiovascular disease. This was followed by high cholesterol, cognitive disorder, thyroid dysfunction, Tick bite, diabetes, myocardial infarction, kidney disease, stroke, facial nerve paralysis, polyneuropathy, and sleep apnoea (for details see Supplementary Table A2 in the Appendices). The patients were asked to mention the name of the medication they take regularly (if any). No prepared list of medications was provided.
Table 2. The covered (marked as ✔) and non-covered (marked as ✗) ICF categories of the brief Core Set for Hearing Loss (Danermark et al. Citation2013; Granberg Citation2015) in the applied database.
Ear-related conditions
The patient’s ear-related conditions in the past were rated by the physician during the interview regarding the following aspects; having history of sudden HL (and age), ear surgery (and age), the onset age of hearing problem, the age at receiving the first hearing aid (if any), and having history of Tinnitus (and age). The reported age is provided in the Appendices, see Supplementary Table A3. Lastly, having history of otitis media (and age category) was inquired. Overall, 19% of the patients reported that they had otitis media since pre-adolescence, 1% as a pubertal, and 4% as an adult.
Table 3. The absolute number and the respective percentages of the covered categories of the ICF brief or comprehensive Core Set for Hearing Loss (Danermark et al. Citation2013; Granberg Citation2015).
The current ear-related conditions were inquired regarding Tinnitus and dizziness which were reported by 32% and 25% of the patients, respectively.
The ear-related health condition was diagnosed by an ENT specialist according to the ICD-10 codes; Chapter 8: Diseases of the ear and mastoid process (see WHO ICD-10 browser https://icd.who.int/browse10/2019/en#/VIII). Overall, 78% of the patients were diagnosed with “Bilateral sensorineural HL” (H90.3) and 62% with “Abnormal auditory perceptions” (H93.2). Seven patients were diagnosed with bilateral HL (H90.0) and 17 of them with unilateral conductive HL (H90.1). The distribution of the ICD codes of the diagnosed ear-related conditions is available in the Appendices, see Supplementary Figure A1. The patients were referred to other medical care providers for a follow-up treatment. This included a referral to an otolaryngologist, neurotologist, neurologist, general practitioner, radiology, or hearing aid providers to receive a hearing aid or adjust the existing one.
Hearing complaints
The physician asked the patients to identify the daily-life scenarios in which they struggled with HL the most. The suggested inquiry included speech comprehension in a group of people, speech comprehension in noise, speech comprehension in a quiet place, having hearing difficulty while watching television or during a phone call, distant listening, distinguishing sound quality or naturalness, directional hearing, listening to music, and any other scenario(s) which was not specifically given. The information regarding the hearing complaints reported by different groups of subjects is available in the Appendices, see Supplementary Figure A2. Having difficulty listening to the radio, birds chirping, doorbell, and alarm clocks were commonly reported.
Ear examination and otoscopy
Ear examination covered general inspection by the ENT specialist of the outer ear (not included in this analysis) as well as otoscopy of the left and right ear regarding the status/structure of the tympanic membrane. The ENT specialist rated the overall otoscopy results concerning the categories “ok”, “not ok”, and “not quite ok”. No further details regarding the applied scale are available.
Middle ear/eustachian tube function
Middle ear and eustachian tube ventilation function was tested with valsalva manoeuvre and tympanometry, respectively.
Valsalva manoeuvre
Ventilation of the middle ear via the Eustachian tube was proved by a valsalva manoeuvre for the left and right ear and rated by the ENT specialist concerning the categories “ok”, “not ok”, and “not quite ok”. No further details regarding the applied scale are available.
Tympanometry
Middle ear function was measured by applying tympanometry. The tympanogram types were rated concerning the classification defined by Jerger (Citation1970): types A, B, C, As, Ad, and tympanic membrane perforation.
Pure-tone audiometry
Air conduction (AC) thresholds, bone conduction (BC) thresholds, and uncomfortable levels (UCL) were measured with pure tones. The descriptive statistics of the recorded thresholds are given in the Appendices, see Supplementary Table B1.
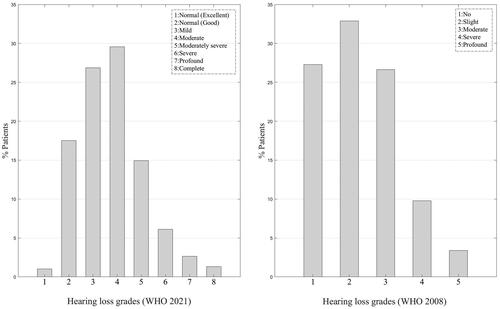
For HL categorisation according to WHO, the Pure Tone Average (PTA) was calculated across frequencies 0.5, 1, 2, and 4 kHz in the respective better ear of each individual. Hearing impairment categorisation has recently been revised by WHO (WHO Citation2021; Olusanya, Davis, and Hoffman Citation2019) according to the Global Burden of Disease Expert Group on Hearing Loss (Stevens et al. Citation2013). The new standard includes the following categories: normal (excellent), normal (good), mild, moderate, moderately severe, severe, profound, and complete. The increased available categories facilitate an improvement in classifying the HL level. The patients were diagnosed according to the earlier hearing impairment grading (World Health Organisation Grades of Hearing Impairment Citation2008), but as the large sample size of this study allowed for a powerful comparison between the old and new grading systems, the grading based on both systems was assessed. According to the new standard, 18.5% of the patients had normal hearing (PTA < 20 dB HL) while by applying the old grading, 27.2% of the patients had normal hearing (PTA ≤ 25 dB HL). Based on the new standard, 71.36% of the patients showed a mild, moderate, or moderately severe HL. According to the previous grading, 59.52% of the patients had a slight or moderate HL. In the earlier system, the patients with profound and complete HL of the new standard were classified into a single group of profound HL. According to the revised categorisation, 36 patients were diagnosed with profound and 18 patients with complete HL. The distribution of the impairment grades according to both categorizations is illustrated in .
Figure 3. Patients’ hearing impairment grade; left: According to the Global Burden of Disease Expert Group on Hearing Loss classification (Stevens et al. Citation2013; WHO Citation2021), right: According to the earlier hearing impairment grading (WHO Citation2008).
Adaptive categorical loudness scaling
To investigate loudness perception across the individual dynamic range, the individual loudness growth functions were determined with ACALOS (Brand and Hohmann Citation2002; Oetting, Brand, and Ewert Citation2014) using narrowband noises with centre frequencies of 0.5, 1, 2, and 4 kHz. Unaided loudness perception was measured monaurally via free-field equalised headphones. In case the patients were aided with hearing aids, also aided loudness perception was measured via loudspeaker presentation from the front direction with the distance of 1 m. In this method, during the adaptive measurements, the test signals are presented at different levels. These presentation levels are individually chosen by an adaptive procedure to avoid presentation levels outside the individual dynamic range (for procedure details, see Brand and Hohmann Citation2002). The listener chooses the subjectively perceived loudness from a visually presented categorical scale. The response scale consists of the category labels “not heard”, “very soft”, “soft”, “medium”, “loud”, “very loud”, and “extremely loud” as well as interim categories without labels. A model function is fitted to the individual data to determine the individual loudness growth function. The verbal scale is mapped to the numeric range of 0 (“not heard”) to 50 (“extremely loud”) as a function of signal level. This model function consists of two linear functions that are smoothed within the junction area (Brand and Hohmann Citation2002). The model function is represented by the junction point corresponding presentation level, called Lcut, which is close to the individual medium loud level. The parameter mlow gives the lower slope of the model function and is a measure of recruitment with higher values showing higher recruitment. The third model function parameter is the higher slope which is not explicitly reported here since there is no specific audiological meaning for that value. The descriptive statistics of the ACALOS results (Lcut and mlow values) are given in the Appendices, see Supplementary Tables C1, C2, C3, and Figure C1.
Speech intelligibility test
Due to the focus of the audiological consulting, for most people, only the data of speech intelligibility in noise were included in the database, and speech intelligibility in quiet results was only included in a few cases, and therefore, it’s not included in the analysis. To measure individual speech intelligibility in noise GOESA, in German: “Göttinger Satztest” (GÖSA) (Kollmeier and Wesselkamp Citation1997), was used. This test was applied to determine the individual Speech Reception Threshold (SRT) which is a signal-to-noise ratio that yields 50% intelligibility with an adaptive procedure (Brand and Kollmeier Citation2002). For all the patients, the noise presentation level was 65 dB SPL.
The SRT was determined in nine different acoustic situations. The descriptive statistics of the measurements are given in the Appendices, see Supplementary Table D1. For the listeners without hearing aids, the SRT was measured binaurally via free-field equalised headphones in S0N0 (speech and noise both from the front) [situation 1] and S0N ± 90 (speech from the front, noise from ±90°, at the side of the worse ear) [situation 2]. In order to investigate the individual binaural speech intelligibility, the SRT was also determined monaurally in the S0N ± 90 setting [situation 3]. The Intelligibility Level Difference (ILD) is given by the SRT difference situation 1-situation 2 and the Binaural Intelligibility Level Difference (BILD) by the SRT difference situation 3-situation 2. For the listeners with hearing aids, the respective S0N0 and S0N ± 90 SRT values were determined unaided [situations 4–6] and aided [situations 7–9] via loudspeakers.
ICF linking procedure
The collected data of each assessment method was linked to the most relative categories of both CSHL according to the recommended ICF linking rules and procedure (Cieza et al. Citation2002; Cieza et al. Citation2005; Granberg et al. Citation2014c). As a result, the ICF categories which were addressed in each method were revealed. The linking procedure was performed by three graders. The doubts and disagreements about the linking among the graders were then resolved by consulting with ICF experts; Prof. Razan Al Fakir and Dr. Lisette van Leeuwen.
Results
As a result of applying the linking rules, the ICF categories which were covered in the database were revealed. In general, the database content was linked to the most specific related category. As a consequence, the detected category and its corresponding lower-level category(s) were compared with the categories of both CSHL. Where a concept was linked to a category that was not directly listed in a core set, but its lower-level was, the concept was also linked to the higher category. Therefore, the lower-level category was counted as a detected category. In the following, each of the detected categories is provided along with the methodology(s) that are linked to it. In the end, for each component, the ratio of the number of the addressed categories over the total number of the categories in the comprehensive and brief CSHL is given in percentage.
Body functions
“Auditory perception” (b1560): Performing the perception task in GOESA requires the ability to perceive the auditory stimuli (in this case, speech signals). Therefore, GOESA was linked to b1560. The “hearing complaints” inquiries demanded perceiving the auditory stimuli, therefore, they were linked to b1560. Pure-tone audiometry and ACALOS were linked to b1560 (Granberg Citation2015) as perceiving the tone signal is a fundamental concept behind these methods.
“Sound detection” (b2300): In any of the “hearing complaints” scenarios, noticing the presence of sound in the auditory scene is the initial step. Therefore, “hearing complaints” were linked to b2300. As performing the task in pure-tone audiometry, ACALOS, and GOESA required identifying the existence of sound, they were linked to b2300.
“Sound discrimination” (b2301): Segregating the sound of interest from two or more other sounds was desired in all “hearing complaints” except for “Speech in quiet”. Therefore they were linked to b2301.
“Localisation of sound source” (b2302) and “Lateralization of sound source” (b2303): “Hearing complaints” and more specifically “Directional hearing” and “Distant listening” scenarios were linked to b2302 and b2303. In Intelligibility Level Difference (ILD) and Binaural Intelligibility Level Difference (BILD) trials of GOESA, the direction of arrival of the target signal and the distracting noise varied and the results were compared. Therefore, these measures were linked to both b2302 and b2303. Code b2303 is not included in the comprehensive CSHL, but its corresponding 2nd level category which is “Hearing functions” (b230) is included in the brief CSHL.
“Speech discrimination” (b2304): All the “hearing complaints” scenarios whether the desired sound was exclusively speech or could be speech in some cases (e.g. “distant listening”) were linked to b2304. GOESA was linked to b2304.
“Ringing in ears or tinnitus” (b2400) and “Dizziness” (b2401): The inquiries regarding the current ear-related health status; Tinnitus and dizziness were linked to b2400 and b2401, respectively. The corresponding second-level category which is “Sensations associated with hearing and vestibular function” (b240) is included in both core sets.
Chapter 2: “Sensory functions and pain”: Tympanometry was linked to BF, Chapter 2 that includes hearing and vestibular functions (Granberg Citation2015). Similarly, the valsalva manoeuvre was linked to Chapter 2.
Body structures
“Structure of external ear” (s240) and “Structure of middle ear” (s250): Performing otoscopy allows the examiner to evaluate the ear canal and tympanic membrane. Therefore, otoscopy examination was linked to s240 and s250. Performing valsalva manoeuvre and tympanometry was linked to s250.
Activities and participation
“Watching” (d110): Watching TV as a “Hearing complaints” scenario was linked to d110 (Granberg Citation2014c).
“Listening” (d115): The patient hearing evaluation via the laboratory-based measurements requires active listening, therefore, GOESA, pure-tone audiometry, and ACALOS were linked to d115. All of the “hearing complaints” inquiries were linked to d115.
“Communicating with receiving spoken messages” (d310): “Hearing complaints” scenarios were all linked to d310 as in some of them, the desired sound is indeed speech and in the others, the target sound may or may not include speech such as watching TV (Granberg Citation2014c).
“Conversation with one person” (d3503) and “Conversation with many people” (d3504): No laboratory-based measurement allowed the evaluation of the patients’ communication ability. The speech-related “hearing complaints” (speech in a group, noise, and quiet) were linked to d3503 and d3504.
“Using communication devices and techniques” (d360): No laboratory-based measurement evaluated the patient’s ability to use communication devices. “hearing complaints” regarding using a phone was linked to d360.
Chapter 8: “Major life areas”: The concept of exposure to noise at work was linked to d8; work and employment.
“Arts and culture” (d9202): Listening to music and watching television as “hearing complaints” scenarios were linked to “Arts and culture” (d9202). The corresponding 2nd level category which is “Recreation and leisure” (d920) is included in the comprehensive CSHL.
Environmental factors
“General products and technology for communication” (e1250): “Hearing complaints” while using a phone and watching TV were linked to e1250 (Granberg Citation2014c).
“Assistive products and technology for communication” (e1251): The patients who had already received hearing aid before their first visit were asked to respond to the “hearing complaints” inquiries both with and without a hearing aid. This enabled the examiner to analyse whether the hearing aid played the role of a facilitator or barrier for the patient when he/she attempted to communicate. As a result, the “hearing complaints” were linked to e1251.
The corresponding second-level category of codes e1250 and e1251 which is “Products and technology for communication” (e125) is included in both core sets.
“Design construction and building products and technology of buildings for public use” (e150): Noise exposure at a workplace or other environments was linked to e150 (Granberg et al. Citation2014c).
“Sound intensity” (e2500): Noise existence in “hearing complaints”, GOESA, pure-tone audiometry, and ACALOS were all linked to e2500.
“Sound quality” (e2501): Noise exposure (Granberg et al. Citation2014c), “hearing complaints”, and GOESA were linked to e2501 as they require sound detection at the existence of noise.
“Health professionals” (e355) and “Health services, systems, and policies” (e580): Issuing a referral for a follow-up visit at a medical centre by a health care provider was linked to e355 and e580 as this can be a facilitator to further treat the hearing disability.
Overall
demonstrates a summary of the categories that were covered in the database along with the methods which were linked to them.
includes the complete list of the categories of brief CSHL and identifies the covered and non-covered ones.
illustrates the absolute number and the respective percentages of the addressed ICF categories of both CSHL.
Not covered by ICF
After revealing the addressed categories of CSHL, the information that was included in the database, but not in CSHL was collected and categorised as either PF, “Time”, or “Health conditions” (Alfakir et al. Citation2019). These concepts were also not classified by nature in the full version of ICF. The age-related inquiries (see Appendices, Table A3) were categorised as “Time”. Gender, age, and occupation were categorised as PF (WHO Citation2001). Having HL family history was categorised as PF/Family History (Alfakir et al. Citation2019). Noise exposure was also categorised as PF/Noise exposures (Alfakir et al. Citation2019).
The information described above as “Health status, ear-related” was categorised as both Health conditions and PF/Medical History (van Leeuwen et al. Citation2017; Alfakir et al. Citation2019) except for the inquiries regarding Tinnitus and dizziness that were additionally linked to b2400 and b2401, respectively. “Ear surgery” was only linked to PF/Medical History. Arguably, ear surgery could be linked to “Health services, systems, and policies” (e580) (Alfakir et al. Citation2019), but as the inquiry was made as a part of the patient medical history with no further information, after consultation with experts, it was considered only as PF. “Health status, general” was categorised as both Health conditions and PF/Medical History (van Leeuwen et al. Citation2017; Alfakir et al. Citation2019) except for “chemotherapy” as PF/Treatment and “Regularly taking medication” as PF/Medication (Alfakir et al. Citation2019).
Discussion
The goal of this study was to evaluate the database generated at Hörzentrum Oldenburg gGmbH based on the patient’s ENT counselling hours with audiological focus under the ICF framework. In comparison with the typical ENT counselling, this database contains more measures that are essential for communication and interaction evaluation, such as speech intelligibility in noise and loudness perception. Although the database is not representative of the common ENT practice, it gives an insight which elements relevant for measuring individual hearing disability, interaction, and participation were already covered by the audiological focus and which ones are yet missing. The content of the database was compared to both CSHL. These non-representative clinical data were collected with the focus on mainly determining the patient’s hearing condition diagnosis and speech intelligibility ability. Therefore, as expected, more BF categories of comprehensive CSHL (27%) were covered in comparison with the AP (17%) and EF (12%) categories. “Hearing functions” were well addressed as all the third-level categories of it were covered. This means the patient’s hearing function was evaluated taking into account all the essential aspects recommended by the BF domain. All of the highly related categories; “Auditory perception”, “Hearing functions”, “Listening”, and “Sound” were evaluated in different ways by all of the methodologies except for ear examination.
The results showed that each of the applied methods was only partially capable of examining impairment according to IC. Therefore, to create a new broad ICF-based protocol for the HL diagnosis and rehabilitation, there is a fundamental need to combine a wide range of different methods and cover more ICF categories. Such protocol would allow for having a broad perspective of the patient’s disability and functioning status caused by HL.
Body functions: Two BF categories that are essential in HL evaluation (“Auditory perception” and “Sound detection”) were assessed with all of the methods (except for Ear examination). The possibility to link different methodologies to the same category indicates that the same concept was rated from different standpoints. Ideally, to design an ICF-based protocol, including more than one method linkable to a category should be expanded to all of the required categories to strengthen the outcome reliability.
Four of the unaddressed BF categories of the brief CSHL (temperament and personality, attention, memory, and emotional functions) are subsets of Chapter 1 (Mental functions). Although the categories of Chapter 3 (voice and speech functions) are only included in comprehensive CSHL, it can be beneficial to incorporate them when designing a broad ICF-based protocol. These categories can be covered using a self-assessment approach (e.g. questionnaire) and more deeply using standard behavioural studies and medical examinations.
Due to the importance of lateralisation of a sound source in the perception of both speech and nonspeech sounds (Granberg Citation2015), including the category “Lateralization of sound source” (b2303) in the comprehensive CSHL can emphasise the necessity of evaluating the lateralisation ability in HL assessment.
Body structures: In case, a category is only measurable by a single method, it would be necessary to ensure this methodology is included in the ICF-based protocol. In the present audiology-focused database, the methodology that was found to be the best approach to practically assess the structure of the ear was the ear examination and otoscopy. In more ENT-focused clinical data, the structure of the ear can also be evaluated using direct structure assessments such as imaging methods.
Activities and participation: A large group of missing AP categories were the subsets of Chapter 7; “Interpersonal interactions and relationship” which refers to the difficulty with having different types of interaction with people. The information required to cover these categories can be gathered with the use of a questionnaire.
The database analysis showed 16% of the patients reported having difficulty watching TV which is an example of performing activities for pleasure. The category “Recreation and leisure” (d920) is not included in the brief CSHL while HL can cause difficulty performing similar activities given by the description of code d920. According to the outcome of this study, as the brief CSHL must include minimum essential categories, it would be beneficial to add this category to the brief CSHL in the future.
The medical interview covered the highest number of categories. However, as the data extracted from this method reflects the patient’s personal perspective, a medical interview might potentially not be a reliable evaluation method when it comes to certain categories. In such cases, for reliability assessment, the data can be compared with the results of other methodologies that are linked to the same ICF category. For instance, the categories “Communicating with - receiving - spoken messages”, “Conversing with one person”, and “Conversing with many people” can be further examined using innovative approaches in which the communication ability can be graded by a researcher. Some recently developed methods include a questionnaire developed with the focus on the communication and conversation ability assessment, named HEAR-COMMAND TOOL (Afghah et al. Citation2021a, Citation2021b) and the inclusion of a communication measure with tasks like e.g. the Diapix task (Schuetze et al. Citation2020; Wagener et al. Citation2021) or the Live Evaluation of Auditory Preference (LEAP) test (Smeds et al. Citation2021).
Environmental factors: Half of the categories of EF in the comprehensive CSHL are the subsets of Chapters 3–5; “Support and Relationships”, “Attitudes”, and “Services, Systems, and Policies”. These categories were missing in the database as these concepts were not traditionally involved as a part of the diagnosis in an audiological clinic. This is where ICF involves the concepts that are not typically noted in the rehabilitation process but yet may have a profound impact on the patient’s life.
Conclusion
This study compared the content of a database created by applying five audiological methods with the brief and comprehensive ICF CSHL. The results showed that 44% of the brief categories and 18% of the comprehensive ones were covered. The patients’ listening ability and hearing functions were thoroughly evaluated. Based on the comprehensive CSHL, the effect of HL on the patients’ social life and activities as well as the impact of the surrounding environment on the patients’ functioning were poorly assessed (17% and 12% of AP and EF categories, respectively). The shortage in covering the third chapter of AP (communication) can be compensated by integrating more methodologies such as newly developed questionnaires or lab-based experiments to evaluate the HL along with the communication and conversation disability from a broader perspective according to the ICF classification.
Supplemental Material
Download PDF (483.8 KB)Acknowledgements
The authors would like to sincerely thank Prof. Razan Al fakir and Dr. Lisette Van Leeuwen for their invaluable input and guidance.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Afghah, Tahereh, Alfakir, Razan, Meis, Markus, van Leeuwen, Lisette, Kramer, Sophia E., Hammady, Mahmoud, Youssif, Mostafa, & Wagener, Kirsten C. 2021a. “The development of a Self-Rated ICF-based questionnaire (HEAR-COMMAND Tool) to evaluate hearing functioning, communication, and conversation disability: multinational researchers' and patients' perspective”. Preprint: Zenodo. doi: 10.5281/zenodo.5534359.
- Afghah, T., K. C. Wagener, J. Schütze, M. Meis, and B. Kollmeier. 2021b. “Conformities and Gaps of Clinical Audiological Data with the International Classification of Functioning Disability and Health Core Sets for Hearing Loss.” Preprint: Zenodo. doi:10.5281/zenodo.5534352.
- Alfakir, R., M. Hall, and A. Holmes. 2015. “How Can the Success Post Cochlear Implant Be Measured or Defined in Older Adults? Implications of the International Classification of Functioning Brief Core Set for Hearing Loss.” International Journal of Physical Medicine & Rehabilitation 3 (5): 302. doi:10.4172/2329-9096.1000302.
- Alfakir, R., A. E. Holmes, and F. Noreen. 2015. “Functional Performance in Older Adults with Hearing Loss: Application of the International Classification of Functioning Brief Core Set for Hearing Loss: A Pilot Study.” International Journal of Audiology 54 (9): 579–586. doi:10.3109/14992027.2015.1023903
- Alfakir, R., L. M. van Leeuwen, M. Pronk, S. E. Kramer, and D. A. Zapala. 2019. “Comparing the International Classification of Functioning, Disability, and Health Core Sets for Hearing Loss and Otorhinolaryngology/Audiology Intake Documentation at Mayo Clinic.” Ear and Hearing 40 (4): 858–869. doi:10.1097/AUD.0000000000000662.
- Brand, T., and V. Hohmann. 2002. “An Adaptive Procedure for Categorical Loudness Scaling.” The Journal of the Acoustical Society of America 112 (4): 1597–1604. doi:10.1121/1.1502902
- Brand, T., and B. Kollmeier. 2002. “Efficient Adaptive Procedures for Threshold and Concurrent Slope Estimates for Psychophysics and Speech Intelligibility Tests.” The Journal of the Acoustical Society of America 111 (6): 2801–2810. doi:10.1121/1.1479152. PMID: 12083215.
- Cieza, A., T. Brockow, T. Ewert, E. Amman, B. Kollerits, S. Chatterji, T. Berdihan Ustün, and G. Stucki. 2002. “Linking Health-Status Measurements to the International Classification of Functioning, Disability and Health.” Journal of Rehabilitation Medicine 34 (5): 205–210. doi:10.1080/165019702760279189.
- Cieza, Alarcos., Szilvia. Geyh, Somnath. Chatterji, Nenad. Kostanjsek, Bedirhan. Ustün, and Gerold. Stucki. 2005. “ICF Linking Rules: An Update Based on Lessons Learned.” Journal of Rehabilitation Medicine 37 (4): 212–218. doi:10.1080/16501970510040263.
- Danermark, Berth, Alarcos Cieza, Jean-Pierre Gangé, Francesca Gimigliano, Sarah Granberg, Louise Hickson, Sophia E. Kramer, et al. 2010. “International Classification of Functioning, Disability, and Health Core Sets for Hearing Loss: A Discussion Paper and Invitation.” International Journal of Audiology 49 (4): 256–262. doi:10.3109/14992020903410110.
- Danermark B, Granberg S, Kramer SE, Selb M, and Möller C. 2013. “The Creation of a Comprehensive and a Brief Core Set for Hearing Loss Using the International Classification of Functioning, Disability and Health.” American Journal of Audiology 22 (2): 323–328. doi:10.1044/1059-0889(2013/12-0052).
- Granberg, S. 2015. “Functioning and Disability in Adults with Hearing Loss: The Preparatory Studies in the ICF Core Sets for Hearing Loss Project.” Doctoral diss., Örebro university.URN: urn:nbn:se:oru:diva-45274
- Granberg, S., J. Dahlström, C. Möller, K. Kähäri, and B. Danermark. 2014b. “The ICF Core Sets for Hearing Loss-Researcher Perspective. Part I: Systematic Review of Outcome Measures Identified in Audiological Research.” International Journal of Audiology 53 (2): 65–76. doi:10.3109/14992027.2013.851799.
- Granberg, S., K. Möller, Å. Skagerstrand, C. Möller, and B. Danermark. 2014c. “The ICF Core Sets for Hearing Loss: Researcher Perspective, Part II: Linking Outcome Measures to the International Classification of Functioning, Disability and Health (ICF).” International Journal of Audiology 53 (2): 77–87. doi:10.3109/14992027.2013.858279.
- Granberg, S., M. Pronk, D. W. Swanepoel, S. E. Kramer, H. Hagsten, J. Hjaldahl, C. Möller, and B. Danermark. 2014d. “The ICF Core Sets for Hearing Loss Project: functioning and Disability from the Patient Perspective.” International Journal of Audiology 53 (11): 777–786. doi:10.3109/14992027.2014.938370.
- Granberg, S., D. W. Swanepoel, U. Englund, C. Möller, and B. Danermark. 2014a. “The ICF Core Sets for Hearing Loss Project: International Expert Survey on Functioning and Disability of Adults with Hearing Loss Using the International Classification of Functioning, Disability, and Health (ICF).” International Journal of Audiology 53 (8): 497–506. doi:10.3109/14992027.2014.900196.
- Jerger, J. 1970. “Clinical Experience with Impedance Audiometry.” Archives of Otolaryngology (Chicago, IL: 1960) 92 (4): 311–324. doi:10.1001/archotol.1970.04310040005002.
- Karlsson, E., E. Mäki-Torkko, S. Widén, J. Gustafsson, V. Manchaiah, F. Mahomed-Asmail, K. Yerraguntla, and S. Granberg. 2021. “Validation of the Brief International Classification of Functioning, Disability and Health (ICF) Core Set for Hearing Loss: An International Multicentre Study.” International Journal of Audiology 60 (6): 412–419. doi:10.1080/14992027.2020.1846088.
- Kollmeier, B., and M. Wesselkamp. 1997. “Development and Evaluation of a German Sentence Test for Objective and Subjective Speech Intelligibility Assessment.” The Journal of the Acoustical Society of America 102 (4): 2412–2421. doi:10.1121/1.419624.
- Oetting, D., T. Brand, and S. D. Ewert. 2014. “Optimized Loudness-Function Estimation for Categorical Loudness Scaling Data.” Hearing Research 316: 16–27. doi:10.1016/j.heares.2014.07.003. Epub 2014 Jul 21. PMID: 25058812.
- Oltman, R., G. Neises, D. Scheible, G. Mehrtens, and C. Grüneberg. 2008. “ICF Components of Corresponding Outcome Measures in Flexor Tendon Rehabilitation – A Systematic Review.” BMC Musculoskeletal Disorders 9: 139. doi:10.1186/1471-2474-9-139.
- Olusanya, B. O., A. C. Davis, and H. J. Hoffman. 2019. “Hearing Loss Grades and the International Classification of Functioning, Disability and Health.” Bulletin of the World Health Organization 97 (10): 725–728. doi:10.2471/BLT.19.230367
- Schuetze, J., M. Yadav, M. Hendrikse, B. Kollmeier, and K. C. Wagener. 2020. A pilot study of realistic communication in a simulated restaurant acoustic environment. Fortschritte der Akustik – DAGA 2020, Dt. Ges. f. Akustik, Berlin.
- Selb, M., R. Escorpizo, N. Kostanjsek, G. Stucki, B. ÜSTüN, and A. Cieza. 2015. “A Guide on How to Develop an International Classification of Functioning, Disability and Health Core Set.” European Journal of Physical and Rehabilitation Medicine 51 (1): 105–117. PMID: 24686893
- Smeds, K., J. Larsson, M. Dahlquist, F. Wolters, and P. Herrlin. 2021. “Live Evaluation of Auditory Preference, a Laboratory Test for Evaluating Auditory Preference.” Journal of the American Academy of Audiology 32 (8): 487–500. doi: 10.1055/s-0041-1735213
- Stevens, G., S. Flaxman, E. Brunskill, M. Mascarenhas, C. D. Mathers, and M. Finucane, Global Burden of Disease Hearing Loss Expert Group. 2013. “Global and Regional Hearing Impairment Prevalence: An Analysis of 42 Studies in 29 Countries.” European Journal of Public Health 23 (1): 146–152. doi:10.1093/eurpub/ckr176.
- van Leeuwen, L. M., P. Merkus, M. Pronk, M. van der Torn, M. Maré, S. T. Goverts, and S. E. Kramer. 2017. “Overlap and Nonoverlap between the ICF Core Sets for Hearing Loss and Otology and Audiology Intake Documentation.” Ear and Hearing 38 (1): 103–116. doi:10.1097/AUD.0000000000000358. PMID: 27556527.
- Wagener, K. C. T. Afghah, J. Schütze, M. Meis, and B. Kollmeier. 2021. “Facing the Individual Hearing Demands in Personalized Hearing Rehabilitation.” In 15th European Federation of Audiology Societies (EFAS), May 20.
- World Health Organization. 1992. International Statistical Classification of Diseases and Related Health Problems, the 10th Revision, Volume 1, Geneva: WHO.
- World Health Organization (WHO). 2001. International Classification of Functioning, Disability, and Health. World Health Organization (WHO). Geneva: WHO. http://www.who.int/classifications/icf/en/
- World Health Organization. 2002. “Towards a Common Language for Functioning, Disability, and Health: ICF.” The International Classification of Functioning, Disability and Health 2002.
- World Health Organization. 2013. How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF). Exposure draft for comment. Geneva: WHO, 10.
- World Health Organization. 2021. World report on hearing.
- World Health Organisation Grades of Hearing Impairment. 2008. European Commission. https://ec.europa.eu/health/scientific_committees/opinions_layman/en/hearing-loss-personal-music-player-mp3/figtableboxes/table-4.htm. Accessed on May 20, 2021.
- World Health Organization’s International Classification of Functioning, Disability, and Health. ICF Browser, an online application of the ICF: http://www.who.int/classifications/icfbrowser. Accessed on May 25, 2022.
