ABSTRACT
This paper introduces a contemporary psychodynamic attachment approach for managing chronic illnesses with a focus on the role of impairments in mentalizing, attachment, and epistemic trust. This approach emphasizes the significance of relational dynamics in healthcare settings and may thus provide a complementary approach in health psychology which currently primarily targets individual and behavioral aspects of chronic illness by addressing the relational dynamics that are typically involved in chronic illness management. We review empirical evidence highlighting the roles of mentalizing, attachment, and epistemic trust in chronic illness. We propose an attachment and mentalizing-based healthcare paradigm that prioritizes relational dynamics that aligns with emerging health psychology trends, offering a holistic approach to patient care. Finally, we present some practical implications of this approach, underscoring the importance of psychologists working in health in fostering secure attachment, epistemic trust and mentalizing within patient-provider relationships. This involves tailoring patient interactions and psychoeducation to individual needs and narratives, enhancing treatment adherence and well-being.
Introduction
Health psychology explores the complex interplay of psychological, behavioral, and cultural factors and their impact on physical health and illness. A key focus within this field is the management of chronic disease, particularly emphasizing the critical role of treatment adherence, defined as the extent to which patients follow their prescribed medication regimen (Vrijens et al., Citation2012).
Patient behavior is typically seen as a key determinant of treatment efficacy in this context with a direct impact on health outcomes and quality of life (Paterick et al., Citation2017), but evidence consistently shows that maintaining regular medical adherence poses a substantial challenge for many patients (Burkhart & Sabaté, Citation2003; Kim et al., Citation2018). These findings highlight an urgent need for health psychology to improve its understanding of these dynamics and develop strategies to address the issue of adherence in chronic disease management effectively.
In recognizing the profound impact of psychological factors on health-related decision-making, health psychology approaches characteristically examine a number of factors influencing adherence. This includes understanding the disease, its progression, and treatment; patient perceptions of medication regarding effectiveness, side effects, costs, and acceptability; and access to treatment. It also considers the patient’s life situation, including personal circumstances, resources, social support, and competing priorities (Atinga et al., Citation2018; Nakajima et al., Citation2021; Oates et al., Citation2020; van der Laan et al., Citation2019).
However, both meta-analyzes and systematic reviews highlight limitations in the effectiveness of traditional approaches in the management of chronic disease (Burnier, Citation2023; Cross et al., Citation2020; Kini & Ho, Citation2018; Nieuwlaat et al., Citation2014)
The limited effectiveness of certain health psychology approaches might be partially attributed to their insufficient focus on relational aspects. Historically, health psychology has prioritized individual behavior and cognition, frequently neglecting the significant influence of a patient’s relational environment. This oversight is somewhat surprising, especially considering the growing body of evidence indicating that the quality of relationships, including those with healthcare providers and the health system, profoundly impacts the management of chronic illnesses. For example, involving patients in decision-making processes has shown enhanced success (Schneider et al., Citation2022), and the quality of the patient-provider relationship is a recognized factor in treatment adherence (Beach et al., Citation2006, Citation2015; Oetzel et al., Citation2015). Moreover, the ability of physicians to communicate effectively, build robust physician-patient relationships, and empower patients is considered vital for adherence (Burnier & Egan, Citation2019). The principles of Trauma-Informed Care (TIC) further reinforce this perspective by emphasizing the need to understand and integrate an individual’s developmental history, past trauma, and current relational dynamics into healthcare interactions (Substance Abuse and Mental Health Services Administration [SAMHSA], Citation2015).
Contemporary psychodynamic theories provide a more relational approach to managing chronic illness (Abbass et al., Citation2009; Costa-Cordella et al., Citation2020a, Citation2020b; Hunter & Maunder, Citation2015; Luyten et al., Citation2012)
In this paper, we discuss the contemporary attachment and mentalizing-based approaches in healthcare as a conceptual framework. Firstly, we present a model that explains the relationship between attachment, mentalizing, epistemic trust, and chronic illnesses. Secondly, we summarize the empirical findings related to chronic illnesses in the context of this theoretical framework. Finally, we provide practical implications of an attachment-mentalizing model applied in health psychology.
Attachment, mentalizing and epistemic trust in chronic illness
Contemporary psychodynamic models provide a comprehensive relational approach to understanding and intervening in populations with chronic illnesses, focusing on relational factors that affect psychological adjustment and disease management. These models emphasize the significance of attachment in the course of chronic diseases (Koelen et al., Citation2014; Luyten & Fonagy, Citation2016; Luyten et al., Citation2012, Citation2013; Malberg & Mayes, Citation2013; Schoenberg et al., Citation2014).
From this perspective, the bodily distress implied in chronic illnesses is seen as a factor influencing problems in attachment, mentalizing (i.e., the capacity to reflect on one’s own self and others), and epistemic trust (i.e., the capacity to trust others, including clinicians as a source of knowledge) (Luyten et al., Citation2010; Citation2020).
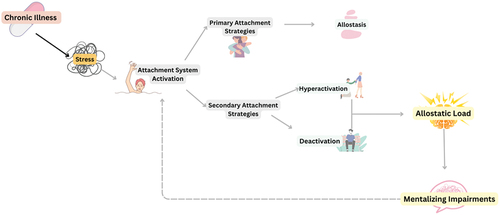
In the context of chronic illness, the activation of the attachment system and subsequent mentalizing impairments present a complex interplay of psychological and physiological responses (see ). From an attachment-mentalizing perspective, somatic discomfort is a significant stressor, triggering a cascade of responses to reestablish allostasis (the achievement of stability through change; McEwen, Citation2007), which can lead to an allostatic load, a disruption of the body’s stress due to extended physical or psychological stress (McEwen, Citation2007). The stress response involves both physiological and psychological systems, central to which is the need for co-regulation within attachment relationships (Luyten & Fonagy, Citation2018). The attachment system is a biobehavioural mechanism central to the stress response. Normally, the presence of responsive attachment figures helps down-regulate distress, supported by the mesocorticolimbic dopaminergic reward system (Diamond et al., Citation2003; Sbarra et al., Citation2008). However, in chronic illnesses, this down-regulation is compromised due to persistent somatic issues where proximity seeking provides only temporary relief. This failure of the primary attachment strategies leads to the individual relying on secondary attachment strategies, such as hyperactivating (desperately seeking support) or deactivating (denying distress and the need for help) the attachment system (Mikulincer & Shaver, Citation2007). These strategies, while adaptive in the short term, ultimately hinder long-term recovery and the ability to seek and benefit from help, including psychological support. The resulting increase in allostatic load can lead to feelings of disappointment, loneliness, or overwhelm (Maunder & Hunter, Citation2008).
This has also implications for neurobiological systems implicated in the regulation of stress. In cases of chronic illness, where the source of stress is internal and constant, there might be a failure of downregulation of the stress system, especially of the HPA axis, which has been associated with a wide array of dysregulations in other neurobiological systems, including the immune system and systems for pain processing (McEwen, Citation2007). In this context, the individual’s ability to mentalize, and embodied mentalizing, can be significantly compromised (Luyten et al., Citation2012). When mentalizing is compromised, three non-mentalizing modes could emerge, which, in the context of chronic illnesses, are expressed as follows:
Pretend Mode functioning: In pretend mode, the individual’s thoughts and feelings become decoupled from the external world. This could be seen in chronic illness as the individual minimizing or ignoring their illness’s impact, discussing it in a detached manner. Parents of children with chronic conditions might display this by discussing the condition in detail but remaining disconnected from their emotional responses. They might focus excessively on medical interventions, neglecting their child’s emotional needs, and fail to fully grasp the illness’s overall impact on the child’s life.
Psychic Equivalence: This mode involves conflating internal feelings with external realities, leading to distorted perceptions. For example, a person with diabetes might irrationally fear death from consuming any sugar, equating an internal sense of danger with an inaccurate external reality. Parents might project their anxieties onto their child’s condition, resulting in overprotective behaviors like micromanaging the child’s diet, which can create conflict and undermine the child’s autonomy.
Teleological Mode: This mode often involves engaging in harmful behaviors to achieve specific goals, neglecting broader health implications. For instance, an individual might omit insulin or self-harm to induce medical crises for attention. Caregivers in this mode might focus narrowly on certain health outcomes, like blood sugar levels, while neglecting other aspects of well-being, leading to an unbalanced approach to health management. Medical teams might also adopt this mind-set, focusing on specific health metrics at the expense of the patient’s overall quality of life.
Current evidence on mentalizing-attachment- epistemic trust and chronic illnesses
Numerous studies have highlighted the importance of attachment styles in chronic illnesses (P. Ciechanowski et al., Citation2004 McWilliams & Bailey, Citation2010; Ravitz et al., Citation2010). For instance, in Type 1 Diabetes, patients with avoidant attachment styles have been found to exhibit lower treatment adherence compared to those with secure or anxious attachment (P. S. Ciechanowski et al., Citation2001). Also, attachment plays a significant role in the caregiving relationship between patients and health providers. Studies, such as one involving adults with diabetes (N = 4,095), have shown that a secure attachment between patient and physician leads to better collaboration and treatment adherence (P. Ciechanowski et al., Citation2004). This evidence highlights the importance of caregiving relationships in healthcare settings.
Similarly, in the context of children with chronic illnesses, the caregiver-child relationship is crucial. The mental health of caregivers and children mutually affects and is influenced by the condition, potentially altering the illness’s trajectory (Hilliard et al., Citation2011; Landolt et al., Citation2002; Lohan et al., Citation2015). For example, parents of children with DM1 who exhibit avoidant attachment face greater stress and more challenges in managing the disease (Moreira & Canavarro, Citation2016).
Further exploring these caregiving dynamics, studies like those by Costa-Cordella et al. (Citation2020a) reveal the intricate links between attachment, stress, and disease outcomes in children with DM1 and their caregivers. Bizzi et al. (Citation2021) found that while insecure attachment in children did not directly affect diabetes control, it significantly impacted their psychological adaptation to the condition.
Similar patterns have been observed in patients with Lupus, chronic pain, and medically unexplained symptoms, where avoidant attachment is associated with lower adherence and quality of life (Bennett et al., Citation2011; Davies et al., Citation2009; Taylor et al., Citation2012).
The role of mentalizing, particularly the impairments in embodied mentalizing, has been extensively demonstrated in chronic illness. Mentalizing refers to the capacity to interpret our own and others’ behaviors in terms of their underlying mental states (Bateman & Fonagy, Citation2006). Various research traditions have focused on the role of impairments in this capacity, either premorbidly or as a consequence of somatic disorders, in chronic illness. Consistent with these assumptions, research has demonstrated problems with both primary or secondary alexithymia (Taylor et al., Citation2013) and emotional awareness (Lane et al., Citation1990) among patients with functional somatic disorders.
Fonagy and Moran (Citation1987, Citation1994) conducted a series of studies at the Anna Freud Centre, focusing on individual psychotherapy and group therapy sessions for children and adolescents with Type 1 diabetes. Their work was among the first to demonstrate a significant association between relational dynamics and specific indicators of diabetes, such as the link between caregiver-daughter relationship conflicts and hypoglycemia (Fonagy & Moran, Citation1990; G. Moran et al., Citation1991).
A number of recent reviews has demonstrated the role of impairments in (embodied) mentalizing in chronic illness and in functional somatic disorders such as in chronic pain and fatigue conditions in adults. There are currently less studies on the role of impairments in mentalizing in children, young people and their carers, although this body of research is rapidly growing (Bizzi et al., Citation2021; Costa-Cordella et al., Citation2020a, Citation2020b; Garrett et al., Citation2019, Citation2021; Thomakos et al., Citation2019)
For instance, we (Costa-Cordella et al., Citation2020b) conducted a study in children with Type 1 diabetes, revealing significant correlations between parental and child mentalization and diabetes outcomes, including metabolic control and treatment adherence. Notably, this study found that mother-child dyads with higher levels of mentalization tended to have better diabetes outcomes. These findings can be understood by examining the impact of parental mentalizing. Theoretically and empirically, parental mentalizing is seen as key to comprehending children’s emotions, aiding in their emotional regulation and stress management. This is crucial for maintaining psychological well-being and adopting necessary behaviors for diabetes management, particularly under the stress of challenging situations like receiving a diagnosis. For instance, caregivers with high reflective functioning are more adept at recognizing their own distress and understanding the mental states of their child prompted by the diagnosis. This ability is critical for assisting the child in identifying and regulating emotions, ultimately managing their stress response more effectively.
Epistemic trust in chronic illness management
Besides impairments in attachment and embodied mentalizing, individuals with chronic illness may also shows high levels of epistemic mistrust. Epistemic trust, as defined by Peter Fonagy and colleagues, is the ability to perceive information from others as trustworthy, relevant, and applicable to oneself (Fonagy et al., Citation2015, Citation2017).
In psychotherapy, establishing ET is a central therapeutic goal, highlighting its importance in the therapeutic relationship (Fonagy & Allison, Citation2014). Many patients with chronic illnesses present epistemic mistrust, either premorbidly or as a result of unhelpful interactions with health professionals. Epistemic mistrust refers to skepticism or disbelief in the validity of knowledge and information provided. This mistrust can be premorbid, often rooted in the individual’s early life experiences and attachment patterns. Additionally, this mistrust can also develop or intensify as a consequence of negative interactions with the healthcare system. Patients with chronic illnesses often navigate complex medical systems and may encounter dismissive, contradictory, or overly clinical interactions with health professionals. This can exacerbate feelings of being misunderstood or not taken seriously, particularly in cases where even though the biological basis of their condition is clear, their psychological and emotional experiences are neglected.
We suggest that epistemic trust’s significance extends to all healthcare interactions, underpinning the dynamics between patient and health provider. Even though epistemic trust is not the primary goal in healthcare interactions, its achievement should be central to ensuring effective communication of relevant information for the patient to adhere to treatments adequately.
Ostensive cues like eye contact and responsive communication are central to establishing epistemic trust (Csibra & Gergely, Citation2006, Citation2009, Citation2011; Gergely & Csibra, Citation2005). These cues signal the intent to convey new, relevant information (Csibra & Gergely, Citation2006, Citation2011). Gergely and Csibra’s experimental studies highlight that effective knowledge sharing relies on such ostensive communication rather than mere observational learning (Csibra & Gergely, Citation2009). These nonverbal cues foster a “pedagogic stance,” creating a conducive environment for exchanging cultural knowledge. This approach enhances the likelihood that the recipient will perceive the information as significant to their own experiences, aiding its retention and application (Kiraly et al., Citation2013).
Ostensive cues act as an acknowledgment by the communicator of the recipient’s mental capacity and agency (Max Weber’s concept of agency, Citation1922). This recognition leads to “shared intentionality,” a concept described by Tomasello and Carpenter (Citation2007), which entails a collaborative pursuit of goals and intentions. Consequently, this process encourages the recipient to learn from someone whom they perceive as understanding them.
Furthermore, this interaction prompts recipients to reduce their inherent epistemic vigilance – a natural, self-protective skepticism. Relaxing this vigilance increases the likelihood that individuals will perceive the shared information as both relevant and significant to their personal experiences.
In the realm of healthcare, particularly in managing chronic illnesses, when patients perceive that their healthcare providers are genuinely concerned and attuned to their personal narratives, a vital bridge forms. This connection facilitates the effective and meaningful transfer of knowledge, significantly enhancing chronic illness management. In this collaborative environment, patients are presented with a unique opportunity to gain valuable and pertinent knowledge.
This interaction between the patient and healthcare provider helps to reduce the patients’ innate epistemic vigilance toward new information, fostering a space of openness and receptivity. This is exemplified in psychotherapy, where it’s observed that patients who trust their therapists to provide relevant and applicable information are more likely to engage in the therapy process and achieve better outcomes (Li et al., Citation2023; Riedl et al., Citation2023).
This is particularly important to be considered in the context of patients with comorbid mental disorders. These individuals often struggle to strike the right balance between epistemic vigilance and credulity, leading to potential issues in treatment adherence – either through disregarding medical advice or indiscriminately following multiple sources of advice. For instance, patients with Borderline Personality Disorder (BPD), often described as challenging to engage, might benefit from tailored approaches to effectively build epistemic trust.
More research concerning the role of epistemic trust in health care is needed, is the application of this concept may considerably improve the relationship between health care providers and patients struggling with chronic medical conditions, and thus ultimately lead to improved health outcomes.
Practical applications in health psychology
Psychologists working in healthcare contexts have a unique opportunity to bring mentalization into the realm of healthcare. Clinicians can have a role in integrating this approach into team-based healthcare, improving patient adherence to treatment and overall care.
Bringing the mind into the conversation should be a fundamental aspect of treating chronic illness. This approach should also extend to medical practitioners as a means to build (epistemic) trust. As we discussed above, establishing trust starts with showing genuine interest in the patient’s mind. This interest lays the groundwork for an open communication channel, enabling patients to receive and process the information provided more effectively. Recognizing the patient as an agent with a mind, with all its mental aspects, thus, is crucial. By creating a secure attachment environment and integrating mentalization into care, healthcare providers can establish trust, enhancing patients’ understanding and belief in their treatment plans.
More specifically, health psychologists can play a pivotal role in evaluating epistemic trust and tailoring communication strategies for each patient to foster trust with healthcare providers. This involves guiding medical professionals on how to interact with each patient effectively, acting as a bridge to establish epistemic trust in patient-provider relationships.
Regarding individual interventions in health psychology, a specific modification could involve the psychoeducational component. This includes tailoring the content and delivery of psychoeducation in a way that ties it contingently with the illness-related themes and consultation motives. The therapist’s expertise doesn’t necessarily require prior knowledge of the patient’s experience with their illness to generate a sense of agency recognition. However, incorporating knowledge about common experiences of people with certain conditions, like diabetes, is relevant, especially in the psychoeducation component, since it often forms the basis of consultations.
For instance, explicitly emphasizing epistemic trust could be crucial in the context of psychoeducation and illness-specific education. By acknowledging and understanding the patient’s personal narrative, healthcare providers can create an environment where the patient feels truly understood. This understanding fosters a willingness in the patient to learn from the provider who has shown a genuine comprehension of their experience.
Discussion and conclusions
The integration of contemporary psychodynamic theories, specifically focusing on mentalizing, attachment, and epistemic trust, into health psychology represents an innovative approach to managing chronic illnesses. In this paper, we have explored how these concepts can transform the care of individuals with chronic conditions by addressing the relational dynamics that play a crucial role in treatment adherence and overall well-being.
Incorporating mentalizing theory into healthcare, particularly in managing chronic illnesses, offers a comprehensive approach to patient care. This paradigm shift involves understanding patients’ behaviors and delving deeper into their relational and psychological dynamics. Training healthcare providers to recognize and respond to the mental states of their patients is essential, fostering a secure attachment environment that promotes trust and adherence to treatment. Establishing epistemic trust between healthcare providers and patients is essential for effective chronic illness management, as it facilitates open communication and enables patients to receive and integrate information more effectively. Health psychologists can play a pivotal role in evaluating and fostering this trust, tailoring communication strategies to each patient’s needs.
Notably, the approach presented in this paper shares some similarities with significant advancements in the field, particularly with the trauma-informed care (TIC) approach (SAMHSA, Citation2015). TIC recognizes the profound influence of an individual’s developmental history, childhood experiences, and the impact of both past and present relationships on health. Despite the progress embodied by TIC, there remains a noticeable gap in understanding the specifics of relational dynamics, particularly aspects like trust. While TIC commendably acknowledges the relational dynamic, it primarily focuses on avoiding re-traumatization rather than actively fostering trust between individuals and health providers. This distinction is critical, especially in the context of chronic illnesses, where establishing deep trust in healthcare relationships is essential. Our approach aims to extend beyond the scope of TIC by recognizing the importance of relational dynamics and actively working toward building genuine trust in healthcare settings, a vital component in effectively managing chronic conditions.
Building on the discussion of trauma-informed care, it becomes evident that patients with chronic illnesses who have a history of trauma warrant special attention. This demographic is particularly vulnerable. Individuals with a history of trauma, compounded by the diagnosis of a chronic illness, are at a heightened risk of non-adherence to treatment and encountering additional mental health challenges (Flaherty et al., Citation2009; Maaranen et al., Citation2004; Wang et al., Citation2022). It is crucial to address their trauma sensitively, adhering to the principles of trauma-informed care while also incorporating additional considerations tailored to their unique needs. This approach involves a delicate balance between acknowledging their traumatic past and ensuring that the management of their chronic condition does not inadvertently lead to retraumatization. Therefore, while applying the principles of trauma-informed care, health professionals must also focus on building robust, trust-based relationships with these patients, enhancing their capacity to engage effectively in their treatment and care plans.
Chronic illness may lead to disruptions in mentalizing, particularly under the stress of managing a prolonged condition. These disruptions can significantly affect how individuals and caregivers perceive and manage the illness. Recognizing and addressing these disruptions are vital in designing interventions that cater to the psychological needs of patients, especially those with a trauma background.
The integration of these psychodynamic concepts into health psychology offers practical implications for healthcare providers. Psychologists working in healthcare settings can aid in fostering epistemic trust and mentalizing within patient-provider relationships. Tailoring communication strategies to individual patients and incorporating psychoeducation that acknowledges and addresses their personal narratives and mental states can significantly enhance treatment adherence and patient well-being.
Further research is necessary to fully understand the interplay of mentalizing, attachment, and epistemic trust in chronic illness management, especially in diverse healthcare settings and populations. Longitudinal studies would provide valuable insights into the long-term effects of these interventions on health outcomes and quality of life for individuals with chronic illnesses.
In conclusion, this paper underscores the potential benefits of a psychodynamic approach in health psychology, especially in managing chronic illnesses. Focusing on relational dynamics and deeper psychological processes offers a more comprehensive understanding and effective intervention strategies. Integrating mentalizing, attachment, and epistemic trust into health psychology represents a promising avenue for enhancing patient care and improving health outcomes in chronic illness management.
Patient anonymization statement
Potentially personally identifying information presented in this article that relates directly or indirectly to an individual, or individuals, has been changed to disguise and safeguard the confidentiality, privacy and data protection rights of those concerned, in accordance with the journal’s anonymization policy.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Abbass, A., Kisely, S., & Kroenke, K. (2009). Short-term psychodynamic psychotherapy for somatic disorders: Systematic review and meta-analysis of clinical trials. Psychotherapy and Psychosomatics, 78(5), 265–274. https://doi.org/10.1159/000228247
- Atinga, R. A., Yarney, L., Gavu, N. M., & Barengo, N. C. (2018). Factors influencing long-term medication non-adherence among diabetes and hypertensive patients in Ghana: A qualitative investigation. PLOS ONE, 13(3), e0193995. https://doi.org/10.1371/journal.pone.0193995
- Bateman, A., & Fonagy, P. (2006). Mentalizing and borderline personality disorder. In J. G. Allen & P. Fonagy (Eds.), The handbook of mentalization-based treatment (pp. 185–200). John Wiley & Sons, Inc. https://doi.org/10.1002/9780470712986.ch9
- Beach, M. C., Keruly, J., & Moore, R. D. (2006). Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? Journal of General Internal Medicine, 21(6), 661–665. https://doi.org/10.1111/j.1525-1497.2006.00399.x
- Beach, M. C., Roter, D. L., Saha, S., Korthuis, P. T., Eggly, S., Cohn, J., Sharp, V., Moore, R. D., & Wilson, I. B. (2015). Impact of a brief patient and provider intervention to improve the quality of communication about medication adherence among HIV patients. Patient Education and Counseling, 98(9), 1078–1083. https://doi.org/10.1016/j.pec.2015.05.011
- Bennett, J. K., Fuertes, J. N., Keitel, M., & Phillips, R. (2011). The role of patient attachment and working alliance on patient adherence, satisfaction, and health-related quality of life in lupus treatment. Patient Education and Counseling, 85(1), 53–59. https://doi.org/10.1016/j.pec.2010.08.005
- Bizzi, F., Della Vedova, A. M., Prandi, E., Cavanna, D., & Manfredi, P. (2021). Attachment representations to parents and emotional-behavioural problems: A comparison between children with type 1 diabetes mellitus and healthy children in middle childhood. Clinical Child Psychology and Psychiatry, 26(2), 393–405. https://doi.org/10.1177/1359104520987871
- Burkhart, P. V., & Sabaté, E. (2003). Adherence to long-term therapies: Evidence for action. Journal of Nursing Scholarship, 35(3), 207. https://doi.org/10.1111/j.1547-5069.2003.tb00001.x
- Burnier, M. (2023). The role of adherence in patients with chronic diseases. European Journal of Internal Medicine, 119, 1–5. https://doi.org/10.1016/j.ejim.2023.07.008
- Burnier, M., & Egan, B. M. (2019). Adherence in hypertension. Circulation Research, 124(7), 1124–1140. https://doi.org/10.1161/CIRCRESAHA.118.313220
- Ciechanowski, P. S., Katon, W. J., Russo, J. E., & Walker, E. A. (2001). The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. The American Journal of Psychiatry, 158(1), 29–35. https://doi.org/10.1176/appi.ajp.158.1.29
- Ciechanowski, P., Russo, J., Katon, W., Von Korff, M., Ludman, E., Lin, E., Simon, G., & Bush, T. (2004). Influence of patient attachment style on self-care and outcomes in diabetes. Psychosomatic Medicine, 66(5), 720–728. https://doi.org/10.1097/01.psy.0000138125.59122.23
- Costa-Cordella, S., Luyten, P., Cohen, D., Mena, F., & Fonagy, P. (2020a). Mentalizing in mothers and children with type 1 diabetes. Development and Psychopathology, 33(1), 216–225. https://doi.org/10.1017/S0954579419001706
- Costa-Cordella, S., Luyten, P., Giraudo, F., Mena, F., Shmueli-Goetz, Y., & Fonagy, P. (2020b). Apego y estrés en niños con Diabetes tipo 1 y sus madres. Revista Chilena de Pediatria, 91(1), 68–75. https://doi.org/10.32641/rchped.v91i1.1197
- Cross, A. J., Elliott, R. A., Petrie, K., Kuruvilla, L., & George, J. (2020). Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database of Systematic Reviews, 2020(5). https://doi.org/10.1002/14651858.CD012419.pub2
- Csibra, G., & Gergely, G. (2006). Social learning and social cognition: The case for pedagogy. In Y. Munakata & M. H. Johnson (Eds.), Processes of Change in Brain and Cognitive Development: Attention and Performance XXI (pp. 249–274). Oxford University Press.
- Csibra, G., & Gergely, G. (2009). Natural pedagogy. Trends in Cognitive Sciences, 13(4), 148–153. PMID:19285912. https://doi.org/10.1016/j.tics.2009.01.005
- Csibra, G., & Gergely, G. (2011). Natural pedagogy as evolutionary adaptation. Philosophical Transactions of the Royal Society B: Biological Sciences, 366(1567), 1149–1157. PMID:21357237. https://doi.org/10.1098/rstb.2010.0319
- Davies, A. N., Dickman, A., Reid, C., Stevens, A. M., Zeppetella, G., & Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. (2009). The management of cancer-related breakthrough pain: Recommendations of a task group of the science committee of the association for palliative medicine of Great Britain and Ireland. European Journal of Pain (London, England), 13(4), 331–338. https://doi.org/10.1016/j.ejpain.2008.06.014
- Diamond, D., Stovall McClough, C., Clarkin, J. F., & Levy, K. N. (2003). Patient-therapist attachment in the treatment of borderline personality disorder. Bulletin of the Menninger Clinic, 67(3), 227–259. https://doi.org/10.1521/bumc.67.3.227.23433
- Flaherty, E. G., Thompson, R., Litrownik, A. J., Zolotor, A. J., Dubowitz, H., Runyan, D. K., English, D. J., & Everson, M. D. (2009). Adverse childhood exposures and reported child health at age 12. Academic Pediatrics, 9(3), 150–156. https://doi.org/10.1016/j.acap.2008.11.003
- Fonagy, P., & Allison, E. (2014). The role of mentalizing and epistemic trust in the therapeutic relationship. Psychotherapy Theory, Research, Practice, Training, 51(3), 372–380. PMID:24773092. https://doi.org/10.1037/a0036505
- Fonagy, P., Luyten, P., & Allison, E. (2015). Epistemic petrification and the Restoration of epistemic Trust: A new conceptualization of borderline personality disorder and its psychosocial treatment. Journal of Personality Disorders, 29(5), 575–609. https://doi.org/10.1521/pedi.2015.29.5.575
- Fonagy, P., Luyten, P., Allison, E., & Campbell, C. (2017). What we have changed our minds about: Part 1. Borderline personality disorder as a limitation of resilience. Borderline Personality Disorder and Emotion Dysregulation, 4(11). PMID:28413687. https://doi.org/10.1186/s40479-017-0061-9
- Fonagy, P., & Moran, G. S. (1990). Studies on the efficacy of child psychoanalysis. Journal of Consulting and Clinical Psychology, 58(6), 684–695. https://doi.org/10.1037/0022-006X.58.6.684
- Fonagy, P., & Moran, G. S. (1994). Psychoanalytic formulation and treatment of chronic metabolic disturbance in insulin-dependent diabetes mellitus. Whurr Publications.
- Garrett, C. J., Choudhary, P., Amiel, S. A., Fonagy, P., & Ismail, K. (2019). Recurrent diabetic ketoacidosis and a brief history of brittle diabetes research: Contemporary and past evidence in diabetic ketoacidosis research including mortality, mental health and prevention. Diabetic Medicine, 36(11), 1329–1335.
- Garrett, C. J., Ismail, K., & Fonagy, P. (2021). Understanding developmental psychopathology in type 1 diabetes through attachment, mentalisation and diabetes distress. Clinical Child Psychology and Psychiatry, 26(3), 682–694. https://doi.org/10.1177/1359104521994640
- Gergely, G., & Csibra, G. (2005). The social construction of the cultural mind: Imitative learning as a mechanism of human pedagogy. Interaction Studies, 6(3), 463–481. https://doi.org/10.1075/is.6.3.10ger
- Hilliard, M. E., Monaghan, M., Cogen, F. R., & Streisand, R. (2011). Parent stress and child behaviour among young children with type 1 diabetes. Child: Care, Health and Development, 37(2), 224–232. https://doi.org/10.1111/j.1365-2214.2010.01162.x
- Kim, J., Combs, K., Downs, J., & Tillman, F. (2018). Medication adherence: The elephant in the room. US Pharmacist, 43(1), 30–34.
- Kini, V., & Ho, P. M. (2018). Interventions to improve medication adherence: A review. JAMA, 320(23), 2461–2473. https://doi.org/10.1001/jama.2018.19271
- Kiraly, I., Csibra, G., & Gergely, G. (2013). Beyond rational imitation: Learning arbitrary means actions from communicative demonstrations. Journal of Experimental Child Psychology, 116(2), 471–486. PMID:23499323. https://doi.org/10.1016/j.jecp.2012.12.003
- Koelen, J. A., Eurelings-Bontekoe, E. H., van Broeckhuysen-Kloth, S. A., Snellen, W. M., & Luyten, P. (2014). Social cognition and levels of personality organization in patients with somatoform disorders: A case-control study. The Journal of Nervous and Mental Disease, 202(3), 217–223. https://doi.org/10.1097/NMD.0000000000000097
- Landolt, M. A., Ribi, K., Laimbacher, J., Vollrath, M., Gnehm, H. E., & Sennhauser, F. H. (2002). Posttraumatic stress disorder in parents of children with newly diagnosed type 1 diabetes. Journal of Pediatric Psychology, 27(7), 647–652. https://doi.org/10.1093/jpepsy/27.7.647
- Lane, R. D., Quinlan, D. M., Schwartz, G. E., Walker, P. A., & Zeitlin, S. B. (1990). The levels of emotional awareness scale: A cognitive-developmental measure of emotion. Journal of Personality Assessment, 55(1–2), 124–134. https://doi.org/10.1080/00223891.1990.9674052
- Li, E., Campbell, C., Midgley, N., & Luyten, P. (2023). Epistemic trust: A comprehensive review of empirical insights and implications for developmental psychopathology. Research in Psychotherapy: Psychopathology, Process and Outcome, 26(3). https://doi.org/10.4081/ripppo.2023.704
- Lohan, A., Morawska, A., & Mitchell, A. (2015). A systematic review of parenting interventions for parents of children with type 1 diabetes. Child: Care, Health and Development, 41(6), 803–817. https://doi.org/10.1111/cch.12278
- Luyten, P., Bateman, A., Gergely, G., Strathearn, L., Target, M., & Allison, D. E. (2010). Attachment and personality pathology. In J. F. Clarkin & P. Fonagy (Eds.), Psychodynamic psychotherapy for personality disorders: A clinical handbook (pp. 37–87). American Psychiatric Publishing, Inc.
- Luyten, P., Campbell, C., Allison, E., & Fonagy, P. (2020). The mentalizing approach to psychopathology: State of the art and future directions. Annual Review of Clinical Psychology, 16, 297–325. https://doi.org/10.1146/annurev-clinpsy-071919-015355
- Luyten, P., & Fonagy, P. (2016). An integrative, attachment-based approach to the management and treatment of patients with persistent somatic complaints. In J. Hunter & R. Maunder (Eds.), Improving patient treatment with attachment theory: A guide for primary care practitioners and specialists (pp. 127–144). Springer International Publishing.
- Luyten, P., & Fonagy, P. (2018). The stress-reward-mentalizing model of depression: An integrative developmental cascade approach to child and adolescent depressive disorder based on the research domain criteria (RDoC) approach. Clinical Psychology Review, 64, 87–98. https://doi.org/10.1016/j.cpr.2017.09.008
- Luyten, P., Van Houdenhove, B., Lemma, A., Target, M., & Fonagy, P. (2012). A mentalization-based approach to the understanding and treatment of functional somatic disorders. Psychoanalytic Psychotherapy, 26(2), 121–140. https://doi.org/10.1080/02668734.2012.678061
- Luyten, P., Van Houdenhove, B., Lemma, A., Target, M., & Fonagy, P. (2013). Vulnerability for functional somatic disorders: A contemporary psychodynamic approach. Journal of Psychotherapy Integration, 23(3), 250. https://doi.org/10.1037/a0032360
- Maaranen, P., Tanskanen, A., Haatainen, K., Koivumaa-Honkanen, H., Hintikka, J., & Viinamäki, H. (2004). Somatoform dissociation and adverse childhood experiences in the general population. Journal of Nervous and Mental Disease, 192(5), 337–342. https://doi.org/10.1097/01.nmd.0000126700.41047.83
- Malberg, N. T., & Mayes, L. C. (2013). The contemporary psychodynamic developmental perspective. Child and Adolescent Psychiatric Clinics of North America, 22(1), 33–49. https://doi.org/10.1016/j.chc.2012.08.002
- Maunder, R. G., & Hunter, J. J. (2008). Attachment relationships as determinants of physical health. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 36(1), 11–32. https://doi.org/10.1521/jaap.2008.36.1.11
- Maunder, R., & Hunter, J. (2015). Love, fear, and health: How our attachments to others shape health and health care. University of Toronto Press.
- McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87(3), 873–904. https://doi.org/10.1152/physrev.00041.2006
- McWilliams, L. A., & Bailey, S. J. (2010). Associations between adult attachment ratings and health conditions: Evidence from the national comorbidity survey replication. Health Psychology, 29(4), 446–453. https://doi.org/10.1037/a0020061
- Mikulincer, M., & Shaver, P. (2007). Attachment in adulthood: Structure, dynamics, and change. Guilford Press.
- Moran, G. S., & Fonagy, P. (1987). Psychoanalysis and diabetic control: A single-case study. British Journal of Medical Psychology, 60(4), 357–372. https://doi.org/10.1111/j.2044-8341.1987.tb02755.x
- Moran, G., Fonagy, P., Kurtz, A., Bolton, A., & Brook, C. (1991). A controlled study of the psychoanalytic treatment of brittle diabetes. Journal of the American Academy of Child and Adolescent Psychiatry, 30(6), 926–935. https://doi.org/10.1097/00004583-199111000-00010
- Moreira, H., & Canavarro, M. C. (2016). Parental attachment insecurity and parenting stress: The mediating role of parents’ perceived impact of children’s diabetes on the family. Families, Systems, & Health, 34(3), 240–249. https://doi.org/10.1037/fsh0000211
- Nakajima, R., Watanabe, F., & Kamei, M. (2021). Factors associated with medication non-adherence among patients with lifestyle-related non-communicable diseases. Pharmacy, 9(2), 90. https://doi.org/10.3390/pharmacy9020090
- Nieuwlaat, R., Wilczynski, N., Navarro, T., Hobson, N., Jeffery, R., Keepanasseril, A., Agoritsas, T., Mistry, N., Iorio, A., Jack, S., Sivaramalingam, B., Iserman, E., Mustafa, R. A., Jedraszewski, D., Cotoi, C., & Haynes, R. B. (2014). Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews, (11). (CD000011). https://doi.org/10.1002/14651858.CD000011.pub4
- Oates, G. R., Juarez, L. D., Hansen, B., Kiefe, C. I., & Shikany, J. M. (2020). Social risk factors for medication nonadherence: Findings from the CARDIA Study. American Journal of Health Behaviour, 44(2), 232–243. https://doi.org/10.5993/AJHB.44.2.10
- Oetzel, J., Wilcox, B., Avila, M., Hill, R., Archiopoli, A., & Ginossar, T. (2015). Patient-provider interaction, patient satisfaction, and health outcomes: Testing explanatory models for people living with HIV/AIDS. Aids Care-Psychological & Socio-Medical Aspects of Aids/hiv, 27(8), 972–978. https://doi.org/10.1080/09540121.2015.1015478
- Paterick, T. E., Patel, N., Tajik, A. J., & Chandrasekaran, K. (2017). Improving health outcomes through patient education and partnerships with patients. Proceedings (Baylor University Medical Center), 30(1), 112–113. https://doi.org/10.1080/08998280.2017.11929552
- Ravitz, P., Maunder, R., Hunter, J., Lokuge, B., & Lancee, W. (2010). Adult attachment measures: A 25-year review. Journal of Psychosomatic Research, 69, 419–432. https://doi.org/10.1016/j.jpsychores.2009.08.006
- Riedl, D., Rothmund, M. S., Grote, V., Fischer, M. J., Kampling, H., Kruse, J., Nolte, T., Labek, K., & Lampe, A. (2023). Mentalizing and epistemic trust as critical success factors in psychosomatic rehabilitation: Results of a single-center longitudinal observational study. Frontiers in Psychiatry, 14, 1150422. https://doi.org/10.3389/fpsyt.2023.1150422
- Sbarra, D. A., & Hazan, C. (2008, May). Coregulation, dysregulation, self-regulation: An integrative analysis and empirical agenda for understanding adult attachment, separation, loss, and recovery. Personality and Social Psychology Review, 12(2), 141–167. https://doi.org/10.1177/1088868308315702
- Schneider, I. K., Novin, S., & van Harreveld, F. (2022). The ambivalent individual: Validation studies for the trait ambivalence scale. OSF Preprints. https://doi.org/10.31219/osf.io/4cbex
- Schoenberg, P. L. A., Hepark, S., Kan, C. C., Barendregt, H. P., Buitelaar, J. K., & Speckens, A. E. M. (2014). Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clinical Neurophysiology, 125(7), 1407–1416. https://doi.org/10.1016/j.clinph.2013.11.031
- Substance Abuse and Mental Health Services Administration. (2015). Samhsa’s concept of trauma and guidance for a trauma-informed approach. https://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf
- Taylor, G. J., & Bagby, R. M. (2013). Alexithymia and the five-factor model of personality. In T. A. Widiger & Jr. P. T. Costa (Eds.), Personality Disorders and the Five Factor Model of Personality (3rd ed., pp. 193–207). Washington, DC: American Psychological Association.
- Taylor, R. E., Marshall, T., Mann, A., & Goldberg, D. P. (2012). Insecure attachment and frequent attendance in primary care: A longitudinal cohort study of medically unexplained symptom presentations in ten UK general practices. Psychological Medicine, 42(4), 855–864. https://doi.org/10.1017/S0033291711001589
- Thomakos, P., Griva, F., Kepaptsoglou, O., Mitrakou, A., Vaslamatzis, G., & Zoupas, C. (2019). Hypoglycemia unawareness is associated with attachment and reflective functioning in people with type 1 diabetes. Diabetes, 68(Supplement 1), 843–P. https://doi.org/10.2337/db19-843-P
- Tomasello, M., & Carpenter, M. (2007). Shared intentionality. Developmental Science, 10(1), 121–125. https://doi.org/10.1111/j.1467-7687.2007.00573.x
- van der Laan, D. M., Elders, P. J. M., Boons, C. C. L. M., Nijpels, G., & Hugtenburg, J. G. (2019). Factors associated with nonadherence to cardiovascular medications: A cross-sectional study. Journal of Cardiovascular Nursing, 34(4), 344–352. https://doi.org/10.1097/JCN.0000000000000582
- Vrijens, B., De Geest, S., Hughes, D. A., Przemyslaw, K., Demonceau, J., Ruppar, T., Dobbels, F., Fargher, E., Morrison, V., Lewek, P., Matyjaszczyk, M., Mshelia, C., Clyne, W., Aronson, J. K., Urquhart, J., & ABC Project Team. (2012). A new taxonomy for describing and defining adherence to medications. British Journal of Clinical Pharmacology, 73(5), 691–705. https://doi.org/10.1111/j.1365-2125.2012.04167.x
- Wang, H., Liao, Y., Guo, L., Zhang, H., Zhang, Y., Lai, W., Teopiz, K. M., Song, W., Zhu, D., Li, L., Lu, C., Fan, B., & McIntyre, R. S. (2022). Association between childhood trauma and medication adherence among patients with major depressive disorder: The moderating role of resilience. BMC Psychiatry, 22(1), 644. https://doi.org/10.1186/s12888-022-04297-0
- Weber, M. (1922). Economy and society: An outline of interpretive sociology (G. Roth & C. Wittich, Eds.). University of California Press.