ABSTRACT
Dissociative Identity Disorder (DID), an illness characterized by multiple personality states, has long been a controversial diagnosis within the psychiatric community. Demonstrating a neuroanatomical basis for the disorder may help to resolve the controversy. Current literature on the neuroanatomy associated with DID has focused on the hippocampus and amygdala and are inconclusive. This meta-analysis pools the results from n = 3 studies to compare the mean size of these two structures between DID patients, non-DID patients, and healthy controls. Patients diagnosed with both DID & PTSD were found to have smaller hippocampi bilaterally (p< .001) compared to healthy controls; no significant difference was seen in the amygdala. When comparing DID to PTSD patients, the left hippocampus was smaller (p< .001), with a trend for a smaller right hippocampus (p = .06). A comparison of the amygdala was not possible due to a lack of data. These findings suggest that a smaller hippocampus is seen in DID patients beyond what is seen for PTSD, provides neuroanatomical evidence for the memory impairment often seen in DID patients (i.e., amnesia experienced by the host and alters), and presents a potentially novel means to understand this disorder.
Introduction
Dissociative Identity Disorder (DID) is a psychiatric illness in which the hallmark is the existence of multiple personalities in one individual, as well as episodes of dissociation characterized by the separation of normal mental processes from other mental processes and perception of the environment (American Psychiatric Association, Citation2013). Other symptoms of the disorder include memory impairment, amnesia, and abnormal responses to and processing of fear (American Psychiatric Association, Citation2013; Reinders et al., Citation2018; Şar et al., Citation2017b; Vissia et al., Citation2016). The disorder affects around 1% of the general population (Şar et al., Citation2017b). Despite ongoing debates regarding neuroanatomical changes seen with the disorder, a few consistent theories have developed: (1) the hippocampus has been implicated due to memory impairments seen in patients (Blihar et al., Citation2020; Chalavi et al., Citation2015b; Şar et al., Citation2017b; Vermetten et al., Citation2006); and (2) the amygdala is most likely involved in the development and manifestation of the disorder due to a history of childhood trauma seen in many DID patients (Blihar et al., Citation2020; Dalenberg et al., Citation2012; Reinders et al., Citation2018; Vermetten et al., Citation2006).
Recent studies on structural abnormalities have repeatedly found decreases in the right and left hippocampi of DID patients compared to healthy controls (Chalavi et al., Citation2015a, Citation2015b; Reinders et al., Citation2019; Vermetten et al., Citation2006; Weniger et al., Citation2008). Structural changes observed in the amygdala have been less consistent. A number of researchers in the field have found a decrease in amygdala size (Reinders et al., Citation2019; Vermetten et al., Citation2006) but other researchers have failed to observe a similar finding (Chalavi et al., Citation2015a; Weniger et al., Citation2008).
Given the disagreement in the literature, a meta-analysis to determine the pooled effect size is appropriate. Comparing reported volumes of the hippocampus and amygdala in patients with DID, patients diagnosed with both post-traumatic stress disorder (PTSD) and DID, and healthy controls would provide more quantitative data on potential differences in brain regions while controlling for PTSD as a potential confounding variable. We hypothesized that patients diagnosed with DID would have smaller hippocampi and amygdala, bilaterally, compared to healthy controls and patients diagnosed with PTSD (but without comorbid DID).
Methods
Article Search and Selection
This manuscript conforms to PRISMA reporting guidelines for systematic reviews and meta-analyses (Shamseer et al., Citation2015) and adopts a similar search procedure to Pham and colleagues (Pham et al., Citation2014). The protocol from Blihar et al. (Citation2020), registered with PROSPERO (NIH, n.d.) under Registration Number: CRD42019125573, was modified to include additional inclusion criteria: (1) articles had to report hippocampal or amygdala volumes; and (2) articles reporting non-univariant voxel pattern data were excluded due to inability to pool that data with other reported article volume data. The initial data search was conducted during March 2020 across six electronic databases (PubMed, Psychiatry Online, MedLinePlus, ScienceDirect, Cochrane Database of Systematic Reviews, and PsycINFO) using the Boolean search (Blihar et al., Citation2020):
(“Dissociative Identity Disorder” OR “Multiple Personality Disorder”) AND MRI.
Search results were not restricted by any filters or timeline. Predefined keywords, such as “Dissociative Personality Disorder,” “Multiple Personality Disorder,” and/or “MRI,” were used to screen articles based on abstracts. Abstracts not including those predefined words were excluded unless the methodology section included brain measurements of DID participants. Articles with reported results pertaining to PTSD participants along with DID participants were also included. The risk of bias in individual studies was controlled using the scoring system described by the US Department of Health and Human Services (USDHSS) (West et al., Citation2002). Articles with a quality rating of greater than or equal to 4 were accepted for data extraction. Article screening, article selection, article exclusion, and data extraction were conducted in duplicate by two independent authors. Disagreements were settled by a decision from a third independent author. summarizes the studies included in this analysis; shows the generated PRISMA flow chart outlining the inclusion and exclusion process.
Table 1. Summary of included studies
Statistical Analysis
Using a random-effects model and the DerSimonian–Laird method (DerSimonian & Laird, Citation1986), a meta-analysis was conducted on the mean difference between the hippocampus and amygdala between two groupings of patients (PTSD/DID vs. healthy controls [HC]; PTSD/DID v DID). The mean difference was used because the study authors reported the mean and standard deviation for the brain volumes (measured in cm3). Heterogeneity of studies was estimated using the I-squared (I2) statistic; an estimate greater than or equal to 75% was taken as evidence of high heterogeneity (Higgins et al., Citation2003), where the pooled analysis was deemed inappropriate. Publication bias was assessed using the funnel plot method (Soeken & Sripusanapan, Citation2003). The analysis was conducted using STATA (version 16).
Results
Three studies (see ) were selected for data extraction because all three papers reported hippocampus and amygdala structural characteristics in units of volume. These studies represented 165 participants (PTSD n = 32; DID n = 32, DID/PTSD n = 17, healthy controls n = 92; see ). All three studies were included in the DID/PTSD vs. HC hippocampus analysis; two of the three (Chalavi et al., Citation2015a; Vermetten et al., Citation2006) were included in the amygdala analysis. The (Vermetten et al., Citation2006) study was not included in the amygdala analysis because they did not report amygdala volume findings. Analysis comparing PTSD and DID for the amygdala could not be conducted as only one study (Weniger et al., Citation2008) reported findings for these populations.
Hippocampal and amygdala volumes in study participants were reported as compared against total brain volumes with “total brain” defined by each study (see whole brain). Reinders et al. (Citation2019,Citation2018) were not selected for extraction because neuroanatomical characteristics were reported in non-univariant voxel patterns. Weniger et al. (Citation2008) were not selected for extraction because all of the participants with dissociative amnesia, DID, and PTSD also had a diagnosis of bipolar personality disorder (BPD) and the healthy controls did not introduce a potential confounding variable (BPD) into the analysis.
Whole Brain
Chalavi et al. (Citation2015a) defined the whole brain as all brain parenchyma and found that DID patients had a significantly smaller cortical volume of total gray matter (TG) (p = .003), left hemisphere gray matter (LG) (p = .001), and right hemisphere gray matter (RG) (p = .009) than healthy controls. Neither Chalavi et al. (Citation2015b) nor Vermetten et al. (Citation2006) found significant differences in the total brain cortical volumes between DID patients and controls. Chalavi et al. (Citation2015a) found that LG cortical thickness was smaller in DID patients.
Hippocampus
Vermetten et al. (Citation2006) found that hippocampal volumes in DID participants were smaller bilaterally compared to healthy controls (HC). They also found that participants who recovered from DID had significantly larger hippocampi than DID participants not having recovered from their disorder or completed therapy (Vermetten et al., Citation2006). Chalavi et al. (Citation2015b) found that DID-PTSD patients had significantly smaller hippocampal volumes bilaterally compared to PTSD-only patients. They also noted that PTSD-only patients had a smaller right-sided hippocampus compared to the left, but they did not observe this pattern in DID-PTSD patients (Chalavi et al., Citation2015b). The authors observed significantly smaller cornu ammonis (CA) 1, CA2-3, and CA4-dentate gyrus in DID-PTSD patients (Chalavi et al., Citation2015b). The subiculum and left presubiculum were also noted to be significantly smaller in DID-PTSD patients compared to HC (Chalavi et al., Citation2015b). Similarly, the CA4- dentate gyrus and subiculum of DID patients were observed to be significantly smaller than PTSD-only patients (Chalavi et al., Citation2015b). Chalavi et al. (Citation2015a) noted that the sizes of the CA1, CA2-3, CA4-dentate gyrus, subiculum, and presubiculum correlated significantly with the severity of trauma experienced by the study patients.
Amygdala
Vermetten et al. (Citation2006) found the DID participants had significantly smaller amygdala volumes bilaterally compared to HC. Chalavi et al. (Citation2015a) observed that the amygdala was preserved in DID patients compared to HC.
Synthesis of results
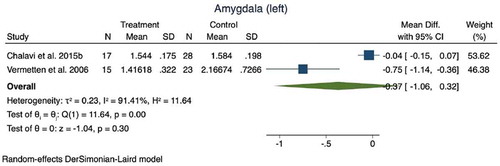
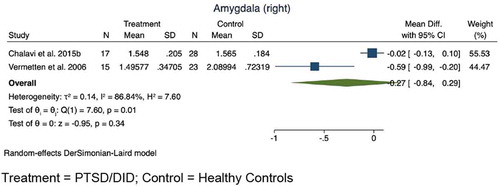
PTSD/DID versus HC: The meta-analysis demonstrated statistically significant differences between patients diagnosed with PTSD and DID compared to healthy controls for both the right hippocampus (mean difference: 0.29, 95% CI: 0.19–0.39, z = −5.70, p < .001; see ) and the left hippocampus (mean difference: 0.25, 95% CI: 0.15–0.36, z = −4.76, p < .001; see ). No statistically significant difference was seen in either the right amygdala (mean difference = 0.27, 95% CI: 0.84 to −0.29, z = −0.95, p = .34) or left amygdala (mean difference: 0.37, 95 CI: 1.06 to −0.32, z = −1.04, p = .30). In both cases, high degrees of heterogeneity limit the conclusions that can be drawn from the small sampling of studies (see and ).
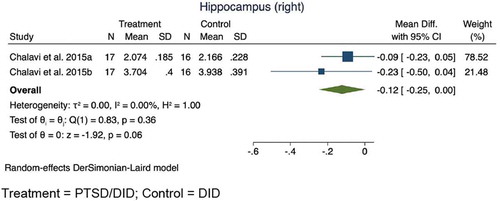
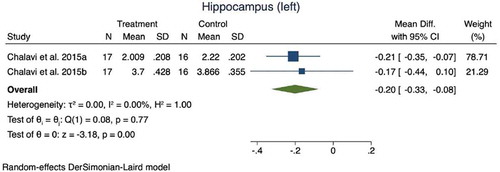
PTSD/DID versus DID: Comparison of patients diagnosed with both PTSD and DID to those diagnosed with only DID showed significant differences in the left hippocampus (mean difference: 0.20, 95% CI: 0.08 to 0.33, z = −3.18, p < .001; see ); however, no significant differences were seen in the right hippocampus, although a trend was observed (mean difference: 0.12, 95% CI: 0 to 0.25, z = −1.92, p = .06; see ). As indicated in the methods section, analysis of the amygdala was not possible due to only one study reporting data on the amygdala (Chalavi et al., Citation2015a).
Figure 2 Meta-analysis results for the hippocampus(Right)
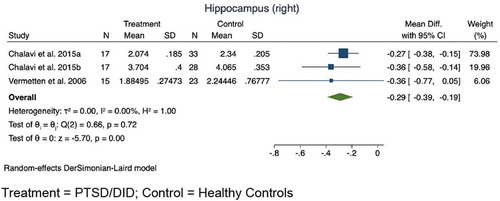
Figure 3 Meta-analysis results for the hippocampus (left)
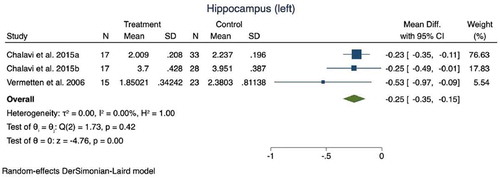
Figure 4 Meta-analysis results for the amygdala (right)
Discussion
The current meta-analysis demonstrated that patients diagnosed with PTSD & DID had significantly smaller bilateral hippocampi compared to healthy controls. Further, patients diagnosed with DID alone had a significantly smaller left hippocampus than patients diagnosed with PTSD & DID, a difference that also emerged at a trend level for the right hippocampus. These findings suggest that a smaller hippocampus is not unique to PTSD, and are consistent with studies that have reported smaller hippocampi in DID patients (Ehling et al., Citation2007; Irle et al., Citation2007; Reinders et al., Citation2018, Citation2019; Weniger et al., Citation2008). The hippocampus is critical for memory consolidation and reconstruction. These findings provide neuroanatomical evidence for the memory impairment often seen in DID patients (American Psychiatric Association, Citation2013; Reinders et al., Citation2012) and extend beyond what is reported for PTSD patients (American Psychiatric Association, Citation2013; Vermetten et al., Citation2006; Weniger et al., Citation2008). Specifically, these findings may underlie the amnesia experienced by the host and alters specifically seen in patients with DID (Brand et al., Citation2016; Chalavi et al., Citation2015b; Reinders et al., Citation2012). Indeed, amnesia for events as DID patients alternate between host and alters is the key differential between DID and PTSD (American Psychiatric Association, Citation2013; Gleaves et al., Citation2001; McSweeney et al., Citation2016; Şar et al., Citation2017a). Despite these theories, the implications of the smaller hippocampi observed in DID patients remain unclear, requiring further investigation. The causal mechanisms, whether smaller hippocampi lead to impairment in memory, whether impairment in memory leads to smaller hippocampi, or whether some other factor mediates the relationship between these two, remain unknown and require further study.
We found no evidence for a significant difference in amygdala volume between PTSD & DID patients and normal controls and could not directly compare DID patients to PTSD patients due to a lack of data. The results of the comparison to normal controls are consistent with Weniger et al. (Citation2008) and Irle et al. (Citation2009). Unlike the hippocampus, there is more disagreement regarding the relationship between DID and the amygdala. Multiple studies have reported a smaller amygdala in patients with DID compared to healthy controls (Ehling et al., Citation2007; Reinders et al., Citation2018, Citation2019; Vermetten et al., Citation2006). Chalavi et al. (Citation2015b), Chalavi et al. (Citation2015a), and Weniger et al. (Citation2008) reported no difference in the size of the amygdala between DID patients and healthy controls. Inconsistent reporting and small sample sizes potentially explain these divergent findings, and more research is needed to determine the relationship between DID and the amygdala.
This is the first meta-analysis of the neuroanatomy of DID. While the field of inquiry is still in its infancy and controversy regarding the neuroanatomical basis of DID continues, the current findings add to the evidence base for a neuroanatomical basis of the disorder. Blihar et al. (Citation2020) reviewed the literature and reported a number of brain regions associated with DID. These included an increase in white matter tracts in the motor regions in the brainstem and right hemisphere, larger precuneus, smaller occipital cortex, smaller insula, smaller orbitofrontal cortex, smaller cingulate cortex, smaller inferior parietal cortex, smaller angular gyrus and supramarginal gyrus, smaller hippocampus/parahippocampal/fusiform gyrus, and smaller amygdala. The current meta-analysis has added to this review by incorporating quantitative comparisons of brain regions between DID and PTSD patients and healthy controls. While the data remain sparse, the findings point to the hippocampus and amygdala as potentially key brain regions underlying DID. Blihar et al. (Citation2020) referenced the existing literature in pointing out the loss of amygdala volume and changes in the left amygdala-hippocampal junction and its association with depersonalization as an important finding for the neuroanatomical basis of DID. Lack of data precluded a direct comparison of amygdala size between DID and PTSD patients in the current meta-analysis, but given the existing evidence in the literature, we believe this is a critical comparison that could provide a significant understanding of the neuroanatomical basis of DID. Future imaging studies should be certain to examine this brain region while carefully dividing PTSD and DID patients.
Limitations
While this meta-analysis used a rigorous search methodology, there are limitations to the conclusions that can be drawn. The small sample of studies for many of the outcomes of interest and the high number of papers from a single author limit conclusive understanding of how the brain differs in people diagnosed with DID. Several other papers have examined this question and would have ideally been included in the analysis, but variation in methodologies precluded this. While several authors reported neuroanatomic differences based on total brain volume, differences in methods of measurement necessitated the exclusion of those articles from this meta-analysis. Finally, several authors reported differences; however, those studies were excluded due to inadequate transparency in reporting to fully extrapolate data for this meta-analysis. It would be helpful if researchers in the field could coordinate to set a standardized methodology for any future studies, that would enable the inclusion of all findings in future meta-analyses. Specifically, future attempts at meta-analysis would be improved by consistent volume reporting across research, including units of volume or a conversion from voxels to a standard volume measurement, and homogenous definitions of total brain.
Conclusions
The results of this meta-analysis partially support our hypothesis: patients diagnosed with DID demonstrated smaller hippocampi, bilaterally, compared to healthy controls and patients diagnosed with PTSD (but without comorbid DID). This study continues to add to the literature base regarding the neuroanatomical basis of DID and provides further quantitative evidence that the brains of DID patients differ from at least one other group of individuals diagnosed with a mental illness (PTSD) as well as healthy controls. This meta-analysis supports the potential for imaging biomarkers in DID patients. Further research is needed to examine causal mechanisms, that is, whether DID leads to smaller hippocampi, whether smaller hippocampi results in DID symptoms, or some other mediating factor drives the relationship between the two.
Abbreviations
BPD (bipolar personality disorder), DID (dissociative identity disorder), LG (left hemisphere gray matter), PTSD (post-traumatic stress disorder), TE (total gray and white matter of entire structure), USDHSS (US Department of Health and Human Services)
Conflict of Interests: Mr. Crisafio has received third-party payment for statistical work funded by Juul Labs; the other authors report no conflicts of interest.
Funding Source: This protocol and systematic review are not sponsored by any external organizations.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed ed.).
- Blihar, D., Delgado, E., Buryak, M., Gonzalez, M., & Waechter, R. (2020). A systematic review of the neuroanatomy of dissociative identity disorder. Eur. J. Trauma Dissociation, 4(3), 100148. https://doi.org/10.1016/j.ejtd.2020.100148
- Brand, B. L., Vissia, E. M., Chalavi, S., Nijenhuis, E. R. S., Webermann, A. R., Draijer, N., & Reinders, A. A. T. S. (2016). DID is trauma based: Further evidence supporting the trauma model of DID. Acta psychiatrica Scandinavica, 134(6), 560–563. https://doi.org/10.1111/acps.12653
- Chalavi, S., Vissia, E. M., Giesen, M. E., Nijenhuis, E. R. S., Draijer, N., Barker, G. J., Veltman, D. J., & Reinders, A. A. T. S. (2015a). Similar cortical but not subcortical gray matter abnormalities in women with posttraumatic stress disorder with versus without dissociative identity disorder. Psychiatry Res. - Neuroimaging, 231(3), 308–319. https://doi.org/10.1016/j.pscychresns.2015.01.014
- Chalavi, S., Vissia, E. M., Giesen, M. E., Nijenhuis, E. R. S., Draijer, N., Cole, J. H., Dazzan, P., Pariante, C. M., Madsen, S. K., Rajagopalan, P., Thompson, P. M., Toga, A. W., Veltman, D. J., & Reinders, A. A. T. S. (2015b). Abnormal hippocampal morphology in dissociative identity disorder and post-traumatic stress disorder correlates with childhood trauma and dissociative symptoms. Hum. Brain Mapp., 36(5), 1692–1704. https://doi.org/10.1002/hbm.22730
- Dalenberg, C. J., Brand, B. L., Gleaves, D. H., Dorahy, M. J., Loewenstein, R. J., Cardeña, E., Frewen, P. A., Carlson, E. B., & Spiegel, D. (2012). Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychol. Bull., 138(3), 550–588. https://doi.org/10.1037/a0027447
- DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Control. Clin. Trials, 7(3), 177–188. https://doi.org/10.1016/0197-2456(86)90046-2
- Ehling, T., Nijenhuis, E. R. S., & Krikke, A. P. (2007). Volume of discrete brain structures in complex dissociative disorders: Preliminary findings. Progress in Brain Research, 167, 307–310. https://doi.org/10.1016/S0079-6123(07)67029-0
- Gleaves, D. H., May, M. C., & Cardeña, E. (2001). An examination of the diagnostic validity of dissociative identity disorder. Clin. Psychol. Rev., 21(4), 577–608. https://doi.org/10.1016/S0272-7358(99)00073-2
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. https://doi.org/10.1136/bmj.327.7414.557
- Irle, E., Lange, C., Sachsse, U., & Weniger, G. (2009). Further evidence that post-traumatic stress disorder but not dissociative disorders are related to amygdala and hippocampal size reduction in trauma-exposed individuals. Acta psychiatrica Scandinavica, 119(4), 330–331. https://doi.org/10.1111/j.1600-0447.2009.01351.x
- Irle, E., Lange, C., Weniger, G., & Sachsse, U. (2007). Size abnormalities of the superior parietal cortices are related to dissociation in borderline personality disorder. Psychiatry Res. - Neuroimaging, 156(2), 139–149. https://doi.org/10.1016/j.pscychresns.2007.01.007
- McSweeney, L. B., Koch, E. I., Saules, K. K., & Jefferson, S. (2016). Exploratory factor analysis of diagnostic and statistical manual, 5th Edition, Criteria for posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 204(1), 9–14. https://doi.org/10.1097/NMD.0000000000000390
- NIH (n.d.). PROSPERO [WWW Document]. NIH. URL https://www.crd.york.ac.uk/PROSPERO/
- Pham, M. T., Rajić, A., Greig, J. D., Sargeant, J. M., Papadopoulos, A., & Mcewen, S. A. (2014). A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods, 5(4), 371–385. https://doi.org/10.1002/jrsm.1123
- Reinders, A. A. T. S., Chalavi, S., Schlumpf, Y. R., Vissia, E. M., Nijenhuis, E. R. S., Jäncke, L., Veltman, D. J., & Ecker, C. (2018). Neurodevelopmental origins of abnormal cortical morphology in dissociative identity disorder. Acta psychiatrica Scandinavica, 137(2), 157–170. https://doi.org/10.1111/acps.12839
- Reinders, A. A. T. S., Marquand, A. F., Schlumpf, Y. R., Chalavi, S., Vissia, E. M., Nijenhuis, E. R. S., Dazzan, P., Jäncke, L., & Veltman, D. J. (2019). Aiding the diagnosis of dissociative identity disorder: Pattern recognition study of brain biomarkers. Br. J. Psychiatry, 215(3), 536–544. https://doi.org/10.1192/bjp.2018.255
- Reinders, A. A. T. S., Willemsen, A. T. M., Vos, H. P. J., & Boer, J. A. D. (2012). Fact or factitious? A psychobiological study of authentic and simulated dissociative identity states. PLoS One, 7(6), e39279. https://doi.org/10.1371/journal.pone.0039279
- Şar, V., Alioğlu, F., Akyuz, G., Tayakısı, E., Öğülmüş, E. F., & Sönmez, D. (2017a). Awareness of identity alteration and diagnostic preference between borderline personality disorder and dissociative disorders. J. Trauma Dissociation, 18(5), 693–709. https://doi.org/10.1080/15299732.2016.1267684
- Şar, V., Dorahy, M., & Krüger, C. (2017b). Revisiting the etiological aspects of dissociative identity disorder: A biopsychosocial perspective. Dovepress.
- Shamseer, L., Moher, D., Clarke, M., Gherso, D., Liberati, A., Petticrew, M., & Shekelle, P. (2015). PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 checklist: Recommended items to address in a systematic review protocol. BMJ, (jan02 1), 349, g7647. https://doi.org/10.1136/bmj.g7647
- Soeken, K. L., & Sripusanapan, A. (2003). Assessing publication bias in meta-analysis. Nurs. Res., 52(1), 57–60. https://doi.org/10.1097/00006199-200301000-00009
- Vermetten, E., Schmahl, C., Lindner, S., & Loewenstein, R. J. (2006). Hippocampal and amygdalar volumes in dissociative identity disorder. The American Journal of Psychiatry, 163(4), 630–636. https://doi.org/10.1176/appi.ajp.163.4.630.Hippocampal
- Vissia, E. M., Giesen, M. E., Chalavi, S., Nijenhuis, E. R. S., Draijer, N., Brand, B. L., & Reinders, A. A. T. S. (2016). Is it trauma- or fantasy-based? Comparing dissociative identity disorder, post-traumatic stress disorder, simulators, and controls. Acta psychiatrica Scandinavica, 134(2), 111–128. https://doi.org/10.1111/acps.12590
- Weniger, G., Lange, C., Sachsse, U., & Irle, E. (2008). Amygdala and hippocampal volumes and cognition in adult survivors of childhood abuse with dissociative disorders. Acta psychiatrica Scandinavica, 118(4), 281–290. https://doi.org/10.1111/j.1600-0447.2008.01246.x
- West, S., King, V., Carey, T., Lohr, K., McKoy, N., Sutton, S., & Lux, L. (2002). Systems to rate the strength of scientific evidence. Rockville, MD: Agency for Healthcare Research and Quality (US); 2002 Apr. (Evidence Reports/Technology Assessments, No. 47). Available from: https://www.ncbi.nlm.nih.gov/books/NBK33881/.