ABSTRACT
This study assessed subjective symptoms associated with exposure to static magnetic fields (SMFs) and radiofrequency (RF) energy, and perceived safety risk of scanners among magnetic resonance (MR) staff working in the 1.5 and 3 T MRI units. A questionnaire survey was completed by 77 clinical imaging staff working in two hospitals (A and B) in the Mangaung metropolitan region. 50 participants working with the MR scanners were regarded as exposed group and 27 participants from CT scan and X-ray departments were classified as control group. The study comprised 57% females and 43% male participants with an average MRI experience of 5.4 years. Using logistic regression, tinnitus was significantly different between various job titles (p< .034) and it was reported more often (OR 8:00; CI 1.51, 15.17) by those who worked on a 3 T scanner. Increased years of MRI experience was a significant predictor of headache (p< .05), and reporting of nausea was significantly different between various job titles (p < .01). There was an increased risks of reporting vertigo often among female participants (OR: 4.43; CI 0.91, 21.47), those with 5–15 years of MRI experience (OR: 2.09; CI 0.47, 9.34), and those with a light to moderate workload (OR: 2.70; CI 0.49, 14.86). Using linear regression, presence in zone IV during image acquisitioning was the only significant predictor for the sensation of glowing (p < .000). Movement of head/ upper body in the scanner bore was a significant predictor of nausea (p< .026), vertigo (p< .014), instability when standing (p< .014), and a metallic taste (p< .031). There was no correlation between reporting of symptoms and perceived risk of scanners. However, shift duration (rs = 0.576), movement of head/upper body in the scanner bore (rs = 0.424), and strength of the scanners (rs = 0.299) were significantly correlated with perceived risk of scanners. MRI safety training and a comprehensive occupational health and safety program are necessary.
Introduction
Every year, an estimate of about 60 million magnetic resonance imaging (MRI) scans are performed worldwide in both private and public healthcare facilities (Hartwig et al. Citation2018). In South Africa, there is a significantly high number of MRI units in private healthcare sectors compared to public hospitals (Van Schouwenburg et al. Citation2014). In the MR scanner room (zone IV), MR staff are exposed to a mixture of MRI-related electromagnetic fields (EMFs) (Frankel et al. Citation2018); static magnetic field (SMF; 0 Hz) that is constantly present in zone IV, radiofrequency (RF) pulses (MHz frequency) used for signal generation, and switched gradient fields (SGF) (kHz frequency) applied for spatial encoding (Capstick et al., Citation2008; International Electrotechnical Commission (IEC) Citation2010). Staff entering zone IV may experience instantaneous SMFs exposure, including exposure to SGFs when standing in close proximity to the scanner bore during image acquisition (Bradley et al. Citation2007; Schaap et al. Citation2013). Occupational exposure to RF fields is uncommon but might occur when an MR worker is scanned voluntarily when testing a new imaging protocol or bending into the scanner bore when assisting a patient (Schaap et al. Citation2013). Other occupations that could be exposed to SMFs and RF energy include maintenance engineers and medical physicists when performing acceptance or quality control tests. There is a limited use of MR scanners worldwide compared to other radiological modalities, and no severe or long lasting health effects relating to occupational exposure to MRI-related EMFs have far been reported (Capstick et al., Citation2008; International Electrotechnical Commission (IEC) Citation2010). However, several studies report on either transient or subjective symptoms among staff working with MR scanners (Heinrich et al. Citation2013; Schaap et al. Citation2014; van Nierop et al. Citation2012; Wilén and De Vocht Citation2011).
In South Africa, the MR radiological services are relatively expensive in private hospitals, and only a limited number of public hospitals perform clinical MR imaging on a 1.5 and seldomly on a 3 T. As a developing country, there is an existing potential to adopt the use of MR scanners for all clinical imaging needs, however, a wide knowledge gap regarding exposure to MRI-related EMFs and reporting of transient or subjective symptoms in the South African healthcare occupations exist. Studies on MRI-related EMFs exposures and reporting of symptoms from the population of MR workers have mostly been conducted in European countries (Bradley et al. Citation2007; Schaap et al. Citation2013), with African exposure scenarios been relatively none existence. In this study, subjective symptoms and risk perception among MR staff working with 1.5 and 3 T scanners in the two public hospitals in South Africa were investigated.
Methodology
Description of the study setting
This study was conducted in the central region (Free State) of South Africa, Mangaung Metropolitan, where there are only two 1.5 tesla (T) scanners and one 3 T MR scanners serving approximately 2.8 million people (Kabongo et al. Citation2015) in the public hospitals. The MRI examinations in the Mangaung public healthcare facilities are mainly performed in two academic hospitals (referred to as hospitals A and B). Hospital A has two MR scanners: 1.5 and 3 T (Theron et al. Citation2015) and hospital B has only one 1.5 T scanner. These hospitals are regarded as referral facilities, in the Free State, for all patients who need radiological services, including MRI scans. In both hospitals, there are very few MR staff assigned to work in the MRI units, hence this study was conducted with a small sample size. Occupations performing work in either zone III (console room) or IV of the units are radiographers, medical physicists, nurses, cleaners, and students undertaking their academic practical in the field of medical physics, radiography, and nursing. The maintenance of MR scanners is primarily undertaken by outsourced maintenance engineers, who assume the responsibility of clinical engineers and are responsible to maintain the MR scanners according to manufacturers’ requirements.
Study design
A descriptive, cross-sectional survey was used to investigate the subjective symptoms associated with exposure to SMFs and RF energy, and safety perception reported by the MR staff during their work shifts in the MRI units. Before the commencement of the study, ethical clearance was obtained from University of the Free State (UFS-HSD2018/0438/3107) and permission to conduct the study was obtained from the Free State department of health (FS201805 020).
Data collection
Questionnaire development
Self-administered questionnaires were used to collect data about working in the MRI units and reporting of symptoms associated with SMFs and RF energy exposures. Questionnaires were administered once consent was obtained from all the participants. Since the questionnaire reflects on the past exposure of entire workweek, participants were asked to complete their questionnaires on Friday afternoon at the end of their shift. The questionnaire included items that were used in previous studies (De Vocht et al. Citation2015; Fatahi et al. Citation2016; Schaap et al. Citation2016). These studies used baseline questionnaires to obtain data on the subjective symptoms of exposure to SMFs. Subjective reference symptoms from the Lund Subjective Health Complaint Inventory (SHC) questionnaire (Eriksen et al. Citation1999) were also included to com-pare commonly reported symptoms between MR staff and the control group. According to De Vocht et al. (De Vocht et al. Citation2015), the SHC questionnaire is a validated instrument used to obtain information about the commonly reported subjective health symptoms within the general population. The questionnaire consisted of three sections collecting biographical, work, and health-related information. The biographical information of the participants gathered included their age, gender, and level of education. The work-related items gathered information about their working shifts, workloads, work activities proximal to MR scanners, health and safety training, job titles, and control measures to minimize exposure. The third section comprised questions that gathered data on the symptoms (without measuring personal exposure). Symptoms related to RF energy exposure included sensation of burning or irritated skin, and feeling warm and hot flushes. The symptoms related to SMFs exposure were vertigo, nausea, seeing light flashes, feeling of instability, metallic taste. To control for potential over-reporting of symptoms, similarly as reported by Fatahi et al. (Fatahi et al. Citation2016), other symptoms such as itchy or watery eyes, headache, and blurred or double vision were used. All symptoms were rated on a five-point Likert scale, ranging from “never” to “always” as a frequency of occurrence.
Participants’ enrolment and sampling
The study population consisted of workers who were employed full time and were assigned to work in the clinical imaging departments. The exposed group were participants who worked shifts in the MRI units, zone IV and the control population were radiographers who worked in the CT scan and X-ray departments. The control population has never worked on MR scanners or visited the MRI units during their work shifts.
Purposive sampling was used to enrol all the study participants. MR staff included maintenance engineers (two) from Philips (3 T) and Siemens (1.5 T) companies, two cleaning personnel members who rotated shifts in hospital A, MRI unit, and four radiographers who were assigned to work in the MRI units of both hospitals. An additional nine radiographers (one from hospital A and eight from hospital B), who were identified to have received in-house MRI safety training and frequently worked in the MRI room (where the scanner is located), also were enrolled for the study. Two medical physicists, both stationed in their respective hospitals, and four radiologists who were available at the time of data collection, were approached for participation. Of the latter group, only three reported rotating between the two hospitals.
A specially designed MRI suite entrance register was used to enrol those participants who entered zone IV, and they were given a questionnaire to complete. From the register, thirteen nurses and three medical doctors, who brought patients for MRI scanning were identified in the two hospitals, provided with consent forms, and requested to complete the questionnaires. Two cleaners who assisted (occasionally) in cleaning the MRI suite, eight porters who, sometimes, brought or fetched patients from the MRI units (zones III or IV) in both hospitals also were included.
Classification of symptoms and exposed group
Since the study population included also small number of participants who frequent the scanner room; doctors, cleaners and porters, these participants were classified as “others.” Initially, a total of 49 exposed and 28 unexposed individuals were identified. However, there was one radiographer from CT scan department who reported to have visited the scanner room during his work shift. For this reason, the radiographer was assigned to an exposed group, resulting to a total of 50 exposed and 27 control participants.
This study was based on subjective symptoms and perceived risks of scanners re-ported by participants, without measuring their personal exposure to time-varying magnetic fields. Previously, spot monitoring for SMFs and RF magnetic fields was performed in zone IV of the MRI units where participants included in this study are employed (Rathebe et al. Citation2021). Based on certain activities participants reported to perform in zone IV, during their workweek, the likelihood of reporting symptoms was categorized as follow:
a) Number of times participants were present in zone IV, proximal to the operating scanner, during image acquisitioning.
b) Number of times participants moved their head/ upper body in the scanner bore, either while the scanner was operating or not operating.
c) Longer stay in zone IV due to irregularities or emergencies.
Several studies have associated exposure to RF energy with the development of thermal effects (Foster et al. Citation2018; Neufeld et al. Citation2015; Shrivastava Citation2007; van Den Brink Citation2019). However, symptoms such as “sensation of glowing and suddenly feeling warm or hot,” which are arguably thermal related, were classified as priori unrelated symptoms in a study that assessed the reporting of symptoms among MR staff (Schaap et al. Citation2014). Based on our previous study that reported the presence of RF magnetic fields, 1 m from the scanner gantry (Rathebe et al. Citation2021), sensation of glowing and suddenly feeling warm or hot were classified as RF exposure-related symptoms. The exposed group was categorized based on the RF and SMFs expose likelihood:
1) Nurses, medical physicists and maintenance engineers = SMFs and RF magnetic fields in zone IV. These are individuals who enters zone IV either during image acquisitioning to assist patient or during quality control tests.
2) Radiographers, radiologists, cleaners, and porters = SMFs in zone IV.
3) Medical doctors = SMFs in zone IV, and occasionally RF magnetic fields when assisting patients.
The control group reported to have no history of work in the MRI units.
Data analysis
Data were captured electronically by the researcher in Microsoft Excel (2016) to check for duplicates and double entries prior analysis. IBM SPSS version 26 was used to analyze the data. Descriptive analysis was performed for obtaining the descriptive data. A chi square test of independence was performed to identify the differences in the descriptive data. A reliability analysis with Cronbach alpha of 0.05 also was per-formed to determine the reliability of the Likert scale for reported symptoms, and all symptoms with zero variance were excluded from further analysis. Logistic regression was performed to evaluate which variables are predictors of reporting symptoms. Odds ratios and 95% confidence intervals were calculated at a significance level of ≤ .05.
Since there was a small number of participants reported to have moved their head/ upper body in the scanner bore, presence in zone IV during image acquisitioning, and longer stay in zone IV due to irregularities, logistic regression could not be performed, instead, a linear regression was performed to determine if these activities could predict the reporting of symptoms. Furthermore, to determine which variables predicted the perception of unsafeness when staff are working with MR scanners, the bivariate spearman correlation was used. The responses on all the symptoms were re-coded and categorized as often and seldom/ never (0/1) and rating of scanners’ safety was categorized into safe and unsafe (0/1) before the statistical relationships could be determined.
Results
Characteristics of study population and work in the MRI units
The study population comprised 44 females (57%) and 33 males (43%). Initially, 12 radiologists were identified and only four agreed to participate, resulting in 91% response rate (77/85). The age of the participants ranged from 21 to 61 years, with one female participant who did not indicate her age. The reporting of tiring workweek (60%) and heavy workload (24%) was more among the exposed participants (). One radiographer (from CT scan, assigned to exposed group) reported to have never being in the scanner room during irregularities/emergencies, image acquisitioning or moved head/upper body in the scanner bore. Majority of participants (66%) indicated not to work shifts in the MRI units, however, those who indicated to work shifts, majority of them (29%) worked 8-hour shift.
Table 1. Characteristics of study participants
The comparison of individual characteristics between exposed and control group were significantly different, except for age (p< .21). In the exposed group, chi square test of independence suggested significant difference in the scanner worked on, presence in the scanner room during image acquisitioning, movement of head/ upper body in the scanner bore, longer stay in the scanner room due to irregularities and presence in the scanner room during work shifts. Comparison on the number of years in the MRI units was statistically non-significantly (p< .44).
Symptoms and predictor variables
All symptoms were recorded on a five-point Likert scale () and 18% (14/77) of the study participants (control group) did not provide responses. Furthermore, the responses were recoded into often and seldom/ never, and those with sufficient responses were used for modelling a relationship in the logistic regression. The use of Likert scale for reporting of symptoms was suggested reliable (α = 0.86) after performing the reliability test. Symptoms such as earaches, vomiting, palpitation, tingling, itching, seeing black spots, seeing light flashes and blurred vision which were initially included to control for over-reporting, were removed based on zero variance.
Table 2. Overview of reported symptoms between exposed and control group on the Likert scale
The symptoms were only reported by 60% of participants in the exposed group. None of the participants from control group reported symptoms, and were excluded from further analysis in the logistic and linear regression. In addition, none of the participants from the exposed group reported the symptoms to have affected their work practice. The majority of participants experienced at least eight symptoms related to SMFs seldomly and half of the time, with few reporting symptoms frequently (usually). RF energy-related and SHC symptoms were reported seldomly and frequently (usually) by very few participants. The relationship between predictors and reporting of symptoms are outlined in .
Table 3. Relationship between predictors and subjective symptoms using logistic regression
The reporting of tinnitus was significantly different (p< .034) between various job titles and the odds of experiencing it often, was noted to be very low (OR: 0.12; CI 0.02, 0.85). MR staff that indicated to have worked on a 3 T scanner during their workweek, were eight times more likely (OR: 8.00; CI 1.51, 42.46) to report tinnitus than those who worked on a 1.5 T or both scanners. There was a two-fold increased risk of reporting tinnitus amongst female MR staff (OR: 2.70; CI 0.48, 15.17), but remained statistically non-significant when compared with male participants. The reporting of headache between those that had one to 4 years and 5 to 15 years of experience working in the MRI units was significantly different (p< .05). As the years of experience in the MRI units increases, the risk of reporting headaches increased by four folds (OR: 4.57; CI 0.96, 21.70).
The odds of reporting nausea also was very low (OR: 0.06; CI 0.01, 0.48) and significantly different between job titles (p< .01). However, an increased risk of reporting it often (11 times higher) among female participants (OR: 11.20; CI 1.57, 79.92) was noted. The relationship between workload and reporting of nausea was statistically non-significant, and the increased risk of reporting it often was twofold (OR: 2.66; CI 0.45, 15.75), higher among those who had a light to moderate workload. The relationship between suddenly feeling warm and all predictors was statistically non-significant. However, those with 5–15 years of MRI experience (OR: 2.86; CI 0.52, 15.60) and those with 8-hour shift duration (OR: 2.39; CI 0.51, 11.16) had twofold increased risk of reporting suddenly feeling of warmth.
The relationship between vertigo and various shift durations (p< .05), and tiring workweek (p< .05) were significantly different. The increased risks of reporting vertigo often among female participants (OR: 4.43; CI 0.91, 21.47), those with 5–15 years of MRI experience (OR: 2.09; CI 0.47, 9.34), and a light to moderate workload (OR: 2.70; CI 0.49, 14.86) were observed. The MR staff who worked on a 3 T scanner (OR: 9.67; CI: 1.44, 64.92), and those with 5–15 years of MRI experience (OR: 3.99; CI 0.53, 29.95) had increased risks of reporting the feeling of lightheaded. Significantly different relationships between metallic taste and various job titles (p< .05), and gender (p< .03) were noted. The MR female staff (OR: 6.42; CI 1.27, 32.51) had a six fold increased risk of reporting metallic taste, and twofold increased risk was observed among those who reported to have little to moderate workload (OR: 2.83; CI 0.51 15.85). The feeling of instability was significantly associated with tiring workweek (p< .05), and the odds of experiencing it often among those who had very, little and hardly tiring workweek were significantly low. Although the non-significant relationships were observed between the feeling of instability and other predictors, female participants had an increased risk (OR: 4.43; CI: 0.91, 21.47) of reporting instability. Those who had little to moderate workload (OR: 2.70; CI: 0.49, 14.86), and 5–15 years of MRI experience (OR: 2.09; CI: 0.47, 9.34) had twofold increased risk of reporting the feeling of instability. The relationship between predictors and subjective symptoms that had insufficient responses are reported in .
Table 4. Relationship between predictors and subjective symptoms using linear regression
Due to significantly low responses on the four subjective symptoms, a linear regression was used to determine predictors of reporting these symptoms. The non-significant relationships between involuntary muscle contraction, concentration problems and tiredness, and all predictors was found. However, Job title (p< .007), gender (p< .015), and years of experience in the MRI units (p< .003) were significant predictors of reporting sensation of glowing. There was an increased risk of reporting sensation of glowing among male participants and those with 1–4 years of MRI experience. In addition, an increased risk of reporting sensation of glowing within the occupational groups represented by small number of participants was observed.
Reporting of symptoms due to performance of activities in zone IV
Linear regression was used to determine if movement of head/ upper body in the scanner bore, presence longer stay in zone IV due to irregularities and during image acquisitioning could predict the reporting of subjective symptoms. Irregularities (mainly emergency) that made MR staff to stay longer in zone IV than usual were significant predictors of all symptoms, except for tiredness (p< .93) and sensation of glowing (p< .89) (). Presence in zone IV during image acquisitioning was the only significant predictor for the sensation of glowing (p < .000). Furthermore, movement of head/ upper body in the scanner bore also was a significant predictor of nausea (p < .026), vertigo (p < .014), instability when standing (p < .014), and a metallic taste (p < .031).
Table 5. Reporting of subjective symptoms based on the presence in zone IV
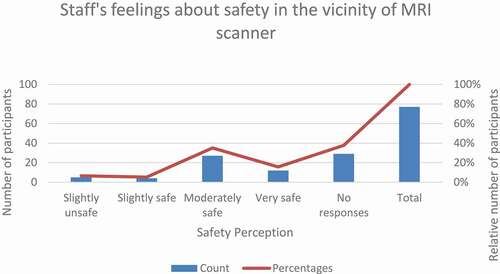
Perceived risk of scanners and safety training
The response on perceived risk of scanners ranged from “very safe to very unsafe”, and the results are summarized in . Out of 62% of respondents (46 exposed and 2 controls), 16% felt very safe, while 35% felt moderately safe, and 5% felt slightly safe around MRI scanners. Only 6% of participants felt slightly unsafe, and none of the participants felt moderately and very unsafe. The bivariate spearman test suggested no correlation between perceived risk of scanners, gender, and reported symptoms except for sensation of glowing. Sensation of glowing was positively correlated with perceived risk of scanners (rs = 0.27; p= .04). Also, shift duration (rs = 0.58; p= .02), scanner worked on during various shifts (rs = 0.30; p= .04) and movement of head/upper body in the scanner bore (rs = 0.42; p= .05) were positively correlated with perceived risk of scanners. A negative correlation between perceived risk of scanners, workload (rs = −0.49; p= .00), tiring workweek (rs = −0.49; p= .000), and training on safety of MR personnel (rs = −0.33; p= .02) was found.
Only thirty-four (44%) participants received training about the safety of personnel in the MRI units, and 46% received training on the health effects of exposure to SMFs and RF energy. Only maintenance engineers and medical physicists suggested that there were control measures in place to minimize the harmful effects of exposure to SMFs and RF energy from MRI scanners.
Discussion
This is the first study to assess perceived risk of scanners and reporting of SMFs- and RF energy- related symptoms among 1.5 and 3 T MR workers in South Africa. The majority of exposed participants (60%) reported to have experienced both symptoms related to SMFs and RF energy exposures. The results of this study suggest that the majority of MR staff working with both 1.5 and 3 T scanners (56%) perceive MR scanners to be safe. Their perception of the safety around MR scanners was not affected by the symptoms they experienced during their work shifts. Although this study only evaluated staff working with 1.5 and 3 T scanner, similar observations were made in a risk perception study conducted in Europe among 7 T MR workers (Fatahi et al. Citation2016). This could be attributed to their knowledge of MR scanners and years of experience working in the MRI units. There was an increased reporting of tinnitus and the feeling of instability among those who worked with 3 T scanner. This support the findings of previous studies (Wilén and De Vocht Citation2011; Schaap et al. Citation2014 & de Vocht et al. Citation2006), where an increased reporting of symptoms were noted when exposure increased from 0 to 7 T. Majority of participants (which were females) also re-ported experiencing symptoms such as headache, nausea, vertigo and tiredness often, and were more prevalent among those reported to have light workload. Light workload was mostly reported than any other workload, and thus was not a significant predictor of reporting these symptoms. This was also highlighted by Wilén and De Vocht (Wilén and De Vocht Citation2011) that workload is not associated with reporting of MRI-related subjective symptoms. Contrary, a tiring workweek was a significant predictor of reporting vertigo and the feeling of instability. It was noted that some medications taken by participants (31%) daily had side effects such as dizziness (vertigo), nausea, and headaches, which are symptoms reported in other studies to be associated with exposure to SMFs (Fatahi et al. Citation2016; Zanotti et al. Citation2016.
Reporting of symptoms was also noted to vary across different years of experience participants had. However, participants with 5–15 years of MRI experience reported more symptoms. Although this is a relatively new study to report symptoms based on years of experience in the MRI units, many of the subjective symptoms reported in this study, and how they occur, remain unknown (De Vocht et al. Citation2015), and a perception threshold may exist for certain symptoms as well (Hansson Mild et al. Citation2019). Sensation of glowing was classified as RF-related exposure symptom, and was reported by small number of participants (medical physicists, maintenance engineers, few nurses and radiographers). These participants have indicated to have been in zone IV, performing activities proximal to the scanner during image acquisitioning. Shift duration was a significant predictor of vertigo. Those who spent longer hours (8 hrs) in zone IV, proximal to the scanner, reported to experience vertigo often. Also, metallic taste was more prevalent among females (majority participants). Antunes et al. (Antunes et al. Citation2012) and Fatahi et al. (Fatahi et al. Citation2016) suggest that strong magnetic fields are the main contributing factor to evoke most of the acute transient symptoms experienced by those proximal to the scanners.
Similarly, longer stay in zone IV, due to emergencies, was a significant predictor of a majority of SMFs-related symptoms. Because of a small room size in zone IV, all participants who entered and stayed longer in the zone were significantly exposed to SMFs, hence an increased reporting of SMFs-related symptoms. Only sensation of glowing, as RF-related symptom, was reported by those who were proximal to the scanner, either repositioning the phantom or assisting a patient, while the scanner was operating. Karpowicz and Gryz (Karpowicz and Gryz Citation2006) also suggested that exposure to RF energy among MR personnel is significant in close proximity to the scanner, particularly when patients are scanned. In addition, exposure to RF energy could raise the tissue temperature and result in thermal effects (Schaap et al. Citation2014). Those who indicated to have moved their head/ upper body in the scanner bore reported nausea, vertigo, instability when standing and a metallic taste. The number of times participants moved their head/ upper body in the scanner bore did not suggest any severity within the symptoms they experienced. However, all the symptoms lasted for a very short period of time, and this has been reported in other studies (De Vocht et al. Citation2015; Schaap et al. Citation2014).
The association between sensation of glowing and perceived risk of scanners could be explained by participants who initially reported sensation of glowing when either reposition phantom or assisting patients while the scanner was operating. Majority of participants who moved their head/upper body in the scanner bore 3–4 times, those with longer shift durations (8 hrs) and those who worked on 3 T scanners perceived MR scanners to be slightly unsafe. As aforementioned, there was an in-creased reporting of symptoms as the strength of the scanner increases; this might have led to participants perceiving the scanners to be unsafe. Also reporting of SMFs-related symptoms due to movement of head/ upper body in the scanner bore attributed to perception of unsafeness. Of all the MR staff, only 44% indicated to have received training on the safety of MR scanners. Although this was negatively correlated, the perception of feeling unsafe around MR scanners was also attributed to insufficient training, and this has been noted in a European study (Fatahi et al. Citation2016).
Conclusions
This is one of the relatively few studies investigating the reporting of SMFs and RF energy-related symptoms among MR staff working with 1.5 and 3 T scanners, and the first such study in Southern Africa. This study revealed that job titles, years of experience in the MRI units, longer shift durations, higher scanner strength, longer stay in zone IV, and movement of head/upper body in the scanner bore are potential predictors for subjective symptoms related to SMFs and RF energy. It is also noted that MR safety training, higher scanner strength and movement of head/upper body in the scanner bore attribute to a perception of unsafeness around MR scanners.
This survey required participants to reflect on the symptoms they experienced during their workweek, this was more likely to invite response bias. The use of certain medication with side effects similar to symptoms reported and psychosocial influences might have affected the reporting patterns among individuals. The variability between job titles and shift durations suggest the importance of personal measurements than to rely only on self-reporting surveys.
Author contributions
“Conceptualization, PCR; methodology, PCR; formal analysis, PCR; investigation, PCR; resources, PCR; data curation, PCR; writing—original draft preparation, PCR; writing—review and editing, PCR. The author has read and agreed to the published version of the manuscript.”
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of University of the Free State (UFS-HSD2018/0438/3107 [2018]).
Informed consent statement
Written informed consent has been obtained from the participants to publish this paper.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Antunes, A., P. M. Glover, Y. Li, O. S. Mian, and B. L. Day. 2012. Magnetic field effects on the vestibular system: Calculation of the pressure on the cupula due to ionic current-induced Lorentz force. Phys. Med. Biol. 57:44–77. doi:https://doi.org/10.1088/0031-9155/57/14/4477.
- Bradley, J. K., M. Nyekiova, D. L. Price, L. D. Lopez, and T. Crawley. 2007. Occupational exposure to static and time-varying gradient magnetic fields in MR units. J. Magn. Reson. Imaging 26:1204–09. doi:https://doi.org/10.1002/jmri.21152.
- Capstick, M., D. McRobbie, J. Hand, A. Christ, S. Kuhn, K. Hansson Mild, E. Cabot, Y. Li, A. Melzer, A. Papadak, K. Prussmann, R. Quest, M. Rea, S. Ryf, M. Oberte, and N. Kuster. 2008. An investigation into occupational exposure to electro-magnetic fields for personnel working with and around medical magnetic resonance imaging equipment. Report on Project VT/2007/017 of the European Commission Employment, Social Affairs and Equal Opportunities DG, http://www.myesr.org/html/img/pool/VT2007017FinalReportv04.pdf. Accessed May 30, 2020.
- De Vocht, F., E. Batistatou, A. Mölter, H. Kromhout, K. Schaap, M. Van Tongeren, S. Crozier, P. Gowland, and S. Keevil. 2015. Transient health symptoms of MRI staff working with 1.5 and 3.0 Tesla scanners in the UK. Eur. Radiol. 25:2718–26. doi:https://doi.org/10.1007/s00330-015-3629-z.
- de Vocht, F., H. van Drooge, H. Engels, and H. Kromhout. 2006. Exposure, health complaints and cognitive performance among employees of an MRI scanners manufacturing department. J. Magn. Reson. Imaging 23:197–204. doi:https://doi.org/10.1002/jmri.20485.
- Eriksen, H. R., C. Ihlebæk, and H. Ursin. 1999. A scoring system for subjective health complaints (SHC). Scand. J. Public Health 27:63–72. doi:https://doi.org/10.1177/14034948990270010401.
- Fatahi, M., L. R. Demenescu, and O. Speck. 2016. Subjective perception of safety in healthy individuals working with 7 T MRI scanners: A retrospective multicentre survey. Magn. Reson. Mater. Phys. Biol. Med. 29:379–87. doi:https://doi.org/10.1007/s10334-016-0527-6.
- Foster, K. R., M. C. Ziskin, Q. Balzano, and G. BitBabik. 2018. Modeling tissue heating from exposure to radiofrequency energy and relevance of tissue heating to exposure limits: Heating factor. Health Phys. J. 115:295–307. doi:https://doi.org/10.1097/HP.0000000000000854.
- Frankel, J., J. Wilén, and K. Hansson Mild. 2018. Assessing exposures to magnetic resonance imaging’s complex mixture of magnetic fields for in vivo, in vitro, and epidemiologic studies of health effects for staff and patients. Front. Public Health 12:66. doi:https://doi.org/10.3389/fpubh.2018.00066.
- Hansson Mild, K., R. Lundström, and J. Wilén. 2019. Non-ionizing radiation in Swedish Health Care: Exposure and safety aspects. Int. J. Environ. Res. Public Health 16:11–86. doi:https://doi.org/10.3390/ijerph16071186.
- Hartwig, V., S. Romeo, and O. Zeni. 2018. Occupational exposure to electromagnetic fields in magnetic resonance environment: Basic aspects and review of exposure assessment approaches. Med. Biol. Eng. Comput. 56:531–45. doi:https://doi.org/10.1007/s11517-017-1779-7.
- Heinrich, A., A. Szostek, P. Meyer, F. Nees, J. Rauschenberg, J. Gröbner, M. Gilles, G. Paslakis, M. Deuschle, W. Semmler, et al. 2013. Cognition and sensation in very high static magnetic fields: A randomized case-crossover study with different field strengths. Radiology 266:236–45. doi:https://doi.org/10.1148/radiol.12112172.
- International Electrotechnical Commission (IEC). 2010. Medical electrical equipment Part 2-33: Particular requirements for the basic safety and essential performance of magnetic resonance equipment for medical diagnosis. 3rd ed. Geneva: International Standard IEC 60601-2-33.
- Kabongo, J. M., S. Nel, and R. D. Pitcher. 2015. Analysis of licensed South African diagnostic imaging equipment. Pan Af. Med. J. 22:57. doi:https://doi.org/10.11604/pamj.2015.22.57.7016.
- Karpowicz, J., and K. Gryz. 2006. Health risk assessment of occupational exposure to a magnetic field from magnetic resonance imaging devices. Int. J. Occup.l Saf. Ergon. 12:155–56. doi:https://doi.org/10.1080/10803548.2006.11076679.
- Neufeld, E., M. Fuetterer, M. Murbach, and N. Kuster. 2015. Rapid method for thermal dose-based safety supervision during MR scans. Bioelectromagnetics 36:398–407. doi:https://doi.org/10.1002/bem.21919.
- Rathebe, P., C. Weyers, and F. Raphela. 2021. Exposure levels of radiofrequency magnetic fields and static magnetic fields in 1.5 and 3.0 T MRI units. SN Appl. Sci. 3:157. doi:https://doi.org/10.1007/s42452-021-04178-3.
- Schaap, K., L. Portengen, and H. Kromhout. 2016. Exposure to MRI-related magnetic fields and vertigo in MRI workers. Occup. Environ. Med. 73:161–66. doi:https://doi.org/10.1136/oemed-2015-103019.
- Schaap, K., Y. Christopher-devries, C. K. Mason, F. De Vocht, L. Portengen, and H. Kromhout. 2014. Occupational exposure of healthcare and research staff to static magnetic stray fields from 1.5–7 tesla MRI scanners is associated with reporting of transient symptoms. Occup. Environ. Med. 71:423–29. doi:https://doi.org/10.1136/oemed-2013-101890.
- Schaap, K., Y. Christopher-devries, P. Slottje, and H. Kromhout. 2013. Inventory of MRI applications and workers exposed to MRI-related electromagnetic fields in the Netherlands. Eur. J. Radiol. 82:2279–85. doi:https://doi.org/10.1016/j.ejrad.2013.07.023.
- Shrivastava, D. 2007. On the choice of RF safety metric in MRI: Temperature, SAR, or thermal dose. eMagRes 15:189–94.
- Theron, I., R. K. Segoenyane, F. Makosa, W. Rae, and A. Conradie. 2015. Comparison between the quality control results of the 3 Tesla and 1.5 Tesla magnetic resonance imaging units at Universitas Academic Hospital. Eur. J. Med. Phys. 31:S13. doi:https://doi.org/10.1016/j.ejmp.2015.07.133.
- van den Brink, J. S. 2019. Thermal effects associated with RF exposures in diagnostic MRI: Overview of existing and emerging concepts of protection. Concepts Magn. Reson. Part B 2019:1–17. doi:https://doi.org/10.1155/2019/9618680.
- van Nierop, L. E., P. Slottje, M. J. van Zandvoort, F. de Vocht, and H. Kromhout. 2012. Effects of magnetic stray fields from a 7 tesla MRI scanner on neurocognition: A double-blind randomised crossover study. Occup. Environ. Med. 69:759–66. doi:https://doi.org/10.1136/oemed-2011-100468.
- Van Schouwenburg, F., C. Ackermann, and R. Pitcher. 2014. An audit of elective outpatient magnetic resonance imaging in a tertiary South African public-sector hospital. S. Afr. J. Radiol. 18:5. doi:https://doi.org/10.4102/sajr.v18i1.689.
- Wilén, J., and F. De Vocht. 2011. Health complaints among nurses working near MRI scanners - A descriptive pilot study. Eur. J. Radiol. 80:510–13. doi:https://doi.org/10.1016/j.ejrad.2010.09.021.
- Zanotti, G., G. Ligabue, L. Korpinen, and F. Gobba. 2016. Subjective symptoms in magnetic reso nance im aging operators: Pre valence, short-term evolu tion and possible related factors. Med. Lav. 107:263–70.