ABSTRACT
Differential diagnoses of primary bladder tumors from metastasis ones can be difficult, for the symptom and imaging findings are pretty similar. Here, we reported a case of bladder metastasis from lung adenocarcinoma. A 73-year-old female patient who was diagnosed with bladder metastasis from lung adenocarcinoma presented as gross hematuria and multiple pedicled masses in the bladder on MRI scan. Such clinical manifestations were easily misdiagnosed as primary bladder malignancy. Additionally, the tumor samples of this case were further harvested and processed for histopathological analysis and gene detections to confirm this case as a metastasis tumor that was refractory to the subsequent therapy. Diagnosis of bladder metastasis should be paid more consideration in patients with a history of cancer despite the fact that primary bladder malignancy accounts for the majority of bladder masses.
Background
Bladder masses, together with hematuria, are common findings of bladder tumors. Among bladder tumors, primary ones are reported to be the most frequent types.Citation1 Secondary tumors of the urinary system usually originate from direct invasion from the surrounding organs, including prostate, lower gastrointestinal tract, and female genital tract cancers. Metastatic spread via vascular and lymphatic ways to urinary routes is rarely reported, especially to the bladder.Citation2 Among non-genitourinary primary sites, colorectal, pulmonary, skin (melanoma), and breast are the most common contributors.Citation3 Here, we described a case of bladder metastasis from lung adenocarcinoma, presenting as gross hematuria and multiple pedicled masses in the bladder on MRI scan, which manifestations were easily confused with primary bladder malignancy. The aim of this report is to demonstrate a rare metastatic pattern of nonsmall cell lung cancer and emphasize the importance of differential diagnosis of primary and metastatic tumors of the bladder from lung cancer.
Case presentation
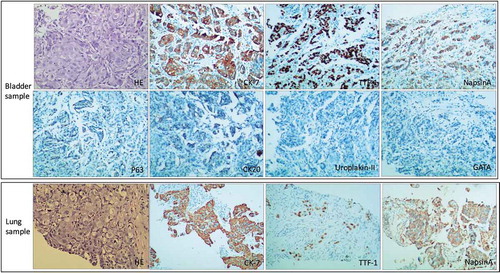
A 73-year-old female patient presented with gross hematuria, combined with odynuria, persisting for 2 days, in June 2018. A urine test showed the number of RBC in urine is 426.8/μl (normal 0–17/μl) and 80% of the RBCs are nonglomerulonephrogenic cells. And the number of white blood cells in urine was 31.20/μl (normal 0–15.4/μl). Urinary infection was considered first, and levofloxacin was administrated for 7 days; however, no significant improvement has been found with regard to hematuria. Herein, urological examinations were performed. Urinary B-mode ultrasound showed a hypoechoic mass (8.7*3.8*4.0 cm) at the bottom of the bladder, with an irregular shape, inhomogeneous internal echoes, and no internal inconspicuous bloodstream signs. Pelvic MRI scan demonstrated multiple pedicled masses hanging on the inner side of the bladder wall (). Based on these findings, the primary bladder tumor was considered first and cystoscopy was highly recommended. During the cystoscopy, a round mass was found in the trigonometric region of the bladder; meanwhile, multiple blood clots were detected inside the bladder, and no further exploration proceeded. Bladder mass biopsy was performed, and histological examination demonstrated the sample was not primary but metastatic bladder tumor. Immunohistochemical staining of the sample was negative with CK20, Uroplakin-II, GATA, diffusely positive with CK7, TTF-1, and NapsinA, and facol positive with P63 ()-A. This immunohistochemical staining result proposed that the primary origin would be lung adenocarcinoma.
Figure 1. Pelvic MRI:several enhancing solid masses protruding into the bladder lumen were detected in T1-weighted image (arrows)
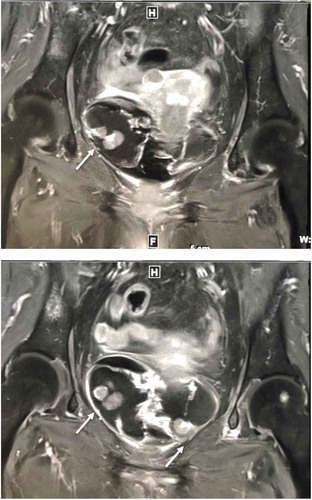
Figure 2. Histopathological findings in metastatic bladder and primary lung adenocarcinoma samples. In bladder sample (upper) and lung sample (under), the adenocarcinoma is visible with hematoxylin and eosin staining. Both samples immunohistochemical stains demonstrate the same positive for cytokeratin-7, TTF-1 and napsin A; negative P63, CK20, Uroplakin-II and GATA staining in bladder sample. Original magnification, ×100
Thirteen months before the presence of gross hematuria, the patient consulted her physician because of cough and expectoration. Her thoracic CT scan revealed a solid mass in the upper lobe of the left lung, together with multiple pleural nodules on the same side ()-A. Punch biopsy histology of the mass was positively stained with CK7, TTF-1, NapsinA, P63, and CK5/6 ()-B, and negatively with P40, CgA, and Syn. Meanwhile, gene detection of the tumor sample demonstrated EGFR gene exon-19 c.2240_2257del18, p.L747_S752delLREATS, and Bim1 gene 2903bp deletion.
Gefitinib 250 mg daily was delivered and progression-free period was 7 months. After the first progression, the patient performed blood gene detection, but no EGFR T790M mutation was found. However, the patients used osimertinib privately for 5 months until a CT scan revealed her disease progression. Since then, a chemotherapy regimen (pemetrexed 900 mg d1 and cisplatin 150 mg d1-3 iv) was delivered. Interestingly, after two cycles of treatment, we detected that her primary tumor in the left lung responded to the chemotherapy regimen, except for her adrenal gland and liver metastasis sites (). One week later, gross hematuria appeared and no further treatment was administrated thereafter. The patient died 1 month after the presence of gross hematuria because of multiple organ failure.
Discussion and conclusions
Lung cancer ranks the first diagnosed malignancy worldwide. According to previous analysis, the main metastatic sites of lung cancer are lymph nodes, liver, brain, bone, and adrenal gland; however, metastasis to the urinary tract from lung cancer is pretty rare.Citation4 A large investigation of uncommon metastatic sites of NSCLC revealed no bladder metastasis out of 2872 stage IV NSCLC patients.Citation3 What is more, a report of autopsies of 250 patients with NSCLC revealed no metastasis to the bladder.Citation5 Reviewing previous literatures, we only found 13 cases of bladder metastasis from lung cancer reported before ().
Table 1. List of reported cases of lung metastases to the bladder
Gross hematuria was the most common clinical presentation of bladder metastasis from lung cancer.Citation19 Just as in our case, gross hematuria in combination with odynuria was the main symptom of the patient, and urinary infection was considered at the very beginning. In such a case, gross hematuria was usually the symptom of infiltration or ulceration of bladder lining by the malignant cells; thus, gross hematuria is usually a hint of late-stage manifestation of bladder metastasis.Citation6 Microscopic hematuria was also reported, but in only one case of bladder metastasis from lung cancer.Citation8 Therefore, when lung cancer patients present with microscopic hematuria, urinary tract metastasis should also be taken into differential diagnosis consideration. Apart from hematuria, hydronephrosis alone or combined with hematuria was another presentation of bladder metastasis.Citation7,Citation8,Citation11,Citation13 Moreover, oliguria and urolithiasis were also reported.Citation9,Citation12 Some cases of bladder metastasis demonstrated no symptoms, which were detected in routine follow-up imaging examinations of lung cancer.Citation10,Citation14 Notably, pelvic pain was usually a manifestation of direct invasion of the bladder from surrounding tumors or pelvic tissue involvement induced by primary bladder cancer, but not usually a symptom of bladder metastasis.Citation20
Imaging technologies, such as pelvic CT and MRI, are quick and noninvasive evaluation methods for exploring space-occupation in the bladder. According to previous reports, most bladder metastasis from lung cancer manifested as thickness or board-based masses on the bladder wall.Citation7,Citation8,Citation11,Citation13,Citation14,Citation20 However, our case is the first reported bladder metastasis tumor, to our knowledge, presenting as pedicled masses on the bladder wall, which imaging appearance was consistent with primary bladder cancer. What is more, the number of lesions on the bladder wall is another part of distinguishing primary and metastatic bladder carcinoma. As summarized before, under cystoscopy, single lesions were detected in 60% cases of bladder metastasis from lung cancer, and multiple lesions account for 20%, the left 20% cases demonstrated intact bladder mucosa.Citation19 Therefore, “multiple lesions” and “pedicled masses” together complicated the differential diagnosis between metastatic bladder tumor from lung and primary bladder cancer in our case, which relied strongly on pathologic evaluation and immunohistochemistry distinguish.
Immunohistochemical staining of marker CK7 and CK20, representing epithelial origins, was performed firstly in our case. The staining result demonstrated CK7+/CK20-, which suggested a lung or bladder primary. Further, two urothelial immunohistochemical markers, including Uroplakin-II and GATA, were selected for differentiating primary bladder cancer from its metastases.Citation21 Strikingly, both Uroplakin-II and GATA staining were negative, though pelvic imaging of our case hinted at “primary bladder tumor”. However, lung adenocarcinoma immunohistochemical markers TTF-1 and Napsin A were stained positively here, which were consistent with the patient’s earlier staining of lung mass biopsy sample. Herein, taken them all together, this case provided us a difficult differential diagnosis of multiple bladder-pedicled masses, which were finally confirmed by pathological staining analysis suggesting bladder metastasis from lung adenocarcinoma.
Reviewing all the published reports of lung cancer with bladder metastasis, only one case mentioned lung cancer gene mutation status.Citation18 Together with this case, both of these two lung cancer patients with bladder metastasis presented EGFR exon-19 deletion without T790M mutation, primarily and after targeted therapy. Additionally, in our case, Bim1 gene deletion was also detected in the primary lung cancer sample. Bim1 deletion was the most important independent prognostic factor in shorter progression-free survival (PFS) of EGFR tyrosine kinase inhibitor treatment.Citation22 In our case, the PFS of gefitinib therapy was 6 months, shorter than the average 10 months. In addition, BIM deletion may also contribute to the intrinsic resistance to chemotherapy in advanced NSCLC.Citation23Citation24 Interestingly, the metastasis sites in our case did not respond well to chemotherapy, except for her primacy lung carcinoma. Thus, further investigation should focus on gene heterogeneity between primary and metastatic sites of lung cancer, especially in the uncommon bladder metastasis part.
Abbreviations
| MRI | = | Magnetic resonance imaging |
| CT | = | Computed Tomography |
| RBC | = | Red blood cells |
| CK20/7 | = | Cytokeratin 20/7 |
| TTF | = | Thyroid transcription factor |
| CgA | = | Chromogranin A |
| Syn | = | Symaptophysin |
| EGFR | = | Epidermal growth factor receptor |
| NSCLC | = | Nonsmall cell lung cancer |
| SCLC | = | Small cell lung cancer |
| ADC | = | Adenocarcinoma |
| n.m | = | Not mention |
| BIM | = | Bcl-2 interacting mediator of cell death |
Ethics approval and consent to participate
Clinical specimens were obtained under the approval of the Institutional Ethics Committee. Informed consent was obtained from the subject. Research involving human subjects, human material, or human data, have been performed in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient’s daughter for publication of this case report. A copy of the written consent is available for review by the editor of this journal.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Author contribution
LLZh and DSZ designed and analyzed the data. XQL and LLZh drafted and revised the manuscript. LLZ and XW made contributions to the acquisition of data. WJS confirmed the pathological imaging. All the authors have given the final approval of the version to be published. All the authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Acknowledgments
The authors thank all of our colleagues who helped us with data collection.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Bates AW, Baithun SI. Secondary neoplasms of the bladder are histological mimics of nontransitional cell primary tumours:clinicopathological and histological features of 282 cases. Histopathology. 2000;36(1):32–40.
- Bates AW, Baithun SI. The significance of secondary neoplasms of the urinary and male genital tract. Virchows Arch. 2002 Jun;440(6):640–647. doi:10.1007/s00428-001-0549-x.
- Fei-Yu N, Qing Z, Jin-Ji Y, Zhong W-Z, Zhi-Hong C, Wei D, Yan-Yan H, Hua-Jun C, Zhu Z, Ke -E-E, et al. Distribution and prognosis of uncommon metastases from non-small cell lung cancer. BMC Cancer. 2016;16:149. doi:10.1186/s12885-016-2169-5.
- L E Q, Tummala S, L J B, I R F, A S K, Kazerooni EA, M D I, R I W, Orringer MB. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg. 1996;62:246–250. doi:10.1016/0003-4975(96)00220-2.
- Budinger JM. Untreated bronchogenic carcinoma: A clinicopathological study of 250 autopsied cases. Cancer. 1958;11(1):106–116. doi:10.1002/1097-0142(195801/02)11:1<106::AID-CNCR2820110121>3.0.CO;2-9.
- Lan SK, Lin YH, Tzai TS, Tsai YS. A rare instance of lung cancer metastasizing to the uri- nary bladder. J Taiwan Urol Assoc. 2006;17:63–66.
- Liao CH, Jan CI, Hsiao PJ. Transurethral resection of bladder metastasis from lung small-cell carcinoma. J Taiwan Urol Assoc. 2006;17:71–74.
- Bivalacqua TJ, Alphs H, Aksentijevich I, Schaeffer EM, Schoenberg MP. Paraneoplastic polyarthritis from non-small-cell lung cancer metastatic to the bladder. J Clin Oncol. 2007;25:2621–2623. doi:10.1200/JCO.2007.11.5600.
- Karatas OF, Bayrak R, Yildirim E, Bayrak O, Cimentepe E, Unal D. Bladder metastasis of non-small cell lung cancer: an unusual cause of hematuria. Int J Hematol Oncol. 2009;19:246–248.
- Raspollini MR, Comin CE, Crisci A, Chilosi M. The use of placental S100 (S100P), GATA3 and napsin A in the differential diagnosis of primary adenocarcinoma of the bladder and bladder metastasis from adenocarcinoma of the lung. Pathologica. 2010;102:33–35.
- Karle W, Barazani Y, Tareen B. A rare case of metastatic lung cancer to the bladder. Can Urol Assoc J. 2012;6:E147–E149. doi:10.5489/cuaj.307.
- Shirakawa H, Kozakai N, Sawafuji M, Sugiura H, Hara S. Urinary bladder metastasis originating from lung adenocarcinoma: a case definitively diagnosed by immunohistochemistry. Urol J. 2012;9:530–532.
- Modh RA, Corbyons KA, Yeung LL. A rare metastasis to the bladder. Case Rep Urol. 2013;2013:789039.
- Cormio L, Sanguedolce F, Fino GD, Massenio P, Liuzzi G. Bufo P and Carrieril G. Bladder metastasis from lung adenocarcinoma: a dif- ficult differential diagnosis with primary bladder adenocarcinoma. World J Surg Oncol. 2014;12:90. doi:10.1186/1477-7819-12-90.
- Raymond KW, Hin TS, Fai KC, Steve CW. Urinary bladder metastasis from lung adenocarcinoma: a rare cause of hematuria. Urol Ann. 2014;6:359–362. doi:10.4103/0974-7796.141006.
- Ye HJ, Ma J, Liu YJ, Ye XF, Zhang LW, Li JG. Metastatic lung adenocarcinoma to the bladder: a case report. Oncol Lett. 2015;10:1674–1676. doi:10.3892/ol.2015.3445.
- Bientinesi R, Pierconti F, Gandi C, Santoro AA, Vaccarella Pinto F, Racioppi M, Palermo G, Bassi P, Sacco E. Bladder and prostate metastasis from small cell lung cancer: a rare entity. Open Access J Urol Nephrol. 2016;1(2):000110.
- Kuga T, Machida K, Ito H, Matsuo M. Bilateral hydronephrotic bladder metastasis from lung cancer. Intern Med. 2018;57(12):1801. doi:10.2169/internalmedicine.9535-17.
- Francesca S, Domenico L, Francesco S, Maurizio DB, Giuseppe L, Giuseppe C, Pantaleo B, Luigi C. Bladder metastases from lung cancer: clinical and pathological implications: a systematic review. Oncology. 2017;92(3):125–134. doi:10.1159/000454731.
- Grignon DJ, Epstein JI, Oliva E, Ro JY, Shen SS. Metastatic tumours. In: Moch H, Humphrey PA, Ulbright TM, Reuter VE editors. WHO classification of tumours of the uri- nary system and male genital organs. 4 ed. Lyon: IARC; 2016.
- Leivo MZ, Elson PJ, Tacha DE, Delahunt B, Hansel DE. A combination of p40, GATA-3 and uroplakin II shows utility in the diagnosis and prognosis of muscle-invasive urothelial carcinoma. Pathology. 2016;48(6):543–549. doi:10.1016/j.pathol.2016.05.008.
- Ng KP, Hillmer AM, Chuah CT, Juan WC, Ko TK, Teo AS, Ariyaratne PN, Takahashi N, Sawada K, Fei Y, et al. A common BIM deletion polymorphism mediates intrinsic resistance and inferior responses to tyrosine kinase inhibitors in cancer. Nat Med. 2012;18(4):521–528. doi:10.1038/nm.2713.
- Zhang J, Zheng D. BIM deletion polymorphism and the clinical outcome of patients with advanced NSCLC who received first- line platinum-based chemotherapy: preliminary results. J Clin Oncol. 2013;31(Suppl):abstr e22137. doi:10.1200/jco.2013.31.15_suppl.e22137.
- Morichetti D, Mazzucchelli R, Lopez Beltran A. Secondary neoplasms of the urinary system and male genital organs. BJU Int. 2009;104(6):770–776. doi:10.1111/j.1464-410X.2009.08746.x.Epub 2009 Jul 14.