Abstract
This study investigates behavioral adaptation to vibrotactile position-avoidance therapy during sleep in patients with obstructive sleep apnea (n =135) across 15 to 52 weeks. The overall compliance, based on nights used ≥ 4 hr, was 71%. Overall regular use, that is, ≥ 4 hr/night over 70% of nights, was 88%. Poor early compliance strongly predicted poor long-term treatment adherence, with 92% of those noncompliant across the first 12 weeks of therapy remaining noncompliant. Conversely, 21% of those with compliant utilization in the short term became noncompliant in the long term. It appears that patients do not habituate to the stimulus during sleep, nor was there a training effect associated with long-term use.
Treatment outcomes in patients with obstructive sleep apnea (OSA) are often limited by poor compliance with prescribed management strategies. Motivational enhancement education was recently shown to affect behavior and improve outcomes for the treatment of OSA with continuous positive airway pressure (CPAP; Aloia, Arnedt, Strand, Millman, & Borrelli, Citation2013; Dantus, Winck, & Figueiredo-Braga, Citation2015; Lai, Fong, Lam, Weaver, & Ip, Citation2014). A potentially more widespread behavioral approach for the treatment of OSA would be to limit supine sleep, given the vast majority (i.e., 55%–87%) of those with OSA studied in the current era are at least twice as severe when back-sleeping than when side-sleeping (Levendowski, Seagraves, Popovic, & Westbrook, Citation2014; Oksenberg & Gadoth, Citation2014; Oksenberg, Citation2014; Ravesloot, van Maanen, Dun, & de Vries, Citation2013; Ravesloot, Frank, Verhagen, de Lange, & de Vries, Citation2015). Although positional therapy effectiveness has traditionally been limited to in those with mild to moderate positional OSA (POSA; Jokic, Klimaszewski, Crossley, Sridhar, & Fitzpatrick, Citation1999; Permut et al., Citation2010; van Maanen et al., Citation2013) favorable outcomes have also been reported in those with severe POSA so long as the patient stays off his or her back (Levendowski et al., Citation2014). It has also been demonstrated that supine avoidance reduces Cheyne-Stokes breathing in heart failure patients with central sleep apnea (Joho, Oda, Hirai, & Inoue, Citation2010; Soll et al., Citation2009) and increases the therapeutic response when combined with other OSA therapies (Dieltjens et al., Citation2015; Lee et al., Citation2011). Thus, the majority of patients with sleep apnea would receive therapeutic benefit if they could be behaviorally trained to avoid supine sleep.
Initially, positional therapy was recommended by having patients attach tennis balls to a night shirt (Skinner et al., Citation2008). This delivery of negative reinforcement (i.e., causing pain) was found to be too uncomfortable to be effective long-term (Bignold et al., Citation2009). The employment of padding or foam worn around the waist that restricts the user’s ability to sleep supine resulted in compliance rates at least as good as CPAP (Eijsvogel et al., Citation2015). More recently, vibrotactile positional therapy has been introduced to restrict supine sleep by delivering feedback, a vibratory or haptic stimulus similar to a cell phone vibration, to the neck (Levendowski et al., Citation2014; Levendowski, Veljkovic, Seagraves, & Westbrook, Citation2015; van Maanen et al., Citation2012) or chest (Bignold, Mercer, Antic, McEvoy, & Catcheside, Citation2011; van Maanen et al., Citation2013; van Maanen and de Vries, Citation2014). Vibrotactile positional therapy was found to be effective in improving sleep quality (Levendowski et al., Citation2014) and reducing the number of arousals per hour (Levendowski et al., Citation2014; van Maanen et al., Citation2012). After 30 nights of use, vibrotactile positional therapy reduced complaints of depression and insomnia (Levendowski et al., Citation2014). It also decreased daytime drowsiness and improved quality of life, and achieved greater than 90% compliance (Levendowski et al., Citation2014; van Maanen et al., Citation2013).
A principal advantage of supine avoidance vibrotactile feedback as compared to tennis balls or padding is that delivery of therapy can be delayed to allow the user time to fall asleep on his or her back, an option that would presumably contribute to improved patient compliance. Vibrotactile therapy enables users to sleep more comfortably due to the ease in changing lateral positions. Another advantage of vibrotactile positional therapy is that it can track how often the device is used and whether the user is responding to therapy. As a result, the impact of nocturnal feedback on behavioral adaptation can be readily evaluated.
This study intends to expand our clinical understanding of user behavior with respect to vibrotactile positional therapy. It provides information about patterns of utilization as well as outcome measures that might be expected in patients who undergo long-term supine avoidance treatment over periods up to 52 weeks.
METHODS
A retrospective analysis was conducted on recordings acquired with the Night Shift positional therapy device (Advanced Brain Monitoring, Inc., Carlsbad, CA). The previously described device (Levendowski et al., Citation2014; Levendowski et al., Citation2015) was affixed to the back of the neck with an adjustable nonlatex silicone rubber strap secured by a magnetic clasp (). The instructions provided with the device explained how to adjust the strap to the neck size, when and how to charge the device, the expected feedback patterns, and where instruction videos and user reports could be accessed.
The supine avoidance feedback was delivered with up to two haptic motors, which provided seven unique intensity levels. The second lowest intensity was similar to the vibration delivered by a cell phone. At the highest intensity, the vibration was equivalent to an old-style electric razor, and generated a 36 dB sound heard by a bed partner one meter from the worn device. Feedback began 15 min after the device is turned on, unless the user optionally adjusted the setting to deliver feedback immediately, or with a 30-min delay. Feedback intensity always began at the lowest level each time the user changed to the supine sleeping position. After six attempts of the stimulus at the lowest stimulus, the intensity increased to the next level for another six attempts. This pattern was repeated across the seven intensity levels, and engaged both haptic motors starting at the fifth intensity level. The algorithm applied to the neck-based 3-D accelerometer measures the supine position superior to the chest and sleep–wake superior to wrist actigraphy (Levendowski et al., Citation2014; Levendowski et al., Citation2015). An acoustic microphone allowed measurement of the percentage of time with loud snoring based on the number of sleep epochs with at least one snore > 50 dB divided by the total number of sleep epochs. The lithium polymer battery was capable of delivering therapy for three nights between charges. Immediately after the device was turned on, it vibrated one, two, or three times to indicate the number of therapy nights available before recharging was required.
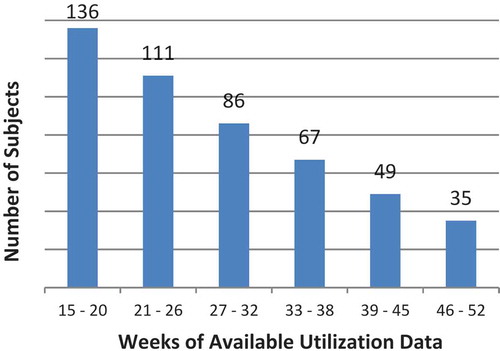
For this study, 141 recordings were selected post-hoc from the report portal. Selection criteria required the device to have been used at least once at the start and end of a 13-week period and had not been repeatedly reformatted (i.e., suggesting an attempt to delete data from the previous user when used by clinicians as a trial device). Only utilization information described below were available; selected recordings were identified by device number. Five records were excluded from analysis to eliminate potentially inaccurate findings resulting from the forward adjustment (by more than one month) of the internal date. Of the remaining recordings, 68% were from users in Australia, 13% from Canada, 7% from Italy, 5% from the Netherlands, 5% from the United States, and 2% from the rest of the world. presents the number of subjects with utilization data available up to a maximum of 52 weeks.
FIGURE 2 Distribution of subjects included in the study based on weeks of available utilization data.
For data reduction, each 24-hr period was analyzed to eliminate utilization bias resulting from the device being turned on or off more than one time. If the elapsed time between the off–on was less than 1 hr and the combined recording time was < 12 hr, the two periods were merged. If the merged recording time was > 12 hr, the longer period was rejected if the shorter study time was > 5 hr, the shorter period was rejected if it was < 5 hr, or the maximum utilization was set to 12 hr. Recording periods were rejected if the sleep efficiency ≥ 97.5% or the recording period was less than 2 hr and the sleep efficiency was < 10% since the patterns suggested user error (e.g., did not properly connect the cable when intending to recharge the device). The elimination of these periods, if made in error, would have biased the data toward underreporting utilization. The last day the device was used was presumed to be the last night of available use. All other gaps in utilization were treated as noncompliance.
Utilization was evaluated by three measures and applied to the most recent 52 weeks of data. The first was defined as the percentage of available nights therapy was used for a minimum of 4 hr (4 hr Compliance). The second was based on at least 4 hr of use on 70% of the available nights of use (Regular Use). The third measure, “Average Hours Used” was computed from the sum of all hours of use divided by the nights the device was available for use. Overall compliance was based on unweighted average across each of the individual “4 hr Compliance” and “Regular Use” measures. Further comparisons between 4 hr Compliance and Average Hours Used were made after stratification into four categories, from Unacceptable to Excellent utilization.
Nightly outcome measures saved in the memory of the device included percentage of sleep time supine, supine attempts per night, the percentage of sleep time snoring > 50 dB, and sleep efficiency. To evaluate behavioral adaption to the feedback, a linear mixed model was applied to “supine attempts per night” and “percent time supine” by and across subjects for the most recent 12 weeks of use. This repeated measures approach accommodated missing data from nights when the device was not used. To further evaluate adaptation of these outcome measures over time, the results from the most recent two weeks of utilization were compared to the two-week period that began 10 weeks earlier (i.e., weeks 11 and 12). A minimum of five nights of utilization was required in each two-week period for the record to be included in the analyses. No effort was made to determine if any of the users delayed the onset of feedback to 30 min or adjust for its impact on the percentage of time supine.
RESULTS
Utilization
Across users, utilization averaged 6.8 hr/night when the device was used. The overall compliance, that is, percentage of nights used at least 4 hr averaged across individuals, was 70.5 ± 20.9%. Overall regular use, defined as more than 4 hr of use per night over 70% of available nights was 88 ± 19.6%.
A further investigation into the underlying variability of compliance results is provided in , whereby 4 hr Compliance rates (nights with ≥ 4 hr use/nights available for use) were compared distributions stratified by the Average Hours Used (total hr used/nights available for use). Both measures delivered essentially equivalent distributions by utilization category with approximately 60% in the acceptable or excellent categories. In total, 29% of subjects were assigned to different categories by the two compliance measures. When those assigned to either acceptable or excellent were consolidated into a “relatively good” compliance category, two utilization measures agreed in 93% of the case. When the marginal and unacceptable groups were similarly combined into a “relatively poor” category, a 91% agreement was obtained between the two utilization measures. While the Average Hours Used provided a better estimate of the total reduction in obstructed breathing events across available night of therapy, the distortion resulting from nonuse could result in the incorrect conclusion that the user was either a short sleeper or that the device was being turned off during the night. The percentage of nights used, and the average hours of use when the device was used, were both substantially lower for those with Average Hours Used < 4 hr ().
TABLE 1 Distributions of Long-Term User Compliance
TABLE 2 Comparison of Long-Term and Initial Compliance
Low utilization during the initial 12 weeks was indicative of those having poor long-term utilization. Of those with Average Hours Used < 4 hr/night, 58% averaged less than 5 hr/night during the first two weeks of therapy and 73% averaged less than 5 hr/night across weeks 11 and 12 (). Those with poor initial compliance (averaged < 5 hr/night) increased from 14% during weeks 1 and 2, to 48% during weeks 11 and 12 for those with long-term Average Hours Used between 4 and 5 hr/night.
Supine Sleep
Three clinically important questions relate to a patient’s behaviorally learned adaptation to position avoidance feedback. First, do patients learn to avoid sleeping supine and thus do not need to constantly use the therapy? Second, do patients adapt to the feedback and ignore it over time? Third, is there a relationship between poor compliance and the frequency of position avoidance feedback?
The linear mixed model, which treated the user as a random effect, showed that the number of supine attempts per night did not change across the 12 weeks of therapy (p = 0.35). A non–statistically significant trend toward a reduction in the percentage of supine sleep time occurred over the same observation period (p = 0.10).
To further investigate whether supine avoidance feedback results is a behaviorally learned response, subjects were stratified into groups who had used position therapy for less than 26 weeks (n = 46), between 26 and 40 weeks (n = 47), and greater than 40 weeks (n = 42) of feedback. The median percentages of supine sleep time for the three groups were 0.3% (IQR = 1.4%), 0.4% (IQR = 1.5%) and 0.3% (IQR = 1.4%) respectively. Across groups, 93% of the subjects experienced a mean supine time less than 10%, and 80% spent less than 5% of their sleep time supine. Ten subjects experienced a mean increase ≥ 5% in supine sleep during the most recent 2-week period compared to the 2-week period that began 10 weeks earlier; six of whom were in the group with the least amount of time on therapy.
The median supine attempts per night for the three groups were 5 (IQR = 7), 5 (IQR = 8) and 5 (IQR = 6), respectively. When comparing the average number of attempts per night from the most recent two weeks of therapy to a two-week period that began 10 weeks earlier, 82% showed a mean change of less than three supine attempts per night. A decrease from a median of nine attempts per night was observed in the 8% of subjects who exhibited a decrease in mean supine attempts of three or more. Conversely, an increase from median of seven supine attempts per night was recorded in the 10% of subjects who exhibited an increase in mean supine attempts. When a more lenient threshold of two or more supine attempts per night was applied to the data set, 70% of the subjects (80/115) exhibited relatively consistent behavior, with 14% of subjects showing a decrease and 16% showing an increase in mean attempts per night.
It did not appear that more frequent supine avoidance feedback had a causal impact on compliance. The trend toward an increased drive to sleep supine in those who averaged at least 5 hr of use per night during the most recent 12 weeks, compared to those who used the therapy less than 5 hr night (mean ± SD: 6.7 ± 21.0 vs. 5.8 ± 12.6 attempts, p = 0.11), was confounded by further stratification. Those who were most and least compliant had a similar distribution of supine attempts (6.1 ± 4.1 and 5.9 ± 3.7, respectively) while those who averaged between 5 and 6 hr of use attempted to sleep supine most often (7.6 ± 5.3) and those who were compliant between 4 and 5 hr per night averaged the fewest supine attempts (5.5 ± 3.6).
Snoring
The median snoring > 50 dB across subject for the most recent 12 weeks of use was 1.1% (IQR = 5.2%). Of clinical interest was whether loud snoring (i.e., snoring > 50 dB in at least 10% of sleep time), a threshold previously associated with at least mild OSA (Levendowski et al., Citation2015), varied or changed substantially over time as a result of supine avoidance therapy. Evaluating the most recent 12 weeks of use across subjects, the percentage of nights with loud snoring from the most recent two weeks of therapy were compared to the two-week period that began 10 weeks earlier. Using differences ≥ 10% as a clinically meaningful threshold, 91% of subjects (105/115) showed no difference in snoring patterns, while 5 subjects showed a decrease and five subjects showed an increase in snoring.
Sleep Efficiency
The sleep efficiency measured by neck actigraphy was previously shown to be negatively correlated with sleep apnea severity; only 25% of those with an apnea-hypopnea index (AHI) < 10 and 16% of those with an AHI < 15 had a sleep efficiency ≥ 80% (Levendowski et al., Citation2015). Evaluating sleep efficiency across the most recent 12 weeks of use, the median value for the group was 83.4% (IQR = 8.8%).
Evaluating the most recent 12 weeks of use across subjects, 77% of subjects (88/115) exhibited no substantial difference (i.e., absolute difference ≥ 5%) when the most recent two weeks of therapy were compared to the 2-week period that began 10 weeks earlier. For those with a sleep efficiency difference > 5%, 12% exhibited a decrease and 11% showed an increase.
DISCUSSION
Applications of vibrotactile feedback to change behavior range from creating awareness when muscles are insufficiently relaxed (Hermens, op den Akker, Tabak, Wijsman, & Vollenbroek, Citation2014) to recognition of uneconomical driving patterns (Birrell, Young, & Weldon, Citation2013). This report provided an assessment of changes in sleep resulting from use of vibrotactile supine avoidance feedback in a relatively large cohort being treated for positional OSA or snoring.
Compliance patterns from users who generate utilization reports were high; 71% of this group used the device an average of at least 4 hr per night over all possible nights. This usage, as well as the Regular Use of 88%, were consistent with previous reports of long-term vibrotactile positional therapy compliance (van Maanen & de Vries, Citation2014). The majority of patients used the therapy on average at least 5 hr or more per night across all available nights. When they wore the device, it was used almost 7 hr night, suggesting poor long-term compliance was impacted more by a lack of consistent nightly use as opposed to partial nightly use. This behavior may be influenced by the fact that positional therapy has been traditionally recommended for patients with milder OSA, and, as a result, symptoms worsening may not be readily noticeable when a night of therapy is missed.
The Average Hours Used was found to be essentially equivalent to the 4 hr Compliance as a measure of utilization. The 4 hr Compliance measure seems more appropriate for therapies like CPAP, in which utilization occurs for only a portion time in bed. Average Hours Use, on the other hand, is easier to calculate and better reflects the amount of time in which therapy reduces the total number of sleep-disordered breathing events and snoring. The agreement between these two compliance measures was substantially greater in those who used the therapy on average < 4 hr/night or ≥ 6 hr/night.
Like CPAP, the vast majority of patients who were noncompliant during the first 12 weeks of therapy were noncompliant long term (Lai et al., Citation2014). Average utilization of less than 5 hr per night during the initial 2 weeks and at 12 weeks were good predictors of those most likely to have poor long-term compliance. Unfortunately, it appears that, like most therapies, additional encouragement will be needed to ensure both initial and long-term compliance. Empowering the user to access and monitor treatment outcomes, similar to how one might track sleep with a consumer-wearable device, was presumed to have a positive impact on compliance. Our experience has been that more than half of those who purchase the device do not use the report portal. It’s unclear if this is due to a lack of interest, lack of education pertaining to the benefit of using the report, lack of positive reinforcement by the clinician, or difficulty using the Web-based software. Research is needed to determine if patient access to treatment outcomes has a similar positive impact on utilization as patient access to diagnostic information (Falcone, Damiani, Quaranta, Capozzolo, & Resta, Citation2014).
A previous positional therapy review suggested a degree of habituation and reduced effectiveness occurs over time (Joosten, O’Driscoll, Berger, & Hamilton, Citation2014). In this study, the repeated measures analysis suggested a slight trend toward increased responsiveness to the feedback resulted in less, rather than more, supine sleep. The number of supine attempts per night was essentially unchanged, with users attempting to sleep supine about five times per night no matter how long they had used the device. Seventy percent of users showed little change in behavior based on an average reduction of one supine attempt per night across 12 weeks of use. It appeared that the drive to sleep supine outweighs any unconscious training that might occur during sleep.
The observed consistency in the number of supine attempts per night, coupled with low time spent in the supine position, suggests that vibrotacile position-avoidance feedback did not lead to either habitation or adaption. This implies that vibrotactile devices should be used every night to avoid the sleeping position. There was not a clear association between an increased drive to sleep supine and frequency of feedback and compliance; however, within-groups variability may have masked this effect on some users.
The generalization of these findings, with respect to both short-term and long-term compliance, may be limited by this data set. Compliance rates were derived retrospectively from records that may have included only periodic use of the device when traveling, and included gaps in utilization unrelated to behavior (i.e., possible technical problems). Inclusion criteria requiring generation of a usability report may have positively influenced utilization rates. Those willing to generate a report to track therapy may indicate a more engaged and motivated patient that results in higher compliance. It is highly likely the device was recommended to the users by their physician (given the distribution channels used to market the device). Thus, compliance rates may have been positively influenced if the physician instructed the user to wear the device each night. Selection bias may have been introduced by the fact that users had disposable incomes sufficient to pay a currency equivalent of US$300–400 to obtain the device. These findings should also be interpreted with caution given the compliance assessment period extended beyond eight months in only half of the data set and the standard deviations for the behavioral measures were large. Another limitation of this data set was the inability to determine if age, body mass index, or supine or nonspine OSA severity influenced short- and long-term utilization in a manner similar to its affect on CPAP adherence (Collen, Lettieri, Kelly, & Roop, Citation2009; Kohler, Smith, Tippett, & Stradling, Citation2010). Further investigations are needed to evaluate the influence of overall and nonsupine OSA severity and the propensity to sleep supine prior to initiating positional therapy on short- and long-term compliance and adaptation. While vibrotactile positional feedback appears to be both safe (i.e., no adverse events reported) and effective, the influence of a neck-worn vs. a chest-worn design on compliance and behavior (i.e., location and comfort of the strap and body location where feedback is delivered) should also be evaluated.
Extending sleep restriction to include multiple positions during late-term pregnancy may be an application worth exploring. Significantly longer sleep times (Warland and Dorrian, Citation2014) and fewer stillbirths (Stacey et al., Citation2011) were observed when sleeping on the left side during late-term pregnancy. Despite the growing evidence of sleep-position related maternal cardiovascular compromise, time spent in nonoptimal sleep positions during late-term pregnancy reportedly exceeds 30% with substantial night to night variability (O’Brien & Warland, Citation2014; Warland & Dorrian, Citation2014). The findings from this study suggested the drive to sleep supine will be sufficiently strong that education-based behavior modification alone may be insufficient in reducing this risk. It could be argued that objective monitoring of late-term sleep position (with or without position restriction) would be clinically beneficial, given the relationship between sleep position and outcomes, and the substantial variability in self-reported sleep position accuracy (Warland & Dorrian, Citation2014).
CONCLUSIONS
As a significant proportion of people have more severe OSA and snoring when back-sleeping, devices to prevent or reduce supine sleep are important clinical tools. This study, which evaluates real-world experience with such a device, shows the following:
Compliance with prescribed therapy with the neck-based vibrotactile position feedback device is high.
There is no evidence that the effectiveness of the therapy in restricting position wears off over time.
There does not seem to be a behavioral or training effect, whereby the number of times a patient attempts to sleep supine diminishes over time.
User compliance does not seem to be significantly influenced by the frequency of vibrotactile feedback.
Sleep efficiency and amount of loud snoring measured by the device during therapy for each patient is unique but relatively consistent.
ACKNOWLEDGMENTS
The authors wish to recognize Bratislav Veljikovic, Elise Ramos, and Amy Mathews for their assistance with data preparation and Maja Stikic for her assistance with the statistical analyses.
REFERENCES
- Aloia, M. S., Arnedt, J. T., Strand, M., Millman, R. P., & Borrelli, B. (2013). Motivational enhancement to improve positive airway pressure in patients with obstructive sleep apnea: A randomized controlled trial. Sleep, 36, 1655–1662.
- Bignold, J. J., Deans-Costi, G., Goldsworthy, M. R., Robertson, C. A., McEvoy, D., Catcheside, P. G., and Mercer, J. D. (2009). Poor long-term compliance with the tennis ball technique for treating positional obstructive sleep apnea. Journal of Clinical Sleep Medicine, 5, 428–430.
- Bignold, J. J., Mercer, J. D., Antic, N. A., McEvoy, R. D., and Catcheside, P. G. (2011). Accurate position monitoring and improved supine-dependent obstructive sleep apnea with a new position recording and supine avoidance device. Journal of Clinical Sleep Medicine, 7, 376–383.
- Birrell, S. A., Young, M. S., and Weldon, A. M. (2013). Vibrotactile pedals: Provision of haptic feedback to support economical driving. Ergonomics, 56, 282–292.
- Collen, J., Lettieri, C., Kelly, C., & Roop, S. (2009). Clinical and polymsomnographic predictors of short-term continuous positive airway pressure compliance. Chest, 135, 704–709.
- Dantus, A. P., Winck, J. C., & Figueiredo-Braga, M. (2015). Adherence to APAP in obstructive sleep apnea syndrome: Effectiveness of a motivational intervention. Sleep and Breathing, 19, 327–334.
- Dieltjens, M., Vroegop, A. V., Verbruggen, A. E., Wouters, K., Willemen, M., De Backer, W. A., … Vanderveken, O. M. (2015). A promising concept of combination therapy for positional obstructive sleep apnea. Sleep and Breathing, 19, 637–644.
- Eijsvogel, M. M., Ubbink, R., Dekker, J., Oppersma, E., de Jongh, F. H., van der Palen, J., & Brusse-Keizer, M. G. (2015). Sleep position trainer versus tennis ball technique in positional obstructive sleep apnea syndrome. Journal of Clinical Sleep Medicine, 11, 139–147.
- Falcone, V. A., Damiani, M. F., Quaranta, V. N., Capozzolo, A., & Resta, O. (2014). Polysomnograph chart view by patients: A new educational strategy to improve CPAP adherence in sleep apnea therapy. Respiratory Care, 59, 193–198.
- Hermens, H., op den Akker, H., Tabak, M., Wijsman, J., & Vollenbroek, M. (2014). Personalized coaching system to support healthy behavior in people with chronic conditions. Journal of Electromyography and Kinesiology, 24, 815–826.
- Joho, S., Oda, Y., Hirai, T., and Inoue, H. (2010). Impact of sleeping position on central sleep apnea/Cheyne-Stokes respiration in patients with heart failure. Sleep Medicine, 11, 143–148.
- Jokic, R., Klimaszewski, A., Crossley, M., Sridhar, G., & Fitzpatrick, M. F. (1999). Positional treatment vs continuous positive airway pressure in patients with positional obstructive sleep apnea syndrome. Chest, 115, 771–781.
- Joosten, S. A., O’Driscoll, D. M., Berger, P. J., and Hamilton, G. S. (2014). Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Medicine Reviews, 18, 7–17.
- Kohler, M., Smith, D., Tippett, V., and Stradling, J. R. (2010). Predictors of long-term compliance with continuous positive airway pressure. Thorax, 65, 829–832.
- Lai, A. Y., Fong, D. Y., Lam, J.C., Weaver, T. E., & Ip, M. S. (2014). The efficacy of a brief motivational enhancement educational program on CPAP adherence in OSA: A randomized controlled trial. Chest, 146, 600–610.
- Lee, C. H., Kim, S. W., Han, K., Shin, J. M., Hong, S. L., Lee, J. E.,… Kim, J. W. (2011). Effect of uvulopalatopharyngoplasty on positional dependency in obstructive sleep apnea. Archives of Otolaryngology - Head and Neck Surgery, 37, 675–679.
- Levendowski, D. J., Seagraves, S., Popovic, D., and Westbrook, P. R. (2014). Assessment of a neck-based treatment and monitoring device for positional obstructive sleep apnea. Journal of Clinical Sleep Medicine, 10, 863–871.
- Levendowski, D. J., Veljkovic, B., Seagraves, S., & Westbrook, P. R. (2015). Capability of a neck worn device to measure sleep/wake, airway position, and differentiate benign snoring from obstructive sleep apnea. Journal of Clinical Monitoring and Computing, 29, 53–64.
- O’Brien, L. M., & Warland, J. (2014). Typical sleep positions in pregnant women. Early Human Development, 90, 315–317.
- Oksenberg, A. S. (2014). Positional therapy for sleep apnea: A promising behavioral therapeutic option still waiting for qualified studies. Sleep Medicine Reviews, 18, 3–5.
- Oksenberg, A., & Gadoth, N. (2014). Are we missing a simple treatment for most adult sleep apnea patients? The avoidance of the supine position. Journal of Sleep Research, 23, 204–210.
- Permut, I., Diaz-Abad, M., Chatila, W., Crocetti, J., Gaughan, J. P., D’Alonzo, G. E., & Krachman, S. L. (2010). Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. Journal of Clinical Sleep Medicine, 6, 238–243.
- Ravesloot, M. J. L., van Maanen, J. P., Dun, L., & de Vries, N. (2013). The undervalued potential of position therapy in position-dependent snoring and obstructive sleep apnea: A review of the literature. Sleep and Breathing, 17, 39–49.
- Ravesloot, M. J. L., Frank, M. H., Verhagen, E. A., de Lange, J., and de Vries, N. (2015). Positional OSA part 2: Restrospective cohort analysis with a new classification system (APOC). Sleep and Breathing. doi:10.1007/s11325-015-1206y
- Skinner, M. A., Kingshott, R. N., Filsell, S., & Taylor, D. R. (2008). Efficacy of the “tennis ball technique” versus nCPAP in the management of position-dependent obstructive sleep apnoea syndrome. Respirology, 13, 708–715.
- Stacey, T., Thompson, J. M., Mitchell, E. A., Ekeroma, A. J., Zuccollo, J. M., and McCowan, L. M. (2011). Association between maternal sleep practices and risk of late stillbirth: A case-control study. British Medical Journal, doi:10.1136/bmj.d33403
- Soll, B. A., Yeo, K. K., Davis, J. W., Seto, T. B., Schatz, I. J., and Shen, E. N. (2009). The effect of posture on Cheyne-Stokes respiration and hemodynamics in patients with heart failure. Sleep, 32, 1499–1506.
- van Maanen, J. P., Meester, K. A. W., Dun, L. N. Koutsourelakis, I., Witte, B. I., Laman, D. M., …de Vries, N. (2013). The sleep position trainer: A new treatment for positional obstructive sleep apnea. Sleep and Breathing, 17, 771–779.
- van Maanen, J. P., Richard, W., van Kesteren, E. R., Ravesloot, M. J., Laman, D. M., Hilgvoord, A. A., & de Vries, N. (2012). Evaluation of a new simple treatment for positional sleep apnoea patients. Journal of Sleep Research, 21, 332–339.
- van Maanen, J. P., & de Vries, N. (2014). Long-term effectiveness and compliance of positional therapy with the sleep position trainer in the treatment of positional obstructive sleep apnea syndrome. Sleep, 37, 1209–1215.
- Warland, J., & Dorrian, J. (2014). Accuracy of self-reported sleep position in late pregnancy. PLoS One, 9, e115760.

