Abstract
The Glittre ADL-test is based on important and common activities of daily living (ADLs), and it is an useful test to objectively distinguish patients with and without self-reported functional limitations. This study aims to analyze if difficulty to perform ADLs, as self-reported by patients with COPD, would reflect a worse Glittre ADL-test performance. In the first visit, patients were evaluated for clinical and nutritional status, spirometry, maximal cardiopulmonary exercise test on a treadmill. One week later, the patients performed two Glittre ADL-tests. Maximal voluntary ventilation (MVV) and the VEGlittre/MVV, VO2Glittre/VO2peak, and HRGlittre/HRpeak ratios were calculated to analyze the ventilatory, metabolic, and cardiac reserves. The London Chest Activity of Daily Living (LCADL) scale was only answered after the two Glittre ADL-test were performed. Patients were splited into two subgroups based on the anchor question of the LCADL: those with and those without self-reported ADL limitation. Sixty-two COPD patients were included (65.3 ± 8.6 years, FEV1 62 ± 22%pred). Those with ADL limitation (39 patients) completed the Glittre ADL-test with a significantly longer time (p = 0.002), as well as higher VEGlittre/MVV (p = 0.005) and lower oxygen pulse (p = 0.021) than those without ADL limitation. The time spent to perform the Glittre ADL-test was significantly associated with total LCADL score (ρ = 0.327, p < 0.05). A cutoff of 253 s was able to distinguish those patients without and with ADL limitation. COPD patients who self-reported ADL limitation according to the LCADL scale took a longer time to perform the Glittre ADL-test with higher VEGlittre/MVV and lower oxygen pulse than those without ADL limitation.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities [Citation1]. During the course of the disease, patients with COPD experience a progressive reduction in the ability to perform activities of daily living (ADLs) [Citation2]. Several studies have shown that limitation of functional capacity is a better predictor of disability and mortality in COPD subjects than airflow limitation [Citation3–5]. Therefore, in these subjects, an adequate evaluation of functional status should be prioritized.
According to Dechman et al. [Citation6], there are two primary methods of assessing functional status, questionnaires and performance-based tests. Self-perceived performance of impaired ADLs can be measured using patient-reported questionnaires that show good validity for measuring problematic ADLs [Citation7] but does not identify the physiological variables that may be influencing performance in their ADLs. In addition, self-reported questionnaires can be influenced by psychological factors, cognitive alterations, or adoption of a sedentary lifestyle, which can lead the patient to report a level of functional capacity that does not provide an accurate estimate of their functional limitation [Citation8]. On the other hand, apart from the performance-based tests that provide objective information of the different physiological mechanisms involved in exercising, they are not very practical for use in clinical practice [Citation9].
In 2006, Skumlien et al. [Citation10] proposed a test that involved five common ADLs in order to address the need for a more representative and objective assessment of function in people with COPD, named the Glittre ADL-test. The validity of the test was tested by the authors by comparing ADL-time with the distance walked in 6 min, the lung function variables, and the results from specific health-related quality of life questionnaires. Moreover, it has been shown that Glittre ADL-test is able to differentiate the functional capacity of people with COPD from healthy individuals [Citation11].
Despite the Glittre ADL-test was developed based on both the London Chest Activity Daily Living (LCADL) [Citation6,Citation12] and the Modified Pulmonary Functional Status and Dyspnea Questionnaire [Citation13], they have never been tested directly in patients with COPD. Furthermore, it has not been shown if difficulty to perform ADLs, as self-reported by people with COPD, would reflect a worse Glittre ADL-test performance. Therefore, the purpose of this study was to analyze whether patients with COPD who self-report limitation to accomplish ADLs due to dyspnea have a worse performance in the Glittre ADL-test than those who do not report this limitation. We hypothesized that self-reported limitation due to dyspnea would be reflected in the Glittre ADL-test performance.
Materials and methods
A prospective cross-sectional study was carried out at the Pulmonary Rehabilitation Center of Escola Paulista de Medicina (Brazil) and conducted according to the World Medical Association Declaration of Helsinki. The study was approved by the Institutional Review Board of the Escola Paulista de Medicina (registration number: 0938/10) and all patients signed an informed consent.
Inclusion criteria
Patients with COPD classified according to the GOLD spirometric criteria [Citation1]; with no episodes of exacerbation in the previous 4 weeks; ≥40 years of age, and have not done pulmonary rehabilitation program in the last 2 years.
Exclusion criteria
Hypoxemia at rest (pulse oxygen saturation [SpO2] < 88%); unstable cardiovascular disease; musculoskeletal, neurological or rheumatic disease that could limit the ability to participate in the physical tests.
Evaluation protocol
Data collection was carried out over the course of two visits within a week interval. During the first visit, patients were evaluated for clinical and nutritional status, spirometry test, and carried out a maximal cardiopulmonary exercise test (CPET). During the second visit, two Glittre ADL-tests were carried out according to Skumlien et al. [Citation10]. The best Glittre ADL-test result was taken for analysis. All tests were performed by the same experienced physiotherapists. Patients with COPD were invited to participate in the study before the researchers knew their ADLs limitation and, in order to avoid any selection bias, the LCADL was answered only after they had performed the two Glittre ADL-test and interpreted by a blinded researcher.
Spirometry
Pulmonary function was assessed according to the ATS/ERS reccomendations [Citation14], using a portable ultrasound-based spirometer (EasyOne®, by NDD Medical Technologies, Andover, MA). Forced vital capacity (FVC) and forced expiratory volume in the first second (FEV1) values obtained were compared with absolute and percentage of predicted values for the Brazilian population [Citation15].
Glittre ADL-test
The test, as described by Skumlien et al. [Citation10], started with the patients seated on a chair. At a starting signal, they stood up and then walked 5 m, crossed over an interposed two-step staircase, walked another 5 m up to a two shelves equipment that was adjusted individually according to shoulder and waist height of each subject. Three bags weighing 1 kg each positioned on the top shelf had to be moved one by one to the bottom shelf, down to the floor, back to the bottom shelf, and finally to the top shelf again. The participants then walked back to the initial chair where they started from, crossed over the two-step stairs, sat down, and immediately started the next lap by rising up again. All participants were asked to complete five laps as quickly as possible. They were allowed to rest if necessary but were told to resume activity as soon as they could. In this case, the chronometer was not stopped. The patients carried a backpack containing 2.5 kg (women) or 5.0 kg (men). Each step of the stair was 17 cm high and 27 cm deep.
Maximal cardiopulmonary exercise test
The test was performed on a treadmill (Cybex Q35 Controlled Impact, Medway, MA) according to the modified Balke protocol [Citation16], in order to evaluate at which proportion of the maximal ventilatory and metabolic rates the Glittre ADL-test was performed. The procedure started with the patient walking on the treadmill at a fixed speed, without any inclination for the first 3 min, followed by a 1% inclination increment at the end of each following minute. The participants were encouraged to continue the exercise until exhaustion but it could be immediately interrupted in case of presenting accepted criteria for exercise termination before symptom limitation according to the ATS/ACCP statement [Citation16].
Outcome measures in the exercise tests
During both exercise tests, the Glittre ADL-test and CPET, the following variables were evaluated in a breath-by-breath mode using a portable device (K4b2Cosmed®, Rome, Italy) and a silicon mask firmly adjusted to the patients face: exercise time, oxygen uptake (VO2), carbon dioxide production (VCO2), tidal volume (VT), respiratory rate (RR), minute ventilation (VE), heart rate (HR), oxygen pulse (VO2/HR). SpO2 was measured using a pulse oximeter (920 M, Healthdyne Technologies, Marietta, USA), and dyspnea (assessed through Borg score [Citation17]) were evaluated at rest and at the end of both Glittre ADL and CPET tests.
The VO2Glittre was considered as the highest value reached at the end of Glittre ADL-test, and the VO2peak was considered as the highest value reached at the end of the CPET; VO2Glittre/VO2peak ratio was used to analyze the metabolic reserve. The VEGlittre was considered as the highest value reached at the end of Glittre ADL-test, and maximal voluntary ventilation (MVV) was calculated as the product of FEV1 times 37.5 [Citation16]; the VE/MVV ratio was used to analyze the ventilatory reserve. The HRGlittre was considered as the highest value reached at the end of Glittre ADL-test, and the HRpeak was considered as the highest value at the end of the CPET; HRGlittre/HRpeak ratio was used to analyze the cardiac reserve.
Questionnaires
The LCADL scale [Citation12] is a questionnaire that evaluates dyspnea in 15 different items of ADL, divided into four domains: personal care (4 items), home care (6 items), physical activity (2 items), and leisure (3 items). The patient selects how much dyspnea interferes in these 15 areas of ADL by selecting a number from a scale of 0 to 5. A sub-score is also calculated for each domain, and the total score is calculated by adding the sub-scores of the four domains. The highest score that may be reached is 75 and the higher the score the worse is the limitation to perform the ADL.
The questionnaire also includes an anchor question, which indicates to which extent breathing interferes with the individual in their daily life; the answers can be (a) “significantly”, (b) “a little bit”, or (c) “does not interfere”. The answers were grouped in “with limitation” for the ones that answered” significantly” and “a little bit”, and “without limitation “for the ones that answered “does not interfere”.
Statistical analysis
To statistical analysis, participants were split into two groups based on the anchor question of the LCADL scale: those whose ADLs were limited (patients who reported at least a slightly loss in performing ADLs due to dyspnea) and those whose ADLs were not limited (patients who declared having no ADLs impairments relating to dyspnea). For sample size calculation, the time spent on Glittre ADL-test was assessed in a pilot study conducted with 10 patients with COPD: five with self-reported limitations (298.4 ± 57.68 s) and five without self-reported limitations (231.2 ± 53.11 s). With an effect-size d of 1.21, an alpha error of 0.01 and a statistical power of 90%, a total sample of 44 patients (22 in each group) was estimated for this study.
Data normality was verified using the Shapiro–Wilk test. The unpaired t test or Mann–Whitney test was used to compare differences between anthropometric, pulmonary function and physiological variables obtained in the exercise tests as well as questionnaire scores. Chi-squared test was used to compare variables presented in proportions. Correlation between time spent on Glittre ADL and LCADL score was evaluated using the Spearman’s rho (ρ) correlation coefficient. In order to study if the anchor question was able to discriminate between those participants with- and without self-reported ADL limitation, the area under the ROC curve (AUC) and its 95% confidence interval were computed and the optimal cutoff point was calculated according to the Youden index [Citation18].
In order to avoid type II error, effect-sizes between subgroups (Cohen’s d) were calculated using the G*Power software (version 3.1.9.2, Kiel, Germany) and interpreted as small (<0.50), moderate (between 0.50 and 0.80), and large (>0.80) [Citation19]. Inferential data analysis was performed in Statistical Package for Social Sciences® version 20. The level of significance was set at p < 0.05 (two-sided) for all statistical analyses.
Results
Sixty-two patients with COPD participated in the study. Of these, 23 reported no ADLs limitation due to dyspnea [11 were classified as GOLD I (48%), 8 were GOLD II (35%) and 4 were GOLD III (17%)], while 39 patients reported having limitation on their ADLs due to dyspnea [9 were GOLD I (23%), 14 were GOLD II (36%) and 16 were GOLD III (41%)]. Chi squared found no significant differences regarding the proportion of participants in each GOLD classification. Those who reported ADLs limitation presented significantly lower FEV1(L) (p < 0.001, Cohen’s d = 0.98), FEV1(%pred) (p < 0.001, Cohen’s d = 0.79), FVC(L) (p = 0.024, Cohen’s d = 0.69), FEV1/FVC (p < 0.001, Cohen’s d = 1.0) and MVV values (p = 0.005, Cohen’s d = 0.57) when compared to those without ADL limitation ().
Table 1. General characteristics of patients with COPD included in the study.
Regarding those variables obtained during the Glittre ADL-test, no difference was observed between groups when assessed at rest (). However, the group with ADL limitation completed the Glittre ADL-test with a significantly longer time (p = 0.002, Cohen’s d = 0.82) when compared with the group without ADL limitation. Additionally, a significantly lower SpO2Glittre (p = 0.017, Cohen’s d = 0.67), and lower VO2/HR (p = 0.021, Cohen’s d = 0.42), and higher VEGlittre/MVV (p = 0.005, Cohen’s d = 0.61) were observed in the group with ADL limitation (). There was no significant difference between groups regarding VO2peak of the Glittre ADL-test and VO2Glittre/VO2peak ratio of both groups.
Table 2. Variables obtained in patients with COPD at rest and peak of Glittre ADL-test.
As shown in , patients with ADL limitation presented significantly higher total LCADL scores (all p < 0.001) when compared with those without ADL limitation. Regarding the LCADL questionnaire, COPD patients reported more perception of dyspnea during their home care activities (9.4%) followed by personal care (6.8%). Regarding relationship, the time spent on Glittre ADL-test was significantly associated with total LCADL score (ρ = 0.327, p = 0.009) (). ROC curve showed an area under the curve of 0.725 (p < 0.001) with a 95% confidence interval of 0.596 to 0.830. According to the Youden index, a cutoff point for the Glittre ADL-test of 253 s (sensitivity of 77.49% and specificity of 56.52%) was able to distinguish those COPD patients without and with ADL limitation based on the anchor question of the LCADL questionnaire ().
Figure 1. Correlation between the Glittre ADL-time and total score of the London Chest ADL (LCADL) scale in people with COPD.
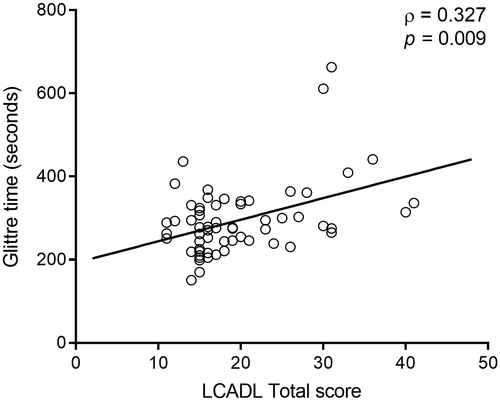
Figure 2. Receiver operating characteristic curve of the anchor question of the London Chest ADL questionnaire and Glittre-ADL time. Arrow indicates the cutoff point. AUC: Area under curve; %: percentage; s: seconds.
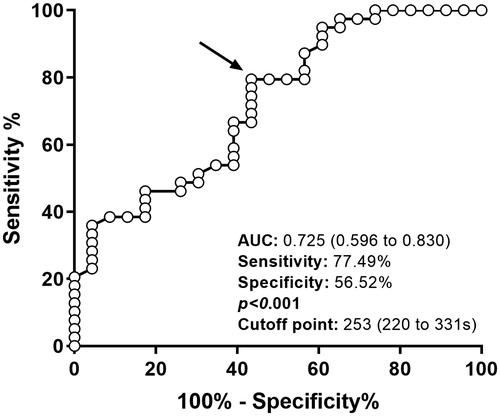
Table 3. LCADL scores of patients with COPD included in the study.
Discussion
The main finding of this study was that patients with COPD who self-report ADLs limitations due to dyspnea, according to the LCADL questionnaire, took a longer time to complete the Glittre ADL-test than those without self-reported limitation; they also presented a higher VE/MVV ratio at the end of the test showing that ventilatory limitation is an important limiting factor to the functional performance in this population. However, lower oxygen pulse in those who self-reported limitations could also suggest that cardiac impairment may have contributed for the limitation of these patients.
Dyspnea in patients with COPD when performing ADLs is a very frequent complaint and it should always exhaustedly investigated. Functional tests such as the Six-minute Walk Test and the Glitter ADL-test are interesting to be used as they allow us to objectively test the patients in routine activities and to compare groups from different centers and different severities. However, these tests may not always be applied to an individual patient, either due to the impossibility of carrying out the test in that particular outpatient clinics or by comparing a single result due to the large variability these tests show in a group of patients. In this sense, by simply questioning patients with COPD how much dyspnea limits their ADLs may give a good indication of how much a patient needs pharmacological and rehabilitation treatment, however such questioning and its association to a test that specifically evaluates the ADL performance such as the Glittre ADL-test has never been demonstrated.
The group self-reporting ADLs limitation took on average one minute longer to complete the Glittre ADL-test than the group without ADLs limitation, a time similar to the minimal important difference in Glittre ADL-time as suggested by Skumlien et al. [Citation10] Recently, a minimal important difference value of 23 s was established for the Glittre ADL-test based on the improvement of 30 meters in the six-minute walk test after 24 sessions of pulmonary rehabilitation with COPD patients [Citation20]. In our study, a cutoff point of 253 s (4.2 min) for the Glittre ADL-time was able to distinguish those patients with COPD without and with self-reported limitation to perform ADL. Establishing performance markers for a test can help the health care professionals in determining therapeutic goals for the patients. In our study, we sought to value the patient’s self-reported functional limitation as this information is easier to be obtained and it is an obligatory questioning during a patient examination in clinical practice.
The group with ADL self-reported limitation had higher VEGlittre/MVV ratio, which resulted in more dyspnea at the end of the Glittre ADL-test, showing the importance that ventilatory reserve has on the functional limitation of these patients. Pitta et al. [Citation21] had already demonstrated that the best parameter associated with total daily energy expenditure, number of steps, and time taken to carry out moderate and vigorous activities in patients with mild to very severe COPD was the MVV. As observed in our study, this parameter also interferes in carrying out simple ADLs. Pitta et al. [Citation21] included very severe patients in their study, which may have biased their response, while our study did not include very severe patients, making our finding more relevant.
Our results showed no difference in the metabolic reserve between the two groups. This result differs from those by Castro et al. [Citation22] and Vaes et al. [Citation23], which showed that as the COPD patients increase the severity of their disease they show a progressive decrease in their metabolic reserve during the performance of ADLs. Similar results were found by Souza et al. [Citation24] while analyzing the physiological requirements to perform the Glittre ADL-test in mild-to-severe COPD patients. However, contrary to Castro et al. [Citation22] and Vaes et al. [Citation23] in our study patients were grouped according to their ADL-limitation and not by their airflow limitation severity. Thus our two groups included patients with different levels of airflow obstruction balancing out the energy cost what may explain the difference between these studies. Our results also suggest that bronchial obstruction degree is not a marker of ADL limitation.
At the end of the Glittre ADL-test, the group with ADL limitation also had lower oxygen pulse than the group without ADL limitation. Functional limitation in COPD patients is multifactorial, including a certain degree of ventilatory limitation, cardiac output, systemic oxygen delivery, and disorders relating to the availability of oxygen to the quadriceps muscle [Citation25]. Thus, we believe that the lower oxygen pulse in this group may reflect the presence of a cardiac component limiting our patients’ abilities to perform the Glittre ADL-test and maybe the more intense ADLs.
In our study, in order to assess dyspnea during ADLs, we chose the LCADL because it was drawn up specifically to evaluate the difficulty of patients with COPD in performing the ADLs. This scale presents an anchor question, the same that allowed us to divide the patients into two groups, that is based on the presence or not of ADL limitations due to dyspnea. The LCADL questions include activities that patients are required to do in their daily lives and represent basic functional requirements [Citation26]. Weak correlations were found between Glittre ADL-time and total score of the LCADL showing that factors others than physical reasons are responsible for the symptom of dyspnea in patients with COPD. However, the LCADL scale was mainly developed to assess dyspnea in patients with severe COPD [Citation12], and as our sample was made up of patients with different degrees of severity, this may have influenced the intensity of the association between the Glittre ADL-time and the total of the LCADL score.
It is worth to mention that the response to the LCADL anchor question is subjective and is dependent on the patient’s definition of their “normal” daily activities. Someone that is normally very sedentary might say they have no limitation just because they do very little, while someone that is normally very active (but in better health than the sedentary patient) would say that their breathing is limiting them because in their daily life they push themselves to do more. Our study did not include a control group of healthy individuals paired by age since our objective was only to compare the performance of the Glittre ADL-test between patients with COPD with and without self-reported limitation to perform ADLs. The study also did not include very severe COPD patients, so our results cannot be extended to this group of patients. There was a slight diffrence in the number of patients between the two groups but both reached the minimal calculated sample size. The study was adequately powered, and we showed that self-reported ADL-limitation by COPD patients could be objectively identified by the Glittre ADL-test. The Glittre ADL-test provides an objective measurement of functional limitation, allowing healthcare providers to more effectively plan interventions that can benefit patients. However when the test cannot be performed, the simple questioning about dyspnea can also provides the health care team a very useful information. So far this association had not been shown.
Conclusions
Patients with COPD who self-report limitation to perform ADL in the LCADL scale take a longer time to perform the Glittre ADL-test with higher VEGlittre/MVV and lower oxygen pulse than those who report no limitation. Questioning about self-reported functional limitation is an obligatory evaluation when examining a patient and should always be taken into account when evaluating patients with COPD.
Acknowledgments
We thank the multidisciplinary team from the Pulmonary Rehabilitation Center of Escola Paulista de Medicina of Federal University of São Paulo, Brazil.
Disclosure statement
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Update of the GOLD-recommendations. https://goldcopd.org. Published 2019. Accessed June 17, 2019. https://goldcopd.org2019 [cited 2019 June 17].
- Kapella MC, Larson JL, Covey MK, et al. Functional performance in chronic obstructive pulmonary disease declines with time. Med Sci Sports Exerc. 2011;43(2):218–224. doi:10.1249/MSS.0b013e3181eb6024.
- Fan VS, Ramsey SD, Make BJ, et al. Physiologic variables and functional status independently predict COPD hospitalizations and emergency department visits in patients with severe COPD. COPD 2007;4(1):29–39. doi:10.1080/15412550601169430.
- Pitta F, Troosters T, Probst VS, et al. Physical activity and hospitalization for exacerbation of COPD. Chest 2006;129(3):536–544. doi:10.1378/chest.129.3.536.
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax 2006;61(9):772–778. doi:10.1136/thx.2006.060145.
- Dechman G, Scherer SA. Outcome measures in cardiopulmonary physical therapy: focus on the glittre ADL-test for people with chronic obstructive pulmonary disease. Cardiopulm Phys Ther J. 2008;19(4):115–118. doi:10.1097/01823246-200819040-00003.
- Stull DE, Leidy NK, Jones PW, et al. Measuring functional performance in patients with COPD: a discussion of patient-reported outcome measures. Curr Med Res Opin. 2007;23(11):2655–2665. doi:10.1185/030079907X233133.
- Reardon JZ, Lareau SC, ZuWallack R. Functional status and quality of life in chronic obstructive pulmonary disease. Am J Med. 2006;119(10):32–37. doi:10.1016/j.amjmed.2006.08.005.
- Kocks JW, Asijee GM, Tsiligianni IG, et al. Functional status measurement in COPD: a review of available methods and their feasibility in primary care. Prim Care Respir J. 2011;20(3):269–275. doi:10.4104/pcrj.2011.00031.
- Skumlien S, Hagelund T, Bjortuft O, et al. A field test of functional status as performance of activities of daily living in COPD patients. Respir Med. 2006;100(2):316–323. doi:10.1016/j.rmed.2005.04.022.
- Correa KS, Karloh M, Martins LQ, et al. Can the Glittre ADL test differentiate the functional capacity of COPD patients from that of healthy subjects? Rev Bras Fisioter. 2011;15(6):467–473. doi:10.1590/S1413-35552011005000034.
- Garrod R, Bestall JC, Paul EA, et al. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL). Respir Med. 2000;94(6):589–596. doi:10.1053/rmed.2000.0786.
- Lareau SC, Meek PM, Roos PJ. Development and testing of the modified version of the pulmonary functional status and dyspnea questionnaire (PFSDQ-M). Heart Lung J Crit Care. 1998;27(3):159–168. doi:10.1016/S0147-9563(98)90003-6.
- American Thoracic Society/European Respiratory S. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624.
- Pereira CA, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397–406. doi:10.1590/S1806-37132007000400008.
- American Thoracic Society, American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–277.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381.
- Youden WJ. Index for rating diagnostic tests. Cancer 1950;Jan3(1):32–35. doi:10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1998.
- Gulart AA, Araujo CLP, Munari AB, et al. The minimal important difference for Glittre-ADL test in patients with chronic obstructive pulmonary disease: minimal important difference for Glittre-ADL test. Braz J Phys Ther. 2018.
- Pitta F, Takaki MY, Oliveira NH, et al. Relationship between pulmonary function and physical activity in daily life in patients with COPD. Respir Med. 2008;102(8):1203–1207. doi:10.1016/j.rmed.2008.03.004.
- Castro AA, Porto EF, Iamonti VC, et al. Oxygen and ventilatory output during several activities of daily living performed by COPD patients stratified according to disease severity. PloS One. 2013;8(11):e79727. doi:10.1371/journal.pone.0079727.
- Vaes AW, Wouters EFM, Franssen FME, et al. Task-related oxygen uptake during domestic activities of daily life in patients with COPD and healthy elderly subjects. Chest 2011;140(4):970–979. doi:10.1378/chest.10-3005.
- Souza GF, Moreira GL, Tufanin A, et al. Physiological Requirements to Perform the Glittre Activities of Daily Living Test by Subjects With Mild-to-Severe COPD. Respir Care. 2017;62(8):1049–1057. doi:10.4187/respcare.05113.
- Louvaris Z, Kortianou EA, Spetsioti S, et al. Intensity of daily physical activity is associated with central hemodynamic and leg muscle oxygen availability in COPD. J Appl Physiol. 2013;115(6):794–802. doi:10.1152/japplphysiol.00379.2013.
- Carpes MF, Mayer AF, Simon KM, et al. The Brazilian Portuguese version of the London Chest Activity of Daily Living scale for use in patients with chronic obstructive pulmonary disease. J Bras Pneumol. 2008;34(3):143–151. doi:10.1590/S1806-37132008000300004.
