Abstract
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) ABCD classification tool has been used to assess the symptom burden and exacerbation risk of patients with chronic obstructive pulmonary disease (COPD). An area requiring further exploration is the relationship between the GOLD classification's basic components and the measurements acquired by Sit-to-Stand tests (STST). We aimed to study the relationship between STST and the component of the GOLD classification tool. This study was conducted on a sample of 42 COPD subjects with patient history, COPD assessment test (CAT) and spirometry. 5STST performance time and the number 30s-STST repetitions showed differences of statistical significance in COPD subjects considered to be more symptomatic and in subjects with high risk of future exacerbations. Both STSTs correlated significantly with forced expiratory volume in one second % predicted (FEV1%), CAT, number of acute exacerbations in the past year and number of hospitalized exacerbations in the past year. STST performance correlates significantly with items of the CAT questionnaire that assess breathlessness, limitation of activities, confidence and lack of energy. Using multivariate analysis, age, FEV1% and CAT score manifested the strongest negative association with STST performance. 5STST performance time and the number 30s-STST repetitions in COPD patients correlates with the level of symptoms and the risk of future exacerbations that define groups A-D based on GOLD 2018 classification tool (at the time of data acquisition). The correlation of STST performance with CAT score involves specific items of the questionnaire that assess breathlessness, limitation of activities, confidence and lack of energy.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major global health issue [Citation1]. The “ABCD” assessment tool of the updated version of 2011 Global Initiative for Chronic Obstructive Lung Disease (GOLD) introduced crucial changes to the stratification of COPD patients [Citation2] incorporating a combined assessment of spirometry with symptom burden and risk of exacerbation. The refined ABCD assessment tool separated spirometric grades (1 to 4) from the “ABCD” groups. Thus, the GOLD 2018 assessment (used at the time of data collection) classifies patients into groups A–D which are derived exclusively from patient symptoms and their history of exacerbation and can be used to guide initial therapy [Citation2]. A comprehensive measure of symptoms and health status impairment in COPD can be offered by the COPD Assessment Test (CAT), which is a validated disease-specific health status questionnaire [Citation2–4]. Eight items are included in CAT (cough, phlegm, chest tightness, breathlessness, limited activities, confidence leaving home, sleeplessness and lack of energy) [Citation3]. The score ranges from 0 to 40, while according to the GOLD 2018 report a CAT score of 10 points or higher classifies patients with COPD as highly symptomatic [Citation2]. A history of earlier treated COPD exacerbations (defined as two or more exacerbations per year) or hospitalization for an exacerbation are used as predictors associated with increased risk of future events and death [Citation2].
A fundamental aspect of COPD management includes an evaluation of exercise performance [Citation5]. Severe exacerbations lead to reduced muscle strength [Citation6] and exercise capacity [Citation7]. Most importantly, the reduction of exercise capacity can predict re-hospitalization and survival in COPD patients [Citation8,Citation9], and is not recovered, even after improvement in the patients’ lung function [Citation7]. The Sit-to-Stand test (STST) is a simple test of lower limb function with minimal requirements in respect to time and equipment. It was first described in the literature in 1985 [Citation10]. Variations of the STST have been validated in stable COPD ranging from 5 repetitions [Citation11] or 30s [Citation12] to the 1 min test [Citation13,Citation14]. STST have been shown to correlate significantly with the 6 min walk test (6MWT), St George’s Respiratory Questionnaire (SGRQ), CAT, the Medical Research Council Dyspnea scale (mMRC) and validated COPD prognostic indices (iBODE and ADO) [Citation11,Citation14,Citation15]. Nevertheless, little attention has been given to STST data in relation to the components of GOLD classification provided by the ABCD assessment tool.
Therefore, the aim of this study was to determine whether the performance during STST of COPD patients is associated with the components of GOLD classification, namely the CAT and the history of previous exacerbations and hospitalizations. The CAT score was chosen because of its multi-dimensional nature in contrast to mMRC scale that is a quantitative assessment tool only for breathlessness. In addition, this study aimed to evaluate the impact of the respiratory and non-respiratory CAT item scores on the STST performance.
Methods
The present cross-sectional study was approved by the Institutional Ethics Committee of a Greek tertiary hospital. At the time of recruitment an informed, written consent was obtained by all study participants. This study is fully compliant with the tenets of the WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects.
Study participants
The study included eligible subjects with a clinical diagnosis of COPD who were recruited from the Outpatient Department of the pulmonary clinic of a tertiary general hospital from January 2018 through May 2018. Inclusion criteria were a previous COPD diagnosis, age of 40–80 years and no history of asthma or any other lung diseases. All subjects had been clinically stable for at least 4 weeks. The exclusion criteria included unstable cardiac conditions within 4 months prior to the study, active cancer, severe concomitant renal failure, cognitive deterioration, or inability to ambulate. Thus, patients with severe musculoskeletal and neurological limitations were excluded.
Measures
At baseline, basic demographic data were obtained with a structured clinical history and physical examination. Weight and height were measured and Body Mass Index (BMI) was calculated with a calibrated scale and stadiometer. Recorded data included age, sex, lung function test results, number of acute exacerbations in the past year and number of hospitalized exacerbations in the past year. Whenever possible patient reports were verified with medical records. Symptoms were evaluated according to the CAT [Citation3]. “Cough”, “phlegm”, “chest tightness”, “breathlessness” were defined as respiratory items. Based on the individualized ABCD tool for the assessment of symptoms and exacerbation risk [Citation2], COPD patients in this study were classified into group A, B, C or D. Briefly, patients in groups A and C have less symptoms (CAT <10), while patients in groups B and D have more symptoms (CAT ≥10). Groups A and B are characterized by 0 or 1 exacerbations that do not lead to hospital admission while groups C and D feature two exacerbations per year or one that leads to hospital admission. Pulmonary function testing (PFT) was performed in a sitting position following the guidelines of the American Thoracic Society and the European Respiratory Society [Citation16]. Flow-volume spirometry was assessed and forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and FEV1/FVC were recorded. COPD diagnosis required an FEV1/FVC ratio less than 70% [Citation2] or less than the lower limit of normal [Citation17].
Subsequently, subjects performed the physical performance tests in a specific order. First, each patient performed the 30s sit-to-stand test (30s-STST) and afterwards the five-repetition sit-to-stand test (5STST). All maneuvers were performed in a chair without an armrest with a height of 43 cm with an interval of 2 h between each test. During the tests, heart rate, oxygen saturation, and blood pressure were measured. For the 30s-STST the subject starts the test seated in the middle of the chair, arms crossed by the wrists placed against the chest. Subjects were instructed to stand up from and sit down on the chair with no support from the hands, repeating the procedure as many times as possible within 30 sec [Citation18,Citation19]. For the 5STST, we measured the time taken to complete five repetitions of the sit-to-stand maneuver was measured [Citation11]. This test required participants to stand up from and sit down on a 43 cm high armless chair as quickly as possible 5 times. Timing began when the subject’s back left the backrest and stopped once the back touched the backrest for the fifth time. The minimum clinically important differences for 30s-STST and 5STST have been previously estimated as at least 2 repetitions and 1.7 s, respectively in COPD patients [Citation11,Citation20].
Statistical analysis
Statistical analysis of the data was carried out using the statistical software SPSS version 21.0 (SPSS, Inc., Chicago, IL, USA). Frequencies for categorical variables, and mean values and Standard Deviation (SD) for continuous variables were calculated. Assumption of the normal distribution of continuous variables was assessed by the Kolgomorov–Smirnov test. Comparisons of discrete variables were performed with a chi-squared test of contingency tables. The comparison of means of continuous quantitative variables was performed by the Student’s t-test for variables normally distributed and the unpaired-samples Mann–Whitney rank-sum test for nonparametric ones. Spearman’s correlation coefficient (ρ) was used to assess the possibility and quantify the linear association between STST measurements and other variables. Finally, multivariate linear regression analyses were performed to evaluate the relationship between STST measurements as dependent variables that correlated significantly with STST measurements as independent variables combined in a multivariate model of interest. In all analyses, a two-sided P value less than 0.05 was considered statistically significant.
Results
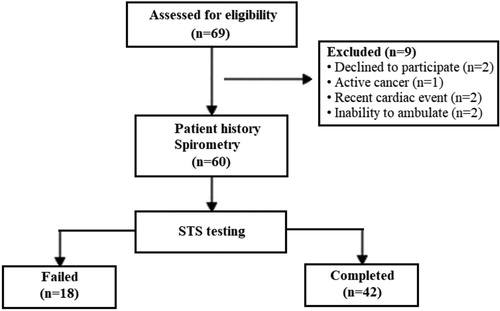
Initial screening identified and recruited 60 eligible subjects for the study (). Their demographic and clinical characteristics are summarized in . However, 18 subjects were unable to perform the initial STST manoeuvre or assistance was necessary and thus the testing was terminated. There were no recorded failures of patients completing the 30s-STST but failing the 5STST. The percentage of GOLD group D was significantly higher among individuals who could not perform the STST (61% vs 28.5%) compared with subjects that completed the tests and were analyzed further. Furthermore, subjects unable to perform the STST manoeuvres were characterized by a significantly higher CAT score and significantly more COPD exacerbations and hospitalizations in the past year ().
Table 1. Patients characteristics and comparison between groups of patients who completed or failed to complete the sit-to-stand tests (5STST and 30s-STST).
Forty-two subjects completed both STSTs and were included in the subsequent analysis. The mean age of the study population was 62.7 ± 12.8 years, 52.8% of which were male. The mean 5STST performance time was 13.1 ± 3.79 s. A significant negative correlation was observed between 5STST time and the number of 30s-STST repetitions (ρ = −0.929, ρ < 0.001). The 30s-STST mean repetitions were 12.85 ± 5.08. The mean values of STST performance in different GOLD groups are summarized in . As it is shown in , COPD patients that were less symptomatic performed better during the 30s-STST (17 ± 7 repetitions vs 11.5 ± 3 repetitions, p < 0.05). Furthermore, the number of 30s-STST repetitions was significantly higher in subjects with low risk of future COPD exacerbations (14 ± 5 repetitions vs 11 ± 4 repetitions, p < 0.01). Likewise, the time to perform the 5STST test was significantly higher in subjects with a high risk of future COPD exacerbations (15.5 ± 3.1 sec vs 11.8 ± 3.5 sec, p < 0.01).
Table 2. Comparison of sit-to-stand (5STST and 30s-STST) measurements between patients with fewer and more symptoms and between patients with low and high risk of future exacerbations.
The correlation analysis of measurements during STST maneuvers with clinical and spirometric parameters is presented in . The number of 30s-STST repetitions correlated negatively with age (ρ = −0.309, Ρ < 0.05) and CAT score (ρ = −0.478, Ρ < 0.01) and positively with predicted FEV1% values (ρ = 0.419, Ρ < 0.01). Similarly, the time to perform the 5STST test correlated positively with age (ρ = 0.334, Ρ < 0.05) and CAT score (ρ = 0.318, Ρ < 0.05) and negatively with predicted FEV1% values (ρ = −0.497, Ρ < 0.01). However, only the time to perform the 5STST maneuvers presented a significant positive correlation with the number of COPD exacerbations (ρ = 0.421, Ρ < 0.01) and relevant hospitalizations (ρ = 0.321, Ρ < 0.05) during the last year. depicts the correlation of CAT with both the number of stands during the 30s-STST and the time to perform 5STST. The relationship between STST measurements and indices that correlated significantly with STST measurements was further tested in two multivariate models. The results of linear regression analysis are presented in and . CAT score, FEV1% predicted and age manifested the strongest association with time to perform the 5STST. CAT score and age were the strongest predictors of the number of repetitions achieved during the 30s-STST.
Figure 2. Correlation between COPD assessment test (CAT) and (A) the time to perform 5STST, and (B) the number of stands during 30s-STST.
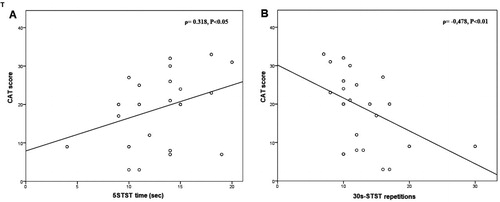
Table 3. Spearman rank correlation of sit-to-stand tests (5STST and 30s-STST) with various clinical and spirometric parameters.
Table 4. Results of multivariate linear regression analysis of the association of the time to complete the 5STST with multiple predictors.
Table 5. Results of multivariate linear regression analysis of the association of the repetitions of the sit-to-stand maneuver completed in the 30s-STST with multiple predictors.
The correlation analysis of STST performance with the eight items included in CAT questionnaire is presented in . As it is shown in , breathlessness (item 4) is the only respiratory item that correlates significantly both with the number of 30s-STST repetitions (ρ = −0.511, Ρ < 0.01) and the time to perform the 5STST test (ρ = 0.508, Ρ < 0.01). Performance in the 30s-STST also correlated negatively with the non-respiratory CAT items 5, 6 and 8, namely, limitation of activities (ρ = −0.427, Ρ < 0.01), lack of confidence (ρ = −0.510, Ρ < 0.01) and lack of energy (ρ= −0.442, Ρ < 0.01). A similar, but positive, the correlation was observed between the time to perform 5STST and the non-respiratory CAT items limitation of activities (ρ = 0.338, Ρ < 0.05), lack of confidence (ρ = 0.321, Ρ < 0.05) and lack of energy (ρ = 0.360, Ρ < 0.05). CAT items with significant correlation with STST measurements were included in two multivariate models. The results of linear regression analysis are summarized in and . Breathlessness and confidence leaving home manifested the strongest association with time to perform the 5STST. Breathlessness, limitation of activities and confidence leaving home were the strongest predictors of the number of repetitions achieved during the 30s-STST.
Table 6. Spearman rank correlation of STST (5STST and 30s-STST) with CAT items.
Table 7. Results of multivariate linear regression analysis of the association of the time to complete the 5STST with different CAT items.
Table 8. Results of multivariate linear regression analysis of the association of the repetitions of the 30s-STST with different CAT items.
Discussion
The ABCD assessment tool acknowledges COPD as a multicomponent disease [Citation2]. This approach guides pharmacological treatment and is based on the evaluation of symptoms by the use of disease-specific questionnaires and the history of previous exacerbations as an indicator of the risk for future adverse events. Meanwhile, the multisystemic effects of COPD are reflected by exercise performance that is predictive of adverse outcomes such as mortality in COPD patients [Citation5]. The STST evaluates the ability to stand up from a sitting position and is partly dependent on lower limb muscle strength and balance, in addition to postural control and cardiorespiratory reserve [Citation12,Citation18,Citation19]. Most importantly, the STST is a practical and well-tolerated tests suitable in most clinical settings, including the bedside [Citation11,Citation21]. STST have been shown to provide a meaningful and relevant metric of functional performance in patients with COPD [Citation18,Citation22]. Despite the increasing popularity of the STST in COPD research and clinical practice, this is the first study to focus on its relationship with the GOLD ABCD classification. In our study, 5STST performance time and the number 30s-STST repetitions displayed statistically significant correlations with the basic components of ABCD classification namely the CAT score, the number of COPD exacerbations in the past year, and in the case of 5STST time, with the number of hospitalizations for COPD exacerbation in the past year. Furthermore, STST performance differed significantly when patients are stratified using the cut off values of CAT score and the number of previous exacerbations that define their classification in the ABCD tool. This finding underlines further the multidimensional nature of the ABCD assessment as a mode of classification aiming at providing further information beyond airflow obstruction and flow limitation.
According to our results, measurements derived from 5STST and 30s-STST correlate significantly with the number of COPD exacerbations in the past year, and in the case of 5STST time, with the number of hospitalizations for COPD exacerbation in the past year. Moreover, the time to perform 5STST was significantly higher in subjects who experienced two or more exacerbations or at least one hospitalization for an exacerbation in the past year. Likewise, the same subgroup of subjects achieved a significantly lower number of 30s-STST of repetitions compared with subjects without exacerbations. These results seem reasonable since it has been recognized that skeletal muscle dysfunction is a common feature in subjects with COPD, and may play a significant role in morbidity and mortality [Citation23]. In particular, lower exercise capacity has been shown to be a predictor of re-hospitalization [Citation8] and survival in COPD patients [Citation9]. Previous research has demonstrated that STSTs have been shown to exhibit excellent reliability, correlation with exercise capacity and lower limb strength in COPD patients [Citation11–13]. Functional measurements that show a strong association with STST parameters, such as lower daily step count and lower 6MWT distance, have been found to predict future COPD exacerbations [Citation24,Citation25]. In brief, our results are in line with the fact that previous exacerbations are accompanied by a significant functional and clinical cost for the COPD patient and STST performance reflects this well-established association. Nevertheless, the prognostic utility of STST concerning future exacerbations remains unclear. Although STST measurements correlate significantly with validated prognostic indices (iBODE and ADO) and mortality risk in COPD [Citation11,Citation14,Citation26], the 1-min STST does not demonstrate a statistically significant correlation with future exacerbations [Citation26]. We believe that our data supports the need and hypothesis for larger prediction studies investigating whether performance in STSTs is an independent predictor of future exacerbations or mortality.
Our study showed a significant correlation between CAT score and time to perform 5STST or the number of 30s-STST of repetitions. This finding is in agreement with a previous study showing that the 5STST score was positively associated with age and with CAT score [Citation27]. Other studies have shown a significant correlation of STST performance not only with CAT scores but also with other health status questionnaires such as the SGRQ and the Chronic Respiratory Questionnaire (CRQ) [Citation11]. This is potentially clinically important information since it links CAT score to a functional measure like STST performance amendable to a suitable therapeutic strategy such as pulmonary rehabilitation. In addition, both STST measurements and health status as assessed by CAT have been reported to improve significantly in patients with COPD after pulmonary rehabilitation [Citation11,Citation15,Citation28]. Thus, STSTs seem to provide a meaningful and relevant metric that reflects the burden of symptoms and at the same time could help define physical recommendations in COPD patients. Most importantly, the availability of such a simple test renders is ideal tests for primary but also for hospital settings.
Nevertheless, our study is the first to investigate the relationship of STST with the separate items of the questionnaire. Our results show that not all out of the eight items which comprise the CAT questionnaire contribute to this correlation. Breathlessness was the only respiratory item that correlated significantly with STST measurements along with the items that evaluate limitation of activities, confidence leaving home and lack of energy. These findings support once again an individualized approach to the alterations in health status in COPD, while focusing exclusively on respiratory symptoms overlooks the multidimensional, systemic approach of COPD. In our cohort of patients, self-reported breathlessness and confidence leaving home emerged as two of the strongest predictors of performance in both STST, while limitation of activities presented a strong association only with the 30s-STST test. The latter seems reasonable since STST evaluate a manoeuvre which is a common activity of daily living [Citation19]. In the case of breathlessness, the findings are following previous studies reporting a significant correlation of STST with the mMRC dyspnea scale [Citation11] and the dyspnea domain of the CRQ [Citation14]. Moreover, earlier findings have revealed the substantial impact of the breathlessness component in the predictive value of the CAT total score [Citation29,Citation30], especially for milder symptomatic patients [Citation3]. At the same time, the discriminative ability of “confidence leaving home” seems better in more severe patients [Citation3]. Therefore, according to our data, the implementation of STSTs in clinical practice serves and could complement the individualized approach of the COPD patient.
Our study design has several limitations. First, the small sample size hinders the extension of our data to the general patient population and should be taken into account when evaluating the value of functional measurements derived from STST tests. The former is particularly apparent in the small proportions of patients in groups A and C of the present cohort. This can be explained by the fact that our clinic operates in a tertiary care hospital and thus the patients referred to us are frequently more symptomatic at presentation. Secondly, although significant correlations were revealed, we are unable to conclude the cause and effect of the associations. Finally, although patients with overt musculoskeletal and neurological conditions were never selected in the first place, it would have been prudent to formally include these pathologies as distinct exclusion criteria to prevent confounding. Individuals (30% of our cohort) who were unable to perform the STST were characterized by a higher percentage of GOLD group D and CAT score and significantly more COPD exacerbations and hospitalizations in the past year. On the one hand, our results may support a potential use for STST as a stratification tool based on the ability to complete the STST manoeuvre, as it has been previously proposed [Citation11]. Obviously, if a patient is unable to perform even 1 STST manoeuvre it is a very poor result, even if the test could not be considered as valid and completed. On the other hand, the value of the STST seems to be confined in better functioning, less symptomatic patients.
Conclusion
In stable COPD patients, our study has shown that the performance in two STST differed according to the level of symptoms and the risk of future exacerbations that define groups A-D based on GOLD 2018 classification tool. In this cohort of patients with stable COPD, 5STST performance time and the number 30s-STST repetitions were significantly correlated with the CAT score, the number of COPD exacerbations within the past year and, in the case of 5STST time, with the number of hospitalizations for COPD exacerbation within the past year. The correlation of STST performance with CAT score was confined to specific items of the questionnaire that assess breathlessness, limitation of activities, confidence and lack of energy. Finally, stratification based on the ability to complete the STST manoeuvre revealed that individuals who could not perform the STST were characterized by a higher percentage of GOLD group D and CAT score and significantly more COPD exacerbations and hospitalizations in the past year.
Declaration of interest
The authors declare that they have no conflict of interest or financial ties to disclose.
References
- Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet. 1997;349(9064):1498–1504. DOI:10.1016/S0140-6736(96)07492-2
- WHO. Global initiative for chronic obstructive lung disease. Wisconsin (USA): WHO; 2019. Available from: https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf.
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. DOI:10.1183/09031936.00102509
- Karloh M, Fleig Mayer A, Maurici R, et al. The COPD assessment test: what do we know so far?: a systematic review and meta-analysis about clinical outcomes prediction and classification of patients into GOLD stages. Chest. 2016;149(2):413–425. DOI:10.1378/chest.15-1752
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society Statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13. DOI:10.1164/rccm.201309-1634ST
- Pitta F, Troosters T, Probst VS, et al. Physical activity and hospitalization for exacerbation of COPD. Chest. 2006;129(3):536–544. DOI:10.1378/chest.129.3.536
- Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest. 2007;131(3):696–704. DOI:10.1378/chest.06-1610
- Emtner MI, Arnardottir HR, Hallin R, et al. Walking distance is a predictor of exacerbations in patients with chronic obstructive pulmonary disease. Respir Med. 2007;101(5):1037–1040. DOI:10.1016/j.rmed.2006.09.020
- Garcia-Aymerich J, Lange P, Benet M, et al. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–778. DOI:10.1136/thx.2006.060145
- Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. 1985;78(1):77–81. DOI:10.1016/0002-9343(85)90465-6
- Jones SE, Kon SS, Canavan JL, et al. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. 2013;68(11):1015–1020. DOI:10.1136/thoraxjnl-2013-203576
- Butcher SJ, Pikaluk BJ, Chura RL, et al. Associations between isokinetic muscle strength, high level functional performance, and physiological parameters in patients with chronic obstructive pulmonary disease. Int J Chronic Obstr Pulm Dis. 2012;7:537–542.
- Ozalevli S, Ozden A, Itil O, et al. Comparison of the Sit-to-Stand Test with 6 min walk test in patients with chronic obstructive pulmonary disease. Respir Med. 2007;101(2):286–293. DOI:10.1016/j.rmed.2006.05.007
- Crook S, Büsching G, Schultz K, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. Eur Respir J. 2017;49(3):1601871. https://doi.org/10.1183/13993003.01871-2016. DOI:10.1183/13993003.01871-2016
- Zanini A, Aiello M, Cherubino F, et al. The one repetition maximum test and the sit-to-stand test in the assessment of a specific pulmonary rehabilitation program on peripheral muscle strength in COPD patients. Int J Chronic Obstruct Pulmon Dis. 2015;10:2423–2430.
- Miller MR, Hankinson J, Brusasco V, et al. Standardization of spirometry. Eur Respir J. 2005;26(2):319–338. DOI:10.1183/09031936.05.00034805
- Quanjer PH, Stanojevic S, Cole TJ, et al. ERS global lung function initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. DOI:10.1183/09031936.00080312
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. DOI:10.1080/02701367.1999.10608028
- Kocks JW, Asijee GM, Tsiligianni IG, et al. Functional status measurement in COPD: A review of available methods and their feasibility in primary care. Prim Care Respir J. 2011;20(3):269–275. DOI:10.4104/pcrj.2011.00031
- Zanini A, Crisafulli E, D’Andria M, et al. Minimum clinically important difference in 30-s Sit-to-Stand Test after pulmonary rehabilitation in subjects with COPD. Respir Care. 2019;64(10):1261–1269. DOI:10.4187/respcare.06694
- Hansen H, Beyer N, Frølich A, et al. Intra- and inter-rater reproducibility of the 6-minute walk test and the 30-second sit-to-stand test in patients with severe and very severe COPD. COPD. 2018;13:3447–3457. DOI:10.2147/COPD.S174248
- Vaidya T, Chambellan A, de Bisschop C. Sit-to-stand tests for COPD: a literature review. Respir Med. 2017;128:70–77. DOI:10.1016/j.rmed.2017.05.003
- Swallow EB, Reyes D, Hopkinson NS, et al. Quadriceps strength predicts mortality in patients with moderate to severe chronic obstructive pulmonary disease. Thorax. 2007;62(2):115–120. DOI:10.1136/thx.2006.062026
- Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. DOI:10.1056/NEJMoa021322
- Moy ML, Teylan M, Weston NA, et al. Daily step count predicts acute exacerbations in a US cohort with COPD. PLoS One. 2013;8(4):e60400. DOI:10.1371/journal.pone.0060400
- Puhan MA, Siebeling L, Zoller M, et al. Simple functional performance tests and mortality in COPD. Eur Respir J. 2013;42(4):956–963. DOI:10.1183/09031936.00131612
- Bernabeu-Mora R, Giménez-Giménez LM, Montilla-Herrador J, et al. Determinants of each domain of the short physical performance battery in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2539–2544. DOI:10.2147/COPD.S138402
- Dodd JW, Hogg L, Nolan J, et al. The COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre, prospective study. Thorax. 2011;66(5):425–429. DOI:10.1136/thx.2010.156372
- Houben-Wilke S, Janssen DJA, Franssen FME, et al. Contribution of individual COPD assessment test (CAT) items to CAT total score and effects of pulmonary rehabilitation on CAT scores. Health Qual Life Outcomes. 2018;16(1):205. DOI:10.1186/s12955-018-1034-4
- Raghavan N, Lam YM, Webb KA, et al. Components of the COPD assessment test (CAT) associated with a diagnosis of COPD in a random population sample. COPD. 2012;9(2):175–183. DOI:10.3109/15412555.2011.650802