Abstract
Lung hyperinflation is an important therapeutic target in symptomatic emphysema patients. Endobronchial therapies that reduce end-expiratory lung volume are increasingly being used in advanced cases. However, there is paucity of data regarding the effects of these therapies on the heart functions. The aim of this study is to evaluate the right ventricular functions before and after the procedure in patients who underwent endobronchial coil therapy (EBCT).
Patients who were between 18 and 80 years of age and scheduled for EBCT with GOLD 3-4 were enrolled in the study. Right heart functions were evaluated using MPI, TAS, TAPSE. Right atrium area and maximum velocity of tricuspid regurgitation were also noted.
A total of 23 patients were enrolled in the study. 21 patients underwent bilateral intervention, while only 2 patients received unilateral treatment. There was an improvement in MPI (0.49 ± 0.15 vs 0.39 ± 0.11, p < 0.001) and TAS (11.6 (9 − 15) vs 13.2 (9.80 − 17.0), p = 0.001). Peak TRV (2.52 ± 0.6, 2.38 ± 0.6, p = 0.02) and PASP values were lower in the post-operative period (41.15 ± 5.94 vs 36.83 ± 8.01 p = 0.019).
In this current study, we found improved echocardiographic RtV parameters in patients who received EBCT treatment.
Introduction
Chronic obstructive pulmonary disease (COPD) is a major global health issue that causes significant morbidity and mortality [Citation1]. Persistent airflow reduction is the hallmark of the disease, and frequently accompanied by hyperinflation in advanced cases. Hyperinflation may impede cardiorespiratory mechanics [Citation2,Citation3] and is related to dyspnea, a decrease in quality of life, frequent exacerbations and even mortality [Citation4–6]. Therefore, not surprisingly lung hyperinflation has become an important therapeutic target in symptomatic COPD patients [Citation7]. Surgical resection of the emphysematous lung tissue, or lung volume reduction surgery (LVRS) can be used in select patients who are severely limited in their daily activities to improve their lung functions and quality life [Citation8]. However, this surgery is associated with significant morbidity and mortality [Citation9]. Recently, bronchoscopic techniques were developed as an alternative to LVRS to achieve results with lesser complications. Consequently, a number of studies have shown that endobronchial coil therapy (EBCT) that reduce end-expiratory lung volume may be a potential therapeutic option in advanced cases of emphysema and hyperinflation [Citation10–14].
There is a complex interaction between the pulmonary and cardiovascular systems. Numerous changes that arise in COPD affects the heart. These include, but not limited to, chronic hypoxemia, constriction and disruption of pulmonary vascular beds, hyperviscosity secondary to hypoxia and polycythemia, systemic inflammation [Citation15]. In addition, hyperinflation and increased intrathoracic pressure reduces right ventricular (RtV) filling and output [Citation16]. In fact, it was shown that RtV dysfunction starts in early stages of COPD even before overt cor pulmonale develops [Citation17,Citation18]. Therefore, lung volume reduction therapies may also influence the cardiac functions, particularly RtV functions. Accordingly, previous studies showed improved RtV function in patients who underwent LVRS [Citation8,Citation19]. Similarly, endobronchial therapies, including both coil and valve treatments are useful practices in emphysema with similar effects on the quality-of-life [Citation20]. Although improved surrogate and echocardiographic markers of ventricular functions have been shown after valve treatments [Citation21,Citation22], there is paucity of data on the effects of EBCT on RtV functions. In the current study, with a hypothesis that lung volume reduction therapy using coils would improve RtV functions, we evaluated the patients who underwent EBCT with echocardiography before and after the procedure.
Methods
Study group
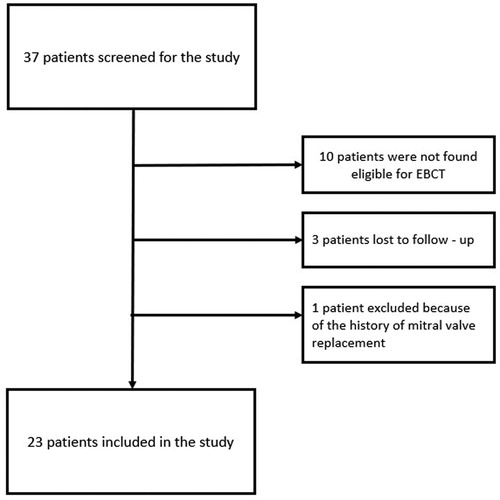
Patients who were between 18 and 80 years of age and scheduled for EBCT with the Global Initiative on Obstructive Lung Disease stage for COPD (GOLD) 3 and 4 at Pamukkale University Hospitals, Denizli between February 2019 and January 2020 were included in the study. Eligibility criteria for EBCT were previously described in an expert panel recommendation [Citation23]. However, patients with left ventricular low ejection fraction (defined as <50%), severe valvular pathology, atrial fibrillation, pulmonary artery (PA) pressure greater than 50 mm Hg (established via echocardiography) were also excluded from the study. Twenty-three patients were enrolled in the study out of 37 consecutive patients. The decision for endobronchial coil therapy was made with body plethysmography in all patients except for 3. In these remaining 3 patients, the decision was made with computed tomography findings. The medical history, demographic characteristics, pre-operative and post-operative pulmonary function test values were collected from hospital registries during their admission.
This prospective observational study was approved by the Medical Ethics Committee, Pamukkale University Hospitals, and was conducted according to the Declaration of Helsinki. Informed consent was obtained from all patients before the measurements.
Endobronchial coil placement procedure
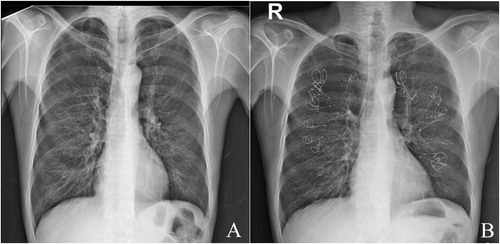
The procedure was performed under general anesthesia with fluoroscopic guidance. The endobronchial coil system (PneumRx, CA, USA) is a two-part system consisting of coils and a delivery system [Citation24]. First, the airway in the selected segment was determined bronchoscopically and its length was measured using a guide wire. Coil of suitable length (generally 100 mm, 125 mm or 150 mm) was placed on the targeted segment using a carrier catheter and takes on the shape of a coil. The targeted lobe was systematically treated with 10-14 coils on average. While a single lobe was treated initially, the other targeted lobe in the opposite lung was treated at least 8 weeks later [Citation24]. An example of a PA chest X-Ray images of a patient who underwent bilateral EBCT procedure is provided in .
Echocardiographic evaluation
The echocardiographic studies including 2 D, M-mode, pulse wave doppler and pulse tissue doppler imaging (TDI) were performed from all standard echocardiographic windows. Left ventricle (LV) and RtV measurements were performed according to current guidelines [Citation25]. Systolic pulmonary artery pressure was calculated using modified Bernoulli equation (4x TRV2 + RAP), where TRV is the continuous Doppler maximum velocity of tricuspid regurgitation in m/s, and RAP is the right atrial pressure estimated from evaluation of the inferior vena cava during respiration. Right ventricular myocardial performance index (MPI) was calculated as the ratio of isovolumic contraction and relaxation time (IVRT + IVCT) divided by ejection time (ET) (MPI = [IVRT + IVCT]/ET). Postoperative echocardiographic examinations were performed at least 1 month after the final EBCT for both patients underwent unilateral or bilateral procedures.
Statistical analyses
Data analyzed using SPSS software for windows (IBM SPSS 20, IBM Corp., Armonk, NY). Kolmogorov Smirnov and Shapiro Wilk tests were used for determination of normal distribution. Continuous variables were defined by the mean ± standard deviation or median, minimum and maximum as appropriate. Normally distributed continuous variables were analyzed using paired sample t-test. The Wilcoxon signed-rank test was used for the abnormally distributed continuous variables. P values < 0.05 were considered as statistically significant.
Results
A total of 23 patients were included in the study (). Sixteen (%70) patients were using long-term oxygenation therapy. Five (%22) patients had hypertension and 3(%13) patients had diabetes mellitus. All patients were under long-acting muscarinic receptor antagonists, long-acting beta agonist and inhaled corticosteroids due to stage 3 and 4 COPD. There were 12 (52%) GOLD 3 and 11 (48%) GOLD 4 patients. Baseline characteristics of the patients were summarized in . All except 2 patients received bilateral treatment. Reasons for unilateral treatment were presence of contralateral large bullae and postponed procedure due to SARS – COV2 outbreak.
Table 1. Baseline characteristics of the study patients.
Pre-procedure and post-procedure pulmonary function tests of patients were evaluated. After the EBCT procedure, forced expiratory volume during first second (FEV-1) and forced vital capacity (FVC) pre-operative and post-operative values showed statistical improvement (FEV1, 30 (15 − 52.8) vs 35 (17.80 − 64), p = 0.001; FVC, 52.6 (34.9 − 83) vs 63 (43.4 − 112), p = 0.004, respectively) (). Pre-procedural body plethysmography data was available for 20 patients. Post-EBCT data was only available for 11 patients, mainly due to inadequate tests related to patient incompliance. Moreover, 3 patients did not attend to their appointments. In these 11 patients, changes in RV% (pre: 341 ± 134 vs post: 240 ± 83, p: 0,037) and TLC% (pre: 158 ± 48 vs post: 128 ± 26, p: 0,021) were statistically significant.
Table 2. Pre-EBCT and post-EBCT clinical and echocardiographic values. Data are presented as means ± standard deviations or median (minimum – maximum). Pre-EBCT and post-EBCT clinical and echocardiographic values. Data are presented as means ± standard deviations or median (minimum – maximum) according to distribution of normality.
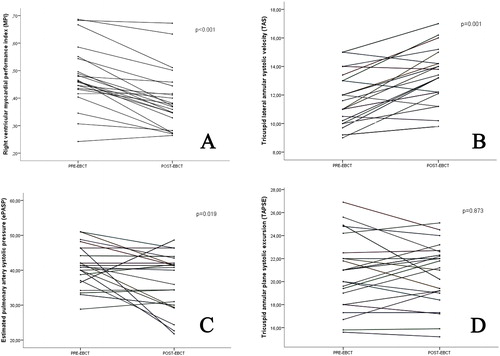
When the pre-operative and post-operative data of the patients were compared, there were statistically significant differences in doppler–derived tricuspid lateral annular systolic velocity (TAS) and myocardial performance index (MPI) values were better than the pre-operative values (TAS, 11.6 (9 − 15) vs 13.2 (9.80 − 17.0), p = 0.001; MPI, 0.49 ± 0.15 vs 0.39 ± 0.11, p < 0.001 pre-operative and post-operative, respectively). Trans-tricuspid E velocity was found to be significantly higher and right atrium (RA) area was smaller in the postoperative period (E velocity, 43 ± 10.88 vs 46.61 ± 9.95, p = 0.013; RA Area, 17.3 ± 3.73 vs 15.26 ± 3.4, p < 0.001; pre-operative and post-operative, respectively). TRV and pulmonary artery systolic pressure (PASP) values of patients were significantly lower compare to the pre-operative period (TRV; 2.52 ± 0.6, 2.38 ± 0.6, p = 0.02, PASP; 41.15 ± 5.94 vs 36.83 ± 8.01 p = 0.019, pre-operative and post-operative, respectively). There was no significant difference between the preoperative and postoperative tricuspid annular plane systolic excursion (TAPSE) values of the patients (21.18 ± 3.91, 21.11 ± 3.58, respectively, p=.873) (). Post-procedural changes in echocardiographic parameters were shown in .
Discussion
In this study, we evaluated 23 patients with severe emphysema before and after EBCT. Our results were as following: 1- We found significantly higher TAS values and lower MPI values indicating improved RtV functions after the procedure. Moreover, RA area, velocity of tricuspid regurgitant jet (TRV), and PA pressure were significantly dropped. 2- We did not find a difference in TAPSE and in tricuspid annulus diameters.
The significance of RtV has frequently been underestimated in routine practice. This is partly due to the vast focus given to the evaluation of the left heart. Moreover, assessment of RtV function remains relatively challenging not only because of the lack of familiarity with ultrasound techniques that are used, but also because of its crescent shape, the irregular endocardial surface, location, and complex contraction mechanisms [Citation25,Citation26]. However, there is a complex interaction between the lungs and the heart, and the RtV plays an important role in the morbidity and mortality of patients with pulmonary disease [Citation1,Citation2]. Previous studies suggest RtV function and structure is affected early in the course of pulmonary disease, which emphasize the importance of the evaluation of RtV in COPD [Citation27]. Hilde et al. evaluated RtV functions in patients with COPD and healthy controls and demonstrated that the RtV dysfunction and remodeling occurs even at slight changes in pulmonary pressures [Citation18]. They also concluded that RtV isovolumic acceleration, MPI, and strain could detect subclinical disease and distinguish controls from those with COPD but without pulmonary hypertension [Citation18]. Furthermore, MPI was shown to correlate with prognosis in COPD patients [Citation28]. In the current study, pre-procedure mean MPI, which is a global estimate of both systolic and diastolic functions was 0.49 ± 0.15 and was in the abnormal range (normal: < 0.40) in 20 (87%) of the patients, indicating a subclinical RtV dysfunction in this group. However, TAS and TAPSE, which were used as regional systolic estimates for RtV systolic functions were in the normal range for most of the patients [Citation25].
A number of studies examined the RtV function and pulmonary hemodynamics after LVRS. Sciurba et al. studied 20 patients with diffuse emphysema undergoing a unilateral or bilateral LVRS. They found that the echocardiographic fractional change in the area of the RtV during cardiac contraction increased from 0.33 ± 0.11 to 0.38 ± 0.10 (p = 0.02) after surgery, suggesting an improvement in RtV function [Citation8]. Similarly, using fast-thermistor thermodilution at rest and during submaximal upright exercise in 12 patients, Mineo et al. showed improved right ventricular indices, including cardiac index and stroke volume at rest and during exercise in addition to significant improvements in respiratory function 6 months after bilateral LVRS [Citation19]. Nevertheless, Criner et al. enrolled 28 patients from the National Emphysema Treatment Trial who underwent right heart catheterization (RHC) before and 6 months after LVRS and compared to patients receiving medical therapy. Changes from baseline pressures to post-treatment, including mean PA pressure or cardiac output were similar between the groups, except for a smaller decrease in pulmonary capillary wedge pressure at end-expiration after LVRS compared with controls (-1.8 vs. 3.5 mm Hg, p = 0.04) [Citation29].
Although it needs further elucidation, several mechanisms can explain the improvements in RtV functions after lung volume reduction procedures. In the study of Mineo et al. RtV stroke volume and EF were correlated with the reduction in RV/TLC ratio (Residual Volume [RV], Total lung capacity [TLC]) suggesting that reduced lung hyperinflation was a major determinant of the overall improvement in RtV performance [Citation19]. Reduction in hyperinflation may lead to improved lung and chest wall mechanics and respiratory muscle performance [Citation12]. Moreover, pulmonary vascular resistance may drop after the procedure, due to the capillary recruitment that may occur as a result of the better pulmonary mechanics in lung zones previously compressed by hyperinflated alveoli or to the “tethering effect” of extra-alveolar vessels with the improvement in elastic recoil [Citation8]. Nevertheless, the latter mechanism is debatable because a study showed lung elastic recoil did not correlate with pulmonary hemodynamics in severe emphysema [Citation30]. Reduction of hyperinflation and intrathoracic pressures may also ameliorate left ventricular diastolic function [Citation3], and decrease pulmonary vascular resistance and enhance the RtV filling [Citation31]. Finally, reduced hyperviscocity and increased arterial oxygenation can contribute to the improvements in RtV performance [Citation27]. However, there is also the potential for the resection of partially preserved vascular tissue with surgical lung volume reduction [Citation8], which may be related with differential effects on RtV function compared to endobronchial techniques.
The alterations in RtV and pulmonary vascular indices after endobronchial techniques have been evaluated only in a limited number of studies. Pizarro et al. enrolled 32 patients with severe emphysematous COPD scheduled for endoscopic lung volume reduction (ELVR) using endobronchial valves for their study [Citation21]. They evaluated RtV functions before and 8 weeks after the procedure and found that RtV apical longitudinal strain improved significantly in the total study cohort (-7.96 ± 7.02% vs. −13.35 ± 11.48%, respectively, p = 0.04), whereas there were no significant changes in other parameters of RtV function such as RtV global longitudinal strain, TAPSE or PA systolic pressure after ELVR [Citation21]. In a pilot study of 6 patients with severe heterogeneous emphysema, and established pulmonary hypertension, investigators showed that mean PA pressure, pulmonary arterial wedge pressure, and cardiac index improved in addition to the symptoms and lung function in 5 out of 6 patients and 90 days after unilateral ELVR with endobronchial valves [Citation31]. We included patients undergoing EBCT rather than endobronchial valves in our study and found significant improvements in parameters regarding right heart functions. Mean MPI values and the number of patients with abnormal MPI were decreased after the treatment. Baseline mean TAS values were within normal ranges, however, still post-procedural values increased. On the other hand, no significant change was found in TAPSE, that is another parameter regional RtV systolic functions. TAS measures tissue velocities, whereas TAPSE measures annular motion, which may partly explain this discrepancy.
There are certain limitations of the study. First, we did not perform RHC to the study participants. Nevertheless, RHC is an invasive procedure, that is not routinely performed in COPD patients as part of the diagnostic or therapeutic process [Citation32]. Second, we also did not measure left ventricular indices at the follow- up. Although this might have provided a more comprehensive assessment of the heart functions, it was beyond the scope of our study. Third, we included consecutive patients after the feasibility of the procedure was evaluated by the operator. This may have resulted in a selection bias. Fourth, one could argue that longer follow-up periods might be needed to observe changes after a such procedure. However, in previous studies 2 to 3 months follow-up periods were sufficient to observe alterations in both the lung and RtV functions, even after unilateral interventions [Citation8,Citation21]. Moreover, most patients received bilateral therapy and they underwent echocardiographic examination 4 weeks after the second session, which is at least 12 weeks after their first session. Fifth, despite significant improvements in echocardiographic parameters, minimal clinical important difference for most RtV imaging parameters are not known. Small study population was another limitation of the study. Finally, post-EBCT body plethysmography measurements for the evaluation of the impact of the procedure on lung volumes were not available for all patients, mainly due to inadequate tests related to the patient incompliance. Therefore, we can only speculate that the observed changes in cardiac functions are a result of reduced lung hyperinflation with coil treatment.
Conclusion
Endobronchial therapies are increasingly being used to reduce end-expiratory lung volume in advanced cases of emphysema and hyperinflation. Considering close relationship between heart and lung, these therapies potentially affect the heart. In this study, we showed improvements in echocardiographic parameters of PA pressure and RtV functions, including TAS and MPI.
Decleration of interest
All authors of this manuscript declare that there are no relevant conflicts of interest.
| Abbreviations | ||
| GOLD | = | Classification of Global Initiative for Chronic Obstructive Lung Disease |
| MPI | = | Right ventricular myocardial performance index |
| TAS | = | Doppler–derived tricuspid lateral annular systolic velocity |
| TAPSE | = | Tricuspid annular plane systolic excursion |
| TRV | = | tricuspid regurgitant jet velocity |
| PASB | = | Systolic pulmonary artery pressure values |
| RtV | = | Right ventricle |
References
- Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–1940.
- Visca D, Aiello M, Chetta A. Cardiovascular function in pulmonary emphysema. Biomed Res Int. 2013;2013:184674–184678.
- JöRgensen K, Houltz E, Westfelt U, et al. Effects of lung volume reduction surgery on left ventricular diastolic filling and dimensions in patients with severe emphysema. Chest. 2003;124(5):1863–1870.
- Kim YW, Lee C-H, Hwang H-G, et al. Resting hyperinflation and emphysema on the clinical course of COPD. Sci Rep. 2019;9(1):1–8.
- Pavasini R, Fiorencis A, Tonet E, et al. Right ventricle function in patients with acute coronary syndrome and concomitant undiagnosed chronic obstructive pulmonary disease. COPD. 2019;16(3–4):284–291.
- Gruenberger J-B, Vietri J, Keininger D, et al. Greater dyspnea is associated with lower health-related quality of life among European patients with COPD. COPD. 2017;12:937–944.
- O'Donnell DE, Laveneziana P. Physiology and consequences of lung hyperinflation in COPD. Eur Respir Rev. 2006;15(100):61–67.
- Sciurba FC, Rogers RM, Keenan RJ, et al. Improvement in pulmonary function and elastic recoil after lung-reduction surgery for diffuse emphysema. N Engl J Med. 1996;334(17):1095–1099.
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348(21):2059–2073.
- Gulsen A, Sever F, Girgin P, et al. Evaluation of bronchoscopic lung volume reduction coil treatment results in patients with severe emphysema. Clin Respir J. 2017;11(5):585–592. DOI:10.1111/crj.12387
- Marchetti N, Kaufman T, Chandra D, et al. Endobronchial coils versus lung volume reduction surgery or medical therapy for treatment of advanced homogenous emphysema. Chron Obstructive Pulm Dis: J COPD Found. 2018;5(2):87–96.
- Klooster K, ten Hacken NH, Slebos D-J. The lung volume reduction coil for the treatment of emphysema: a new therapy in development. Expert Rev Med Devices. 2014;11(5):481–489. DOI:10.1586/17434440.2014.929490
- Shah PL, Zoumot Z, Singh S, et al. Endobronchial coils for the treatment of severe emphysema with hyperinflation (RESET): a randomised controlled trial. Lancet Respir Med. 2013;1(3):233–240.
- Toker Ugurlu T, Ugurlu E. Impacts of coil treatment on anxiety and depression in emphysema. Can Respir J. 2020;2020:4270826–4270826.
- Han MK, McLaughlin VV, Criner GJ, et al. Pulmonary diseases and the heart. Circulation. 2007;116(25):2992–3005. DOI:10.1161/CIRCULATIONAHA.106.685206
- Kolb TM, Hassoun PM. Right ventricular dysfunction in chronic lung disease. Cardiol Clin. 2012; 30(2):243–256. DOI:10.1016/j.ccl.2012.03.005
- Sabit R, Bolton CE, Fraser AG, et al. Sub-clinical left and right ventricular dysfunction in patients with COPD. Respir Med. 2010;104(8):1171–1178.
- Hilde JM, Skjørten I, Grøtta OJ, et al. Right ventricular dysfunction and remodeling in chronic obstructive pulmonary disease without pulmonary hypertension. J Am Coll Cardiol. 2013;62(12):1103–1111.
- Mineo TC, Pompeo E, Rogliani P, et al. Effect of lung volume reduction surgery for severe emphysema on right ventricular function. Am J Respir Crit Care Med. 2002;165(4):489–494.
- Intepe YS, Metin B, Kilic M, et al. A comparison of the effects of endobronchial valve and coil treatments used in emphysema on respiratory functions and quality of life. Eur Respir J. 2016. 48 (suppl 60) PA1861. DOI:10.1183/13993003.congress-2016.PA1861
- Pizarro C, Schueler R, Hammerstingl C, et al. Impact of endoscopic lung volume reduction on right ventricular myocardial function. PLoS One. 2015;10(4):e0121377. DOI:10.1371/journal.pone.0121377
- Faisal A, Zoumot Z, Shah PL, et al. Effective bronchoscopic lung volume reduction accelerates exercise oxygen uptake kinetics in emphysema. Chest. 2016;149(2):435–446. DOI:10.1378/chest.15-0404
- Herth FJF, Slebos D-J, Criner GJ, et al. Endoscopic lung volume reduction: an expert panel recommendation - update 2017. Respiration. 2017;94(4):380–388. DOI:10.1159/000479379
- Slebos D-J, Ten Hacken NH, Hetzel M, et al. Endobronchial coils for endoscopic lung volume reduction: best practice recommendations from an expert panel. Respiration. 2018;96(1):1–11. DOI:10.1159/000490193
- Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713. DOI:10.1016/j.echo.2010.05.010
- Markley RR, Ali A, Potfay J, et al. Echocardiographic Evaluation of the Right Heart. J Cardiovasc Ultrasound. 2016;24(3):183–190. DOI:10.4250/jcu.2016.24.3.183
- Cuttica MJ, Shah SJ, Rosenberg SR, et al. Right heart structural changes are independently associated with exercise capacity in non-severe COPD. PLoS One. 2011;6(12):e29069. DOI:10.1371/journal.pone.0029069
- Tanaka Y, Hino M, Mizuno K, et al. Evaluation of right ventricular function in patients with COPD. Respir Care. 2013;58(5):816–823.
- Criner GJ, Scharf SM, Falk JA, et al. Effect of lung volume reduction surgery on resting pulmonary hemodynamics in severe emphysema. Am J Respir Crit Care Med. 2007;176(3):253–260. DOI:10.1164/rccm.200608-1114OC
- Falk JA, Martin UJ, Scharf S, et al. Lung elastic recoil does not correlate with pulmonary hemodynamics in severe emphysema. Chest. 2007;132(5):1476–1484. DOI:10.1378/chest.07-0041
- Eberhardt R, Gerovasili V, Kontogianni K, et al. Endoscopic lung volume reduction with endobronchial valves in patients with severe emphysema and established pulmonary hypertension. Respiration. 2015;89(1):41–48. DOI:10.1159/000368369
- Bugalho A. Is endoscopic lung volume reduction able to reverse pulmonary hypertension in patients with severe emphysema? Respiration. 2015;89(1):12–14. DOI:10.1159/000368967