Abstract
Pulmonary rehabilitation (PR) is a mandatory component of a comprehensive treatment of patients with chronic respiratory disease. However, there is no officially published data about PR Centers in Latin America.
The objetive is to identify Latin American Pulmonary Rehabilitation Centers and evaluate their characteristics and organizational aspects.
A cross-sectional study with the Pulmonary Rehabilitation Centers indicated by the Latin American Respiratory and Physiotherapy Societies and by our own personal survey among physicians and physiotherapists. An eletronic transmission questionnaire with 20 questions was sent to the Coordinator of each one of the Centers.
217 Pulmonary Rehabilitation Centers were found throughout Latin America and a total of 160 (73.7%) Centers answered the questionnaire. Of these, 65.8% had private administration; 68.8% had an associated program for patients with heart disease; programs lasted an average of 24 sessions; the rehabilitation team consisted mainly of physiotherapists, physicians and dietitians; 90.6% of the centers evaluated the patients with different questionnaires; 91.9% used treadmill and 90.6% bicycle for exercises of lower limbs and 80.1% proprioceptive neuromuscular facilitation technique with weights to train the upper limbs of their patients; 55.6% had an educational program and 36.9% presented a home-based program.
There has been a great increase in the number of Latin American Pulmonary Rehabilitation Centers, presenting diversity in organizational aspects.
Introduction
Even though pulmonary rehabilitation provides several benefits for chronic respiratory diseases, attendance at such programs is still low [Citation1,Citation2]. A study conducted in Latin America (1998) showed that 28 pulmonary rehabilitation centers located in eight countries assisted Latin American population: Brazil (15), Argentina (3), Mexico (3), Uruguay (2), Colombia (2), Chile (1), Venezuela (1), and Peru (1). Despite the low number of pulmonary rehabilitation centers, these results were optimistic since communication within Latin American countries would encourage the opening of new centers [Citation3].
In 2014, an international survey involved 40 countries and 430 rehabilitation centers, 43.7% were located in Europe, 43.5% in North America, and the remaining centers in Oceania, Asia, South America, or Africa. They found great organization heterogenicity, highlighting the need for future standardization of rehabilitation centers. Although unofficial information regarding the opening of new Pulmonary Rehabilitation Centers in Latin America has been reported over the past few years, only eight centers were contacted in this survey, which does not reflect the reality of this area [Citation4].
As the Latin American Thoracic Association (ALAT) aims to stimulate pulmonary rehabilitation in Latin American countries, information regarding center localization, equipment, and personnel is essential because these centers may serve as models for diffusing and training rehabilitation professionals in this region. In this context, we aimed to identify the number of pulmonary rehabilitation centers in Latin America and evaluate their profile, including administration type, diseases attended, personnel, evaluations, care routines, program duration, equipment used, and association with cardiac care.
Materials and methods
Pulmonary rehabilitation centers of Latin American countries were tracked through Medical and Physiotherapy Societies and direct information from pulmonologists and physiotherapists.
Once a center was indicated, a letter explaining study aims and a 20-question questionnaire (Supplementary material 1) were sent via e-mail. This questionnaire was developed based on other published questionnaires on rehabilitation surveys conducted in other countries, like administration type, diseases attended, personnel, evaluations, care routines, program duration, equipment used, and associations with cardiac care [Citation3–7]. The project was submitted to and approved by the Institutional Review Board (Hospital São Paulo/Unifesp). As the study was not directly involved with patients the Institutional Review Board considered not necessary a formal signed consent form and that the acceptance by the Center to answer the questionnaire could be officially accepted as a consent. In case of no response, centers were contacted twice by e-mail or telephone or both.
Data was inserted into an Excel spreadsheet and statistical analysis was performed using SPSS software (IBM Corp. USA), version 21.0. Outcomes were expressed as median, 25-75% interquartile intervals, and absolute and relative frequencies. The proportion of pulmonary rehabilitation centers per 100.000 population in each country was also analyzed, being the country population obtained from official websites.
Results
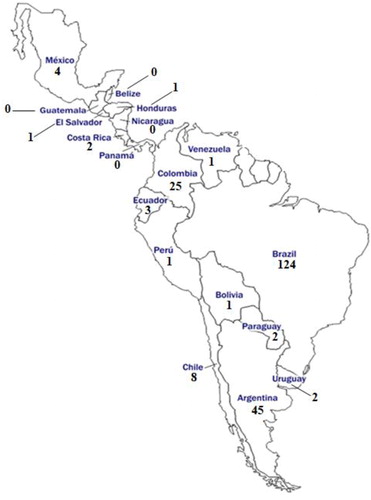
We located 217 pulmonary rehabilitation centers throughout Latin America and 160 (73.7%) responded to the questionnaire. Brazil, Argentina, and Colombia prevailed in the number of centers ().
Table 1. Estimated distribution and population of Pulmonary Rehabilitation Centers in Latin American countries and percentages of responders.
Most pulmonary rehabilitation centers in Latin America were operated by private administrators (65.8%), including universities, hospitals, and outpatient clinics: most private hospital services (81.8%) were covered by insurance health plans; in private clinics, payments were predominantly performed by patients; and rehabilitation programs were free in all public universities.
All rehabilitation centers treated patients with lung diseases and 68.8% also accepted cardiovascular disease patients. The most frequent lung diseases were COPD (99.4%), asthma (71.9%), and bronchiectasis (70.6%).
Median number of prescribed training sessions was 24 [19–36], with a minimum frequency of two sessions/week [2–3] and maximum frequency of three sessions/week [3–4]. Pulmonary rehabilitation teams included physiotherapists (96.9%), physicians (78.1%), dietitians (45.6%), psychologists (41.9%), nurses (33.8%), physical education professionals (23.1%), occupational therapists (7.5%), and others (23.1%).
Patients were evaluated using 6-minute walking test (6MWT) (88.8%), body mass index (87.5%), spirometry (76.3%), maximum respiratory strength test (66.3%), one maximum repetition test (1RM) for upper (60.6%) and lower limbs (58.8%), incremental lower (47.5%) and upper limbs exercise test (39.4%), lower limbs endurance test (36.9%), shuttle walking test (23.1%), bioimpedance (21.9%), incremental gas analysis test (22.5%), skinfolds (8.1%), and Dual-energy X-ray Absorptiometry (DEXA) (7.5%).
The most applied questionnaires were Dyspnea Scale/Modified Dyspnea Scale (MRC/mMRC) (68.1%), Saint George Respiratory Questionnaire (SGRQ) (56.9%), COPD Assessment Test (CAT) (50.0%), Short Form-36 Questionnaire (SF-36) (38.1%), Anxiety and Depression Scale Hospital (HADS) (21.9%), Chronic Respiratory Questionnaire (CRQ) (17.5%), International Physical Activity Questionnaire (IPAQ) (17.5%), Baseline Dyspnea Index/Transitional Dyspnea Index (BDI/TDI) (11.3%), World Health Organization Quality of Life (WHOQOL) (3.8%), and Short Form-12 questionnaire (SF-12) (1.9%). Only 9.4% of the centers did not use questionnaires.
Treadmills, cycle ergometers, dumbbells and anklets were the most frequent described equipments (). Approximately 57,5% of the centers use 40-60% of the maximum load for aerobic and resistance upper limbs training; for lower limbs the most frequent load was 70-80% of the maximum load in aerobic training (51,3%) and 40-60% of the maximum load in resistance training (68,1%). Approximately 55.6% of the centers offered an educational program and 36.9% offered a home-based exercise program
Table 2. Equipments available in the Pulmonary Rehabilitation Centers of Latin America according to the answered questionnaires (n = 160).
Discussion
The main finding of this study was the observation of an 8-fold increase in the number of Rehabilitation Centers in Latin America (217 centers) compared to a study conducted in 1998 (27 centers) and the increased number of countries (from eight to 14) with at least one pulmonary rehabilitation center [Citation3].
Although many new centers have been identified in Latin America, four Central American countries (Panama, Guatemala, Belize and Nicaragua) still do not have any pulmonary rehabilitation center, but only five countries have four or more centers (Brazil, Argentina, Colombia, Chile and Mexico) (). The largest increases in the number of rehabilitation centers were mainly observed in Argentina, Brazil, and Colombia; however, if we take into consideration the ratio of centers per 100.000 inhabitants, we observe that this ratio may be considered low. For instance, considering the COPD prevalence in Brazil, there is only one center for around 4,000 COPD patients. The lack of studies looking at the ratio of rehabilitation centers over general population or COPD prevalence precludes the possibility of comparing our data to data derived from a similar population. Despite this large increase in the number of rehabilitation centers in Latin America in the recent years, we clearly see that there is still a lot of work to be done in several countries in order for the dissemination of the importance of rehabilitation centers for patients with chronic pulmonary diseases. We really hope that our findings may stimulate all professional health care societies in Latin America to create awareness of the importance of rehabilitation as a mandatory non-pharmacological part of treatment of patients with chronic pulmonary diseases.
Most of the patients with chronic pulmonary disease in Latin America has had the opportunity to attend the rehabilitation centers program with no direct expenses as the programs are reimbursed by their governments or insurance companies. This is in agreement with the European policy for chronic pulmonary diseases where 62.8% of the centers are reimbursed by the government [Citation4] and United States with the health insurance plans reimbursing 92.5% of the centers.
Overall, all rehabilitation centers in Latin America receive COPD patients in their programs, like what had already seen in the first survey conducted in Latin America (1998)3; the same was also observed in Canada (2005), where 90% of the centers described COPD as the most frequent seen disease at their centers [Citation7]. A study on pulmonary rehabilitation centers in Europe and North America also described COPD as the most frequent disease (90%) attended at their rehabilitation centers [Citation4]. However, it is well known that besides COPD all patients with chronic pulmonary disease should be offered the opportunity of a rehabilitation program. Currently, it was shown that patients with interstitial lung diseases and pulmonary hypertension submitted to pulmonary rehabilitation programs improve their physical capacity and quality of life [Citation8–10].
Most rehabilitation centers in Latin America provides a comprehensive multidisciplinary support to their patients and similar to what was observed in the first survey in Latin America (1998)3 the most reported professionals were respiratory physiotherapists, physicians, and dietitians. In Europe, respiratory physiotherapy was described as the most frequent profession in pulmonary rehabilitation programs, whereas physicians and dietitians were more frequent in North America [Citation4]. A recent global study on cardiology rehabilitation centers also reported respiratory physiotherapists, physicians, and dietitians as the most frequent professionals in their rehabilitation programs [Citation11].
Around 90% of the centers answered that they evaluate the physical capacity of their patients using the 6MWT, a simple and easy-to-apply test [Citation1]Citation2 a much large proportion that was related in European (33%) and in North American centers (53%) [Citation4]. In several European countries, shuttle walking test was more popular than 6MWT for assessing exercise capacity. In Latin America, shuttle walking test is used by only 17% of the centers, and only 22.5% of the centers evaluate exercise capacity using cardiopulmonary exercise test.
Despite dyspnea being the most frequent symptom of COPD patients. only 68% of Latin American rehabilitation centers evaluate dyspnea in their routine assessing, but a value superior to Europe (49%) and North America (36%) [Citation4]. One would expect that globally dyspnea would be routinely evaluated.
Over 90% of the centers use treadmill or cycle ergometers for lower limbs training, increasing from 79% and 68%, respectively, compared to the Latin American survey in 19983. European centers predominantly described the use of cycle ergometers for aerobic training, while 43% used outdoor walks. In North America, treadmills and cycle ergometers were used in the same proportion [Citation4]. Treadmill training is probably more physiological than cycle ergometer since walking is part of everyday life. However, some centers prefer cycle ergometers because they are smaller than treadmills, occupying less space, allowing training a larger number of patients, being more cost-effective. Most centers in Latin America use high aerobic training loads (70% to 80% of maximum), what suggests that appropriate aerobic training concepts have been properly disseminated [Citation13].
Upper limb aerobic training was mainly performed using dumbbells and proprioceptive neuromuscular facilitation technique with loads of 40% to 60% of maximal incremental exercise test. Although arm cycle ergometer is still considered gold standard for upper limb training, Castro et al. [Citation1]Citation4 showed that upper limb exercise with cycle ergometer causes more thoracoabdominal asynchrony and pulmonary hyperinflation than proprioceptive neuromuscular facilitation technique. It has already been shown that pulmonary hyperinflation leads to dyspnea and early respiratory muscle fatigue [Citation15].
Mean duration of pulmonary rehabilitation programs was 24 sessions, with a frequency of 2 to 3 sessions per week. It has been reported that minimum duration for COPD patients should be six weeks [Citation16], but severe patients may require longer time to improve physical capacity. A study conducted with international rehabilitation centers in Europe [Citation4] reported median duration of pulmonary rehabilitation programs of eight weeks [5.6-12].
Overall, the number of pulmonary rehabilitation centers in Latin America, Europe, and North America is insufficient for all chronic pulmonary disease patients needing this care. We expect that this survey triggers some stimuli for developing new centers in Latin America, especially in countries without rehabilitation centers. Rehabilitation centers in countries with few centers could also operate as training centers for multidisciplinary personnel. In low-income countries, low-cost rehabilitation centers and home-based rehabilitation should be stimulated [Citation17]. Although most centers said they orient their patients to continue performing exercises at home, only few had well-structured home-based rehabilitation programs to follow up patients. We believe that home-based rehabilitation program is the opportunity that would make possible a larger number of COPD patients to exercise.
Conclusion
The number of pulmonary rehabilitation centers increased in Latin America since 2000s, mainly in Argentina, Brazil, and Colombia. Organization and exercise routines among centers were diverse. The number of rehabilitation centers in Latin America is low, and efforts should be made to develop rehabilitation centers in all countries. Low-cost rehabilitation centers and home-based rehabilitation should be also stimulated in order that most of the patients with chronic and limiting pulmonary diseases could have access to this important and mandatory non-pharmacological treatment.
Supplemental Material
Download PDF (165.6 KB)Acknowledgments
The authors thank Probatus Academic Services for providing scientific language revision and editing.
Disclosure statement
There is no conflict of interest with any of the authors.
None of the authors have had any commitment with the Tobacco Industry.
This is an original paper that describes the Rehabilitation Centers in Latin America after an exhausting survey in every country. The only survey of Rehabilitation centers in Latin America before was in 1998 and it was published as a chapter in a book.
Jose R. Jardim MD Gabriela Barreto PT MSc.
References
- Rochester CL, Vogiatzis I, Holland AE, et al. An official American Thoracic Society/European Respiratory Society Policy Statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. 2015;192(11):1373–1386. DOI:10.1164/rccm.201510-1966ST
- Janssens W, Corhay JL, Bogaerts P, et al. How resources determine pulmonary rehabilitation programs: a survey among Belgian chest physicians. Chron Respir Dis. 2019;16:1–5 DOI:10.1177/1479972318767732
- Jardim JR, Camelier A, Miki D, et al. Pulmonary rehabilitation: guidelines to success. Cap The Latin American Perspective, cap 37, 661-667. Lippincott Williams & Wilkins Editora, 2000. Chest physicians. Chron Respir Dis. 2018;16:1–10.
- Spruit MA, Pitta F, Garvey C, et al. Differences in content and organizational aspects of pulmonary rehabilitation programmes. Eur Respir J. 2014;43(5):1326–1337. DOI:10.1183/09031936.00145613
- Korenfeld Y, Bastidas CM, Saavedra L, et. al. Current status of cardiac rehabilitation in Latin America and the Caribbean. Am Heart J. 2009;158(3):480–487. DOI:10.1016/j.ahj.2009.06.020
- Bowen JM, Campbell K, Sutherland S, et. al. Pulmonary rehabilitation in Ontario: a cross-sectional survey. Ont Health Technol Assess Ser. 2015;15(8):1–67.
- Brooks D, Sottana R, Bell B, et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J. 2007; 14(2):87–92. DOI:10.1155/2007/951498
- Desveaux L, Ferreira TJ, Goldstein R, et al. An international comparison of pulmonary rehabilitation: a sytematic review. COPD. 2015;12(2):144–153. DOI:10.3109/15412555.2014.922066
- Nakazawa A, Cox NS, Holland AE. Current best practice in rehabilitation in interstitial lung disease. Ther Adv Respir Dis. 2017;11(2):115–128. DOI:10.1177/1753465816676048
- Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The joint task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): endorsed by: association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67–119. DOI:10.1093/eurheartj/ehv317
- Supervia M, Turk-Adawi K, Lopez-Jimenez F, et al. Nature of cardiac rehabilitation around the globe. E Clinical Medicine. 2019;13:46–56. DOI:10.1016/j.eclinm.2019.06.006
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002; 166(1):111–117.
- Casaburi R, Patessio A, Loli F, et al. Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis. 1991; 143(1):9–18. DOI:10.1164/ajrccm/143.1.9
- Castro AA, Porto EF, Feltrim MI, et al. Asynchrony and hyperinflation in patients with chronic obstructive pulmonary disease during two types of upper limbs exercise. Arch Bronconeumol. 2013;49(6):241–248. DOI:10.1016/j.arbres.2012.12.009
- Celli BR, Rassulo J, Make BJ. Dyssynchronous breathing during arm but not leg exercise in patients with chronic airflow obstruction. N Engl J Med. 1986;314(23):1485–1490. DOI:10.1056/NEJM198606053142305
- Bolton CE, Bevan-Smith EF, Blakey JD, British Thoracic Society Pulmonary Rehabilitation Guideline Development Group, on behalf of the British Thoracic Society Standards of Care Committee, et. al. British thoracic society guideline on pulmonary rehabilitation in adults. Thorax. 2013;68(Suppl 2):ii1–30. DOI:10.1136/thoraxjnl-2013-203808
- Pradella CO, Belmonte GM, Maia MN, et. al. Home-based pulmonary rehabilitation for subjects with COPD: a randomized study. Respir Care. 2015;60(4):526–532. DOI:10.4187/respcare.02994