Abstract
Pulmonary Rehabilitation (PR) is a key intervention in the management of people with chronic obstructive pulmonary disease (COPD), though few studies have assessed where changes in outcomes occur during a PR program. The aim of this study was to determine the changes in exercise capacity and health-related quality of life at four and eight weeks during a twice-weekly supervised PR program in people with COPD. Fifty participants with COPD were recruited and attended PR twice-weekly for eight weeks. The outcome measures were the endurance shuttle walk test (ESWT), six-minute walk distance (6MWD), St George’s Respiratory Questionnaire (SGRQ), COPD Assessment Test (CAT) and the Hospital Anxiety and Depression Scale (HADS) which were measured at baseline, four and eight weeks. Compared to baseline, at week four there were significant improvements in ESWT (mean difference [95%CI] 197 [89 to 305] seconds), 6MWD (22 [8 to 36] metres), SGRQ symptom score (-6 [-12 to −1] points) and SGRQ total score (-4 [-7 to −1] points). Between week four and eight there were further significant improvements in ESWT (94 [8 to 181] seconds) only. By week eight, ESWT, 6MWD, SGRQ symptoms and total score, and CAT had all improved significantly compared to baseline measures. This study demonstrated that participants with moderate to very severe COPD who participated in a twice weekly, eight-week PR program (16 sessions) had significant improvement in ESWT, 6MWD, SGRQ, and CAT score with the greatest improvements occurring in the first four weeks of the program.
Supplemental data for this article is available online at https://doi.org/10.1080/15412555.2021.2013793 .
Introduction
Pulmonary rehabilitation (PR) is a key intervention in the management of people with chronic obstructive pulmonary disease (COPD) [Citation1,Citation2]. There is extensive evidence that PR improves exercise capacity, health-related quality of life (HRQoL) and reduces hospital admissions and length of stay [Citation3–7].
The common duration of PR programs is between six and 12 weeks [Citation4]. While the outcomes of PR programs in terms of improvements in exercise capacity and HRQoL have been well documented, there are only a small number of studies that have evaluated the changes in these outcomes during a PR program. With shared decision making becoming an increasingly important aspect of healthcare [Citation8], it is important to provide patients with more information about their likely treatment outcomes. Understanding the trajectory of change during a PR program may provide clinicians and patients with knowledge regarding when they can expect changes to occur while participating in a PR program. Two studies that did sequential measurements of exercise capacity using the six-minute walk test (6MWT) demonstrated a plateau of improvement at eight weeks of a 12-week PR program [Citation9,Citation10]. Another study measuring exercise capacity by endurance treadmill walking at a constant speed every two weeks found the walk distance plateaued at 10 weeks of a 12 week PR program (24 sessions) [Citation11]. Changes in HRQoL over the course of a PR program have been reported using the Chronic Respiratory Disease Questionnaire (CRQ) [Citation12], and shown that the most significant improvements were made early in the program. In one study the greatest improvements were in the first two weeks (four session) [Citation11], and in the other study at four weeks (12 sessions) [Citation9] with minimal change after this in either study. Both studies were limited by relatively small participant numbers (n = 28 [Citation9] and n = 13 [Citation11]).
As exercise training is a main component of PR programs it is important to accurately measure an individual’s exercise outcomes. Field walking tests have been commonly used to assess changes in functional exercise capacity as they are low cost, require minimal equipment and reflect daily living. The endurance shuttle walk test (ESWT) measures the ability to sustain submaximal exercise intensities relative to an individual’s maximal exercise capacity, which may be a good reflection of ability to perform activities of daily living [Citation13]. There is evidence which suggests measuring endurance exercise capacity using the ESWT is more responsive to change after a PR program than a six-minute walk test (6MWT), since improvements in six-minute walk distance (6MWD) require an individual to walk faster whereas improvements in the ESWT time require individuals to walk at a constant speed for longer, which more closely reflects the aim of exercise training in PR [Citation14]. No studies assessing changes in exercise capacity over time have used a measurement of both endurance exercise capacity (ESWT) and functional exercise performance (6MWT) to compare changes during the course of a PR program.
The primary aim of this study was to determine changes in endurance exercise capacity and HRQoL at four and eight weeks of a PR program in people with COPD. Secondary aims were 1) to determine the changes at four and eight weeks in functional exercise performance, health status, anxiety and depression, and 2) to determine whether disease severity using spirometric criteria [classified by the Global Strategy for Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (GOLD)] [Citation5], affected the magnitude of changes in exercise capacity or HRQoL.
Methods
Study design
This was a prospective cohort study that was part of a larger clinical trial, with a published trial protocol [Citation15]. Ethics approval was obtained from the Sydney Local Health District Research Ethics and Governance Committee (RPAH zone) and registered with the Australian and New Zealand Clinical Trials Registry: ACTRN12616001586404. Written consent was obtained from all participants prior to data collection.
Participants
Participants were recruited from three hospitals within Sydney Local Health District and were eligible to participate if they had: a diagnosis of COPD (post bronchodilator forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) ratio of <0.7; FEV1 < 80%predicted) [Citation5]. The Global Lung Foundation Initiative (GLI) predictive equations were used for normative values, and participants met the criteria for the FEV1/FVC ratio below the lower limit of normal [Citation16]. Exclusion criteria were: a body mass index of greater than 35 kg/m2; long term oxygen therapy (LTOT); musculoskeletal, cardiovascular or neurological conditions which would adversely affect ability to participate in the exercise assessments or exercise programs; or had participated in a supervised exercise program within the last 12 months.
Eligible participants attended a PR program twice a week for eight weeks. The PR program was held in hospital outpatient settings using gym-based equipment and was supervised by physiotherapists experienced in the management of people with COPD and providing PR programs.
Spirometry was assessed using a hand-held spirometer (EasyOne, NND Medical Technologies, Andover, Massachusetts, USA) at baseline to characterise participants based on the GOLD spirometric criteria of disease severity and at eight weeks to confirm stability of lung function during the PR program. The GOLD categories were moderate (GOLD II); FEV1 50-79%predicted, severe (GOLD III); FEV1 30-49%predicted, and very severe (GOLD IV); FEV1 < 30% predicted.
Outcome measures
Participants performed exercise testing and completed questionnaires at baseline, week four and week eight of the PR program. The primary outcomes were endurance exercise capacity measured by the ESWT and HRQoL measured by the St George’s Respiratory Questionnaire (SGRQ). Secondary outcomes included functional exercise performance measured by the 6MWT, health status measured by the COPD Assessment Test (CAT) and anxiety and depression measured by the Hospital Anxiety and Depression Scale (HADS).
Measurement of exercise capacity
At baseline participants completed two 6MWTs and two ESWTs with the greater distance and time (respectively) being recorded as the baseline measures. The six minute walk distance (6MWD) was used in an equation to determine the participant’s starting level for the ESWT [Citation17]. The ESWT is an externally paced walking test where participants are asked to walk back and forth along a 10-metre course until they are no longer able to keep up with the predetermined pace. The ESWT has a ceiling effect of 20 min, so if at baseline a participant reached 10 min comfortably the test was ceased and after a 30-minute rest the test was repeated at the next higher level with the aim of the participant achieving an ESWT time of between five and 10 min to allow for improvement over the PR program. The minimal clinically important difference (MCID) following PR for the ESWT is 186 s [Citation18] and for the 6MWT is 30 metres [Citation19].
Measurement of HRQoL, health status, anxiety and depression
HRQoL was measured using the SGRQ, a self-administered questionnaire designed to measure self-perceived impairments in health and quality of life. It measures three domains (symptoms, activity limitations and impact of disease) and gives a total score between zero (good health) and 100 (poor health). A reduction in the total score of the SGRQ of four points is the MCID [Citation20]. Health status was measured using the COPD Assessment Test (CAT) [Citation21]. This questionnaire has eight items which include questions about cough, sputum, chest tightness, breathlessness on hills/stairs, activity limitation at home, sleep and fatigue. Measured out of 40, a higher score indicates greater impact of COPD [Citation22]. A reduction of two points in the CAT is the MCID [Citation23]. Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS) [Citation24]. Higher scores indicate a higher likelihood of anxiety or depression, with a cut off score (in each domain) of greater than or equal to eight indicating possible anxiety or depression [Citation25].
PR program
Exercise training
Participants attended the hospital-based, outpatient program for 90 min, allowing for rests. The PR program consisted of walking and cycle exercise training, strength training and education. Walking training consisted of overground or treadmill walking. Walking commenced at 80% of each participant’s average walk speed determined from the 6MWT [Citation26]. Walking duration commenced at 15 min and progressively increased to 30 min by week four. Walk speed was progressed based on symptoms of dyspnoea and rate of perceived exertion (RPE) aiming for three to four (‘moderate’ to ‘somewhat severe’) on the modified zero to 10 category-ratio scale [Citation27].
Lower limb cycle training intensity commenced at 60% of each participant’s estimated peak work rate, using an equation based on the results of the 6MWT [Citation28]. Cycling duration commenced at 15 min and increased to 20 min by week two. Intensity progressed to 70% peak work rate based on symptoms of dyspnoea or RPE score of at least three to four on the modified zero to 10 category-ratio scale.
Lower limb strengthening exercises used body weight (squats, sit-to-stands and step-ups) aiming to achieve three sets of eight to 10 repetitions before local muscle exhaustion. Upper limb strengthening exercises using free weights were commenced in week two at a load that could be achieved for eight to 10 repetitions before local muscle exhaustion. Fixed weight strengthening exercises for the lower limbs (leg extension and leg press) and upper limbs (latissimus dorsi pull downs and chest press/fly) commenced in week three at a load that could be achieved for eight to 10 repetitions before local muscle exhaustion. Resistances were increased once participants could achieve three sets of 10 repetitions in two consecutive training sessions.
Education
All participants received individualised (one-on-one) education, as applicable, on the following topics: the function of the lungs; what is COPD; medication use; managing breathlessness; importance of exercise training; smoking cessation (if current smokers); sputum clearance (if appropriate); symptom monitoring and exacerbation management.
Statistical analysis
Data were analysed using Statistical Package for the Social Sciences (SPSS) software (V.25.0.0.2, IBM Corporation, Armonk, New York, USA) for each outcome measure and expressed as mean and standard deviations (SD). Changes in each outcome over time were analysed using repeated measures analysis of variance (ANOVA). If the ANOVA for any outcome was significant, a post hoc analysis of the ANOVA using pairwise comparisons (with adjustments for multiple comparisons using Fisher’s least significant difference test) was used to determine between which time points the significant change occurred. Values of p < 0.05 were considered statistically significant. For the analyses of GOLD grades, those with moderate COPD were compared to a combined group of those with severe and very-severe COPD.
The standardised response mean (SRM) was calculated to assess the responsiveness of the ESWT and the 6MWT. The SRM is a ratio of change of the average scores divided by the SD of change. The SRM was used to assess responsiveness to change of ESWT and 6MWT from baseline to week four, and from week four to week eight. A SRM of 0.2 is small, 0.5 is moderate and 0.8 is high responsiveness [Citation29].
Sample size
A sample size of 35 participants was needed to have an 90% chance of detecting as significant at the 5% level a change in the ESWT of 186 s (the MCID) [Citation18,Citation19] given a standard deviation of 239 s [Citation30]. To account for a 20% dropout, 42 participants were needed. For this study the participants were part of a larger clinical trial [Citation15], which required a larger sample size.
Results
Of the 66 participants recruited to the larger clinical trial, eight participants withdrew prior to the week four assessment (n = 5 no longer interested, n = 1 work commitment, n = 2 withdrew for other health reasons), an additional eight participants were excluded for not having three data points for at least one outcome measure. Therefore, 50 participants were included in the analyses ().
Table 1. Baseline characteristics.
Exercise capacity
ESWT
Results for 46 (92%) participants were included in the ESWT analysis (, , and ). There was a statistically significant increase in ESWT time between baseline and week four, and between week four and week eight. By week four, 21 (42%) participants reached the MCID of 186 s improvement in ESWT. Nine of these participants (20%) completed 20 min in the ESWT. At week eight, 29 (58%) participants had reached the MCID and 12 participants (26%) completed 20 min in the ESWT. The SRM at week four was 0.54 and the SRM between week four and week eight was 0.32.
Figure 1. a and 1b. Improvement in endurance shuttle walk test time during an eight-week pulmonary rehabilitation program. Participants were assessed at baseline (week 0), week four and week eight. Standard error bars are included.
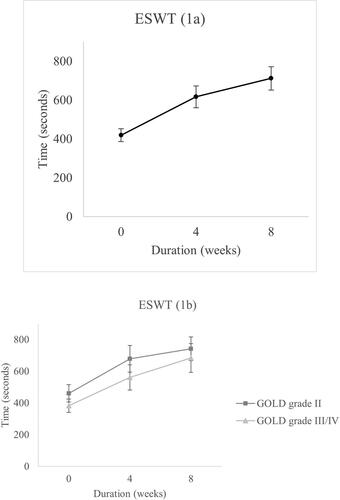
Table 2. Outcome measures at baseline, week four and week eight.
Table 3. Differences between measurement time points.
Results by GOLD grade are presented in , , and . Both the GOLD grade II group and the GOLD grade III/IV group significantly improved ESWT time between baseline and week four with smaller non-significant improvements between week four and eight.
Table 4. Outcome measures at baseline, week four and week eight by GOLD grade.
Table 5. Differences between measurement time points by GOLD grade.
6MWT
Results for 47 (94%) participants were included in the analysis of the 6MWT. The 6MWD increased significantly by week eight of the program. In the first four weeks of the program there was a significant increase in 6MWD of 22 metres and a non-significant increase between week four and week eight. By week four, 17 (36%) participants had reached the MCID of 30 metres improvement. At week eight, this had increased to 24 (51%) participants. The SRM at week four was 0.47 and the SRM between week four and week eight was 0.2. When analysed by GOLD grade, both the GOLD grade II group and GOLD grade III/IV group had statistically significant improvement in 6MWD from baseline to week four. The GOLD grade II group had further statistically significant improvement from week four to week eight ( and ).
HRQoL, health status, anxiety and depression
St George’s respiratory questionnaire
HRQoL measured by the SGRQ was available in 45 (90%) participants and showed a statistically significant improvement in total scores by week four of the program and a small non-significant improvement from week four to week eight. By week four, 22 (49%) participants had reached the MCID of a reduction of four points. At week eight, 26 (58%) participants had reached the MCID. shows that GOLD grade II group had a statistically and clinically significant improvement in SGRQ total score by week four, with no significant change from week four to week eight. The GOLD grade III/IV group had small, non-significant improvements in SGRQ total score from baseline to week four and from week four to week eight. By week eight the mean change of score had reached the MCID of a reduction of four points, however due to variance in participants’ results this change was not statistically significant.
Health status
COPD assessment test
Results for 48 (96%) participants showed a non-significant improvement in CAT score from baseline to week four and from week four to week eight with an overall statistically and clinically significant improvement from baseline to week eight. By week four, 21 (44%) participants had reached the MCID of a reduction of two points. At week eight, 27 (56%) participants had reached the MCID.
Anxiety and depression
Hospital anxiety and depression scale
Baseline results for 47 (94%) participants demonstrated that the majority of participants (57%) had anxiety and depression scores below the cut off eight, indicating low incidence of anxiety or depression in this cohort. While there was a statistically significant reduction in anxiety scores at week four this was not maintained at week eight. There was no significant change in depression scores from baseline to week four or from week four to week eight ( and ).
Discussion
The study aimed to determine the changes that occurred in endurance exercise capacity and HRQoL at four and eight weeks during an eight-week outpatient PR program in people with COPD. The main findings were that for people with COPD, who participated in a twice weekly outpatient PR program for eight weeks, there was a significant improvement in endurance exercise capacity and HRQoL. Significant improvements also occurred in 6MWT and CAT scores which met the MCID by week eight. The magnitude of improvements in ESWT, SGRQ, 6MWD and CAT were greatest in the first four weeks of the program. There was a significant reduction in anxiety scores at week four though this was not maintained at week eight and there was no change in depression scores at any time point.
The ESWT was used as the primary outcome measure and demonstrated significant positive change early in the PR program, surpassing the MCID of 186 s by week four with a smaller increase from week four to week eight. Although other studies have used the ESWT as an outcome measure to assess changes at completion of a PR program, no other studies have used the ESWT to assess changes at timepoints during a PR program to determine the trajectory of change in the ESWT. One study examined the change in endurance exercise capacity using a constant work rate treadmill walking test in people with COPD and found a linear response of increased walking capacity until week 10 of a 12 week (24 sessions) program [Citation11]. This study had a number of limitations including low numbers of participants (n = 13), as well as participants having severe airflow obstruction (mean FEV1 <35%predicted), which the authors acknowledged may reduce the generalisability to PR programs which include patients with less severe COPD. Our findings indicated that significant improvements in the ESWT could be achieved in the first four weeks of a PR program.
The greatest change in the 6MWT also occurred in the first four weeks of the program though did not reach the MCID until week eight. These results differ from previous studies which reported a linear increase in 6MWT distance until plateauing between week eight and week 10 of a PR program [Citation9,Citation10]. The results of a more recent study on the trajectories of change in 6MWT assessed participants in three groups according to their 6MWT improvement in an eight-week PR program (low, moderate and high responders) [Citation31]. At four and eight weeks of the PR program they found a similar pattern to this current study, with greater improvements occurring in the first four weeks for all three groups and smaller gains made between week four and eight.
In the first four weeks the ESWT reached moderate responsiveness to change while the 6MWT did not. Both the ESWT and the 6MWT showed smaller levels of responsiveness to change in the second four weeks of PR. Other studies have reported that the ESWT was more responsive to change in people with COPD who completed PR [Citation32]. Our study has shown that the ESWT is responsive to change over different time points during a PR program.
A secondary aim of our study was to assess changes in the ESWT and 6MWT according to disease severity as categorised by the GOLD classification spirometric criteria. Both the GOLD grade II group and the GOLD grade III/IV group achieved significant changes in the ESWT in the first four weeks of the PR program. The GOLD grade II group reached the MCID for ESWT by week four while the GOLD grade III/IV group did not reach the MCID until week eight. The 6MWT changes showed both groups made significant improvement in the first four weeks with the GOLD grade II group continuing to make further significant improvements between week four and eight. These results demonstrated that those with more severe obstruction may plateau in their ability to walk faster (as required in the 6MWT) by week four of a PR program, while, with further exercise training, they may continue to improve the length of time they can sustain activity at a submaximal level (as measured by the ESWT). Such findings highlight that the peak improvement in the ESWT may take longer to achieve [Citation14] in those with more severe airway obstruction. The differences in improvements in 6MWT between these groups may also reflect that those with more severe COPD often have a higher degree of muscle dysfunction [Citation33] at program commencement that may be more responsive to exercise training in the first four weeks of a PR program. Lee et al [Citation31] suggested that lower muscle strength, higher levels of baseline breathlessness and lower FEV1% predicted in the low/moderate responder groups (similar to the GOLD stage III&IV in our study) may have played a role in the differences they observed between 6MWD in the low/moderate versus high responders (similar to the GOLD grade II in our study) in their PR program. Those in the high responder group made significant gains at four weeks of PR and continued to make significant gains between week four and week eight, similar to those observed in our study in the GOLD grade II group.
HRQoL measured by the SGRQ was also a primary outcome measure. Results demonstrated significant changes by week four of the PR program which reached the MCID (i.e. a reduction in the SGRQ total score of four points). These results support previous findings regarding HRQoL with significant changes occurring early during a PR program [Citation9,Citation11], though these other studies used the CRQ to assess HRQoL. One other study did compare HRQoL scores using the SGRQ after three weeks of participating in a PR program (10 sessions), and six and a half weeks (20 sessions of PR) [Citation34]. This study did not report raw results but found that after 10 sessions of PR, 36% of participants reached the MCID for SGRQ total score and by 20 sessions, 64% of participants reached the MCID. These results closely reflect our study which found 49% reached the MCID of the SGRQ total score by week four (eight sessions) and 58% by week eight (16 sessions).
Despite the changes HRQoL early in the program, significant improvements in health status as measured by the CAT were not recorded until week eight. Change in CAT scores on completion of PR programs has previously been well documented [Citation35–38], though no studies have assessed the changes of scores during a PR program. Our study has demonstrated new knowledge in requiring completion of a PR program to optimise benefits in health status.
When assessing changes in HRQoL according to disease severity as categorised by the GOLD spirometric criteria the largest changes occurred in the first four weeks for the GOLD grade II group and remained significant at week eight. While there was trend to an improvement in HRQoL in the GOLD grade III/IV group, there was higher variation in participant responses which resulted in no significant improvement in HRQoL in this group. Two previous studies have compared SGRQ results based on COPD severity by GOLD classification [Citation39,Citation40]. Both studies found that following a PR program of six to eight weeks that participants in all GOLD grades improved HRQoL, regardless of disease severity. Neither of these studies examined when changes occurred during the program. The observed difference in results compared to our study may be due to lower patient numbers in our study.
For the GOLD grade II group, health status measured by the CAT demonstrated significant change in the first four weeks reaching the MCID, which was not achieved in the GOLD grade III/IV group. No previous studies have assessed changes in CAT scores according to disease severity. The differences in response between these two groups indicates that those with greater disease severity may take longer to respond to a PR program.
The strength of this study was that it is the first to report changes in endurance exercise capacity at four and eight weeks of a PR program using the ESWT in a large number of participants with a range of disease severity which enables generalisation of these findings to other PR programs. One limitation of the study was that the ESWT has a ceiling effect which impacted the ability of continuing to measure change in endurance capacity for those who reached 20 min at week four. This may have resulted in an underestimation of improvement in ESWT. The ESWT test procedures require the same ESWT level to be used at repeat test times to determine change in endurance capacity, thus for those who reach the maximum test time during a PR program overall change will be underestimated. Another limitation was that outcomes were not measured more often, which could have provided greater insights into when changes occurred. However, increased measurements would have increased participant burden. The inclusion of more participants with severe and very severe COPD would have increased the power of the subgroup analysis based on the GOLD spirometric criteria of disease severity.
In conclusion, this study demonstrated that participants with moderate to very severe COPD who participated in a twice weekly, eight-week PR program (16 sessions) had significant improvement in endurance exercise capacity and HRQoL, functional exercise performance and health status, with the greatest magnitude of improvements occurring in the first four weeks of the program.
Author contributions
JB was the principal investigator and with LS and JA developed the original idea for the study. JB procured funding for the study with assistance from LS and JA. JB, LS and AM ran the PR programs. JB and LS evaluated the outcomes together with JA, TD and ZM. All authors played a role in the clinical investigation and in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The authors wish to thank Dr Regina Leung and Natanya Haggman for their contributions to participant recruitment and training. We also would like to thank all the patients who participated in the study.
Declaration of interest
The authors certify that they have no conflicts of interests.
Additional information
Funding
References
- Puhan MA, Gimeno-Santos E, Cates CJ, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;12:CD005305.
- McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;(2):CD003793.
- Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand pulmonary rehabilitation guidelines. Respirology. 2017;22(4):800–819. DOI:https://doi.org/10.1111/resp.13025
- Bolton CE, Bevan-Smith EF, Blakey JD, et al. British thoracic society guideline on pulmonary rehabilitation in adults. Thorax. 2013;68(Suppl 2):ii1–ii30. DOI:https://doi.org/10.1136/thoraxjnl-2013-203808
- Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;49(3):1700214. DOI:https://doi.org/10.1183/13993003.00214-2017
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. DOI:https://doi.org/10.1164/rccm.201309-1634ST
- Marciniuk DD, Brooks D, Butcher S, et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease-practical issues: a Canadian Thoracic Society Clinical Practice Guideline. Can Respir J. 2010;17(4):159–168. DOI:https://doi.org/10.1155/2010/425975
- Trevena L, Shepherd HL, Bonner C, et al. Shared decision making in Australia in 2017. Z Evid Fortbild Qual Gesundhwes. 2017;123–124:17–20. DOI:https://doi.org/10.1016/j.zefq.2017.05.011
- Solanes I, Guell R, Casan P, et al. Duration of pulmonary rehabilitation to achieve a Plateau in quality of life and walk test in COPD. Respir Med. 2009;103(5):722–728. DOI:https://doi.org/10.1016/j.rmed.2008.11.013
- Rejbi IB, Trabelsi Y, Chouchene A, et al. Changes in six-minute walking distance during pulmonary rehabilitation in patients with COPD and in healthy subjects. Int J Chron Obstruct Pulmon Dis. 2010;5:209–215. DOI:https://doi.org/10.2147/COPD.S7955
- ZuWallack R, Hashim A, McCusker C, et al. The trajectory of change over multiple outcome areas during comprehensive outpatient pulmonary rehabilitation. Chron Respir Dis. 2006;3(1):11–18. DOI:https://doi.org/10.1191/1479972306cd096oa
- Guyatt GH, Berman LB, Townsend M, et al. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42(10):773–778. DOI:https://doi.org/10.1136/thx.42.10.773
- Revill SM, Morgan MD, Singh SJ, et al. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax. 1999;54(3):213–222. DOI:https://doi.org/10.1136/thx.54.3.213
- McNamara RJ, McKeough ZJ, McKenzie DK, et al. Water-based exercise in COPD with physical comorbidities: a randomised controlled trial. Eur Respir J. 2013;41(6):1284–1291. DOI:https://doi.org/10.1183/09031936.00034312
- Bishop J, Spencer L, Alison J. Effect of a pulmonary rehabilitation programme of 8 weeks compared to 12 weeks duration on exercise capacity in people with chronic obstructive pulmonary disease (PuRe duration): protocol for a randomised controlled trial. BMJ Open Respir Res. 2020;7(1):e000687.
- Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–1343. DOI:https://doi.org/10.1183/09031936.00080312
- Wootton SL, Ng C, McKeough ZJ, et al. Estimating endurance shuttle walk test speed using the six-minute walk test in people with chronic obstructive pulmonary disease. Chron Respir Dis. 2014;11(2):89–94. DOI:https://doi.org/10.1177/1479972314527470
- Pepin V, Laviolette L, Brouillard C, et al. Significance of changes in endurance shuttle walking performance. Thorax. 2011;66(2):115–120. DOI:https://doi.org/10.1136/thx.2010.146159
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. DOI:https://doi.org/10.1183/09031936.00150314
- Jones PW. St. George’s respiratory questionnaire: MCID. COPD. 2005;2(1):75–79. DOI:https://doi.org/10.1081/copd-200050513
- Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. DOI:https://doi.org/10.1183/09031936.00102509
- Jones PW, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD assessment test (CAT™) scores. BMC Pulm Med. 2011;11:42. DOI:https://doi.org/10.1186/1471-2466-11-42
- Kon SS, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD assessment test: a prospective analysis. Lancet Respir Med. 2014;2(3):195–203. DOI:https://doi.org/10.1016/S2213-2600(14)70001-3
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. DOI:https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. DOI:https://doi.org/10.1016/S0022-3999(01)00296-3
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117.
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381.
- Hill K, Jenkins SC, Cecins N, et al. Estimating maximum work rate during incremental cycle ergometry testing from six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2008;89(9):1782–1787. DOI:https://doi.org/10.1016/j.apmr.2008.01.020
- Garratt AM, Ruta DA, Abdalla MI, et al. SF 36 health survey questionnaire: II. Responsiveness to changes in health status in four common clinical conditions. Qual Health Care. 1994;3(4):186–192. DOI:https://doi.org/10.1136/qshc.3.4.186
- Leung RW, McKeough ZJ, Peters MJ, Alison JA. Short-form sun-style t’ai chi as an exercise training modality in people with COPD. Eur Respir J. 2013;41(5):1051–1057. DOI:https://doi.org/10.1183/09031936.00036912
- Lee CT, Hsieh PL, Chien MY, et al. Trajectories of functional exercise capacity in patients undergoing pulmonary rehabilitation. Int J Chron Obstruct Pulmon Dis. 2019;14:863–870. DOI:https://doi.org/10.2147/COPD.S200247
- Eaton T, Young P, Nicol K, et al. The endurance shuttle walking test: a responsive measure in pulmonary rehabilitation for COPD patients. Chron Respir Dis. 2006;3(1):3–9. DOI:https://doi.org/10.1191/1479972306cd077oa
- McDonald ML, Diaz AA, Ross JC, et al. Quantitative computed tomography measures of pectoralis muscle area and disease severity in chronic obstructive pulmonary disease. A cross-sectional study. Annals Ats. 2014;11(3):326–334. DOI:https://doi.org/10.1513/AnnalsATS.201307-229OC
- Rossi G, Florini F, Romagnoli M, et al. Length and clinical effectiveness of pulmonary rehabilitation in outpatients with chronic airway obstruction. Chest. 2005;127(1):105–109. DOI:https://doi.org/10.1378/chest.127.1.105
- Dodd JW, Hogg L, Nolan J, et al. The COPD assessment test (CAT): response to pulmonary rehabilitation. A multicentre, prospective study. Thorax. 2011;66(5):425–429. DOI:https://doi.org/10.1136/thx.2010.156372
- Dodd JW, Marns PL, Clark AL, et al. The COPD assessment test (CAT): short- and medium-term response to pulmonary rehabilitation. COPD. 2012;9(4):390–394. DOI:https://doi.org/10.3109/15412555.2012.671869
- Jones PW, Harding G, Wiklund I, et al. Tests of the responsiveness of the COPD assessment test following acute exacerbation and pulmonary rehabilitation. Chest. 2012;142(1):134–140. DOI:https://doi.org/10.1378/chest.11-0309
- Kon SS, Clark AL, Dilaver D, et al. Response of the COPD assessment test to pulmonary rehabilitation in unselected chronic respiratory disease. Respirology. 2013;18(6):974–977. DOI:https://doi.org/10.1111/resp.12084
- Golmohammadi K, Jacobs P, Sin DD. Economic evaluation of a community-based pulmonary rehabilitation program for chronic obstructive pulmonary disease. Lung. 2004;182(3):187–196. DOI:https://doi.org/10.1007/s00408-004-3110-2
- Korkmaz Ekren P, Gurgun A, Elmas UF, et al. Effects of pulmonary rehabilitation in patients with mild-to-moderate chronic obstructive pulmonary disease: Bottom of an iceberg. Turk J Phys Med Rehab. 2018;64(2):162–169. DOI:https://doi.org/10.5606/tftrd.2018.1006
