ABSTRACT
Pulmonary rehabilitation (PR) is an essential method for Acute exacerbation in chronic obstructive pulmonary disease (AECOPD) recovery. We perform a meta-analysis to compare early PR with usual care. A literature search was performed through these databases: PubMed, MEDLINE database, Google Scholar, Cochrane, Embase from inception to July 2021. Eligible trials were clinical randomized controlled trials comparing the effects of early PR and usual care in AECOPD patients. The primary endpoint of this meta-analysis was FEV1% predicted, 6-min walk test (6MWD), modified Medical Research Council (mMRC) and George Respiratory Questionnaire-total (SGRQ-total). The secondary outcomes were borg dyspnea score, short-form 36 health survey questionnaire physical (SF-36 physical) and SF-36 mental. We included 13 RCTs with a total of 866 patients. There were no significant effects of the PR group on measures of FEV1% predicted (MD = 0.50, 95%CI −1.43 to 2.44, Z = 0.51, p = 0.61), borg dyspnea score (MD = −0.88, 95%CI −1.89 to 0.13, Z = 1.71, p = 0.09) and SF-36 mental (MD = 4.34, 95%CI −1.64 to 10.32, Z = 1.42, p = 0.16) compared with usual care. PR group achieved better 6MWD (MD = 97.58, 95%CI 17.21 to 177.96, Z = 2.38, p = 0.02), mMRC (MD = −0.36, 95%CI −0.52 to −0.21, Z = 4.56, p ˂ 0.00001), SGRQ-total (MD= −9.67, 95%CI −16.23 to −3.11, Z = 2.89, p = 0.004) and SF-36 physical (MD = 4.98, 95%CI 0.60 to 9.35, Z = 2.23, p = 0.03) compared with usual care group. Early PR in AECOPD patients would lead to better 6MWD, mMRC, SGRQ-total and SF-36 physical. But there were no significant effects of the PR group on measures of FEV1% predicted, borg dyspnea score and SF-36 mental.
Introduction
For the high rates of smoking and air pollution worldwide, Chronic obstructive pulmonary disease (COPD) is still a challenge for clinicians today [Citation1]. COPD patients sometimes experience an acute worsening of symptoms like sputum color changes or an increase in dyspnea and leading to a change in medication. This event is defined as an Acute exacerbation in chronic obstructive pulmonary disease (AECOPD) [Citation2]. AECOPD is the most common result in hospital admission and higher mortality [Citation3]. Hospitalization is accompanied by a rapid decline in lung function and other adverse outcomes like endotracheal intubation [Citation4]. AECOPD is associated with a delay in the recovery of lung function. There is a risk of another exacerbation during this period [Citation5]. Repeated acute exacerbation will cause low exercise capacity, which is related to a high risk of mortality [Citation6].
Pulmonary rehabilitation (PR) because of its beneficial effects on maximal exercise capacity and health-related quality of life has been suggested in AECOPD [Citation7]. Exercise training is an essential part of PR in COPD patients [Citation8]. A meta-analysis demonstrates the effectiveness of an early supervised PR following AECOPD can reduce mortality, the number of readmissions, and the number of days in hospital [Citation9]. The increase in exercise capacity was associated with oxygen uptake increases. Many research found that the ability to achieve the anaerobic threshold predicts more extensive improvements after PR [Citation10]. Some research found PR following AECOPD could improve skeletal muscle function [Citation11].
PR has been shown to be an essential method for AECOPD recovery. However, the meta-analysis of PR study before compared early PR to delay PR [Citation9]. Whether early PR can improve lung function, release dyspnea and improve quality of life is still need more study. We perform a meta-analysis to compare early PR with usual care.
Methods
Search strategies
We searched electronic literature databases for randomized controlled trials (RCTs) comparing early PR with usual care in AECOPD patients. A literature search was performed through these databases: PubMed, MEDLINE database, Google Scholar, Cochrane, Embase from inception to March 2021. The following search terms were used: pulmonary rehabilitation, acute exacerbation of the chronic obstructive pulmonary disease, early rehabilitation, randomized controlled trial.
Data extraction
Two reviewers independently evaluated the included studies and extracted data into RevMan 5.3 (Review Manager: Cochran handbook for systematic reviews). Any disagreement about whether the trials meet the inclusion or exclusion criteria between the two reviewers was resolved by discussing with a third reviewer. If still more data was required, communication through E-mail would be carried out with the authors.
Study selection
We included RCTs comparing early PR with usual care in AECOPD patients. The inclusion criteria included: (1) human studies, (2) randomized control trials (RCT), (3) the comparison between early PR with usual care in AECOPD patients was performed in the study, (4) all participants were adults, (5) if more than one eligible study from the same center using the same protocol, the study with the longest follow-up was used. The exclusion criteria were:(1) studies reported none of these outcomes: 6-min walk test (6MWD), modified Medical Research Council (mMRC), borg dyspnea score, short-form 36 health survey questionnaire (SF-36) physical, SF-36 mental, George Respiratory Questionnaire-total (SGRQ-total), FEV1% predicted. (2) The studies compared the effect of PR initiated after 4 weeks of hospital discharge with early supervised PR initiated during admission or within 4 weeks of hospital discharge.
Outcome measures
The primary endpoint of this meta-analysis was FEV1% predicted, 6MWD, mMRC, and SGRQ-total. The secondary outcomes were borg dyspnea score, SF-36 physical and SF-36 mental.
Quality assessment
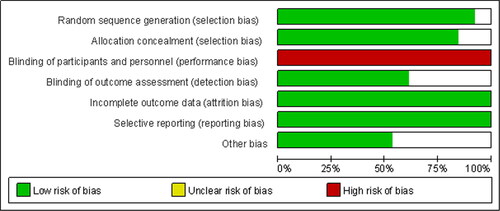
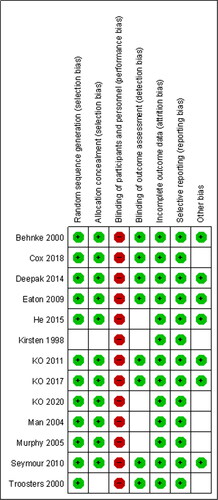
We used the Cochran Handbook for Systematic reviews of Interventions guidelines to assess the risk of bias. Each study was evaluated for random sequence generation, concealment of allocation sequence, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome, and selective reporting. And they were classified by two authors as having a high risk of bias and unclear risk of bias, or a low risk of bias based on the Cochrane tool.
Statistical analysis
Statistical analysis of our meta-analysis was using Cochrane systematic review software RevMan 5.3. We used Mann-Whitney U-test to help us verify the hypothesis and rendered statistical significance as a p-value and Z-value < 0.05. Odds ratio (OR) and 95% confidence intervals (CI) were calculated for dichotomous outcomes, and weighted mean differences (WMD) and 95% confidence intervals (CI) were calculated for continuous outcomes in each included study. I2 value was used to assess statistical heterogeneity. If I2 value ≤50% was considered as having no statistical heterogeneity, a fixed-effects model was used to estimate the overall summary effect sizes. Otherwise, we used a random-effects model. And subgroup analysis or sensitivity analysis would be carried out.
Assessment of PR extensiveness
Intervention in the hospital included: PR consisted of conventional therapy including 30 min of daily breath exercises with repirologists and hospital-based training. Exercise training consisted of 6MWT and 5 self-controlled walking sessions at 75% of the treadmill walking distance of the respective. Some patients completed 16 revolutions on the “bike” with both the upper and lower. Three times a day for 5 consecutive days. Intervention after discharge included: Supervised home-based training for 6 months walking training 3/day at 125% of the best 6MVWD. Physiotherapists deliver the sessions to provide them with a functional assessment of participants. Four sessions were delivered over 2 weeks, starting within 72 h of discharge. Or consisted of 90 min supervised endurance training and resistance training. Endurance training consists of cycling, treadmill walking, and stair climbing at 60–80% of initial Wmax during cycle ergometer/maximal walking speed. Resistance training consists of strength exercises for 5 muscle groups, 10 reps at 60% 1 repetition maximum. Others consisted of supervised exercise training including treadmill, arm cycling, arm and leg strength training at 60–70% of VO2max or HRmax.
Result
Study selection
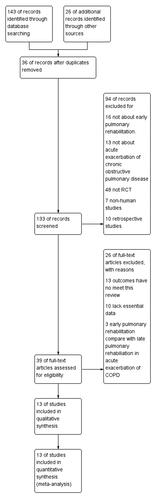
The search algorithm identified 169 records. We identified 143 records from electronic databases and 26 additional records from reference lists and other sources. After deduplication 36 records were excluded. 133 records were screened. 94 records were excluded by reading the abstracts for not about early PR (n = 16), not about AECOPD (n = 13), not RCT (n = 48), non-human studies (n = 7), retrospective studies (n = 10). 39 full-text studies were assessed for eligibility. 13 articles were excluded for outcomes that have not met this review, 10 articles were excluded for lack of essential data, 3 articles were excluded for comparing early PR with late PR in AECOPD. Finally, 13 articles were included in the final meta-analysis [Citation12–24] ().
Included studies
We included a total of 866 patients. All included studies had been published (). Three trials included in and outpatients with AECOPD [Citation12, Citation13, Citation15]. Eight trials included outpatients with AECOPD [Citation14, Citation18–24]. Two trials included inpatients with AECOPD [Citation16, Citation17].
Table 1. Characteristics of the Thirteen Randomized Controlled Trials included in the Meta-analysis.
Quality assessment
The risk of bias abuts the methodological quality of the included studies are elaborated and summarized respectively in ( and ). Quality assessment of 13 included studies indicated that blinding of participants in the PR is impossible, so the performance bias is high. Different rehabilitation training plans in included studies also caused bias in our meta-analysis.
Heterogeneity
There was no statistical heterogeneity between PR and usual care group in FEV1% predicted, mMRC, SF-36 physical and SF-36 mental. Statistical heterogeneity was found between PR and usual care in 6MWD, SGRQ-total and borg dyspnea score.
Effect of the intervention
The primary endpoint
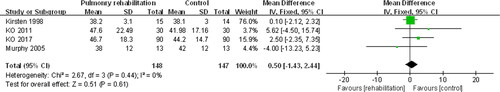
The primary endpoint contains four outcomes: FEV1% predicted, 6MWD, mMRC, and SGRQ-total. Firstly, “FEV1% predicted” was reported in four studies. 148 patients in the PR group and 147 patients in the control group were available to compare the FEV1% predicted. There were no significant effects of the PR group on measures of FEV1% predicted compared with usual care (MD = 0.50, 95%CI −1.43 to 2.44, Z = 0.51, p = 0.61) ().
Figure 4. The graph shows a forest plot of standardized mean difference with a confidence interval for the FEV1% predicted.
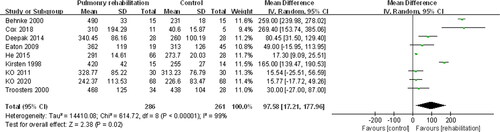
Secondly, “6MWD” was reported in nine studies. 286 patients in the PR group and 261 patients in the control group were available to compare the 6MWD. The result showed that the 6MWD was significantly higher in the PR group (MD = 97.58, 95%CI 17.21 to 177.96, Z = 2.38, p = 0.02) ().
Figure 5. The graph shows a forest plot of standardized mean difference with a confidence interval for the 6MWD.
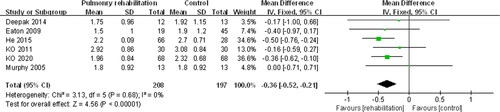
Thirdly, mMRC was reported in six studies. 208 patients in the PR group and 197 patients in the control group were available to compare the mMRC. The result showed that the mMRC was significantly lower in the PR group (MD = −0.36, 95%CI −0.52 to −0.21, Z = 4.56, p ˂ 0.00001) (). It means PR group achieved better mMRC.
Figure 6. The graph shows a forest plot of standardized mean difference with a confidence interval for the mMRC.
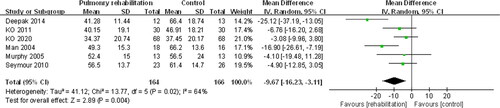
Fourth, SGRQ-total was reported in six studies. 164 patients in the PR group and 166 patients in the control group were available to compare the SGRQ-total. The result showed that the SGRQ-total was significantly lower in the PR group (MD = −9.67, 95%CI −16.23 to −3.11, Z = 2.89, p = 0.004) (). It means PR group achieved a better SGRQ-total.
The second endpoint
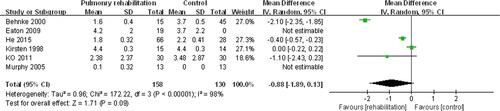
The second endpoint contains three outcomes: borg dyspnea score, SF-36 physical and SF-36 mental. Firstly, “borg dyspnea score” was reported in six studies. 158 patients in the PR group and 130 patients in the control group were available to compare the borg dyspnea score. There were no significant effects of the PR group on measures of borg dyspnea score compared with usual care (MD = −0.88, 95%CI −1.89 to 0.13, Z = 1.71, p = 0.09) ().
Figure 8. The graph shows a forest plot of standardized mean difference with a confidence interval for the borg dyspnea score.
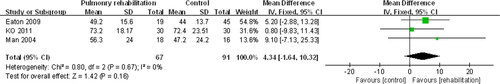
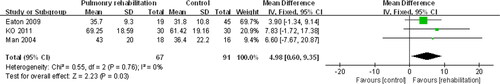
Secondly, SF-36 physical was reported in three studies. 67 patients in the PR group and 91 patients in the control group were available to compare the SF-36 physical. The result showed that the SF-36 physical was significantly higher in the PR group compared with the usual care group. (MD = 4.98, 95%CI 0.60 to 9.35, Z = 2.23, p = 0.03) (). It means PR group achieved better SF-36 physical.
Figure 9. The graph shows a forest plot of standardized mean difference with a confidence interval for the SF-36 physical.
Thirdly, SF-36 mental was reported in three studies. 67 patients in the PR group and 91 patients in the control group were available to compare the SF-36 mental. The result showed that there was no significant difference between the PR group and control group (MD = 4.34, 95%CI −1.64 to 10.32, Z = 1.42, p = 0.16) ().
Discussion
Our meta-analysis found that an early PR in AECOPD patients during recovery did not alter FEV1% predicted, borg dyspnea score and SF-36 mental, but did improve mMRC, 6MWD, SGRQ-total and SF-36 physical when compared with usual care in the early PR group.
Some other research only includes stable COPD patients, usually meaning for at least two months no exacerbation. However, our meta-analysis just included patients who had just experienced an episode of AECOPD. And found early RP improved mobility and prevented muscle atrophy. The results of this preliminary meta-analysis suggest that starting rehabilitation of COPD patients as soon as possible after an exacerbation is useful.
6MWD may have been the favored walking distance that was chosen as the outcome measure. And changes of more than 54 m have been stated to be clinically relevant [Citation25]. Both retrospective and prospective studies have used walking distance as the endpoint. Many results reported that early PR is associated with improvement in 6MWD. Initial 6MWD was predictive of survival in severe COPD patients. Patients with low initial 6MWD achieved poor overall survival at three years [Citation26]. Our meta-analysis showed that the 6MWD was significantly higher in the PR group. Other RCT showed that early PR with AECOPD patients could effectively counterbalance the loss of skeletal muscle function in the hospitalization period. And found that balance and lower limb strength can improve with an early PR in AECOPD patients [Citation27].
Our meta-analysis found that PR could improve breathlessness as measured by scores of mMRC. This is consistent with skeletal muscle dysfunction leads to activity reduction in COPD patients. PR improves exercise tolerance and health-related quality of life, alleviates fatigue and dyspnea, and reduces mortality and hospital readmission [Citation28]. Some PR included therapist-assisted stretching of the respiratory muscles before starting PR to relieve dyspnea. Stretching the respiratory muscles can decrease the chest wall stiffness and expand expiratory flow. And reduce hyperinflation of the lungs at rest. This effect improves the mobility of the diaphragm and consequently greater the exercise capacity [Citation29]. So PR can lead to less dyspnea as measured by mMRC.
The PR group reported a more remarkable improvement in the SGRQ-total. This may be due to the exercise making them more self-sufficient and helping the patients to break the deterioration of functional capacity, which causes heavier dyspnea.
We found that Moderate-to-high-intensity exercise with a compromised respiratory function may be inappropriate for AECOPD. Low-intensity activity has been found to benefit acutely ill patients. It was feasible and safe for COPD patients admitted with an exacerbation to have early inpatient-outpatient rehabilitation. After the hospital-based training in acutely ill patients, overall dyspnea assessed by mMRC was significantly reduced. But the improvement was reached in about ten days. Even a low regular exercise can lead to a persistent reduction in dyspnea. So a home-based training could be maintained after discharge. And early inpatient-outpatient rehabilitation reduced COPD related readmissions, length of hospital stays, and mortality [Citation9]. A randomized controlled trial found that early pulmonary rehabilitation after AECOPD led to a better improvement in the incremental shuttle walk test compare to rehabilitation initiated two months after discharge [Citation30]. A period of low-level chest physiotherapy and breathing retraining may have beneficial effects on SF-36 physical and SGRQ-total. Less strenuous exercise performed with minimal facilities provide improvement in SF-36 physical and SGRQ-total. The SF-36 mental remained unchanged in both groups. But patients can undertake a more intensive exercise to achieve the greatest benefit.
Our study observed that quadriceps muscle strength was increased by PR and may underlie the observed increase in exercise capacity. And we found that physiological or psychological changes brought about by the PR were responsible for improving healthcare utilization. An increase in quadriceps strength following PR is usually achieved by increased volitional drive. The maximum isometric voluntary contraction force was associated with the twitch response to femoral nerve stimulation. Whole-body muscle mass was similar, so competing could involve a change in muscle fiber orientation [Citation31].
Some study has shown that tiotropium could provide benefit with sustained improvement in health status and lung function, reduced exacerbations and hospitalizations [Citation32, Citation33]. But patients in our meta-analysis were used the same drugs at the baseline between the two groups. The improvement in mMRC and 6MWD suggests the possibility that patients may have been suboptimally treated with bronchodilators before beginning rehabilitation. We carefully adjusted every included RCT and found patients in both treatment and control groups stayed on the same medications throughout the study. The FEV1% predicted and borg dyspnea score remained unchanged in both groups.
Limitations
Our meta-analysis found it impossible to bind participants and personnel. Patients who participate in PR will feel better psychologically and perform better on the test. So the risk of bias for binding participants was high in our meta-analysis. The rehabilitation interventions varied in types of exercise, frequency of sessions and duration. So statistical heterogeneity could be found between PR and usual care in 6MWD, SGRQ-total and borg dyspnea score.
Conclusion
Our meta-analysis found early PR in AECOPD patients would lead to better 6MWD, mMRC, SGRQ-total and SF-36 physical. But there were no significant effects of the PR group on measures of FEV1% predicted, borg dyspnea score and SF-36 mental compared with the usual care group.
Funding
There has not been any financial support used in the meta-analysis.
Declaration of interest
All authors declare no conflict of interest.
References
- López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14–23. DOI:10.1111/resp.12660
- Crisafulli E, Barbeta E, Ielpo A, et al. Management of severe acute exacerbations of COPD: an updated narrative review. Multidiscip Respir Med. 2018;13:36. DOI:10.1186/s40248-018-0149-0
- Halpin DM, Miravitlles M, Metzdorf N, et al. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J Chron Obstruct Pulmon Dis. 2017;12:2891–2908. DOI:10.2147/COPD.S139470
- Berkius J, Sundh J, Nilholm L, et al. What determines immediate use of invasive ventilation in patients with COPD? Acta Anaesthesiol Scand. 2013;57(3):312–319. DOI:10.1111/aas.12049
- Wageck B, Cox NS, Holland AE. Recovery following acute exacerbations of chronic obstructive pulmonary disease - a review. COPD. 2019;16(1):93–103. DOI:10.1080/15412555.2019.1598965
- Seidel D, Cheung A, Suh ES, et al. Physical inactivity and risk of hospitalisation for chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2012;16(8):1015–1019. DOI:10.5588/ijtld.12.0050
- McCarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;23(2):Cd003793. DOI:10.1002/14651858.CD003793.pub3
- Gloeckl R, Marinov B, Pitta F. Practical recommendations for exercise training in patients with COPD. Eur Respir Rev. 2013;22(128):178–186. DOI:10.1183/09059180.00000513
- Ryrsø CK, Godtfredsen NS, Kofod LM, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD-exacerbations: a systematic review and Meta-analysis. BMC Pulm Med. 2018;18(1):154. DOI:10.1186/s12890-018-0718-1
- Neunhäuserer D, Reich B, Mayr B, et al. Impact of exercise training and supplemental oxygen on submaximal exercise performance in patients with COPD. Scand J Med Sci Sports. 2021;31(3):710–719. DOI:10.1111/sms.13870
- Jones SE, Barker RE, Nolan CM, et al. Pulmonary rehabilitation in patients with an acute exacerbation of chronic obstructive pulmonary disease. J Thorac Dis. 2018;10(Suppl 12):S1390–s1399. DOI:10.21037/jtd.2018.03.18
- Behnke M, Taube C, Kirsten D, et al. Home-based exercise is capable of preserving hospital-based improvements in severe chronic obstructive pulmonary disease. Respir Med. 2000;94(12):1184–1191. DOI:10.1053/rmed.2000.0949
- Cox M, O’Connor C, Biggs K, et al. The feasibility of early pulmonary rehabilitation and activity after COPD exacerbations: external pilot randomised controlled trial, qualitative case study and exploratory economic evaluation. Health Technol Assess. 2018;22(11):1–204. DOI:10.3310/hta22110
- Deepak TH, Mohapatra PR, Janmeja AK, et al. Outcome of pulmonary rehabilitation in patients after acute exacerbation of chronic obstructive pulmonary disease. Ind J Chest Dis Allied Sci. 2014;56(1):7–12.
- Eaton T, Young P, Fergusson W, et al. Does early pulmonary rehabilitation reduce acute health-care utilization in COPD patients admitted with an exacerbation? A randomized controlled study. Respirology. 2009;14(2):230–238. DOI:10.1111/j.1440-1843.2008.01418.x
- He M, Yu S, Wang L, et al. Efficiency and safety of pulmonary rehabilitation in acute exacerbation of chronic obstructive pulmonary disease. Med Sci Monitor. 2015;21:806–812.
- Kirsten DK, Taube C, Lehnigk B, et al. Exercise training improves recovery in patients with COPD after an acute exacerbation. Respiratory Med. 1998;92(10):1191–1198. DOI:10.1016/S0954-6111(98)90420-6
- Ko FW, Dai DL, Ngai J, et al. Effect of early pulmonary rehabilitation on health care utilization and health status in patients hospitalized with acute exacerbations of COPD. Respirology. 2011;16(4):617–624. DOI:10.1111/j.1440-1843.2010.01921.x
- Ko FW, Cheung NK, Rainer TH, et al. Comprehensive care programme for patients with chronic obstructive pulmonary disease: a randomised controlled trial. Thorax. 2017;72(2):122–128. DOI:10.1136/thoraxjnl-2016-208396
- Ko FW, Tam W, Siu EHS, et al. Effect of short-course exercise training on the frequency of exacerbations and physical activity in patients with COPD: a randomized controlled trial. Respirology. 2021;26(1):72–79. DOI:10.1111/resp.13872
- Man WD, Polkey MI, Donaldson N, et al. Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. BMJ (Clin Res ed). 2004;329(7476):1209. DOI:10.1136/bmj.38258.662720.3A
- Seymour JM, Moore L, Jolley CJ, et al. Outpatient pulmonary rehabilitation following acute exacerbations of COPD. Thorax. 2010;65(5):423–428. DOI:10.1136/thx.2009.124164
- Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Am J Med. 2000;109(3):207–212. DOI:10.1016/S0002-9343(00)00472-1
- Murphy N, Bell C, Costello RW. Extending a home from hospital care programme for COPD exacerbations to include pulmonary rehabilitation. Respir Med. 2005;99(10):1297–1302. DOI:10.1016/j.rmed.2005.02.033
- Beaumont M, Losq A, Péran L, et al. Comparison of 3-minute step test (3MStepT) and 6-minute walk test (6MWT) in patients with COPD. COPD. 2019;16(3–4):266–271. DOI:10.1080/15412555.2019.1656713
- Dajczman E, Wardini R, Kasymjanova G, et al. Six minute walk distance is a predictor of survival in patients with chronic obstructive pulmonary disease undergoing pulmonary rehabilitation. Can Respir J. 2015;22(4):225–229. DOI:10.1155/2015/280187
- Torres-Sánchez I, Valenza MC, Cabrera-Martos I, et al. Effects of an exercise intervention in frail older patients with chronic obstructive pulmonary disease hospitalized due to an exacerbation: a randomized controlled trial. COPD. 2017;14(1):37–42. DOI:10.1080/15412555.2016.1209476
- Gloeckl R, Schneeberger T, Jarosch I, et al. Pulmonary rehabilitation and exercise training in chronic obstructive pulmonary disease. Deutsch Arzteb Int. 2018;115(8):117–123.
- Wada JT, Borges-Santos E, Porras DC, et al. Effects of aerobic training combined with respiratory muscle stretching on the functional exercise capacity and thoracoabdominal kinematics in patients with COPD: a randomized and controlled trial. COPD. 2016;11:2691–2700. DOI:10.2147/COPD.S114548
- Kjaergaard JL, Juhl CB, Lange P, et al. Early pulmonary rehabilitation after acute exacerbation of COPD: a randomised controlled trial. ERJ Open Res. 2020;6(1):00173-2019. DOI:10.1183/23120541.00173-2019
- Kortianou EA, Papafilippou EK, Karagkounis A. Respiratory, cardiac and metabolic responses during electrical muscle stimulation in quadriceps muscle versus comparable voluntary muscle contractions. Scand J Clin Lab Invest. 2021;81(1):12–17. DOI:10.1080/00365513.2020.1846210
- Zhou Y, Zhong NS, Li X, et al. Tiotropium in early-stage chronic obstructive pulmonary disease. N Engl J Med. 2017;377(10):923–935. DOI:10.1056/NEJMoa1700228
- Anzueto A, Miravitlles M. Tiotropium in chronic obstructive pulmonary disease - a review of clinical development. Respir Res. 2020;21(1):199. DOI:10.1186/s12931-020-01407-y