Abstract
Patients with chronic obstructive pulmonary disease (COPD) may have a limited level of physical activity in daily life (PADL) and health-related quality of life (HRQOL). The interrelationships of these variables should be measure by cluster analysis to characterize this population and enable rehabilitation programs to target each patient profile identified. This study investigates different phenotypes in COPD according to PADL and HRQOL. A cross-sectional study with cluster analysis was done, in which 76 people with COPD were submitted to measurements to characterize the sample on first day, followed by used of physical activity monitor, which was worn for 7 days. After 7 days, the six-minute walk test (6MWT) and HRQOL questionnaires were applied (St. George’s Respiratory Questionnaire). The main results: three phenotypes were identified (A, B and C), with phenotype A who exhibited an inactive physical activity level and HRQOL scores above the value deemed satisfactory, phenotype B those with active physical activity level and poor HRQOL scores, and phenotype C subjects with inactive physical activity level and HRQOL scores but the value is close to cutoff point. To conclude, three phenotypes were found, with one indicating disproportionality between PADL and HRQOL.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by dyspnea due to airflow limitation and systemic manifestations, such as musculoskeletal, cognitive, nutritional and cardiovascular impairments [Citation1]. Disease progression can alter patients’ clinical condition, which ultimately limits their performance and level of physical activity in daily life (PADL), and impairs their self-reported health-related quality of life(HRQOL), leading to a greater risk of mortality and morbidity [Citation2].
Cluster analysis may be a way to understand the interrelationships between these important variables, and it is widely used in the literature to investigate phenotypes in order to better understand how the clinical characteristics of individuals in different chronic diseases are grouped [Citation3]. Other studies have also identified phenotypes for COPD and found as phenotype determinants peripheral muscle strength, body composition, physical activity level [Citation3], prognosis [Citation4], symptoms, quality of life [Citation2] and airflow obstruction severity [Citation5].
Once characteristic grouping of these individuals has been identified with cluster analyses, the literature recommends [Citation6] that the patients be referred to treatments, as pulmonary rehabilitation programs, to prevent and treat the disorders; however, current intervention models still are developed using a standard protocol, which might not address different groups needs and goals, despite the clinical relevance.
Thus, considering the complex interrelationships between the different aspects previously mentioned, a question is raised of whether pulmonary rehabilitation programs should target each patient profile identified for the different clinical characteristics in order to obtain better results than conventional rehabilitation [Citation7] Overall the literature review presented in this section indicates the need for a more detailed analysis of the phenotypes involved in PADL and HRQOL. As such, this article aims to investigate and describe different phenotypes in patients with COPD according to PADL and HRQOL.
Methods
Study design and participants
This is a cross-sectional study (following the recommendation from the Strengthening the Reporting of Observational studies in Epidemiology- STROBE statement) with prospective data collection, conducted at two e Pulmonology Outpatient Clinic in Brazil. The study was conducted according to the guidelines established in the Declaration of Helsinki and all procedures involving human beings were approved by the Research Ethics Committee of the Federal University of São Carlos (CAAE: 85901318.0.0000.5504).
Individuals with age between 60 and 75 years and with clinical and spirometric diagnosis of COPD were included in the study. Exclusion criteria were: i) body mass index (BMI) >35 kg/m2; ii) hemodynamic instability; iii)change in medications; iv) clinical stability (no exacerbation in the last 2 months); v) presence of contraindications for the 6MWT [Citation8], skin problems that prevent attachment of the physical activity monitor to the lower limb; and vi) inability to understand the questionnaires/explanations.
Data collection procedure
Data were collected on two different occasions. The first consisted of clinically characterizing the patients, applying the pulmonary function test and fixing the physical-activity monitor. Seven days after the initial assessment, participants underwent two 6MWT, quality of life questionnaires (St. George’s Respiratory Questionnaire) and removal of the physical-activity monitor.
Measures
Sample characterization
Information was collected on the patients’ anthropometric data, schooling level, presence of continuous use of oxygen therapy, ongoing pulmonary rehabilitation, active smoking and comorbidities (Charlson Comorbidity Index).
Pulmonary function
Spirometry was conducted in accordance with Brazilian recommendations [Citation9]. Disease severity criteria were defined based on the GOLD report classification (2020) [Citation1].
Assessment of health-related quality of life (HRQOL) was composed of:
St. George’s respiratory questionnaire (SGRQ)
This instrument has been validated for the Brazilian population [Citation10] and consists of 76 items covering three domains (symptoms, activity and impact).
Each domain is scored from 0 (no decline in quality of life) to 100 (maximum decline in quality of life). It should be noted that the GOLD report (2020) [Citation1] established scores higher than 25 as a cutoff point to identify poor QRQOL and symptomatic patients in need of intervention. So, values above of 25 is considered satisfactory HRQOL.
Monitoring levels of physical activity in daily life (PADL)
PADL level was assessed using a light, compact (35x53x7mm and 20 g) activity monitor (activPAL3TM, PAL Technologies Ltd., Glasgow, United Kingdom). The device was fixed to the middle third of the participant’s thigh using transparent impermeable adhesive film dressing, which did not need to be removed for showering. It remained fixed for seven consecutive days, 24 h a day, but data from the first and last days (fixed and removal, respectively) were excluded from analysis.
The average value of the five collection days was used in analysis, for the following variables of interest: active time (min/day), walking time (min/day), standing time (min/day), sitting/lying time (min/day), and step number (active person is defined by 7000-8000 or more steps/day)[Citation11, Citation12]. Additionally, the intensity of physical exercise was measured in METS (metabolic equivalents), based on the time (min/day) that patients remained at certain intensities, and classified as mild (≤1.5 METS), moderate (1.5 to 3 METS) and intense (≥ 3 METS). The time that participants remained within each of the intensity ranges was calculated using a script developed with MATLAB software (MATLAB version 9.6.0. Natick, Massachusetts: The MathWorks Inc., 2019.) Poor physical activity is characterized by less than 7182 steps and low intensity of exercise.
Bode index
The index was calculated by adding the scores for its four variables: predicted FEV1 percentage after bronchodilation (0 to 3 points), body mass index (0 to 1 point), distance walked in the 6MWT (0 to 3 points), and the modified MRC dyspnea scale (0 to 3 points). The total score ranges from 0 to 10, with high scores indicating a greater chance of mortality and risk of acute exacerbation [Citation13].
Six-minute walk test (6MWT)
Two 6MWTs were performed using the standardized technique [Citation8], considering the greatest distance between the two tests for statistical analysis.
Statistical analysis
We conducted a partitioning around medoids (PAM) with an estimation of the number of clusters analysis using physical activity in daily life and health-related quality of life measures. The ideal number of clusters (k) was determined by silhouette analysis and the internal stability of each cluster was tested using the Jaccard index (Supplementary analysis). Once the number of clusters and the median distance between each cluster’s median point was established, patients were classified into groups according to proximity functions by PAM algorithm clustering.
Continuous data are presented as mean (standard deviation) or median [interquartile range], based on the Shapiro-Wilk test for normality. Categorical variables are presented as counts and percentages. Intergroup comparisons were performed using the Kruskal-Wallis test, followed by a post hoc Dunn test with the Bonferroni correction for continuous variables and Pearson’s chi-squared test with Yates’ continuity correction for categorical variables. Statistical significance was assessed at a two-tail p-value of < 0.05. All analyses were conducted using R 3.6.1 software (The R Project for Statistical Computing, Vienna, Austria) in R version 1.3.443 (RStudio Inc., Boston, MA, USA).
We used Dalmaijer et al. (2020) recommendations to calculate the minimum sample size. Accordingly, sufficient statistical power can be achieved with 20 observations per cluster expected by theoretical arguments and considering a relatively large cluster separation. We assumed that HRQOL assessments could identify at least three phenotypes of COPD patients: (1) active physical activity level and HRQOL scores above the value deemed satisfactory; (2) active physical activity level and poor HRQOL scores; and (3) poor physical activity levels and HRQOL scores.
Results
A total of 82 participants were included, but 6 withdrew before the second assessment (transportation or time difficulty), with the final sample consisting of 76 individuals. According and Supplementary analysis: Cluster-wise assessment of cluster stability, the majority were men (58%), with an average age of 67 ± 8 years and a history of current or past smoking (100%). Around 12% used oxygen therapy at home and 89% had never taken part in a pulmonary rehabilitation program. According to the GOLD criterion (2020)[Citation1], most subjects had moderate to severe airflow obstruction (82%, 63/76) and were symptomatic. With respect to PADL, all the participants remained largely at a mild intensity of exercise.
Table 1. Characteristics COPD and the three identified phenotypes on the cluster analyses.
Cluster analysis identified three phenotypes (A, B and C), according to PADL and HRQOL. Phenotype A clustered patients who exhibited an inactive physical activity level and HRQOL scores above the value deemed satisfactory, phenotype B those with activity physical activity level and poor HRQOL scores, and phenotype C subjects with inactive physical activity level and HRQOL scores but the value is close to cutoff point and the most patients were active.
There was no significant difference between the phenotypes for the variables sex, smoking habits, history of pulmonary rehabilitation, comorbidities, schooling level and BMI. With respect to age, phenotypes B and C obtained lower and statistically different values when compared to phenotype A. For BODE score, a significant difference was identified between phenotypes A with C and A with B (p = 0.05).
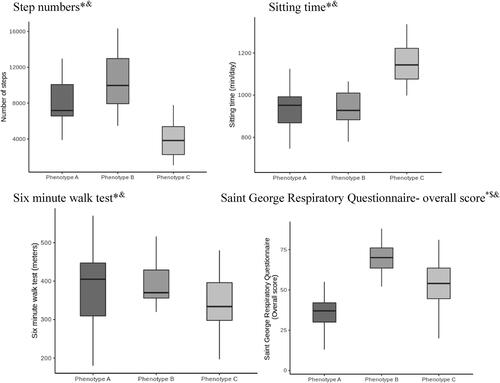
Phenotypes A, B and C were different in PADL assessment, but statistically different when compared phenotype A to B and C and B to C for the variables sitting time, walking time, and step numbers (all at p < 0.01). There was no statistically significant difference between phenotypes for METS >3.0 because only 2 patients reached this exercise intensity. For distance walked in the 6MWT, a significant difference was observed between phenotypes A and C (p = 0.02), and A and B (p = 0.03) ( and ).
Discussion
In the present study, analysis of the clustering trends of patients with COPD, based on objective and patient-centered assessments, indicated that the variables that influenced phenotype construction were HRQOL, assessed by SGRQ and PADL. On separating the phenotypes, other variables that differed between groups were identified, such as age, the BODE index, exercise intensity and 6MWT.
The variables PADL and SGRQ enabled clustering into three phenotypes (A, B and C).Regarding PADL, B and C were similar for all studied variables, however, once again, phenotype A differed in that the subjects engaged in less intense exercise (longer at 1.5 METS and less time at 1.5 to 3 METS), took fewer steps and spent more time sitting. Similar behavior was observed in the 6MWT, with patients from B and C obtaining similar results and differing from those in phenotype A, who walked shorter distances. In line with our findings that patients with poor functional capacity also exhibited low physical activity levels, previous studies have demonstrated an association between the 6MWT and walking time (r = 0.42; p = 0.007), exercise intensity (r = 0.64; p = 0.0001) and step numbers, assessed by accelerometry [Citation14, Citation15].
Phenotype A patients obtained higher BODE and mMRC scores and therefore a worse prognosis and more symptoms than those in group B or C. Thus, participants from B had C had a better prognosis and less symptom than their phenotype A counterparts, who also displayed lower exercise intensity and a worse prognosis factor, as observed in a study by Mesquita et al. (2017)[Citation4]. Thus, these findings reinforce the concept that patients with worse exercise intensive have a worse prognosis and higher symtoms. However, the present study identified other variables in the characteristics of patients with COPD that differed between clusters, such as HRQOL.
In terms of the impact of the disease on quality of life, it is strongly associated with PADL[Citation16], which was confirmed in the present study on phenotype A, with that exhibiting worse QRQOL and PADL than the latter. However, this was not observed for patients in phenotype B, who, despite showing a better prognosis and obtaining higher physical activity levels, but the perceived the disease as having a worse impact on their quality of life and the phenotype C that represents a poor QRQOL and the most patients were normal physical activity levels. In a study by Xavier et al. (2018)[Citation2], one phenotype also exhibited disproportionality between quality of life and physical activity level, obtaining better and worse results, respectively. Thus, the main concept of this study shows that there is no linearity between the PADL and QRQOL variables when considering the individual clinical characteristics (phenotypes).
Previous studies have added that, in some situations, disproportionality about HRQOL and PADL may also be explained by age since, despite their chronic disease and physical limitations, older patients have better perceived HRQOL because they view aging as inevitable and linked to health problems and restrictions in everyday activities [Citation3, Citation17]. By contrast, younger individuals may find it difficult to accept reduced HRQOL and therefore tend to view limitations in their daily activities negatively, despite trying to perform them every day.
Given the no linearity between HRQOL and PADL and the response of other variables (6MWT, mMRC and BODE index) verified on cluster analyses, suggest that it may be beneficial to design pulmonary rehabilitation programs to target defined patient profiles.
So, the article suggests that the cluster analysis findings could be used to help focus rehabilitation programmer. Therefore, strategies of behaviors changes with multidisciplinary teams (as physiotherapist, psychologist, occupational therapist and psychiatrist) should be incorporated on rehabilitation program with aimed at each profile identified, as observed for the three phenotypes in the present study.
To conclude, three phenotypes were identified according to PADL and HRQOL, with one exhibiting disproportionality between these variables, suggesting a different therapeutic approach for these patients. Is important to emphasize that this is a primary study that identified important clinical characteristics to amplify and target the rehabilitation program in people with COPD. And this early research could be a precursor to future research that verify the results of different strategies of rehabilitation targeting these phenotypes
Limitation
This study had some limitations, including a restricted population (about restrictive area and severity of airflow limitation), and the absence of research tools that assess other dimensions of psychological state that could better explain the disproportionality between HRQOL and PADL in phenotype B. However, the study identified the phenotypes its possibility of recommending specific treatments of pulmonary rehabilitation, which should be tested by future studies of rehabilitation program.
Data availability statement
Data availability on university database.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Marcela Maria Carvalho da Silva
Marcela Maria Carvalho da Silva: Literature search, Data collection, Study design, Analysis of data, Manuscript preparation and Review of manuscript and final approval of the version to be submitted.
Juliano Ferreira Arcuri
Juliano Ferreira Arcuri: Literature search, Study design, Analysis of data, Manuscript preparation and Review of manuscript and final approval of the version to be submitted.
Henrique Pott
Henrique Pott Jr: Study design, Analysis of data, Manuscript preparation and Review of manuscript and final approval of the version to be submitted.
Anna Claudia Sentanin
Anna Claudia Sentanin: Data collection, Manuscript preparation and Review of manuscript and final approval of the version to be submitted.
Francisco José Barbosa Zorrer Franco
Francisco José Barbosa Zorrer Franco: Study design, Analysis of data, Manuscript preparation and Review of manuscript and final approval of the version to be submitted.
Luiz Henrique Pessôa da Costa Trondoli
Luis Henrique Pessôa da Costa Trondoli: Study design, Analysis of data, Manuscript preparation, Review of manuscript and final approval of the version to be submitted.
Valéria Amorim Pires Di Lorenzo
Valéria Amorim Pires Di Lorenzo: Literature search, Data collection, Study design, Analysis of data, Manuscript preparation and Review of manuscript and final approval of the version to be submitted. All authors have significantly contributed, read and approved the manuscript.
References
- Global Strategy for diagnosis, manegent and prevention of Chronic Obstructive Lung Desease (2020 Report). 2020 Glob Initiat Chronic Obstr Lung Dis Inci; 2020.
- Lopes AC, Xavier RF, Carolina A, et al. Identifying COPD patients at risk for worse symptoms, HRQoL, and self-efficacy: a cluster analysis. Chronic Illn. 2018;0:1–11.
- Xavier RF, Pereira ACAC, Lopes AC, et al. Identification of phenotypes in people with COPD: Influence of physical activity, sedentary behaviour, body composition and skeletal muscle strength. Lung [Internet]. 2019;197(1):37–45. DOI:10.1007/s00408-018-0177-8
- Mesquita R, Spina G, Pitta F, et al. Physical activity patterns and clusters in 1001 patients with COPD physical activity patterns and clusters in 1001 patients with COPD. Chron Respir Dis. 2017;14:1–14.
- Torres JD, Marin J, Martinez-gonzalez CR, et al. The importance of symptoms in the longitudinal variability of clusters in COPD patients: a validation study. Respirology. 2017;23(5):485–491. DOI:10.1111/resp.13194.
- Garvey C, Bayles MP, Hamm LF, et al. Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary Disease: Review of Selected Guidelines: An official statement from the American Association of Cardiovascular and Pulmonary Rehabilitation. J Cardiopulm Rehabil Prev. 2016;36(2):75–83. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=01273116-201603000-00001. DOI:10.1097/HCR.0000000000000171
- Langer D, Probst V, Pitta F, et al. Clinical practice guideline for physical therapy in patients with chronic obstructive pulmonary disease (COPD). Rev Bras Fisioter. 2009;13(3):183–204. DOI:10.1590/S1413-35552009005000034
- Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–1446. Available from: https://www.thoracic.org/statements/resources/copd/FWT-Tech-Std.pdf. DOI:10.1183/09031936.00150314
- Pereira CADC. Espirometria. J Bras Pneumol. 2002;28:S1–S82.
- SOUSA TCD, JARDIM JR, JONES PAUL. Validação do Questionário do Hospital Saint George na Doença Respiratória (SGRQ) em pacientes portadores de doença pulmonar obstrutiva crônica no Brasil * validation of the Saint George‘s respiratory questionnaire. J. Pneumologia. 2000;26(3):119–128. DOI:10.1590/S0102-35862000000300004
- Demeyer H, Burtin C, Van Remoortel H, et al. Standardizing the analysis of physical activity in patients with COPD following a pulmonary rehabilitation program. Chest [Internet]. 2014;146(2):318–327. DOI:10.1378/chest.13-1968
- Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8(1):80. DOI:10.1186/1479-5868-8-80
- Mantoani LC, Hernandes NA, Guimarães MN, et al. Does the BODE index reflect the level of physical activity in daily life in patients with COPD? Rev Bras Fisioter. 2011;15(2):131–137. DOI:10.1590/s1413-35552011000200008
- Eliason G, Zakrisson A, Piehl-aulin K, et al. Physical activity patterns in patients in different stages of chronic obstructive pulmonary disease. COPD J Chronic Obstruct Pulm. 2011;8(5):369–374. DOI:10.3109/15412555.2011.605403
- Hernandes NA, Teixeira DDC, Probst VS, et al. Profile of the level of physical activity in the daily lives of patients with COPD in Brazil. J Bras Pneumol. 2009;35(10):949–956. DOI:10.1590/S1806-37132009001000002
- Miravitlles M, Cantoni J, Naberan K. Factors associated with a low level of physical activity in patients with chronic obstructive pulmonary disease. COPD J Chronic Obstr Pulm Dis. 2014;192(2):259–265. DOI:10.1007/s00408-014-9557-x
- Laudański K, Nowak Z, Nowak Z. Age-related differences in the quality of life in end-stage renal disease in patients enrolled in hemodialysis or continuous peritoneal dialysis. Med Sci Monit. 2013;19:378–385. DOI:10.12659/MSM.883916