ABSTRACT
This systematic review and meta-analysis aimed to assess the association between athletic performance and periodontal disease (PD). Observational studies published up to April 2022 were searched in online databases (PubMed, Scopus, Web of Science, The Cochrane Library, LILACS, OpenGrey, and Google Scholar). PECO statement focused on studies with professional athletes (Participants) with PD (Exposition) compared to those with healthy periodontium (Comparison) and its effects on sports performance (outcome). Searches were conducted according to the PRISMA guidelines (registration protocol: 10.17605/OSF.IO/7ADH6) and risk of bias evaluation according to the Joanna Briggs Institute checklist. A total of 793 references were retrieved, of which eight were considered eligible. Two studies did not show an association between clinical PD parameters and performance. A meta-analysis with 396 participants suggested a relationship between PD and self-reported reduction in sports performance (odds ratio [OR] = 1.55; 95% confidence interval [CI] 1.04–2.31; p = 0.03; I2 = 0%) with moderate quality of evidence accordingly GRADE analysis. Despite the differences in performance evaluations between studies, PD was associated with reduced self-reported sports performance. Additional studies assessing confounding factors and objective assessment of PD and performance are needed to clarify the real effect of both conditions.
Introduction
Athletic performance refers to the efforts made by athletes to achieve specific performance goals. Skill, strength, endurance, and recovery are four significant sports performance dimensions (Handelsman, Citation2016). A particular combination of these features may result in maximum performance at different exercises. Many diseases, such as oral diseases, may affect an athlete’s physiological, psychological, and functional abilities, resulting in a lower quality of life and, consequently, a lower level of performance (Ashley et al., Citation2015). Continuing healthcare assistance is, therefore, one of many methods to manage athletes’ health and ensure that these dimensions are balanced to achieve better performance, especially during competitive seasons (Needleman et al., Citation2014).
Periodontal disease is a multifactorial inflammatory disease of the dental supporting tissues (gingiva, periodontal ligament, cement, and alveolar bone) and one of the most prevalent oral diseases in the worldwide population (Oppermann et al., Citation2015). Despite its widespread occurrence, healthcare providers often overlook the impact of periodontal disease on overall health. In fact, mild signs of periodontal diseases, such as bleeding during flossing and swelling, affect approximately half of the adults aged 30 and older (Genco & Sanz, Citation2020). In contrast, severe signs such as dental mobility and tooth loss are common among individuals aged 65 and older (Oppermann et al., Citation2015). Addressing the prevention and management of periodontal disease is essential for maintaining oral and overall health, yet it is often overlooked. The high prevalence of periodontal disease may be related to its low symptomatic status because, in most cases, there is no pain in the dental supporting tissues (Genco & Sanz, Citation2020). Thus, mild or moderate conditions may be neglected or masked by smoking or conditions such as diabetes (Genco & Sanz, Citation2020). Due to its multifactorial nature, periodontal disease is influenced by variables intrinsic to individuals and environmental and behavioural factors such as smoking, self-care, and hygiene (Meyle & Chapple, Citation2015).
In periodontal disease, dysbiotic dental biofilm triggers a host immune response and may be a potential cause of inflammation leading to possible systemic alterations (Ferreira et al., Citation2019; Zhao et al., Citation2018; Ferreira de Brito Silva et al., Citation2019). Without regular debridement, plaque accumulation can elevate the risk of periodontal damage and increase proinflammatory mediators, such as IL-1B, IL-6, C-reactive protein, and TNF-a (Ebersole et al., Citation2017). Some of these biomarkers are related to muscle fatigue, risk of sports injuries, and persistent inflammation status in high-intensity exercise practitioners (Lee et al., Citation2017). Therefore, it begs the question: could periodontal inflammation contribute to increased exercise-induced inflammation and the risk of injuries? Studies show that athletes with signs and symptoms of periodontal disease are more likely to experience recurrent injuries (Ford et al., Citation2017), a significant concern for athletes and technical staff (Solleveld et al., Citation2015). Poor oral hygiene is common among athletes, and many struggle to access preventive care, leading to a high prevalence of the periodontal disease among sports practitioners (Gallagher et al., Citation2020; Needleman et al., Citation2014). These findings underscore the importance of oral hygiene and regular dental care for athletes to reduce the risk of injury and maximize performance.
To maintain a high level of performance, athletes must manage small physiological and psychological changes that can impair their abilities. This necessitates careful health management, including monitoring signs and symptoms of easily preventable diseases such as periodontal disease (Gallagher et al., Citation2019). Since periodontal disease significantly influences systemic health, we hypothesized that it might affect athletes’ performance variables related to skills, strength, endurance, or recovery. This systematic review investigated the association between periodontal disease and athletic performance.
Materials and methods
Registration protocol and study design
This systematic review was conducted according to The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (Page et al., Citation2021) (S1). The PRISMA criteria were followed after obtaining a registration code from Open Science Framework (10.17605/OSF.IO/7ADH6).
Eligibility criteria, search strategy, and data extraction
After developing a PECO statement that focused on comparisons between professional athletes (participants) with periodontal disease (exposure) and those with a healthy periodontium (comparison) and the effects of periodontal disease on sports performance (outcome), observational studies published until April 2022 were searched for in online databases. This study defined sports performance as any factor affecting an athlete’s skills, strength, endurance, or recovery (Handelsman, Citation2016). No restrictions were placed on the type of sports. Cross-sectional, case-control and cohort studies were included in the search.
Regarding performance definition, several qualitative and quantitative variables can assess sports performance by analysing an athlete’s health state, psychological status, training level, nutrition, as well as a sport technique and genetic heritage (D’Isanto et al., Citation2019). Body composition measurements (body mass index, skinfold measurements, bioelectrical impedance, etc.), blood and muscle biomarkers (CRP, creatine kinase, IL-1) (Lee et al., Citation2017), and categorical outcomes (win/loss, quality of life, presence/absence of self-reported issues or injuries) (Houston et al., Citation2016; Lochbaum et al., Citation2022) were considered for this review. To assess periodontal health, variables considered in this review were: gingival index > 30% of teeth, bleeding on probing (BOP >25% of sites), probing pocket depth, and plaque index (Papapanou et al., Citation2018). Secondary variables of periodontal health were the basic periodontal examination index, community periodontal index (CPI), community periodontal index of treatment needs (CPITN), and self-report periodontal issues, such as bleeding while flossing/brushing or gum swelling (Gallagher et al., Citation2017).
A search was conducted in the databases of PubMed, Scopus, Web of Science, Cochrane Library, and LILACS. Gray literature was also evaluated using OpenGrey and Google Scholar. Combined searches with “athletes” or “exercise” and “periodontitis” or “periodontal disease” or “gingivitis” and “sports performance” employed a combination of controlled pre-defined MeSH (Medical Subject Headings) and free terms linked to athletes, periodontal disease, and sports performance. Supplementary File 2 shows the search strategy for the selected databases. Differences in database syntax rules were accounted for when executing a combination of pre-defined phrases.
We employed a reference manager (EndNote, x9 version, Thomson Reuters) to save the retrieved citations in all databases. Duplicate results were eliminated, and only one citation for each article was considered. Opinion papers, technical articles, guidelines, and animal experiments were excluded because their titles and abstracts did not meet the eligibility criteria. The full texts of the remaining papers were evaluated to select the relevant articles. Citations from the reference lists of previously selected articles were also assessed using full-text analysis. All database searches were completed by two examiners (ROF and DRF). In disagreement, the articles were examined by a third examiner (RRL).
Data extraction was performed for the selected publications. shows the publication year, study design, participant characteristics (source and sample size), age, periodontal assessment, sports performance assessment, and outcomes. An attempt was made to contact the authors via email if the lack of information affected data extraction or the risk of bias evaluation. The attempt consisted of sending a weekly email for up to 5 consecutive weeks.
Table 1. Data extracted from the selected studies.
Quality assessment analysis and risk of bias
The Joanna Briggs Institute’s checklist for prevalence studies was used to evaluate the methodological quality and risk of bias. The study samples, measurement quality, confounding factor identification, outcome analysis, and statistical analysis were all part of the analysis (Moola et al., Citation2017). The response “No” was assigned to significant issues related to the assessed criteria or to criteria without a description. When there was no clear description of a criterion in the study, the response “unclear” was used. If there were no problems with the criterion, the response “yes” was used. Analyses that were not applicable owing to the study’s design was also checked, but with the notation “NA.” lists all the assessment criteria.
Table 2. Quality assessment of methods and risk of bias for selected studies.
After analysing the checklist domains, an overall statement adapted for this review was written. If “yes” was selected for all domains, the study was labelled as having a “low risk of bias.” If one or two criteria were marked as “unclear,” the study was labelled as showing “some concerns.” The study was labelled as having a “high risk of bias” if “no” was applied to at least one domain or if “unclear” statements were used to multiple parts in a way that resulted in a low-confidence result in the outcome.
Quantitative synthesis
RevMan software (Review Manager, version 5.3, The Cochrane Collaboration; Copenhagen, Denmark) was used to analyse the extracted data to determine the relationship between periodontal disease and self-perceived sports performance measured by the oral impact on daily performance (OIDP) questionnaires. The presence of periodontal disease (events) was investigated in a meta-analysis, and the total number of participants in the case (performance effect) and control (no performance effect) groups were included in determining the odds ratio (OR) with the 95% confidence interval (CI). Random-effects models would be used if the studies were not methodologically equivalent (Borenstein et al., Citation2021). The meta-analysis aimed to generalize the findings, and heterogeneity was assessed using the I2 index. If the heterogeneity was high or considerable, implicating many differences among studies’ methodologies, participants, risk of bias, or outcomes measurements (Chang et al., Citation2022); sensitivity analyses were performed to assess and validate the influence of individual studies or groups of studies on the pooled results (50%–100%) (Higgins et al., Citation2016). A funnel plot was created, if appropriate, to indicate a possible publication bias. Only papers with a “low risk of bias” or “some concerns” were considered in the quantitative analysis. If any selected papers had omitted part of the information needed for the meta-analysis, the authors were contacted and asked to provide missing data.
Quality of evidence assessment
The quality of the evidence (certainty in the estimates of effect) for the outcome “periodontal disease impact on performance” was determined using the GRADE approach (Ryan & Hill, Citation2016), in which observational studies begin with moderate quality of evidence and the quality of, or certainty in, the body of evidence decreases to low or very low quality if serious or very serious issues, such as risk of bias, inconsistency, or indirectness, are identified. Furthermore, if the magnitude of the effect is high or very large, or if the effect of all conceivable confounding factors is to lower the effect or suggest a spurious effect, the quality of the evidence can be improved. Consequently, the quality of evidence can range from very low to high.
Results
Study selection and characteristics
Of the 793 references identified in the database searches, 258 duplicates were removed. After reading the titles and abstracts, 521 of the remaining 535 references were excluded based on the eligibility criteria; thus, 14 references were selected for full-text appraisal. Subsequently, one study was excluded since it evaluated police officers (Hoppe et al., Citation2017), three were excluded since they did not include periodontal evaluations (Mendes et al., Citation2012; Solleveld et al., Citation2018; Suzuki & Toyoda, Citation2015); and two were excluded since they performed an assessment of Olympic athletes without a performance evaluation (Opazo-García et al., Citation2021; Oredugba & Perlman, Citation2010) (See Supplementary file 3). Finally, eight articles were eligible for qualitative evaluation ().
Results of individual studies
Eight cross-sectional studies were included in this meta-analysis. The relationship between periodontal disease and sports performance was demonstrated in six studies (Alshail et al., Citation2016; Botelho et al., Citation2021; Gallagher et al., Citation2018; Gay-Escoda et al., Citation2011; Needleman et al., Citation2016; Solleveld et al., Citation2015). However, two studies found no association between periodontal disease parameters and sports performance or injuries (Kragt et al., Citation2019; Needleman et al., Citation2013). The participants’ ages ranged from 16 to 47 years. Three studies analysed national athletes before or during competitions in various sports, including track and field, boxing, hockey, swimming, water polo, judo, volleyball, shooting, football, weightlifting, fencing, archery, handball, beach volleyball, taekwondo, wrestling, cycling, basketball, canoeing, gymnastics, equestrian, sailing, table tennis, rowing, and badminton (Kragt et al., Citation2019; Needleman et al., Citation2013).
One study evaluated practitioners of athletics, track and field, gymnastics, cycling, swimming, rowing, sailing, football, rugby/sevens, and hockey (Gallagher et al., Citation2018). Finally, five studies only evaluated soccer athletes (Alshail et al., Citation2016; Botelho et al., Citation2021; Gay-Escoda et al., Citation2011; Needleman et al., Citation2016; Solleveld et al., Citation2015).
The clinical and oral health/periodontal parameters reported in the selected studies were: probing pocket depth (PPD), bleeding on probing (BOP), Löe and Silness gingival index (GI), community periodontal index and treatment needs (CPITN), basic periodontal examination (BPE), and self-reported gum problems. Primary features of periodontal assessment are bleeding on probing (BOP) and clinical attachment loss (CAL). Then, only one study did not evaluate periodontal disease with more precision since its used self-report gum problems (Solleveld et al., Citation2018). All indexes reported have the evaluation of CAL and BOP. For sports performance assessment, studies focused in two major features: 1 - physiological variables such as serum levels of creatine kinase (CK) and medical records of extrinsic and intrinsic injuries, and 2- Questionnaire instruments to highlight how oral health problems affects performance and quality of life (OIDP questionnaire) and also self-reported questionnaire scores about repeated exercise-associated muscle cramps (REAMC), muscle or tendon reinjury (MTR), and other multiple types of injuries.
For performance analysis, the studies investigated serum CK levels, muscle and articular injuries, increased risk for damages, and a range of self-reported OIDP questionnaires. Therefore, some studies demonstrated that periodontal disease is associated with higher levels of serum CK (Alshail et al., Citation2016), muscle injuries (Gay-Escoda et al., Citation2011), self-reported sports performance impact (Gallagher et al., Citation2018), and risk of injuries (Solleveld et al., Citation2015). Regarding the type of sport, soccer showed relationships with periodontal disease possibly because it was the major sport evaluated (Alshail et al., Citation2016; Botelho et al., Citation2021; Gay-Escoda et al., Citation2011; Needleman et al., Citation2016; Solleveld et al., Citation2015). Olympic sports did not show such associations, but the authors reported limitations related to the low response rate of participants and participant sampling for medical assistance care (Kragt et al., Citation2019; Needleman et al., Citation2013).
Methodological quality of studies
Six of the eight studies identified a relationship between periodontal disease and athletic performance (Alshail et al., Citation2016; Botelho et al., Citation2021; Gallagher et al., Citation2018; Gay-Escoda et al., Citation2011; Needleman et al., Citation2016; Solleveld et al., Citation2015). Most problems among studies were related to sampling methods, clear description of eligibility criteria, clear description of study participants, the validity of condition measurements, and cofounding factor management. Regarding sampling methods, one study selected participants who needed dental healthcare during competitions (Needleman et al., Citation2013). Four studies recruited participants through questionnaires sent to sports organizations (Gallagher et al., Citation2018; Kragt et al., Citation2019; Needleman et al., Citation2016; Solleveld et al., Citation2015). Two studies selected a sample from a single sports organization (Botelho et al., Citation2021; Gay-Escoda et al., Citation2011). Additionally, one study did not describe the sampling method (Alshail et al., Citation2016).
In terms of eligibility criteria, the major problem was the lack of additional criteria and being an athlete (Alshail et al., Citation2016; Gay-Escoda et al., Citation2011; Needleman et al., Citation2013; Solleveld et al., Citation2015). No clear description of the participant’s demographic characteristics was provided in the two studies (Alshail et al., Citation2016; Gay-Escoda et al., Citation2011). One study raised concerns about the periodontal condition and performance measurement due to considering only self-reported data without clinical evaluation (Solleveld et al., Citation2015). Performance measurement concerns were related to a few outcome measurements without properly identifying confounding factors (Alshail et al., Citation2016; Gay-Escoda et al., Citation2011). A low response rate was verified in one study (Kragt et al., Citation2019).
Risk of bias
The quality of the measurements reported in each study is presented in . One study was considered to have an increased risk of bias (Alshail et al., Citation2016). As mentioned above, some issues related to sampling methods, clear description of eligibility criteria, clear description of study subjects, validity of condition measurements, and cofounding factor management reduced the quality of the generated evidence. The other seven included studies were classified as having some concerns.
Quantitative analysis of studies
Three studies concerning the overall evaluation were included for quantitative synthesis (Gallagher et al., Citation2018; Needleman et al., Citation2013, Citation2016). The other five studies were excluded because they used different performance evaluations. The same group published two studies (Needleman et al., Citation2013, Citation2016). However, they were considered eligible because different athlete populations were evaluated. Thus, the sample overlap hypothesis was discarded. The majority of athletes presented a BPE score 1 and 2 ranging 50% to 83% of the research samples(gingivitis and mild periodotitis). Needleman et al. (Citation2013) reported 74.0% (97/131) of athletes with BPE score 1 or 2 without effects on performance and 77.1% (101/131) of athletes with BPE score 1 or 2 with effects on performance. The study of Needleman et al. (Citation2016), 80.9% (72/89) of athletes with BPE score 1 or 2 without effects on performance and 83.0% (73/88) of athletes with BPE score 1 or 2 with effects on performance.
Gallagher et al. (Citation2018) showed that 50% (134/268) of athletes with BPE score 1 or 2 have impact on performance.
The meta-analysis showed reduced heterogeneity (I2 = 0%) and no statistical significance (p = 0.55); thus, no sensitivity analysis was conducted. A negative self-report of athletic performance (participation, experience of pain, training volume/quality reduction) was identified in 72.5% of athletes with periodontal disease (240 out of 331) in comparison with 60.1% of those (238/396) without periodontal disease. Therefore, a positive association was observed among the analysed factors (OR = 1.55; 95% CI 1.04–2.31; p = 0.03; I2 = 0%). Periodontal disease status was significantly associated with increased odds of negative effects on sports performance (). This evidence was considered moderate ().
Figure 2. Forest plot reporting the association of periodontal disease with self-perceived reduction of sports performance according to the OIDP questionnaire.
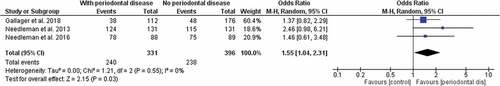
Table 3. Summary of findings for the influence of periodontal disease on athletic daily performance.
Summary of findings and level of evidence
Findings derived from the meta-analysis of self-perceived performance reduction associated with periodontal disease in athletes (). The low heterogeneity among the studies (I2 = 0%) indicated low inconsistency in the GRADE analysis. The absolute and relative effects of performance analysis, absence of possible publication bias, absence of serious problems among evaluation domains, and reduced influence of distortions yielded moderate evidence for the outcomes. However, the presence of potentially confounding factors may lead to a reduction in estimated effects.
Discussion
This review analysed the relationship between periodontal disease and sports performance, and the findings suggest an association between them, particularly in terms of self-perceived reductions in performance during training and competitions. The hypothesis under study relates to the fact that periodontal disease elicits a systemic inflammatory status, which could affect sports performance. Nevertheless, it needs to be highlighted that good standards of oral hygiene and periodontal health are rare (up to 70% in some studies), and six of the eight articles showed an association between periodontal disease and sports performance (Alshail et al., Citation2016; Botelho et al., Citation2021; Gallagher et al., Citation2018; Gay-Escoda et al., Citation2011; Needleman et al., Citation2016; Solleveld et al., Citation2015). Performance reduction dimensions included difficulty participating in routine training, reduction of training volume, and pain experience according to the OIDP questionnaires applied in three studies (Gallagher et al., Citation2018; Needleman et al., Citation2013, Citation2016). At least one of these dimensions was linked to periodontal disease.
Performance analysis comprehends an area of sport science concerned with actual sports performance in training and competitions, but also evaluates technical, physical and psychological aspects gathered in athlete’s capacities (O’Donoghue, Citation2009). The nature of performance analysis is complex due to the diversity of sports and their implications on athletes' health. Many measurements entail different impacts in performance dimensions. Fatigue variables may negative impact motor skills but also muscle recovery (Landers-Ramos et al., Citation2022; Mougios, Citation2007). Thus, due to the diversity of variables involving high-performance physical training and the multifactorial aspect of periodontal disease (Hecksteden et al., Citation2018; Meyle & Chapple, Citation2015), other associations should be carefully evaluated. These include changes in biochemical markers of muscle injury (CK) (Alshail et al., Citation2016; Gay-Escoda et al., Citation2011), increase in fat mass, reduction in muscle mass (Botelho et al., Citation2021), and prevalence of recurrent injuries (Solleveld et al., Citation2015). These associations should be taken into consideration, as they could also have an impact on athletic performance.
The relationship between physical activity and exercise and periodontal disease has been studied, and moderate physical activity has been associated with a reduction in the prevalence of periodontal disease (Ferreira et al., Citation2019). Individuals who engage in moderate physical activity or exercise for 30 to 150 min per week have a decreased risk of periodontal disease occurrence (Ferreira et al., Citation2019). The potential causes of this link could be related to inflammatory mediator regulation (IL-1b, IL-6, TNF-α, IL-10) or the behavioural changes related to self-care that promote a healthier lifestyle (e.g., adequate oral hygiene) (Al-Zahrani et al., Citation2005). However, athletes differ from the general population because of their high physical and psychological function levels and perceived health (Swann et al., Citation2015). Because athletes frequently engage in high-intensity training, periodontal disease may play a different role in triggering deficits in sports performance, such as an increased risk of injuries (Solleveld et al., Citation2015). Thus, a two-way relationship may exist between periodontal disease and sports performance.
Periodontal disease is a multifactorial condition characterized by a significant inflammatory profile of periodontal tissues, which is caused by the interaction of bacterial pathogens, host response, genetic factors, environmental factors, and personal health habits (Chapple et al., Citation2018). Multiple potential molecular processes involving cytokines, such as IL-1b, IL-6, IL-8, and TNF-α, are involved in periodontal disease. Increased levels of Il-6 and IL-8 play pivotal roles in matrix metalloproteinase-2 (MMP-2) activation by fibroblasts, leading to the degradation of gingival fibres and periodontal ligaments in periodontal disease (Cekici et al., Citation2014; Chapple & Matthews, Citation2007; Hajishengallis et al., Citation2020).
These cytokine functions result from the fight against the primary periodontal pathogens in an attempt to overcome bacterial challenges, but they are also related to high-intensity exercise (Cerqueira et al., Citation2020). Increased IL-6 and IL-8 levels were observed after moderate exercise. The concentration of IL-6 ranged from 1 to 4 times and from 1.5 to 26.79 in high-intensity exercises immediately after training execution, while IL-8 concentrations may vary from 1.37 to 2.77 times after high-intensity exercise compared to baseline levels (Cerqueira et al., Citation2020). Chronically increased levels of IL-6 and IL-8 are reported to be associated with fatigue (Silva et al., Citation2018), which is a severe risk factor for muscle injuries and leakage of CK (Ament & Verkerke, Citation2009).
Other important cytokines with similar roles in exercise and PD are IL-1β and TNF-α. Increased levels of these cytokines were found in intense exercise with predominant eccentric movements but not after moderate exercise (Cerqueira et al., Citation2020). IL-1β and TNF-α are potent proinflammatory cytokines that influence adhesion molecules and chemokines and are possibly related to leukocyte migration and function, especially osteoclast bone resorption in PD (Cekici et al., Citation2014; Meyle & Chapple, Citation2015). Thus, the inflammatory mediators shared by PD and high-intensity exercise could be related to an increased risk of fatigue, repeated muscle injuries, and potential aggravation of both PD and muscle function, consequently causing plasma leakage of CK (Alshail et al., Citation2016; Gay-Escoda et al., Citation2011; Silva et al., Citation2018; Solleveld et al., Citation2015).
CK is a protein involved in muscle metabolism (Baumert et al., Citation2016). The CK content is commonly used as a stress indicator and is regarded as a semi-quantitative indicator of muscle fibre injury (Baumert et al., Citation2016). Reference intervals of CK in athletes was previously published (Mougios, Citation2007) establishing parameters to identify normal values in sports practicing. Nevertheless, intervals of CK may differ considering the sport type and also the level of inflammation (Landers-Ramos et al., Citation2022). Thus, the upper limits of CK in a specific sport should be evaluated since their might increase risk for overexertion or injury (Mougios, Citation2007).
Although one of the studies showed a correlation between CK content and periodontal evaluation parameters such as BOP and PPD in soccer players’ dental evaluation (Alshail et al., Citation2016), serum CK levels can vary based on demographic factors such as age, sex, race, habits, and exercise style. Therefore, multivariate analysis is recommended to assay the actual effect of PD on CK levels. We also noted that the type of sport, such as soccer, may serve as another cofounding factor since eccentric exercise produces more significant muscle injury than concentric exercise, even at the same intensity (Baumert et al., Citation2016). Despite the biological mechanisms and other associations between PD and muscle injuries, further studies are needed to establish evidence of a real relationship between these events.
An important consideration while evaluating these findings is that observational studies cannot clarify causality. However, with plausible mechanisms, associations between exposure and outcomes should receive attention from the scientific community. Periodontal diseases are chronic noncommunicable diseases (Papapanou et al., Citation2018). These diseases share risk factors and indicators; therefore, common risk approaches are recommended (Meyle & Chapple, Citation2015). A healthy lifestyle should include good standards of oral hygiene, which will eventually influence the impacts of periodontal disease occurrence and severity (Al-Zahrani et al., Citation2005; Julie; Gallagher et al., Citation2019).
A quantitative synthesis of three studies showed that self-perceived reduction in performance analysed by the OIDP questionnaire was associated with PD (p = 0.03). Little heterogeneity (I2 = 0%) and non-serious issues of inconsistency, indirectness, risk of bias, and imprecision after the GRADE assessment of evidence led to a 1.5-fold increased risk of sports performance decline in athletes (Ryan & Hill, Citation2016). However, caution is needed when interpreting the pooled results, as dichotomous variables require more events to establish a relationship (Ryan & Hill, Citation2016). Furthermore, despite the relationship of self-reported decreased performance and periodontal disease, the univariate models only depict a possible effect between conditions among several other influences on the athlete’s routine and the pathogenesis of the periodontal disease (McKay & Verhagen, Citation2016; Meyle & Chapple, Citation2015). Poor periodontal health can affect athletes’ ability to compete, so the evidence is considered moderate and relevant (Ryan & Hill, Citation2016). Any changes in training volume, absences, or painful experiences can harm athletes, their teams, and investors (McKay & Verhagen, Citation2016).
Based on the review’s findings, athletes with periodontal disease should maintain good oral hygiene, seek treatment, be aware of potential performance reductions, and evaluate other possible associations. Those athletes should include regular brushing and flossing, as well as regular visits to the dentist. Besides, they should be aware of potential performance reductions, such as difficulty participating in routine training, reduction of training volume, and pain experience. These reductions could be linked to periodontal disease and impact overall sports performance. To support this, several studies have emphasized the importance of maintaining good oral hygiene and seeking treatment for periodontal diseases, such as Needleman et al. (Citation2016), who discovered a link between periodontal disease and sports performance, and Alshail et al. (Citation2016) who found that periodontal disease can alter biochemical markers of muscle injury. Additionally, Ferreira et al. (Citation2019) found that moderate physical activity can reduce the prevalence of the periodontal disease.
A significant limitation of this review was that only observational studies were included in the search strategy. Thus, the selected studies did not employ random allocation and group-matching methods to reduce bias. Furthermore, even though six studies showed a relationship between PD and decreased performance and another three found a link between the two conditions, several limitations of these studies require consideration. Most studies did not examine the prevalent confounding factors for PD (e.g., smoking, and glycaemic status) by using multivariate analyses. Also, one study used self-report of gum problems to establish periodontal status instead of bleeding on probing (BOP) and clinical attachment loss (CAL), some of primary features of periodontal evaluation (Chapple et al., Citation2018; Papapanou et al., Citation2018). Health research involving athletes should consider a specific definition when recruiting participants that may represent this population (Handelsman, Citation2016; Hecksteden et al., Citation2018). Discrepant results in evaluating the effects of risk factors or implemented treatments can be avoided by implementing defined eligibility criteria, which can generate fewer indirect results (Hecksteden et al., Citation2018; Schisterman et al., Citation2009). However, considering different aspects of sports practice, the great variability in sports results in different physiologies related to the athlete’s biotype and oxygen consumption (Baumert et al., Citation2016). Thus, the influence of aerobic, anaerobic, strength, and endurance sports implies an increase in variables that can influence the evaluation of the results (Powers et al., Citation2016).
In addition to the significant variability across different types of sports, the use of self-reported questionnaires for periodontal evaluation and assessment of sports performance may have influenced the survey results because many studies used questionnaires with weak reliability and validity (Gallagher et al., Citation2017). Thus, epidemiological studies on the relationship between PD and sports performance require an accurate assessment of both conditions (Schisterman et al., Citation2009). Nevertheless, an important point to consider is that research linking sports practice and periodontal evaluation is inherently challenging (Hecksteden et al., Citation2018; Oppermann et al., Citation2015), with the following aspects being particularly notable: difficulties in obtaining participants who meet specific eligibility criteria (Hecksteden et al., Citation2018), yielding reduced sample sizes; the cost and time constraints associated with the large-scale application of methods used in sports or periodontal evaluation (McKay & Verhagen, Citation2016), such as VO2max measurements and complete periodontal assessments (Oppermann et al., Citation2015), which are impractical in certain situations; and finally, athlete and technical team compliance and adherence to activities outside the training routine (McKay & Verhagen, Citation2016). As a result, there is uncertainty about the available evidence, necessitating additional studies using robust methodologies to reduce biases.
Conclusions
Within the limitations of this review, the findings revealed an association between PD and a self-perceived decrease in sports performance in elite athletes. We highlight the importance of preventive dental care, including engagement of athletes in oral health behavioural changes and developing periodontal treatment programmes to reduce the possible risks associated with athlete health. Further studies with larger sample sizes, assessment of confounding factors, and objective evaluations of PD and sports performance are needed to clarify the actual effect of both conditions. Considering the evidence of an association, randomized clinical trials to assess this two-way relationship are warranted.
Supplemental Material
Download MS Word (51.5 KB)Acknowledgements
The authors would like to thank the Federal University of Pará, Federal University of Rio de Janeiro, University of Alberta and Federal University of Rio Grande do Sul for technical and scientific support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/15438627.2023.2235048
Additional information
Funding
References
- Alshail, F., Aljohar, A., & Alshehri, M. (2016). Periodontal status and serum creatine kinase levels among young soccer players: A preliminary report. Nigerian Journal of Clinical Practice, 19(5), 655–658. https://doi.org/10.4103/1119-3077.188708
- Al-Zahrani, M. S., Borawski, E. A., & Bissada, N. F. (2005). Periodontitis and three health-enhancing behaviors: Maintaining normal weight, engaging in recommended level of exercise, and consuming a high-quality diet. Journal of Periodontology, 76(8), 1362–1366. https://doi.org/10.1902/jop.2005.76.8.1362
- Ament, W., & Verkerke, G. J. (2009). Exercise and fatigue. Sports Medicine, 39(5), 389–422. https://doi.org/10.2165/00007256-200939050-00005
- Ashley, P., DiIorio, A., Cole, E., Tanday, A., & Needleman, I. (2015). Oral health of elite athletes and association with performance: A systematic review. British Journal of Sports Medicine, 49(1), 14. https://doi.org/10.1136/bjsports-2014-093617
- Baumert, P., Lake, M. J., Stewart, C. E., Drust, B., & Erskine, R. M. (2016). Genetic variation and exercise-induced muscle damage: Implications for athletic performance, injury and ageing. European Journal of Applied Physiology, 116(9), 1595–1625. https://doi.org/10.1007/s00421-016-3411-1
- Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2021). Introduction to meta-analysis. John Wiley & Sons. https://doi.org/10.1002/9781119558378
- Botelho, J., Vicente, F., Dias, L., Júdice, A., Pereira, P., Proença, L., Machado, V., Chambrone, L., & Mendes, J. J. (2021). Periodontal health, nutrition and anthropometry in professional footballers: A preliminary study. Nutrients, 13(6), 1792. https://doi.org/10.3390/nu13061792
- Cekici, A., Kantarci, A., Hasturk, H., & Van Dyke, T. E. (2014). Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontology 2000, 64(1), 57–80. https://doi.org/10.1111/prd.12002
- Cerqueira, É., Marinho, D. A., Neiva, H. P., & Lourenço, O. (2020). Inflammatory effects of high and moderate intensity exercise—A systematic review. Frontiers in Physiology, 10. https://doi.org/10.3389/fphys.2019.01550
- Chang, Y., Phillips, M. R., Guymer, R. H., Thabane, L., Bhandari, M., Chaudhary, V., Wykoff, C. C., Sivaprasad, S., Kaiser, P., Sarraf, D., Bakri, S., Garg, S. J., Singh, R. P., Holz, F. G., Wong, T. Y., & on behalf of the, R. E. T. I. N. A. s. g. (2022). The 5 min meta-analysis: Understanding how to read and interpret a forest plot. Eye, 36(4), 673–675. https://doi.org/10.1038/s41433-021-01867-6
- Chapple, I. L. C., & Matthews, J. B. (2007). The role of reactive oxygen and antioxidant species in periodontal tissue destruction. Periodontology 2000, 43(1), 160–232. https://doi.org/10.1111/j.1600-0757.2006.00178.x
- Chapple, I. L. C., Mealey, B. L., Van Dyke, T. E., Bartold, P. M., Dommisch, H., Eickholz, P., Geisinger, M. L., Genco, R. J., Glogauer, M., Goldstein, M., Griffin, T. J., Holmstrup, P., Johnson, G. K., Kapila, Y., Lang, N. P., Meyle, J., Murakami, S., Plemons, J. … Yoshie, H. (2018). Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. Journal of Clinical Periodontology, 45(S20), S68–S77. https://doi.org/10.1111/jcpe.12940
- D’Isanto, T., D’Elia, F., Raiola, G., & Altavilla, G. J. S. M. (2019). Assessment of sport performance: Theoretical aspects and practical indications. Sport Mont, 17(1), 79–82. https://doi.org/10.26773/smj.190214
- Ebersole, J. L., Dawson Iii, D., Emecen-Huja, P., Nagarajan, R., Howard, K., Grady, M. E., Thompson, K., Peyyala, R., Al-Attar, A., Lethbridge, K., Kirakodu, S., & Gonzalez, O. A. (2017). The periodontal war: Microbes and immunity. Periodontology 2000, 75(1), 52–115. https://doi.org/10.1111/prd.12222
- Ferreira, R. D. O., Corrêa, M. G., Magno, M. B., Almeida, A. P. C. P. S. C., Fagundes, N. C. F., Rosing, C. K., Maia, L. C., & Lima, R. R. (2019). Physical activity reduces the prevalence of periodontal disease: Systematic review and meta-analysis. Frontiers in Physiology, 10, 234. https://doi.org/10.3389/fphys.2019.00234
- Ferreira de Brito Silva, R., Magno, M. B., Carvalho Almeida, A., Fagundes, N. C. F., Maia, L. C., & Lima, R. R. (2019). Does periodontitis represent a risk factor for rheumatoid arthritis? A systematic review and meta-analysis. Therapeutic Advances in Musculoskeletal Disease, 11, 1759720X19858514. https://doi.org/10.1177/1759720X19858514
- Ford, J. L., Ildefonso, K., Jones, M. L., & Arvinen-Barrow, M. (2017). Sport-related anxiety: Current insights. Open Access Journal of Sports Medicine, 8, 205–212. https://doi.org/10.2147/oajsm.S125845
- Gallagher, J., Ashley, P., & Needleman, I. (2020). Implementation of a behavioural change intervention to enhance oral health behaviours in elite athletes: A feasibility study. BMJ Open Sport & Exercise Medicine, 6(1), e000759. https://doi.org/10.1136/bmjsem-2020-000759
- Gallagher, J., Ashley, P., Petrie, A., & Needleman, I. (2018). Oral health and performance impacts in elite and professional athletes. Community Dentistry and Oral Epidemiology, 46(6), 563–568. https://doi.org/10.1111/cdoe.12392
- Gallagher, J., Ashley, P., Petrie, A., & Needleman, I. (2019). Oral health-related behaviours reported by elite and professional athletes. British Dental Journal, 227(4), 276–280. https://doi.org/10.1038/s41415-019-0617-8
- Gallagher, J., Needleman, I., Ashley, P., Sanchez, R. G., & Lumsden, R. J. S. M. (2017). Self-reported outcome measures of the impact of injury and illness on athlete performance: A systematic review. Sports Medicine, 47(7), 1335–1348. https://doi.org/10.1007/s40279-016-0651-5
- Gay-Escoda, C., Vieira-Duarte-Pereira, D. M., Ardevol, J., Pruna, R., Fernandez, J., & Valmaseda-Castellon, E. (2011). Study of the effect of oral health on physical condition of professional soccer players of the football club Barcelona. Medicina Oral Patologia Oral Y Cirugia Bucal, 16(3), E436–E439. https://doi.org/10.4317/medoral.16.e436
- Genco, R. J., & Sanz, M. (2020). Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontology 2000, 83(1), 7–13. https://doi.org/10.1111/prd.12344
- Hajishengallis, G., Chavakis, T., & Lambris, J. D. (2020). Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontology 2000, 84(1), 14–34. https://doi.org/10.1111/prd.12331
- Handelsman, D. J. (2016). Chapter 24 - performance enhancing hormones in sports doping. In J. L. Jameson, L. J. De Groot, D. M. de Kretser, L. C. Giudice, A. B. Grossman, S. Melmed, J. T. Potts, & G. C. Weir (Eds.), Endocrinology: Adult and pediatric (Seventh Edition) (pp. pp. 441–454.e4). Elsevier. https://doi.org/10.1016/B978-0-323-18907-1.00024-X
- Hecksteden, A., Faude, O., Meyer, T., & Donath, L. (2018). How to construct, conduct and analyze an exercise training study? Frontiers in Physiology, 9, 1007. https://doi.org/10.3389/fphys.2018.01007
- Higgins, J. P., Sterne, J. A., Savovic, J., Page, M. J., Hróbjartsson, A., Boutron, I., Reeves, B., & Eldridge, S. J. C. D. (2016). A revised tool for assessing risk of bias in randomized trials. Cochrane Database of Systematic Reviews, 10(Suppl 1), 29–31.
- Hoppe, C. B., Oliveira, J. A. P., Grecca, F. S., Haas, A. N., & Gomes, M. S. (2017). Association between chronic oral inflammatory burden and physical fitness in males: A cross-sectional observational study. International Endodontic Journal, 50(8), 740–749. https://doi.org/10.1111/iej.12686
- Houston, M. N., Hoch, M. C., & Hoch, J. M. (2016). Health-related quality of life in athletes: A systematic review with meta-analysis. Journal of Athletic Training, 51(6), 442–453. https://doi.org/10.4085/1062-6050-51.7.03
- Kragt, L., Moen, M. H., Van Den Hoogenband, C. R., & Wolvius, E. B. (2019). Oral health among Dutch elite athletes prior to Rio 2016. The Physician and Sportsmedicine, 47(2), 182–188. https://doi.org/10.1080/00913847.2018.1546105
- Landers-Ramos, R. Q., Dondero, K., Nelson, C., Ranadive, S. M., Prior, S. J., Addison, O., & Loenneke, J. P. (2022). Muscle thickness and inflammation during a 50km ultramarathon in recreational runners. PLOS ONE, 17(9), e0273510. https://doi.org/10.1371/journal.pone.0273510
- Lee, E. C., Fragala, M. S., Kavouras, S. A., Queen, R. M., Pryor, J. L., & Casa, D. J. (2017). Biomarkers in sports and exercise: Tracking health, performance, and recovery in athletes. Journal of Strength and Conditioning Research, 31(10), 2920–2937. https://doi.org/10.1519/JSC.0000000000002122
- Lochbaum, M., Stoner, E., Hefner, T., Cooper, S., Lane, A. M., Terry, P. C., & Imperatori, C. (2022). Sport psychology and performance meta-analyses: A systematic review of the literature. PLOS ONE, 17(2), e0263408. https://doi.org/10.1371/journal.pone.0263408
- McKay, C. D., & Verhagen, E. (2016). ‘Compliance’versus ‘adherence’in sport injury prevention: Why definition matters. British Journal of Sports Medicine 50 (7), 382–383 BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine. 10.1136/bjsports-2015-095192
- Mendes, L. S., Silva, L. S., Mello, D. B., & Dantas, E. H. M. (2012). Saúde bucal e marcadores bioquímicos de jogadores amadores de futebol do Estado do Piauí - Brasil [Oral health and blood biochemical markers of amateur´s soccer players in Brazil]. Review ABO Nac, 20(6), 356–362. https://pesquisa.bvsalud.org/portal/resource/pt/lil-671902
- Meyle, J., & Chapple, I. (2015). Molecular aspects of the pathogenesis of periodontitis. Periodontology 2000, 69(1), 7–17. https://doi.org/10.1111/prd.12104
- Moola, S., Munn, Z., Tufanaru, C., Aromataris, E., Sears, K., Sfetcu, R., Currie, M., Qureshi, R., Mattis, P., & Lisy, K. (2017). Chapter 7: Systematic reviews of etiology and risk. Joanna Briggs institute reviewer’s manual. The Joanna Briggs Institute, I, 5.
- Mougios, V. (2007). Reference intervals for serum creatine kinase in athletes. British Journal of Sports Medicine, 41(10), 674–678. https://doi.org/10.1136/bjsm.2006.034041
- Needleman, I., Ashley, P., Fine, P., Haddad, F., Loosemore, M., de Medici, A., Donos, N., Newton, T., van Someren, K., Moazzez, R., Jaques, R., Hunter, G., Khan, K., Shimmin, M., Brewer, J., Meehan, L., Mills, S., & Porter, S. (2014). Consensus statement: Oral health and elite sport performance. British Dental Journal, 217(10), 587–590. https://doi.org/10.1038/sj.bdj.2014.1000
- Needleman, I., Ashley, P., Meehan, L., Petrie, A., Weiler, R., McNally, S., Ayer, C., Hanna, R., Hunt, I., Kell, S., Ridgewell, P., & Taylor, R. (2016). Poor oral health including active caries in 187 UK professional male football players: Clinical dental examination performed by dentists. British Journal of Sports Medicine, 50(1), 41–44. https://doi.org/10.1136/bjsports-2015-094953
- Needleman, I., Ashley, P., Petrie, A., Fortune, F., Turner, W., Jones, J., Niggli, J., Engebretsen, L., Budgett, R., Donos, N., Clough, T., & Porter, S. (2013). Oral health and impact on performance of athletes participating in the London 2012 Olympic games: A cross-sectional study. British Journal of Sports Medicine, 47(16), 1054–1058. https://doi.org/10.1136/bjsports-2013-092891
- O’Donoghue, P. (2009). Research methods for sports performance analysis. Research Methods for Sports Performance Analysis, 1–278. https://doi.org/10.4324/9780203878309
- Opazo-García, C., Moya-Salazar, J., Chicoma-Flores, K., & Contreras-Pulache, H. (2021). Oral health problems in high-performance athletes at 2019 Pan American Games in Lima: A descriptive study. BDJ Open, 7(1), 21. https://doi.org/10.1038/s41405-021-00078-1
- Oppermann, R. V., Haas, A. N., Rösing, C. K., & Susin, C. (2015). Epidemiology of periodontal diseases in adults from Latin America. Periodontology 2000, 67(1), 13–33. https://doi.org/10.1111/prd.12061
- Oredugba, F. A., & Perlman, S. P. (2010). Oral health condition and treatment needs of special Olympics athletes in Nigeria. Special Care in Dentistry: Official Publication of the American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry, 30(5), 211–217. https://doi.org/10.1111/j.1754-4505.2010.00155.x
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., Stewart, L. A., Thomas, J., Tricco, A. C., Welch, V. A., Whiting, P., & Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
- Papapanou, P. N., Sanz, M., Buduneli, N., Dietrich, T., Feres, M., Fine, D. H., Flemmig, T. F., Garcia, R., Giannobile, W. V., Graziani, F., Greenwell, H., Herrera, D., Kao, R. T., Kebschull, M., Kinane, D. F., Kirkwood, K. L., Kocher, T., Kornman, K. S. … Tonetti, M. S. (2018). Periodontitis: Consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. Journal of Clinical Periodontology, 45(S20), S162–S170. https://doi.org/10.1111/jcpe.12946
- Powers, S. K., Radak, Z., & Ji, L. L. (2016). Exercise-induced oxidative stress: Past, present and future. The Journal of Physiology, 594(18), 5081–5092. https://doi.org/10.1113/JP270646
- Ryan, R., & Hill, S. J. C. C. O. A. R. V. J. (2016). Cochrane consumers and communication group. How to GRADE the quality of the evidence.
- Schisterman, E. F., Cole, S. R., & Platt, R. W. J. E. (2009). Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology, 20(4), 488. https://doi.org/10.1097/EDE.0b013e3181a819a1
- Silva, J. R., Rumpf, M. C., Hertzog, M., Castagna, C., Farooq, A., Girard, O., & Hader, K. (2018). Acute and residual soccer match-related fatigue: A systematic review and meta-analysis. Sports Medicine, 48(3), 539–583. https://doi.org/10.1007/s40279-017-0798-8
- Solleveld, H., Flutter, J., Goedhart, A., & VandenBossche, L. (2018). Are oral health and fixed orthodontic appliances associated with sports injuries and postural stability in elite junior male soccer players? Bmc Sports Science Medicine and Rehabilitation, 10(1), 10. https://doi.org/10.1186/s13102-018-0105-5
- Solleveld, H., Goedhart, A., & Vanden Bossche, L. (2015). Associations between poor oral health and reinjuries in male elite soccer players: A cross-sectional self-report study. BMC Sports Science, Medicine and Rehabilitation, 7(1). https://doi.org/10.1186/s13102-015-0004-y
- Suzuki, M., & Toyoda, H. J. (2015). Survey of oral health condition in professional soccer players. Journal of Oral Science and Health, 2(1), 1–4. https://doi.org/10.17653/2374-9075.SS0007
- Swann, C., Moran, A., & Piggott, D. J. (2015). Defining elite athletes: Issues in the study of expert performance in sport psychology. Psychology of Sport & Exercise, 16, 3–14. https://doi.org/10.1016/j.psychsport.2014.07.004
- Zhao, D., Khawaja, A., Jin, L., Li, K. Y., Tonetti, M., & Pelekos, G. (2018). The directional and non‐directional associations of periodontitis with chronic kidney disease: A systematic review and meta‐analysis of observational studies. Journal of Periodontal Research, 53(5), 682–704. https://doi.org/10.1111/jre.12565