Abstract
Epicutaneous exposure to allergenic proteins is an important sensitization route for skin diseases like protein contact dermatitis, immunologic contact urticaria, and atopic dermatitis. Environmental allergen sources such as house dust mites contain proteases, which are frequent allergens themselves. Here, the dependency of T-helper (TH) cell recall responses on allergen protease activity in the elicitation phase in mice pre-sensitized via distant skin was investigated. Repeated epicutaneous administration of a model protease allergen, i.e. papain, to the back skin of hairless mice induced skin inflammation, serum papain-specific IgE and TH2 and TH17 cytokine responses in the sensitization sites, and antigen-restimulated draining lymph node cells. In the papain-sensitized but not vehicle-treated mice, subsequent single challenge on the ear skin with papain, but not with protease inhibitor-treated papain, up-regulated the gene expression of TH2 and TH17/TH22 cytokines along with cytokines promoting these TH cytokine responses (TSLP, IL-33, IL-17C, and IL-23p19). Up-regulation of IL-17A gene expression and cells expressing RORγt occurred in the ear skin of the presensitized mice even before the challenge. In a reconstructed epidermal model with a three-dimensional culture of human keratinocytes, papain but not protease inhibitor-treated papain exhibited increasing transdermal permeability and stimulating the gene expression of TSLP, IL-17C, and IL-23p19. This study demonstrated that allergen protease activity contributed to the onset of cutaneous TH2 and TH17/TH22 recall responses on allergen re-encounter at sites distant from the original epicutaneous sensitization exposures. This finding suggested the contribution of protease-dependent barrier disruption and induction of keratinocyte-derived cytokines to the recall responses.
Introduction
Environmental allergen sources, such as house dust mites, insects, fungi, and pollen, contain proteases, and the proteolytic activity of such allergens is involved in the pathogenesis of allergy to them (Takai and Ikeda Citation2011; Cayrol et al. Citation2018; Serhan et al. Citation2019; Perner et al. Citation2020). Papain is a papaya fruit-derived occupational protease allergen used in the food industry and pharmaceuticals. Papain causes respiratory allergic reactions and, more rarely, allergic skin diseases such as protein contact dermatitis and contact urticaria (Milne and Brand Citation1975; Niinimaki et al. Citation1993, Quiñones et al. Citation1999; Basketter and Lahti Citation2011; Basketter et al. Citation2012; Barbaud Citation2020). Papain and the house dust mite major allergens Der f 1 and Der p 1 belong to the same family of cysteine proteases (Chua et al. Citation1988; Thomas Citation2015). With papain acting as a model protease allergen, recent studies conducted using murine models of airway inflammation (Kamijo et al. Citation2013; Hara et al. Citation2014; Halim et al. Citation2014; Nishioka et al. Citation2018; Maruyama et al. Citation2019; Kunimine et al. Citation2021) or sensitization via skin (Iida et al. Citation2014; Shimura et al. Citation2016; Ochi et al. Citation2017; Kamijo, Suzuki, Hara, et al. Citation2016; Kamijo et al. Citation2021; Yokozeki et al. Citation2021) have demonstrated that the protease activity of papain is essential to the induction of airway and skin inflammation and of serum IgE/IgG1 responses.
Epicutaneous allergen exposure is an important sensitization route for allergic diseases such as asthma, rhinitis, and food allergy (Paller et al. Citation2019). This is also applicable to allergenic skin disorders, such as protein contact dermatitis, immunologic contact urticaria, and atopic dermatitis (AD). These disorders are inducible by re-exposure to an allergen at both the sensitization sites and distant skin sites. In a murine model, onset of allergic airway inflammation after epicutaneous papain pre-sensitization requires intact T/B epitope structures and protease activity (Nishioka et al. Citation2018). Previous studies have demonstrated the importance of protease activity for skin sites during sensitization with repeated allergen exposure (Iida et al. Citation2014; Shimura et al. Citation2016). However, to date, no study has investigated the role of allergen protease activity in allergen re-encounter at distant skin sites compared to original allergen exposure sites.
Accordingly, the present study was conducted to examine the dependency of the onset of cutaneous TH recall responses on allergen protease activity at ear skin sites for the allergen challenge in mice, pre-sensitized via back skin to induce allergen-specific TH2, TH17, and IgE responses. Protease-dependent keratinocyte responses in a reconstructed human epidermal (RhE) model were also examined.
Materials and methods
Materials
Papain was purchased from Calbiochem (San Diego, CA). E64-papain was prepared according to a previously described protocol using E64 (Sigma, St Louis, MO) (Kamijo et al. Citation2013). Papain was biotinylated using an EZ-Link™ Sulfo-NHS-LC-Biotinylation Kit (Thermo Fisher Scientific, Tokyo, Japan) according to manufacturer instructions. The biotinylated papain was then treated with E64 to prepare E64-papain. Papain or biotinylated papain, which were incubated and dialyzed similarly to E64-papain or E64-biotinylated papain, respectively (except for addition of E64), were used in experiments investigating the dependency on the protease activity of papain. Purity, absence of degradation, and absence of aggregation of protein samples were confirmed using electrophoresis. Protease activity was analyzed using synthetic fluorogenic substrates in the presence of dithiothreitol (Takai et al. Citation2005).
Mice
HOS:HR-1 hairless mice (7-wk-old, female) were obtained from Japan SLC (Shizuoka, Japan). All animals were housed in pathogen-free facilities maintained at 23 °C with a 55% relative humidity and a 12-hr light:dark cycle. All mice had ad libitum access to standard feed pellets and filtered tap water. The Kao Corporation Animal Care Committee approved all animal experiments. All studies were conducted according to committee guidelines.
Epicutaneous sensitization
Papain (100 μg/100 μl phosphate-buffered saline [PBS]/2.25 cm2/site) or PBS (100 μl/2.25 cm2/site) was perfused to a square piece of gauze (PIP, Osaka, Japan) under an acrylic adhesive waterproof film (3 M Japan, Tokyo), then placed on the back skin of the hairless mice and immobilized using a polyurethane film (Alcare, Tokyo). The sensitization concentration was determined based on previous studies (He et al. Citation2007; Iida et al. Citation2014). The application was performed twice weekly for 5 wk (total number of applications = 10). Two days after the final sensitization, the mice were anesthetized with isoflurane (FUJIFILM Wako Pure Chemical, Osaka) and blood samples were collected from the abdominal aorta. The mice were subsequently euthanized by cervical dislocation. The sensitization sites (back skins) were collected at necropsy and stabilized in RNA-later (QIAGEN, Manchester, UK). Other samples from the sites were processed for histology by placing the tissues into Mildform® 10 N (FUJIFILM Wako Pure Chemical).
Draining lymph node (DLN) cells were collected aseptically from the axillary lymph and inguinal lymph nodes. These cells were harvested in, washed with, re-suspended in RPMI 1640 medium (Invitrogen, Carlsbad, CA) supplemented with 10% (v/v) heat-inactivated fetal bovine serum, 1% (v/v) penicillin-streptomycin solution, and 0.05 mM 2-mercaptoethanol (all Invitrogen) and then counted for use in the assays outlined below.
Epicutaneous challenge
A volume of 25 µl/ear of 1.0% papain or E64-papain in PBS containing 0.5% Tween-20 (Kanto Chemical, Tokyo) was applied to, respectively, the backside of the left or right ear of the mice. The challenge concentration was determined according to a previous study (Shimura et al. Citation2016). Before and then 3, 24, 48, and 96 hr after the challenge, the mice were anesthetized and then euthanized. The challenge sites (ear skins) were collected and stabilized in RNA-later or Mildform® 10 N.
Histology
All back and ear skin samples for histologic analyses were de-paraffinized, sectioned to 4-µm-thickness. Subsets of each sample set were stained with hematoxylin and eosin and toluidine blue using standard protocols. For immunohistochemical staining to assess RORγt status, antigen retrieval was performed using 100× Tris-EDTA buffer (pH 9.0) (Abcam, Cambridge, UK) and placing the section in PBS. Anti-RORγ antibody (Abcam) was diluted 1:400 in PBS containing 1.0% bovine serum albumin (BSA, FUJIFILM Wako Pure Chemical) and then solution was placed atop the tissue section. The materials were incubated overnight at 4 °C, before the section was gently rinsed with PBS. Thereafter, anti-rabbit IgG peroxidase conjugate (Jackson Immunochemicals, West Grove, PA) diluted in PBS containing 1.0% BSA (antibody dilution: 1:100) was placed atop the section and the materials incubated for 1 hr at room temperature. After the section was gently rinsed with PBS, the slides were stained using a 3,3′-diaminobenzidine Substrate Kit (Vector Labs, Burlingame, CA) and then embedded with Entellan® new (Merck, Darmstadt, Germany). Stained sections were observed under an optical microscope (Olympus Corporation, Tokyo) with a minimum of 3 regions per animal evaluated. (data shown are representative images from 4 mice/group).
RT-qPCR
The other dedicated samples of back and ear skins that had been stabilized in RNA-later were placed in Buffer RLT (QIAGEN) containing 1% 2-mercaptoethanol (Serva, Heidelberg, Germany) and homogenized using a micro-homogenizer (Microtec, Chiba, Japan). Total RNA from each sample was extracted and purified using an RNeasy Fibrous Tissue Mini Kit and an RNeasy MinElute Cleanup Kit (QIAGEN). Purity and concentration of the isolated RNA was confirmed using a NanoDrop system (Thermo Fisher Scientific). First-strand cDNA was then synthesized from total RNA using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Waltham, MA). RT-qPCR was then performed using the Taqman method in a QuantStudio 5 Real-Time PCR system (Applied Biosystems). mRNA levels of the target gene were normalized to gene expression levels of GAPDH (glyceraldehyde 3-phosphate dihydrogen- ase). All data are presented as relative expression levels to the control group ( - back skin of vehicle-treated mice; and - ear skin of vehicle-treated mice before challenge).
Figure 1. Epicutaneous papain sensitization on back skin of mice induced skin inflammation, serum papain-specific IgE and IgG1, and differentiation of TH2 and TH17 cells. (a) Timeline. (b) Serum antibodies. (c) Cytokine production in DLN cells restimulated with E64-papain. (d) Histology (hematoxylin-eosin staining). (e) Gene expression in back skin. Data shown are means ± SD of 4 (b,e) or 3-6 mice/group (c) and represent three independent experiments with similar results. *p < 0.05 vs. vehicle (b,e) or no restimulation (c) by Mann-Whitney U-test. Scale bar = 50 µm.
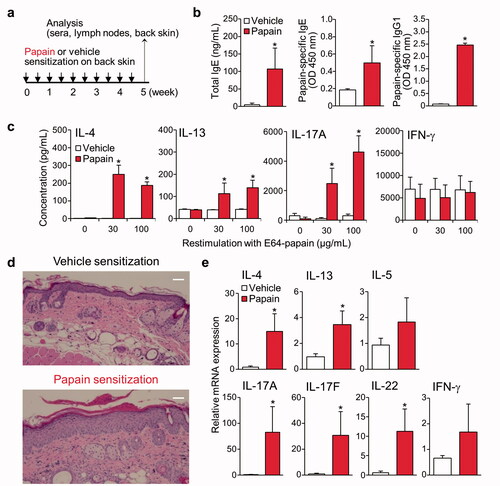
Figure 2. Epicutaneous papain challenge on the ear skin stimulated TH2 and TH17/TH22 cytokine gene expression and triggered mast cell degranulation in a manner dependent on the epicutaneous presensitization. (a) Timeline. (b) Gene expression in ear skin before and after challenge. Data shown are means ± SD of 4-6 mice/group and represent three independent experiments with similar results. *p < 0.05 vs before challenge, #p < 0.05 vs vehicle (Mann-Whitney U-test). (c) Toluidine blue staining. Red arrows show degranulated mast cells. Scale bar = 50 µm. (d) RORγt IHC staining of ear skin before papain challenge. Red dotted line circles indicate positively-stained cells. Scale bar = 100 µm.
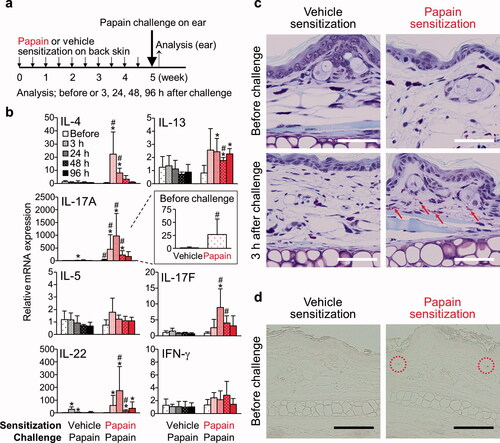
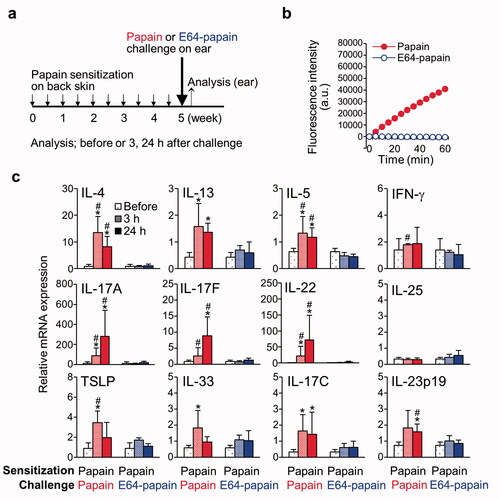
Figure 3. Epicutaneous papain challenge on the ear skin after pre-sensitization stimulated TH2 and TH17/TH22 cytokine gene expression in a manner dependent on protease activity. (a) Timeline. (b) Protease assay for papain or E64-papain. (c) Gene expression in ear skin before and after papain or E64-papain challenge. Data shown are means ± SD of 4 mice/group. * p < 0.05 vs before challenge, # p < 0.05 vs vehicle (Mann-Whitney U-test).
Serum antibodies ELISA
A sandwich enzyme-linked immunosorbent assay, based on a previously-described protocol (Kamijo et al. Citation2013) with minor modifications, was used to measure serum antibody levels. In brief, serum total IgE or papain-specific IgE/IgG1 levels were detected using plates coated with 2 µg/ml anti-mouse IgE antibody (BD Biosciences, San Jose, CA) or 10 µg/ml papain in PBS, respectively. All plates were pre-blocked with 20% Immunoblock (DS Pharma Biomedical, Osaka) in distilled water. To assess total IgE and papain-specific IgG1 levels, sera and detection antibodies were each diluted using PBS containing 0.05% Tween-20 and 5% Immuno- block (serum dilutions of 1:50 for total IgE and 1:5000 for papain-specific IgG1). To assess papain-specific IgE levels, sera and detection antibodies were each diluted with Solutions 1 and 2 of CanGetSignal (Toyobo, Osaka), respectively (serum dilution 1:50). Plates were then treated with TMB Microwell Peroxidase Substrate (Seracare, Milford, MA) according to manufacturer protocols, and the absorbance at 450 nm in each well was read on a CLARIOstar plate reader (BMG Labtech, Ortenberg, Germany).
Re-stimulation of DLN cells
DLN cells were plated at a density of 5 × 105 cells/well in flat-bottom 96-well plates (Nippon Genetics, Tokyo) containing 30 or 100 µg/ml E64-papain or medium alone. Skin DLN cells were re-stimulated in vitro for cytokine production with E64-papain to avoid possible stimulatory effects via protease activity (Kamijo et al. Citation2013). After 72 hr, culture supernatants were collected and analyzed in a MILLIPLEX MAP Mouse TH17 Magnetic Bead Panel-Immunology Multiplex Assay (Merck) to measure specific cytokines (e.g. interleukin [IL]-4,-13, and -17 A). The cytokine assays were conducted according to manufacturer protocols.
Reconstructed epidermal model with a three-dimensional culture of human keratinocytes
A RhE model “LabCyte EPI-MODEL (24-well format)” (Japan Tissue Engineering, Aichi, Japan) was purchased and used in this study. The RhE model tissues were pre-cultured overnight at 37 °C (5% CO2) in the culture medium provided by the manufacturer. After pre-cultivation, the medium was changed to Dulbecco’s modified Eagle’s medium (Merck) containing 25% Nutrient Mixture F-12 Ham (Merck) and 0.2% gentamicin/amphotericin solution (Invitrogen). Biotinylated papain or E64-biotinylated papain (0.1%, 100 µl) in PBS, or an equal volume PBS as the vehicle-treated control, was applied to the surface of the RhE model and incubated for 3 or 6 hr at 37 °C (5% CO2). After treatment, the medium from each well was collected, and 50 µl of 20 mM E64 in PBS (final concentration 2 mM) was added to each. The samples with equal volume, which contained biotinylated proteins that permeated through the tissues, were subjected to SDS-PAGE separation. After incubation at 80 °C for 1 min, 15 µl of the samples was loaded into 12% gels (BioRad, Hercules, CA) and electrophoresis was performed at 4 °C with 70 mA and 200 V for 40 min. The proteins were then electrotransferred to PVDF membranes (BioRad) at 4 °C with 220 mA and 100 V. The membranes were then soaked in 5% skimmed milk (FUJIFILM Wako Pure Chemical) to block nonspecific binding. Ultimately, biotinylated proteins were detected using streptavidin-horseradish peroxidase conjugate (Merck) and a SuperSignal™ West Dura Extended Duration Substrate (Thermo Fisher Scientific). Sample protein concentration comparisons based on total intensity in each lane were quantified using an Image Quant LAS 4000 system (GE Healthcare Japan, Tokyo) and Multi Gauge software (FUJIFILM, Tokyo).
After harvesting of the culture medium, the tissues were gently removed from their well, rinsed three times in 2 mM E64 in PBS, and then lysed using Buffer RLT. Total RNA was extracted from the lysed tissues using the RNeasy Mini kit (QIAGEN), and RT-qPCR analysis was performed (see above). Target gene mRNA levels were normalized to those of GAPDH. All data are presented as expression levels relative to those in untreated wells.
Statistical analysis
A Mann-Whitney U-test (two-tailed) or one-way analysis of variance (ANOVA) with a Tukey-Kramer post-hoc test was used to determine any significant differences between mean values. A p-value < 0.05 was considered statistically significant. All data were analyzed using the software EZR v.1.40 (Saitama Medical Center, Jichi Medical University, Saitama, Japan).
Results
Epicutaneous papain sensitization on back skin of mice induced skin inflammation, serum papain-specific IgE and IgG1, and TH2 and TH17 cell differentiation
HOS:HR-1 hairless mice were epicutaneously sensitized by applying papain on the back skin via an occlusive patch (). The sensitization up-regulated the serum total IgE levels and induced the production of papain-specific IgE and IgG1 (). The papain-sensitized mice showed the production of IL-4, -13, and -17 A in antigen- re-stimulated skin DLN cells, indicating differentiation of papain-specific TH2 and TH17 cells (). The papain-treated skin demonstrated more severe dermal and epidermal thickening and granulocyte infiltration than the vehicle-treated skin () and higher gene expression levels of TH2 (IL-4 and -13) and TH17/TH22 (IL-17A, -17 F, and -22) cytokines (). Hence, epicutaneous papain sensitization induced serum papain-specific IgE/IgG1, DLN TH2, and TH17 responses and inflammation in the sensitization sites with up-regulated gene expression of TH2 and TH17/TH22 cytokines.
Epicutaneous papain challenge on ear skin stimulated TH2 and TH17/TH22 cytokine gene expression and triggered mast cell degranulation in a manner dependent on epicutaneous pre-sensitization
After sensitization via the back skin, the mice were subsequently challenged with papain on their ear surface (). The epicutaneous challenge with papain, but not a vehicle, in the pre-sensitized mice resulted in local responses of up-regulated gene expression of TH2 (IL-4 and -13) and TH17/TH22 (IL-17A, -17 F, and -22) cytokines - with peaks at 3 and 24 hr after the challenge, respectively (). Mast cell degranulation appeared at 3 hr after the challenge (). None of these responses were detected in the vehicle-treated mice. As such, epicutaneous papain presensitization via back skin was indispensable for the responses, indicating adaptive skin immune responses induced by pre-sensitization (such as increases in papain-specific TH cells and antibodies) contributed to the responses in the elicitation phase.
Interestingly, IL-17A gene expression in the ears was up-regulated significantly in the pre-sensitized mice even before the papain challenge (, insert for IL-17A). Cells expressing RORγt (key transcription factor for IL-17A-producing cells) (Ivanov et al. Citation2006; Unutmaz Citation2009) were observed in the ears without the challenge in the sensitized mice, but there were fewer cells in the unsensitized mice ().
Epicutaneous papain challenge on ear skin after pre-sensitization up-regulated local TH2 and TH17/TH22 cytokine gene expression in a manner dependent on its protease activity
After the epicutaneous papain pre-sensitization, papain or E64-papain which lacks the protease activity but maintains the intact T/B epitope structures (Kikuchi et al. Citation2006; Nishioka et al. Citation2018) was topically applied to the left or right ear of the mice, respectively (). Elimination of the protease activity of E64-papain was confirmed using a synthetic fluorogenic substrate (). The epicutaneous challenge with papain, but not E64-papain, up-regulated gene expression of TH2 (IL-4, -13, and -5) and TH17/TH22 cytokines (IL-17A, -17 F, and -22) and cytokines promotive for these TH cytokine responses (TSLP, IL-33, IL-17C, and IL-23p19) (Takai Citation2012; Gaffen et al. Citation2014; Cayrol and Girard Citation2018; Vandeghinste et al. Citation2018; Corren and Ziegler Citation2019; Nies and Panzer Citation2020) in the challenge sites (). Therefore, the protease activity of papain administered in the epicutaneous challenge was essential for triggering the local up-regulation of TH2 and TH17/TH22 cytokines, and their promoter cytokines, in mice that were epicutaneously pre-sensitized via distant sites.
Papain increased epidermal permeability and stimulated gene expression of TSLP, IL-17C, and IL-23p19 in the RhE model in a manner dependent on its protease activity
To examine the contribution of papain protease activity in disrupting the epidermal barrier, a penetration assay was conducted using biotinylated papain and E64-biotinylated papain in the RhE model (a three-dimensional culture of normal human keratinocytes without the other cell types). We analyzed the protease activities of biotinylated papain and E64-biotynylated papain to confirm the maintenance and elimination of enzyme activity, respectively (). Our results showed that treatment of the RhE model with biotinylated papain led to higher epidermal permeability than that obtained by treatment with E64-biotinylated papain ().
Figure 4. Papain, but not E64-papain, penetrated reconstructed human epidermis and stimulated TSLP, IL-17C, and IL-23p19 gene expression. (a) Protease assay for biotinylated papain or E64-biotinylated papain. (b) Permeability of biotinylated papain and E64-biotinylated papain. (c) Gene expression of cytokines that induce TH2/TH17 cell differentiation or stimulate TH2/TH17 cell cytokine production. Data shown are means ± SD of 6 wells/group. * p < 0.05 vs. E64-biotinylated papain (Mann-Whitney U-test) (b). * p < 0.05 vs vehicle, # p < 0.05 vs. E64-biotinylated papain by analysis of variance (c) followed by Tukey-Kramer post-hoc test.
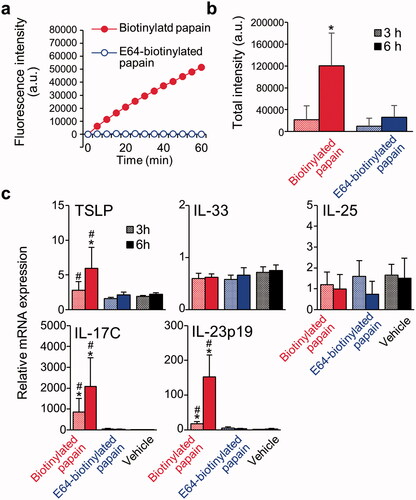
Moreover, expression of genes for cytokines that promote TH2 and TH17/TH22 cytokine responses was also analyzed. The results indicated expression of TSLP, IL-17C, and IL-23p19 were stimulated by biotinylated papain, but not E64-biotinylated papain (). Thus, it is likely papain protease activity disrupted barrier functions and stimulated the keratinocyte-derived gene expression of cytokines that promote TH2 and TH17/TH22 cytokine responses in the RhE model.
Discussion
The present study using allergen challenges in mice investigated the dependency of the onset of cutaneous TH recall responses on allergen protease activity at ear skin sites. The results here demonstrated that protease activity of papain contributed to the onset of TH2 and TH17/TH22 recall responses. The onset might have been related to papain acting to disrupt the epidermal barrier and allow events to occur that stimulated promoter cytokine expression in keratinocytes at the challenge sites distant from the sensitization sites.
Among many immune cells, TH2, TH17, and other cell subsets are reportedly key factors for the development and intensity of allergic diseases/responses. The major subtypes of AD reveal an association with TH2 and IL-22-producing TH22 cells, and some subtypes reveal an association with TH17 cells (Brunner et al. Citation2017b; Ahn et al. Citation2020). The model used in our study showed an association with TH2, TH17, and TH22 cytokine pathways in common with AD, which is different from the classical TH1/TC1 pathway in allergic contact dermatitis (Kimber and Dearman, Citation2002; McFadden et al. Citation2013). Because the mice unsensitized to papain did not exhibit any significant responses to the papain challenge (), we considered that the adaptive immune responses of papain-specific TH cells and/or antibodies contributed to the elicitation phase in the pre-sensitized mice. However, innate-type cells such as innate lymphoid cells, basophils, and γδT cells have a potential to produce some of these cytokines in direct or indirect responses to protease allergens (Sokol et al. Citation2008; Halim et al. Citation2012; Kamijo et al. Citation2013, Citation2021; Kamijo, Nunomura, Ra, et al. Citation2016).
The up-regulation of IL-17A mRNA expression and the numbers of RORγt+ cells found in the untreated ears of pre-sensitized mice suggested to us that epicutaneous papain pre-sensitization caused IL-17A-producing RORγt+ cells to infiltrate into the distant ear skin. Clinically, the non-lesional skin of patients with AD exhibits weaker inflammatory infiltration than lesional skin. However, non-lesional AD skin is distinct from normal skin in terms of terminal differentiation, some immune abnormalities, and elevated levels of T-cells (Suárez-Fariñas et al. Citation2011), and shares T-cell clones with lesional AD skin (Brunner et al. Citation2017a). Further, non-lesional skin from patients with early-onset pediatric AD exhibits dysregulated expression of TH2 and TH17/TH22- related genes (Guttman-Yassky et al. Citation2019, Pavel et al. Citation2021). The model used in the current study showing a dissemination of RORγt+ cells after the epicutaneous pre-sensitization in distant skin sites - even without the antigen challenge - might be useful for elucidating mechanisms underlying the abnormalities in the non-lesional AD skin.
TSLP, IL-33, IL-17C, and IL-23p19, whose gene expressions were up-regulated by the epicutaneous challenge with papain but not E64-papain, are cytokines involved in causing the differentiation of TH2 and TH17/TH22 cells and/or the enhancement of their cytokine production (Takai Citation2012, Gaffen et al. Citation2014; Cayrol and Girard Citation2018; Vandeghinste et al. Citation2018; Corren and Ziegler Citation2019; Nies and Panzer Citation2020). The study here also showed that papain protease activity enhanced transdermal permeability and stimulated keratinocyte-derived mRNA expression of TSLP, IL-17C, and IL-23p19 in the RhE model. The barrier disruption could be due to papain-mediated cleavage of tight junction proteins (Stremnitzer et al. Citation2015). These results suggest allergen protease activity allows the allergen to access both epidermal and dermal cells, effectively re-calling TCR-mediated TH2 and TH17/TH22 cell responses in mice pre-sensitized to the allergen in synergy with keratinocyte-derived cytokines like TSLP, IL-17C, and IL-23p19. It is also possible that the barrier is further disrupted by following mechanisms. In vivo, IL-23 could also come from antigen-presenting cells, including dendritic cells (Gaffen et al. Citation2014). TH2 cytokines, IL-4 and IL-13, reportedly decrease profilaggrin synthesis (Howell et al. Citation2007). A TH17 cytokine, IL-17A, decreases synthesis of tight junction proteins and degradation of filaggrin monomers (Yuki et al. Citation2016), suggesting a vicious cycle between TH2 and TH17 sensitization and skin barrier dysfunction. Another study reported that IL-17A enhances the formation of tight junction proteins and barrier function (Brewer et al. Citation2019).
As the focus here was on any protease activity dependency of the elicitation phase, the current study did not explore contributions of protease activity to the epicutaneous sensitization phase in the present model. Previous studies using papain models with 2-wk epicutaneous sensitization on intact or tape-stripped ear skin demonstrated protease activity dependency (Iida et al. Citation2014, Shimura et al. Citation2016). The protease activity-dependent epidermal barrier disruption and keratinocyte responses in the RhE model also suggest the contribution of the protease activity to the epicutaneous sensitization (Iida et al. Citation2014, Shimura et al. Citation2016; Kunimine et al. Citation2021). However, one study showed protease activity-independent induction of IgE responses and skin inflammation in a 12-wk model with papain application in an occlusive patch on depilated back skin (Stremnitzer et al. Citation2015). Studies have reported that epicutaneous 7- or 4-wk sensitization to non-protease antigens such as ovalbumin via skin with shaving and an occlusive patch dressing with (Spergel et al. Citation1998; He et al. Citation2007) or without tape-stripping (Wang et al. Citation1996, Citation2009), respectively, resulted in induction of IgE production and TH2 and TH17 cell development. These results suggest that the allergen-derived protease activity accelerates the epicutaneous sensitization. However, epicutaneous sensitization to antigens without protease activity is inducible through epicutaneous exposure for longer periods via barrier-disturbed skin.
The present model resulted in an ear swelling [after epicutaneous challenge with papain] that was less severe than that observed in hapten-induced contact hypersensitivity models (Honda et al. Citation2013) (data not shown). This may be due to a lower transdermal permeability efficiency of protein antigens of larger molecular sizes than of haptens. Shimura et al. (Citation2016) noted that a combination of epicutaneous administration of papain and tape-stripping in naive mice led to a significant change in ear thickness in a manner dependent on papain protease activity. Addition of mechanical barrier disruption and/or increasing the number of papain application times in the challenge might effectively induce more severe responses in the elicitation phase.
In conclusion, the present study demonstrated that protease activity of papain contributed to the onset of TH2 and TH17/TH22 recall responses at distant epicutaneous challenge sites in mice pre-sensitized at the sensitization sites. This study provides important insights into the roles of proteases derived from environmental and occupational allergen sources in eliciting skin responses in protein contact dermatitis, immunologic contact urticaria, and AD. The results of this study also allow for the suggestion to be made that disruption of the protease-mediated epidermal barrier and the induction of keratinocyte-derived cytokines [e.g. TSLP, IL-17C, and IL-23] that promote TH2 and TH17/TH22 cytokine responses contribute to the elicitation phase. While papain was used as the protein allergen in this study, it remains necessary to conduct similar experiments in the future using other protein allergens (e.g. proteases subtilisin and Der p 1, as well as non-proteases like ovalbumin) to confirm the results of this study.
Author contributions
AO, TY, KY, AK, and YT performed the experiments. AO and TY designed the experiments and analyzed the data. AO, TY, and TT wrote the manuscript. TT, HY, DB, and HS provided scientific suggestions and review.
Acknowledgments
The authors thank Dr. Frank Gerberick (GF3 Consultancy LLC) and Prof. Kayoko Matsunaga (Fujita Health University) for the expertise and advice and Dr. Seiji Kamijo and Dr. Natsuko Maruyama (Juntendo University) for their technical advice. The authors also thank all the members of their laboratory for their informative help and advice.
Disclosure statement
Authors TT and DB received a consultation fee for this study from Kao Corporation. All other authors declare no conflicts of interest.
References
- Ahn K, Kim B, Kim J, Leung D. 2020. Recent advances in atopic dermatitis. Curr Opin Immunol. 66:14–21.
- Barbaud A. 2020. Mechanism and diagnosis of protein contact dermatitis. Curr Opin Allergy Clin Immunol. 20(2):117–121.
- Basketter D, 2011. and, Lahti A. Immediate Contact Reactions. In: Johansen J, Frosch P, Lepoittevin J, editors. Contact dermatitis. Berlin: Springer Berlin Heidelberg. p. 137–153.
- Basketter D, Berg N, Broekhuizen C, Fieldsend M, Kirkwood S, Kluin C, Mathieu S, Rodriguez C. 2012. Enzymes in cleaning products: An overview of toxicological properties and risk assessment/management. Regul Toxicol Pharmacol. 64(1):117–123.
- Brewer M, Yoshida T, Kuo F, Fridy S, Beck L, De Benedetto A. 2019. Antagonistic effects of IL-4 on IL-17A-mediated enhancement of epidermal tight junction function. Intl J Mol Sci. 20(17):4070.
- Brunner P, Emerson R, Tipton C, Garcet S, Khattri S, Coats I, Krueger J, Guttman-Yassky E. 2017. Nonlesional atopic dermatitis skin shares similar T-cell clones with lesional tissues. Allergy. 72(12):2017–2025.
- Brunner P, Guttman-Yassky E, Leung D. 2017. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 139(4S):S65–S76.
- Cayrol C, Girard J. 2018. Interleukin-33 (IL-33): A nuclear cytokine from the IL-1 family. Immunol Rev. 281(1):154–168.
- Cayrol C, Duval A, Schmitt P, Roga S, Camus M, Stella A, Burlet-Schiltz O, Gonzalez-de-Peredo A, Girard J. 2018. Environmental allergens induce allergic inflammation through proteolytic maturation of IL-33. Nat Immunol. 19(4):375–385.
- Chua K, Stewart G, Thomas W, Simpson R, Dilworth R, Plozza T, Turner K. 1988. Sequence analysis of cDNA coding for a major house dust mite allergen, Der p 1. Homology with cysteine proteases. J Exp Med. 167(1):175–182.
- Corren J, Ziegler SF. 2019. TSLP: From allergy to cancer. Nat Immunol. 20(12):1603–1609.
- Gaffen S, Jain R, Garg A, Cua D. 2014. The IL-23-IL-17 immune axis: From mechanisms to therapeutic testing. Nat Rev Immunol. 14(9):585–600.
- Guttman-Yassky E, Diaz A, Pavel A, Fernandes M, Lefferdink R, Erickson T, Canter T, Rangel S, Peng X, Li R, et al. 2019. Use of tape strips to detect immune and barrier abnormalities in the skin of children with early-onset atopic dermatitis. JAMA Dermatol. 155(12):1358–1370.
- Halim T, Krauss R, Sun A, Takei F. 2012. Lung natural helper cells are a critical source of TH2 cell-type cytokines in protease allergen-induced airway inflammation. Immunity. 36(3):451–463.
- Halim T, Steer C, Matha L, Gold M, Martinez-Gonzalez I, McNagny K, McKenzie A, Takei F. 2014. Group 2 innate lymphoid cells are critical for the initiation of adaptive T-helper 2 cell-mediated allergic lung inflammation. Immunity. 40(3):425–435.
- Hara K, Iijima K, Elias M, Seno S, Tojima I, Kobayashi T, Kephart G, Kurabayashi M, Kita H. 2014. Airway uric acid is a sensor of inhaled protease allergens and initiates Type 2 immune responses in respiratory mucosa. J Immunol. 192(9):4032–4042.
- He R, Oyoshi M, Jin H, Geha R. 2007. Epicutaneous antigen exposure induces a TH17 response that drives airway inflammation after inhalation challenge. Proc Natl Acad Sci U S A. 104(40):15817–15822.
- Honda T, Egawa G, Grabbe S, Kabashima K. 2013. Update of immune events in the murine contact hypersensitivity model: Toward the understanding of allergic contact dermatitis. J Invest Dermatol. 133(2):303–315.
- Howell M, Kim B, Gao P, Grant A, Boguniewicz M, Debenedetto A, Schneider L, Beck L, Barnes KC, Leung D. 2007. Cytokine modulation of atopic dermatitis filaggrin skin expression. J Allergy Clin Immunol. 120(1):150–155.
- Iida H, Takai T, Hirasawa Y, Kamijo S, Shimura S, Ochi H, Nishioka I, Maruyama N, Ogawa H, Okumura K, et al. 2014. Epicutaneous administration of papain induces IgE and IgG responses in a cysteine protease activity-dependent manner. Allergol Int. 63(2):219–226.
- Ivanov I, McKenzie B, Zhou L, Tadokoro C, Lepelley A, Lafaille J, Cua D, Littman D. 2006. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T-helper cells. Cell. 126(6):1121–1133.
- Kamijo S, Hara M, Suzuki M, Nakae S, Ogawa H, Okumura K, Takai T. 2021. Innate IL-17A enhances IL-33-independent skin eosinophilia and IgE response on subcutaneous papain sensitization. J Invest Dermatol. 141(1):105–113.
- Kamijo S, Nunomura S, Ra C, Kanaguchi Y, Suzuki Y, Ogawa H, Okumura K, Takai T. 2016. Innate basophil IL-4 responses against allergens, endotoxin, and cytokines require the Fc receptor γ-chain. J Allergy Clin Immunol. 137(5):1613–1615.
- Kamijo S, Suzuki M, Hara M, Shimura S, Ochi H, Maruyama N, Matsuda A, Saito H, Nakae S, Suto H, et al. 2016. Subcutaneous allergic sensitization to protease allergen is dependent on mast cells but not IL-33: Distinct mechanisms between subcutaneous and intranasal routes. J Immunol. 196(9):3559–3569.
- Kamijo S, Takeda H, Tokura T, Suzuki M, Inui K, Hara M, Matsuda H, Matsuda A, Oboki K, Ohno T, et al. 2013. IL-33-mediated innate response and adaptive immune cells contribute to maximum responses of protease allergen-induced allergic airway inflammation. J Immunol. 190(9):4489–4499.
- Kikuchi Y, Takai T, Kuhara T, Ota M, Kato T, Hatanaka H, Ichikawa S, Tokura T, Akiba H, Mitsuishi K, et al. 2006. Crucial commitment of proteolytic activity of a purified recombinant major house dust mite allergen Der p1 to sensitization toward IgE and IgG responses. J Immunol. 177(3):1609–1617.
- Kimber I, Dearman R. 2002. Allergic contact dermatitis: The cellular effectors. Contact Dermatitis. 46(1):1–5.
- Kunimine S, Takai T, Kamijo S, Maruyama N, Kimitsu T, Masutani Y, Yoshimura T, Suchiva P, Shimizu S, Ogawa H, et al. 2021. Epicutaneous vaccination with protease inhibitor-treated papain prevents papain-induced TH2-mediated airway inflammation without inducing TH17 in mice. Biochem Biophys Res Commun. 546:192–199.
- Maruyama N, Takai T, Kamijo S, Suchiva P, Ohba M, Takeshige T, Suzuki M, Hara M, Matsuno K, Harada S, et al. 2019. Cyclooxygenase inhibition in mice heightens adaptive- and innate-type responses against inhaled protease allergen and IL-33. Allergy. 74(11):2237–2240.
- McFadden J, Puangpet P, Basketter D, Dearman R, Kimber I. 2013. Why does allergic contact dermatitis exist? Br J Dermatol. 168(4):692–699.
- Milne J, Brand S. 1975. Occupational asthma after inhalation of dust of the proteolytic enzyme, papain. Br J Ind Med. 32(4):302–307.
- Nies J, Panzer U. 2020. IL-17C/IL-17RE: Emergence of a unique axis in TH17 biology. Front Immunol. 11:341.
- Niinimaki A, Reijula K, Pirila T, Koistinen A. 1993. Papain-induced allergic rhinoconjuctivitis in a cosmetologist. J Allergy Clin Immunol. 92(3):492–493.
- Nishioka I, Takai T, Maruyama N, Kamijo S, Suchiva P, Suzuki M, Kunimine S, Ochi H, Shimura S, Sudo K, et al. 2018. Airway inflammation after epicutaneous sensitization of mice requires protease activity of low-dose allergen inhalation. J Allergy Clin Immunol. 141(6):2271–2273.
- Ochi H, Takai T, Shimura S, Maruyama N, Nishioka I, Kamijo S, Iida H, Nakae S, Ogawa H, Okumura K, et al. 2017. Skin treatment with detergent promotes protease allergen-dependent epicutaneous sensitization in a manner different from Tape Stripping in Mice. J Invest Dermatol. 137(7):1578–1582.
- Paller A, Spergel J, Mina-Osorio P, Irvine A. 2019. The atopic march and atopic multi-morbidity: Many trajectories, many pathways. J Allergy Clin Immunol. 143(1):46–55.
- Pavel A, Renert-Yuval Y, Wu J, Del Duca E, Diaz A, Lefferdink R, Fang M, Canter T, Rangel S, Zhang N, et al. 2021. Tape strips from early-onset pediatric atopic dermatitis highlight disease abnormalities in nonlesional skin. Allergy. 76(1):314–325.
- Perner C, Flayer C, Zhu X, Aderhold P, Dewan Z, Voisin T, Camire R, Chow O, Chiu I, Sokol C. 2020. Substance P release by sensory neurons triggers dendritic cell migration and initiates the Type-2 Immune Response to Allergens. Immunity. 53(5):1063–1077.
- Quiñones D, Alonso S, López R, Sánchez I, Rodríguez F, Fernández L, Jerez J. 1999. Contact urticaria, rhinoconjunctivitis and bronchial asthma from occupational use of papain. Allergol Immunopathol (Madrid). 27:273–275.
- Serhan N, Basso L, Sibilano R, Petitfils C, Meixiong J, Bonnart C, Reber L, Marichal T, Starkl P, Cenac N, et al. 2019. House dust mites activate nociceptor-mast cell clusters to drive Type 2 skin inflammation. Nat Immunol. 20(11):1435–1443.
- Shimura S, Takai T, Iida H, Maruyama N, Ochi H, Kamijo S, Nishioka I, Hara M, Matsuda A, Saito H, et al. 2016. Epicutaneous allergic sensitization by cooperation between allergen protease activity and mechanical skin barrier damage in mice. J Invest Dermatol. 136(7):1408–1417.
- Sokol C, Barton G, Farr A, Medzhitov R. 2008. A mechanism for the initiation of allergen-induced T-helper Type 2 responses. Nat Immunol. 9(3):310–318.
- Spergel J, Mizoguchi E, Brewer J, Martin T, Bhan A, Geha R. 1998. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 101(8):1614–1622.
- Stremnitzer C, Manzano-Szalai K, Willensdorfer A, Starkl P, Pieper M, Konig P, Mildner M, Tschachler E, Reichart U, Jensen-Jarolim E. 2015. Papain degrades tight junction proteins of human keratinocytes in vitro and sensitizes C57BL/6 mice via the skin independent of its enzymatic activity or TLR4 activation. J Invest Dermatol. 135(7):1790–1800.
- Suárez-Fariñas M, Tintle S, Shemer A, Chiricozzi A, Nograles K, Cardinale I, Duan S, Bowcock A, Krueger J, Guttman-Yassky E. 2011. Nonlesional atopic dermatitis skin is characterized by broad terminal differentiation defects and variable immune abnormalities. J Allergy Clin Immunol. 127(4):954–964.
- Takai T, Ikeda S. 2011. Barrier dysfunction caused by environmental proteases in the pathogenesis of allergic diseases. Allergol Int. 60(1):25–35.
- Takai T, Kato T, Sakata Y, Yasueda H, Izuhara K, Okumura K, Ogawa H. 2005. Recombinant Der p 1 and Der f 1 exhibit cysteine protease activity but no serine protease activity. Biochem Biophys Res Commun. 328(4):944–952.
- Takai T. 2012. TSLP expression: Cellular sources, triggers, and regulatory mechanisms. Allergol Int. 61(1):3–17.
- Thomas W. 2015. Hierarchy and molecular properties of house dust mite allergens. Allergol Int. 64(4):304–311.
- Unutmaz D. 2009. RORC2: The master of human Th17 cell programming. Eur J Immunol. 39(6):1452–1455.
- Vandeghinste N, Klattig J, Jagerschmidt C, Lavazais S, Marsais F, Haas J, Auberval M, Lauffer F, Moran T, Ongenaert M, et al. 2018. Neutralization of IL-17C reduces skin inflammation in mouse models of psoriasis and atopic dermatitis. J Invest Dermatol. 138(7):1555–1563.
- Wang L, Chiu H, Hsu C, Liu C, Hsueh Y, Miaw S. 2009. Epicutaneous sensitization with a protein antigen induces TH17 cells. J Dermatol Sci. 54(3):192–197.
- Wang L, Lin J, Hsieh K, Lin R. 1996. Epicutaneous exposure of protein antigen induces a predominant TH2-like response with high IgE production in mice. J Immunol. 156(11):4077–4082.
- Yokozeki K, Yuki T, Ogasawara A, Katagiri A, Takahashi Y, Basketter D, Sakaguchi H. 2021. Total dose defines the incidence of percutaneous IgE/IgG1-mediated immediate-type hypersensitivity caused by papain. J Appl Toxicol. 41(6):898–906.
- Yuki T, Tobiishi M, Kusaka-Kikushima A, Ota Y, Tokura Y. 2016. Impaired tight junctions in atopic dermatitis skin and in a skin-equivalent model treated with IL-17. PLoS One. 11(9):e0161759.
