Abstract
Background: Unroofed coronary sinus is a congenital cardiac anomaly usually associated with persistent left superior vena cava. Premature restriction or closure of foramen ovale is described in association with hypoplastic left heart syndrome. Abdominal peritoneal bands when present manifest clinically. Case report: A 27 years, gravida 2, presented with intrauterine fetal death at 24 weeks gestation due to fetal congestive cardiac failure, cardiomegaly and hydrops. Perinatal autopsy showed absent coronary sinus with cardiac veins draining directly into the heart. There was no persistent left superior vena cava. The foramen ovale was restricted prematurely. The ductus arteriosus was present and non-restrictive. Abdomen showed a cysto-colic peritoneal band. Conclusion: This is the first report showing a triad of (1) complete absence of coronary sinus without left superior vena cava (type-II); (2) premature restriction of foramen ovale without hypoplastic left heart; and (3) a cysto-colic peritoneal band between the gall bladder and colon.
Introduction
Unroofed coronary sinus is a congenital cardiac anomaly usually associated with persistent left superior vena cava [Citation1,Citation2]. Premature restriction or closure of foramen ovale has been described in association with hypoplastic left heart syndrome [Citation3]. Abdominal peritoneal bands when present manifest with minor to major clinical symptoms [Citation4]. This perinatal autopsy aims to document a triad of (1) complete absence of coronary sinus without left superior vena cava (type II); (2) premature restriction of foramen ovale without hypoplastic left heart syndrome; and (3) a cysto-colic peritoneal band between the gallbladder and colon.
Case report
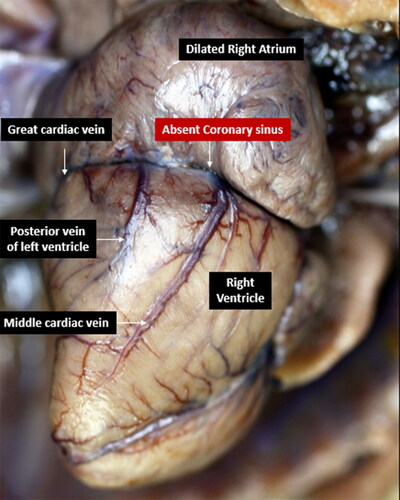
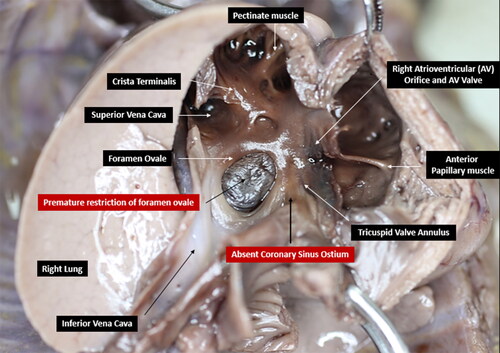
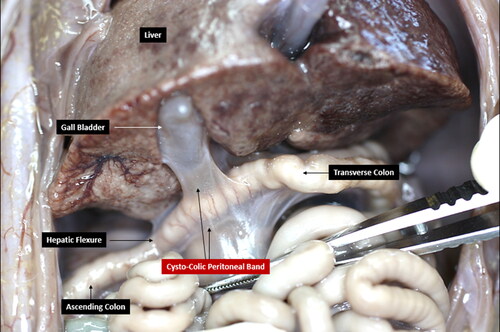
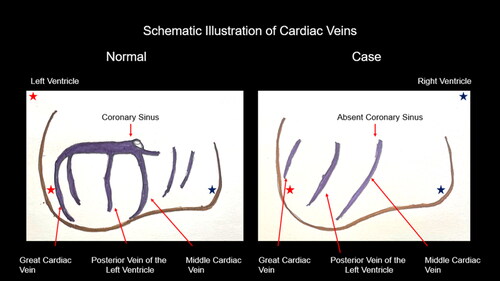
A 27 Years, gravida 2, presented with intrauterine fetal death at 24 weeks gestation due to fetal congestive cardiac failure, cardiomegaly and hydrops. Perinatal autopsy showed baby weight at 98th centile, hydrops, and enlarged liver. The venous system was engorged including brachiocephalic vein, jugular vein, inferior vena cava, renal veins and other tributaries. The heart showed absent coronary sinus with drainage of all the cardiac veins directly into the heart ( and ) without the persistent left superior vena cava (type II defect). The right atrium was dilated and the foramen ovale was restricted prematurely by a thickened and folded flap (). The ductus arteriosus was present and nonrestrictive. The aortic root had normal left and right coronary ostia, and there was no left ventricular hypoplasia. The abdomen showed an abnormal cysto-colic peritoneal band between the gall bladder and the colon ().
Figure 2. Schematic illustration of cardiac veins in a normal heart (left) and as observed in the case (right).
Discussion
The coronary sinus is formed by coalescence of venous tributaries comprised of a small, middle, great, and oblique cardiac vein; the left marginal vein; and the left posterior ventricular vein [Citation5,Citation6]. Together with the vena cavae (superior and inferior), the coronary sinus delivers deoxygenated blood to the right atrium [Citation6]. Unroofed coronary sinus is a congenital cardiac anomaly first described by Raghib et al [Citation1]. There is an overwhelming association of this anomaly with persistent left superior vena cava that drains the left internal jugular and subclavian veins into the coronary sinus [Citation7]. A persistent left superior vena cava occurs in 0.1–0.5% of the general population, with 8% draining into the left atrium [Citation2]. The morphologic type of unroofed coronary sinus have been classified as Kirklin and Barratt-Boyes types whereby (1) type I is completely unroofed with persistent left superior vena cava; (2) type II is completely unroofed but without persistent left superior vena cava; (3) type III shows partially unroofed midportion; and (4) type IV shows partially unroofed terminal portion [Citation2,Citation8,Citation9].
The foramen ovale, a transitory atrial septum aperture that allows shunting of oxygenated placental blood to the left side of the heart and into systemic fetal circulation, is formed during the fourth week of gestation [Citation10]. In most instances, the foramen ovale closes at birth or within the first three 3 months of life [Citation10]. Premature restriction or closure of foramen ovale, first described by Hansmann and Redel [Citation11], is a deleterious condition occurring either as an isolated defect or in association with other congenital and cardiovascular anomalies [Citation10]. As an isolated defect, restricted foramen ovale was identified in 23 cases by Uzun et al [Citation12] who examined 1682 fetuses ultrasonographically, reporting an overall frequency of 1.4% [Citation12]. All the restricted foramen ovale cases except for two were reported alive (21/1682 = 1.24%). Premature restriction or closure of foramen ovale in association with other anomalies was evaluated in an autopsy series by Levy et al [Citation13] who analyzed 1,150 cases of congenital heart disease and found 10 with premature restriction/closure of foramen ovale reporting a frequency of 0.8%. While, Naeye and Blanc [Citation14] reported 12 cases of prenatal narrowing or closure of the foramen ovale in their autopsy series, most other reports are anecdotal [Citation15]. Literature suggests that majority of premature restriction or closure of foramen ovale are associated with hypoplastic left heart syndrome [Citation3].
The coronary sinus is the most constant feature of the cardiac venous system [Citation16–18], and of all of the branches of the coronary venous system, the great cardiac and middle cardiac vein [Citation19] and posterior cardiac veins are the ones present most consistently [Citation17]. Many of the these major cardiac veins anastomose and two rather constant venous anastomotic rings have been described [Citation17]. The larger and more constant anastomotic ring (90%) connects the ends of the middle and great cardiac veins and the less constant (70%) ring connects the ends of the posterior and left marginal veins with a branch of the middle cardiac vein [Citation17]. All the major veins also receive inconstant albeit innumerable, smaller branches, which contribute to an anastomotic network of veins in the epicardium [Citation17]. Without the persistent left superior vena cava and left hypoplastic heart and in the absence of coronary sinus, it is tempting to speculate that the direct drainage of the major cardiac veins and their anastomotic channels into the left heart may have contributed to hemodynamic forces potentiating the closure of the foreman ovale ().
Gastrointestinal tract and mesenteric development are embryologically complex and provides a platform for the formation of a wide variety of peritoneal bands. These bands are most commonly identified in the regions of the duodenum, duodenojejunal flexure, ileocecal junction, and ascending colon. The diverse location of these variant structures result in variable clinical manifestations. These may range from bloating, constipation, nausea, vomiting, abdominal distention, intermittent to chronic vague abdominal pain, and localized abdominal tenderness. The bands may also cause relatively severe complications including intermittent colicky pain, malabsorption, intestinal malrotation with or without midgut volvulus, internal herniation, intestinal stasis and/or obstruction, necrosis, and organ atrophy [Citation4]. A Cysto-colic band, specifically, may either remain asymptomatic, manifest the aforementioned milder symptoms, or cause gallbladder atrophy, large intestinal stasis, obstruction and necrosis.
This report demonstrates a complete absence of the coronary sinus without left superior vena cava (type II defect). The case showed premature restriction of foramen ovale without hypoplastic left heart syndrome. An additional finding was an abnormal cysto-colic peritoneal band between the gallbladder and colon.
Acknowledgement
The author gratefully acknowledges Fernandez Foundation for infrastructural support.
References
- Raghib G, Ruttenberg HD, Anderson RC, Amplatz K, Adams P, Jr., Edwards JE. Termination of left superior vena cava in left atrium, atrial septal defect, and absence of coronary sinus: a developmental complex. Circulation. 1965;31:906–18. doi:10.1161/01.cir.31.6.906.
- Ootaki Y, Yamaguchi M, Yoshimura N, Oka S, Yoshida M, Hasegawa T. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg. 2003;126(5):1655–6. doi:10.1016/s0022-5223(03)01019-5.
- Noonan JA, Nadas AS. The hypoplastic left heart syndrome; an analysis of 101 cases. Pediatr Clin North Am. 1958;5(4):1029–56. doi:10.1016/S0031-3955(16)30727-1.
- Oelhafen K, Shayota BJ, Muhleman M, Klaassen Z, Shoja MM, Tubbs RS, Loukas M. Peritoneal bands: a review of anatomical distribution and clinical implications. Am Surg. 2012;78(4):377–84. doi:10.1177/000313481207800424.
- Loukas M, Bilinsky S, Bilinsky E, el-Sedfy A, Anderson RH. Cardiac veins: a review of the literature. Clin Anat. 2009;22(1):129–45. doi:10.1002/ca.20745.
- Lee HS, Song BG, Park MJ, Kim KH, Ok HS, Kim BK, Chun WJ, Oh JH. Rare case of an unroofed coronary sinus. Heart Lung. 2012;41(4):390–3. doi:10.1016/j.hrtlng.2011.12.001.
- Yonekura H, Kanazawa S, Miyawaki I, Yamazaki K. Partially unroofed coronary sinus with persistent left superior vena cava: the utility of two and three-dimensional transesophageal echocardiography: a case report. Korean J Anesthesiol. 2014;67(1):52–6. doi:10.4097/kjae.2014.67.1.52.
- Kouchoukos NT, Kirklin JW. Kirklin/Barratt-Boyes cardiac surgery: Morphology, diagnostic criteria, natural history, techniques, results, and indications. Philadelphia: Elsevier/Saunders; 2013.
- Krivenko G, Maag B, Nelson JS, Madueme P, Douglas K, Dorotan-Guevara MM. Preoperative imaging and surgical repair of a coronary sinus septal defect: A case report. Prog Pediatr Cardiol. 2022; 65:101513. doi:10.1016/j.ppedcard.2022.101513.
- Furtado LV, Putnam AR, Erickson LK, Opitz JM. Premature closure of the foramen ovale secondary to congenital aortic valvular stenosis in a stillborn. Fetal Pediatr Pathol. 2012;31(2):43–9. doi:10.3109/15513815.2011.648723.
- Redel DA, Hansmann M. Fetal obstruction of the foramen ovale detected by two-dimensional Doppler echocardiography. In: Rijsterborgh H, editor. Echocardiology. Dordrecht: Springer Netherlands; 1981. p. 425–9.
- Uzun O, Babaoglu K, Ayhan YI, Moselhi M, Rushworth F, Morris S, Beattie B, Wiener J, Lewis MJ. Diagnostic ultrasound features and outcome of restrictive foramen ovale in fetuses with structurally normal hearts. Pediatr Cardiol. 2014;35(6):943–52. doi:10.1007/s00246-014-0879-5.
- Lev M, Arcilla R, Rimoldi HJ, Licata RH, Gasul BM. Premature narrowing or closure of the foramen ovale. Am Heart J. 1963;65:638–47. doi:10.1016/0002-8703(63)90126-1.
- Naeye RL, Blanc WA. Prenatal narrowing or closure of the foramen ovale. Circulation. 1964;30:736–42. doi:10.1161/01.cir.30.5.736.
- Olson RW, Nishibatake M, Arya S, Gilbert EF. Nonimmunologic hydrops fetalis due to intrauterine closure of fetal foramen ovale. Birth Defects Orig Artic Ser. 1987;23(1):433–42.
- von Lüdinghausen M. Clinical anatomy of cardiac veins, Vv. cardiacae. Surg Radiol Anat. 1987;9(2):159–68. doi:10.1007/BF02086601.
- Parsonnet V. The anatomy of the veins of the human heart with special reference to normal anastomotic channels. J Med Soc N J. 1953;50(10):446–52.
- Mantini E, Grondin CM, Lillehei CW, Edwards JE. Congenital anomalies involving the coronary sinus. Circulation. 1966;33(2):317–27.
- Gilard M, Mansourati J, Etienne YVES, Larlet J-M, Truong B, Boschat J, Blanc J-J. Angiographic anatomy of the coronary sinus and its tributaries. Pac. Clin Electr. 1998;21(11):2280–4. doi:10.1111/j.1540-8159.1998.tb01167.x.