 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose: Detection of body stuffers is challenging in emergency departments. Because of the small size of baggies, plain radiograph is of little value in most suspects. On the other hand, abdomen CT scan is burdened by high cost and radiation dose. This study was performed to compare the image quality, radiation dose and accuracy of low-dose CT scan in comparison with standard dose.
Material and methods: In this prospective study, suspected body stuffers who were referred to the radiology department underwent two different protocols of abdominal non-contrast CT scan simultaneously: low-dose (with equivalent dose to conventional abdominal x-ray) and standard dose. Standard dose CT scan was considered as the reference. Low-dose CT scans were evaluated for detection of baggies by two radiologists blinded to the result of standard dose CT. Image quality, noise, dose-length product (DLP) and effective dose (ED) compared between two groups.
Results: The study consisted of 40 patients (33.38 ± 7.4 years). Standard dose CT evaluation was positive in 22 patients (55%). In comparison with standard dose CT scan, low-dose group had a sensitivity of 86%, specificity of 100%, PPV and NPV of 100% and 86%. The accuracy of low-dose CT scan for detection of baggies larger than 1 cm was 100%. However, from the 3 cases that could not be detected with low dose protocol, one had CT features suspected for baggies rupture which was intubated and later deceased. Noise average of low-dose protocol, was approximately 7 times greater than standard dose group, while DLP and ED were 9.7 times less.
Conclusion: Low dose CT scan appears to be an appropriate screening method for body stuffers, especially when the baggies are larger than one centimeter. However, in the presence of severe clinical symptoms, a standard dose CT scan will be more helpful due to better image quality especially in suspected ruptured baggies.
Keywords:
Introduction
“Body packing”, refers to smuggling multiple drug packets by intracorporeal means such as swallowing or inserting them in rectal or vaginal cavities [Citation1]. In contrast to body packers, stuffers or mini-packers swallow smaller baggies (3–20 mm) [Citation2]. They are usually street drug dealers or users, who hastily ingest fewer drug pellets. Because of loose and insecure drug wrapping, body stuffers are prone to encounter leakage or rupture of packets, which can be fatal [Citation3–5]. Emergency departments increasingly deal with drug mules in recent years. Therefore, using the appropriate diagnostic tool is of great concern. Low drug metabolite concentrations of body stuffers may not be detected by toxicology tests [Citation6]. On the other hand, a portion of body stuffers has addiction history that renders the test results positive without real smuggling [Citation7].
Diagnostic imaging has a key role in identifying ingested packages. Acceptability of plain abdominal radiography as a screening tool for suspected body packers is due to its simplicity, low cost and radiation dose [Citation8]. However, conventional x-ray is an unhelpful investigation for body stuffers with significant false negative results because of limited contrast resolution, small number and size of pellets [Citation3,Citation5]. Ultrasound has low specificity for body packers [Citation9] and its usefulness in body stuffers is unclear. Therefore, imaging diagnosis mostly relies on CT examination as a fast and relatively accurate diagnostic tool. It should be performed without contrast agents [Citation10]. Scout CT view can be used as a substitute for plain X-ray [Citation5] and packet detection rate is improved by reviewing in lung window setting, in addition to the usual window for abdomen [Citation11]. Although high resolution CT scan has false negative results too [Citation12,Citation13], it has remained the best available imaging modality, considering the unreliable history presented by body stuffers [Citation4,Citation5,Citation10].
Widespread usage of routine CT scan is burdened by its radiation dose. Besides, repeated imaging may be needed to follow the passage of packets from the gastrointestinal tract with consequent cumulative radiation dose [Citation5]. Low-dose CT protocols may overcome this concern by producing acceptable image quality with lower radiation exposure. Low-dose CT scan has been performed for detection of appendicitis [Citation14,Citation15] and renal stones [Citation16]. Recent investigations have examined the sensitivity and specificity of low dose CT protocols for detection of body packers [Citation17,Citation18]. Also, low dose dual-energy CT scan has studied a small population of suspected body packers and body stuffers for discriminating cocaine from heroin filled packets [Citation19]. However, the efficacy of low dose CT scan in body stuffers remained to be elucidated.
The purpose of this study is to evaluate the diagnostic performance and image quality of low dose CT protocol in detection of illicit drug stuffers, in comparison with standard dose as the reference.
Material and methods
In a prospective observational study, we identified all potential patients who had ingested at least a pack of illicit drug and referred to a large tertiary poison center hospital from July to December 2015 with an annual ED census of 24–28 thousand poisoning cases [Citation20,Citation21]. They were interviewed by a research assistant to document their demographic and clinical characteristics. Patients self-reporting baggie ingestion AND had a positive urine test OR expelled baggies were recruited in the study. Participants underwent both low-dose and standard-dose CT scans at the same time. Body packers were excluded. The study protocol was approved by the ethical committee of the university. Informed consent was obtained from each patient and they were made aware of additional radiation exposure of low-dose CT scan (estimated at a similar dose to plain abdominal X-ray).
Both CT protocols were obtained stretched from lung base to the pelvis without administration of contrast agents, by using the 16-MDCT unit (Activion 16, Toshiba, Japan), with following parameters: Pitch Factor: 1.4, rotation time: 0.75, 5 mm and 2.5 mm section thickness and interval. Standard-dose CT scan was performed with automated mA tube charge and tube potential of 120 kV. On the other hand, low-dose CT scan was done with 80 kV and 50 mA tube potential and charge (). Images were sent to PACS (Picture Achieving and Communication System), immediately (Medal Electronic Workstation, Tehran, Iran).
Table 1. MDCT Low dose versus standard dose protocols.
Delivered dose by CT protocols was estimated using CTDI (CT dose index) in the air. Radiation exposure calculated as:
in which DLP is the dose-length product, CTDIvol is the volume of CTDI and L is the scan length. Effective dose (ED) is used to compare patient doses for different imaging modalities. The unit is milliSievert (mSv) and calculated as DLP × k, in which k (mSv/(mGy cm)) is a specific conversion factor set as 0.015 for abdominal CT as American Association of Physicists in Medicine report in 2008 [Citation22]. CTDIvol and DLP of both protocols were reported in the last image of every CT image series, according to the manufacturing factory data setting.
Standard-dose CT images were interpreted by attending radiologists the next day, and the written report was sent to the referring physician. Low-dose CT images were stored in the PACS. At the end of the study, low-dose CT scans were analyzed independently by two attending radiologists, with 8 and 4 years’ experience in abdominal CT who were blinded to standard-dose CT findings and patient information.
Once all low-dose CT examinations were interpreted, standard-dose CT images were analyzed a second time, in a random order, by the same two reviewers, using the same workstation and software. Data set were reviewed for baggies in soft tissue and lung window setting. CT report information including presence or absence of pellets, package number, size and density of positive cases were recorded in a form. If non-accordance occurred in the presence/absence of pellets, read-out was performed in consensus of both radiologists. The number, size and density of baggies were calculated as the mean of measures by two radiologists for each series. Package rupture or leak was suspected when there was hyperdense semi-fluid content mixed with enteric content or layered within the dependent portion of lumen [Citation23].
Image quality was determined in two ways:
Qualitative method according to subjective analysis in 4 scores as 1 = not-acceptable, 2 = acceptable, 3 = good and 4 = excellent.
Quantitative method by calculation of the mean noise. Densitometric circle object (region of interest, ROI) with a constant radius placed over the air around the trunk at 3 spaces, (midline, flank and mid-axillary line) at the level of L1. Standard deviation of air density at each region recorded and the mean of 3 measures calculated.
Severe clinical outcome determined as hypertensive urgency (systolic blood pressures above 180 mmHg OR diastolic blood pressure above 120 mmHg), OR occurrence of seizure, OR severe agitation requiring continuous sedation in intensive care unit, OR myocardial ischemia/infarction, OR cerebrovascular accidents, OR decreased level of consciousness, OR respiratory depression mandating intubation or death AND any organ damage requiring therapy [Citation24].
Statistical analysis was performed using SPSS version 19. Low-dose CT scan results for packet detection were compared with standard-dose protocol as the reference standard method and sensitivity, specificity, negative predictive value, positive predictive value was calculated. McNemar’s test was used to pair standard versus low dose CT protocols. Descriptive approach was applied to compare the patients’ demographic characteristics, clinical findings and outcome. For qualitative variables, percent of frequency and for quantitative variables with normal and non-normal distribution, mean (±SD) and median (interquartile range) were used, respectively. Significance level fixed at %5 (p value = .05).
Results
The study population consisted of 40 suspected body stuffers, 39 (97.5%) male and 1 (2.5%) female, age range 19–51 years; mean age, 33.38 ± 7.4 years. The content of packets was amfetamine/metamphetamine in thirteen (32.5%), opioid in fifteen (37.5%) and mixed amfetamine/metamphetamine and opioid in 6 (15%) patients. No cocaine or cathinone was detected. Baggies’ contents in 6 patients remained unknown. All baggies were wrapped in plastic cover either sealed or heated bags. The patients were referred to emergency department with the time range of half an hour up to 48 hours after pellet ingestion (mean 5 hours and 51 minutes).
Vital signs and selected clinical manifestations are presented in . There were four patients with severe outcome. Three were unresponsive requiring intubation, two of them deceased. One patient had seizure during the hospitalization.
Table 2. Clinical manifestation and severe outcome in each CT group.
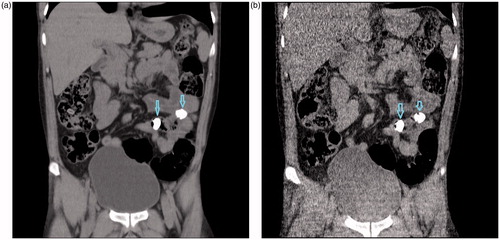
In analysis of standard-dose CT scan, 22 (55%) of total cases were considered to have evidence of body stuffing, of which 6 (27%) had less than three, 5 (22%) had three to five and 9 (41%) had five or more baggies. On the other hand, baggies were found in 19 (47%) cases of low dose protocol, of which 8 (42%) had less than three, 6 (32%) had three to five and 4 (21%) had five or more pellets (). The median number of pellets in low-dose group was 3 versus 3.5 in standard dose group (p = .1). There were three patients that low dose CT scan demonstrated less number of packets as 1, 1 and 3 compared to 6, 7 and 7 packets in standard dose group, respectively with the mean size of missed packets less than one centimeter. There was evidence of ruptured package in two (9%) cases in standard dose group in comparison with one (5%) in low dose category.
Figure 1. Reformatted coronal non-contrast abdominopelvic CT images of a 33-year-old man with the history of package ingestion, who underwent both CT protocols: Standard dose CT, (a) and low dose (b) represent two drug baggies (arrows) within small bowel loops.
Of the 40 cases, location of baggies was determined in 22 cases as follow: 9 cases with baggies in the stomach, 2 in proximal small bowel, 2 in distal small bowel, 2 cases with concurrent baggies in the stomach and proximal small bowel, 4 cases with concurrent baggies in the stomach and colon and 3 cases with baggies in the colon and rectum. In both groups, most packages were detected in stomach, 58% versus 53% in standard and low dose groups, respectively.
The size of pellets was between 5 and 40 mm in both groups. Mean diameters were 17.6 and 17.8 mm in low dose and standard dose groups, respectively (p = .845). Sixteen out of 19 (84%) of detected packs in low dose CT were 10 mm and larger, in comparison with thirteen out of 22 (59%) in standard dose CT images. The median density of baggies was 200 Hounsfield unit (HU) in low dose group (range: 97–1717) and 148 HU in standard dose group (range: 57–1220, p = .023). We were unable to correlated Hounsfield unit with opioids or met/amfetamine.
Radiation dose calculated as CTDIvol, DLP and ED together with image noise are listed in . Visual grading score between two readers is presented in . The inter-rater agreement of Kappa was 0.41 (p = .001) in standard-dose group, however was not significant in low-dose group. There was one unacceptable study in low dose group according to each reader.
Table 3. CTDIvol, DLP, Effective dose and mean noise in two different protocols.
Table 4. Visual grading score (rater 1 and rater 2) by using a four-step scale (1 = not-acceptable, 2 = acceptable, 3 = good and 4 = excellent.
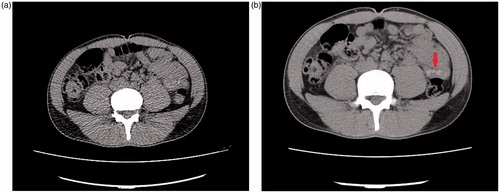
When compared with standard dose protocol, low dose CT had 86% sensitivity and 100% specificity for detection of any packets in each patient. Positive predictive value and negative predictive value were 100% and 86%, respectively. McNemar’s test was not significant between standard and low dose CT group. Compared to standard CT as the reference, there were 3 cases that could not be detected in low dose CT. One was hyperdense semi-fluid content layered in the stomach which was suspected to result from the rupture of the baggies and could not be appreciated in low dose CT (). The patient was later intubated and subsequently the patient died. Two other cases had 6 mm and 8 mm hyperdense foci in colon and stomach, with the mean size of foreign content measuring less than one centimeter (). Both had favorable outcome and been discharged.
Figure 2. Axial CT images without contrast of a 48-year-old man: (a) standard dose CT image reveals hyperdense content within the dependent portion of stomach (arrow) likely representing ruptured package which cannot be clearly seen in low dose images (b).
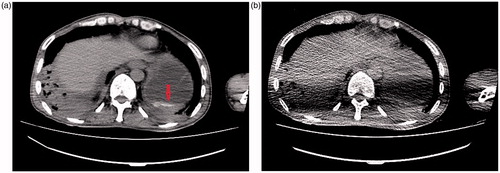
Figure 3. Axial non-contrast CT images of a 35-year-old body stuffer. With the low dose protocol (a), No definite pellets detected in abdomen secondary to increased image noise, however standard dose image (b) shows few small pellets in bowel loops in left abdomen (arrow).
In terms of severe outcome (), there were three other cases, one with seizure which demonstrated baggies detected in both standard and low dose protocols. Two other cases which were intubated had negative CT results in both protocols and one of them passed away.
Discussion
Intracorporeal drug transport is a potentially life-threatening condition. Despite lower mortality rate of stuffers compared to body packers [Citation25], there are some reports of death in body stuffers [Citation3]. There were four cases resulting in severe outcome in our study with two deaths. Definite diagnosis of body stuffers is a clinical challenge because of multiple limitations. The history is unreliable in many cases because of the legal concerns [Citation5]. Some packers/stuffers arrive in the emergency department with decreased level of consciousness and a drug toxicity diagnosis [Citation26]. Available toxicological tests are not specific enough to differentiate between daily dose of addicted patients and those who may overdosed through rupture of baggies [Citation7]. Baggies without proper cover are prone to leak or rupture, therefore collection of stool in safeguard toilets would be falsely negative [Citation5]. Imaging modalities also do not have satisfying sensitivity and specificity in body stuffers since the amount of ingested material both in number and size are small to be confidently detected in CT scan. Small pellets can even be missed and inadvertently ruptured at the time of surgery [Citation27].
Radiologic departments are facing these CT studies frequently and a conclusive diagnosis may not be made. CT findings needed to be correlated to the underlying clinical context and ancillary biochemical results [Citation1]. There is not a universal guideline for the role of CT scan in body stuffers and the trend of its usage is diverse [Citation4,Citation25]. In some medical centers, it is limited to the cases with abdominal symptoms for exclusion of complication. Other emergency departments may use the CT scan for exclusion of large amounts of body trafficking which is mostly denied by the suspect worrying the legal consequences. In this regard, plain abdominal X-ray does not have enough sensitivity even in body packers in comparison with the low dose CT scan [Citation3,Citation5,Citation17]. Since the detection of baggies in body stuffers are even difficult with standard-dose CT scan, and then the question is by reducing the radiation dose, how much difference will occur in accuracy and especially in sensitivity. Earlier, the accuracy of low-dose CT was examined in body packer population, whose packs are larger and more obvious [Citation17,Citation18]. Some studies were targeted animals as population group [Citation28]. Low dose study in body stuffers has been performed in a limited group of 6 suspected body stuffers with dual energy CT scan. Our study aimed to compare low-dose CT scan protocol with standard-dose, as the reference method for body stuffer’s screening. So far, no prior study was conducted with the same methodological approach.
Previously, Poletti et al. [Citation16] demonstrated that in cases with suspected renal colic, low dose CT scan had sensitivity of 100% for ureteral calculi larger than 3 mm while sensitivity decreased to 86% if calculi were less than 3 mm. In a similar way, we showed that low dose CT scan had similar sensitivity to standard dose for detection of baggies larger than 10 mm. There is no solid reference to suggest a safe size for the baggies in body stuffers and even baggies less than one centimeter would have the potential for mortality especially in unhabituated user and considering that baggies in body stuffers are more prone to leak or rupture. Nevertheless, it would not change the clinical management unless there is large size or non-progressive baggies, which can be well diagnosed with low dose scans while imposing less radiation. On-time diagnosis of body-stuffing may even convince the treating physicians to evacuate baggies by endoscope and avoid probable surgical interventions [Citation29].
Of the two patients that died in our study, one was intoxicated with a combination of stimulants and opioids and had negative results in both CT protocols. The other one with opioid toxicity had semi-fluid hyperdense content in the stomach suspected to represent ruptured packet which could not be well seen in low dose CT scan due to higher noise level (). The quality might become even worse in these cases with decreased consciousness due to artifacts from respiratory motion and patient’s hand beside the torso as in our case. In these situations, with adverse clinical features, it seems to be more reasonable to obtain a standard dose protocol. From clinical perspective, low dose CT and even standard dose protocol may not be able to detect ruptured baggies, which could lead to significant toxicity and the physician in charge should treat the patients accordingly and none of the present imaging studies have an effective role to prognosticate the patient or change the management. On the other hand, in the absence of adverse clinical signs and symptoms and negative low dose CT results, the patient likely will not require further imaging.
In our study, low-dose CT scan detected less number of baggies however the difference was not statistically significant. The mean diameter of missed baggies was below 10 mm which most likely explains their non-visualization with low dose protocol. Most pellets were found in the stomach, which can be secondary to early imaging after early admission of patients. Previous studies described higher attenuation values of the packets when applying lower tube voltage [Citation18,Citation19]. We found a similar increase in mean densities of the baggies in low dose group which was significant. Increase in CT attenuation is suggested to be caused by increased photoelectric effect produced by the low tube voltage setting which depends on the mean atomic number of the material being scanned [Citation30].
In low dose CT scan, the DLP and ED were reduced 9.7 times in comparison to standard dose. It was resulted from reduction in both tube voltage and tube charge depicted as kV and mA, respectively. The effective dose was 0.93 mSv which is in the range of effective dose for an abdominal radiograph (from 0.04 to 1.1 mSv) [Citation16–19]. Lack of sufficient accuracy in body stuffer evaluation makes abdominal X-ray undesirable. Number and size of baggies, presence of bowel gas and impacted feces, along with low contrast resolution influence on image interpretation. Earlier detection of possible complications and quicker discharge of negative cases can overcome higher cost of CT scan over radiography.
As expected, overall visual quality was higher in standard dose group compared to the low dose. The interobserver agreement for visual grading score was moderate (kappa =0.41) in standard dose group while it was poor in low dose group. It is likely related to poor quality of images in the low dose CT group compared to the standard CT group. One of the readers (reader 2) assigned most of the cases as just acceptable while the other reader (reader 1) assigned some of them to be of good quality (). There was only one study in low dose group assigned as unacceptable by each reader within 40 cases (). Aissa et al. [Citation18] demonstrated no unacceptable images however they used tube voltage of 100 kV, compared to lower tube voltage of 80 kV with lower radiation dose in our study. The mean noise in standard dose group was 8.01 in our study which is comparable to previous investigations [Citation18,Citation19]. In lower dose group, it was 6.9 times more which is secondary to concurrent reduction in tube voltage and charge with the resultant grainier appearance of the images. Also, the presence of streak artifact due to bony pelvis limited the assessment of baggies in the lower intestinal tract. Because of a low number of obese patients, we did not evaluate the effect of BMI on image quality. According to previous studies, higher BMI can burden the image analysis [Citation16,Citation17]. However, Keyzar et al. [Citation14] did not reveal any difference in image analyzing between BMI subgroups.
As discussed earlier, there is no single gold standard for detection of body stuffers or uniform generally accepted imaging feature of the baggies. We used standard dose CT scan as “reference”, and the best available imaging modality to compare our proposed low dose protocol with. Therefore, the calculated sensitivity, specificity, PPV and NPV is based on that. None of the two methods can detect all the baggies or be confident about their leak or rupture. Another limitation is the relative low sample size of the study.
Our study suggests that low dose CT scan has a close sensitivity to standard dose CT scan in detection of suspected body stuffers reaching the same sensitivity for baggies greater than 1 cm. The selection of CT protocol should be tailored to clinical symptoms. In the absence of adverse clinical features, low dose CT scan would be a good substitute for standard dose to rule out body packers or large-size body stuffers and their presumable follow up. In the presence of severe clinical symptoms, a standard dose CT scan will be more helpful due to better image quality especially in suspected ruptured baggies.
Ethical approval
Regulatory and ethical approvals were obtained and all prospectively recruited patients gave informed written consent.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Acknowledgement
This article has been extracted from the thesis written by Dr Zahra Mahboubi-Fooladi in School of Medicine Shahid Beheshti University of Medical Sciences (Registration No: 386M).
Disclosure statement
All the authors declare that he/she has no conflict of interest.
References
- Bulakci M, Kalelioglu T, Bulakci BB, et al. Comparison of diagnostic value of multidetector computed tomography and X-ray in the detection of body packing. Eur J Radiol. 2013;82:1248–1254.
- Püschel K, Stein S, Stobbe S, et al. Analysis of 683 drug packages seized from “body stuffers”. Forensic Sci Int. 2004;140:109–111.
- June R, Aks SE, Keys N, et al. Medical outcome of cocaine body stuffers. J Emerg Med. 2000;18:221–224.
- Schmidt S, Hugli O, Rizzo E, et al. Detection of ingested cocaine-filled packets—diagnostic value of unenhanced CT. Eur J Radiol. 2008;67:133–138.
- Flach PM, Ross SG, Ampanozi G, et al. “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol. 2012;81:2518–2526.
- Marc BR. Managing high-risk body-stuffers who swallow the evidence. J Forensic Leg Med. 2008;15:200–201.
- Pollack CV, Biggers DW, Carlton FB, et al. Two crack cocaine body stuffers. Ann Emerg Med. 1992;21:1370–1380.
- Hergan K, Kofler K, Oser W. Drug smuggling by body packing: what radiologists should know about it. Eur Radiol. 2004;14:736–742.
- Cengel F, Bulakci M, Selcuk T, et al. The role of ultrasonography in the imaging of body packers comparison with CT: a prospective study. Abdom Imaging. 2015;40:2143–2151.
- Shahnazi M, Hassanian-Moghaddam H, Gachkar L, et al. Comparison of abdominal computed tomography with and without oral contrast in diagnosis of body packers and body stuffers. Clin Toxicol. 2015;53:596–603.
- Bahrami-Motlagh H, Vakilian F, Hassanian-Moghaddam H, et al. Added value of lung window in detecting drug mules on non-contrast abdominal computed tomography. Radiol Med. 2016;121:472–477.
- Sengupta A, Page P. Window manipulation in diagnosis of body packing using computed tomography. Emerg Radiol. 2008;15:203–205.
- Eng JG, Aks SE, Waldron R, et al. False-negative abdominal CT scan in a cocaine body stuffer. Am J Emerg Med. 1999;17:702–704.
- Keyzer C, Tack D, De Maertelaer V, et al. Acute appendicitis: comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology. 2004;232:164–172.
- Seo H, Lee KH, Kim HJ, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose iv contrast-enhanced CT scans. Am J Roentgenol. 2009;193:96–105.
- Poletti PA, Platon A, Rutschmann OT, et al. Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR Am J Roentgenol. 2007;188:927–933.
- Poletti PA, Canel L, Becker CD, et al. Screening of illegal intracorporeal containers (“body packing”): is abdominal radiography sufficiently accurate? A comparative study with low-dose CT. Radiology. 2012;265:772–779.
- Aissa J, Rubbert C, Boos J, et al. Low-tube voltage 100 kVp MDCT in screening of cocaine body packing: image quality and radiation dose compared to 120 kVp MDCT. Abdom Imaging. 2015;40:2152–2158.
- Fornaro J, Leschka S, Hibbeln D, et al. Low dose dual-energy computed tomography in suspected body packers and body stuffers—preliminary clinical experience. J Forensic Radiol Imaging. 2013;1:83.
- Hassanian-Moghaddam H, Zamani N, Rahimi M, et al. Acute adult and adolescent poisoning in Tehran, Iran; the epidemiologic trend between 2006 and 2011. Arch Iran Med. 2014;17:534.
- Hassanian-Moghaddam H. An educational and research opportunity for the largest university hospital poison control centers; Tehran and Cairo. Egypt J Forensic Sci. 2013;2:64–65.
- American Association of Physicists in Medicine, College. The measurement, reporting, and management of radiation dose in CT. Report No. 96. Park; 2008.
- Shahnazi M, Taheri MS, Pourghorban R. Body packing and its radiologic manifestations: a review article. Iran J Radiol. 2011;8:205.
- Matsumoto RR, Seminerio MJ, Turner RC, et al. Methamphetamine-induced toxicity: an updated review on issues related to hyperthermia. Pharmacol Ther. 2014;144:28–40.
- Moreira M, Buchanan J, Heard K. Validation of a 6-hour observation period for cocaine body stuffers. Am J Emerg Med. 2011;29:299–303.
- Booker RJ, Smith JE, Rodger MP. Packers, pushers and stuffers—managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26:316–320.
- Bahrami-Motlagh H, Hassanian-Moghaddam H, Behnam B, et al. Failure of surgical treatment in methamphetamine body-stuffers. J Forensic Legal Med. 2015;32:70–72.
- Maurer MH, Niehues SM, Schnapauff D, et al. Low-dose computed tomography to detect body-packing in an animal model. Eur J Radiol. 2011;78:302–306.
- Shabani M, Zamani N, Hassanian-Moghaddam H. Endoscopic retrieval of baggies in body stuffers. Endosc Int Open. 2016;4:E443–E445.
- Nakaura T, Kidoh M, Nakamura S, et al. Low-dose abdominal CT protocols with a tube voltage setting of 100 kVp or 80 kVp: performance of radiation dose reduction and influence on visual contrast. Clin Radiol. 2014;69:804–811.
