Abstract
Introduction
Intentional pesticide poisoning is a major clinical and public health problem in agricultural communities in low and middle income countries like Nepal. Bans of highly hazardous pesticides (HHP) reduce the number of suicides. We aimed to identify these pesticides by reviewing data from major hospitals across the country and from forensic toxicology laboratories.
Methods
We retrospectively reviewed medical records of 10 hospitals for pesticide poisoned patients and two forensic laboratories of Nepal from April 2017 to February 2020. The poison was identified from the history, referral note, and clinical toxidrome in the hospitals and from gas chromatography analysis in the laboratories. Data on demographics, poison, and patient outcome were recorded on a data collection sheet. Simple descriptive analysis was performed.
Results
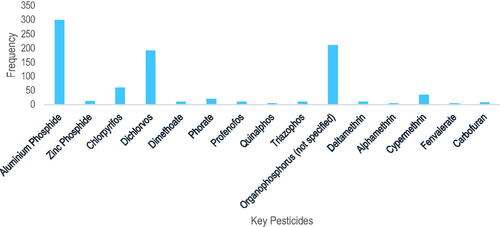
Among hospital cases (n = 4148), the commonest form of poisoning was self-poisoning (95.8%) while occupation poisoning was rare (0.03%). Case fatality was 5.3% (n = 62). Aluminum phosphide (n = 38/62, 61.3%) was the most commonly identified lethal pesticide for deaths. Forensic toxicology laboratories reported 2535 deaths positive for pesticides, with the compounds most commonly identified being organophosphorus (OP) insecticides (n = 1463/2535; 57.7%), phosphine gas (n = 653/2535; 25.7%; both aluminum [11.8%] and zinc [0.4%] phosphide) and organochlorine insecticides (n = 241/2535; 9.5%). The OP insecticide most commonly identified was dichlorvos (n = 273/450, 60.6%).
Conclusion
The data held in the routine hospital medical records were incomplete but suggested that case fatality in hospitals was relatively low. The pesticides identified as causing most deaths were dichlorvos and aluminum phosphide. Since this study was completed, dichlorvos has been banned and the most toxic formulation of aluminum phosphide removed from sale. Improving the medical record system and working with forensic toxicology laboratories will allow problematic HHPs to be identified and the effects of the bans in reducing deaths monitored.
Introduction
Suicide is a major global public health problem with estimated 700,000 deaths every year, 79% of which occur in low- and middle-income countries (LMICs) [Citation1]. The official suicide rate in South East Asia region is 13.4 per 100,000 [Citation2], but is likely to be substantially higher due to stigma and under-reporting [Citation3]. Pesticide self-poisoning accounts for about one in five of global suicides [Citation4]. In LMICs, self-poisoning with pesticide is a common method to attempt suicide [Citation5–7].
Nepal is an agricultural country where pesticides are widely used for pest control and easily accessible [Citation8,Citation9]. Poisoning is the second most common method of suicide in Nepal after hanging [Citation10]. The exact burden of pesticide self-poisoning in Nepal is not known, partly because of underreporting due to stigma and perceived negative consequences associated with suicide and attempted suicide and partly due to gaps in reporting [Citation11]. National data are available for 2017 and 2018 [Citation10]. During these years, 5317 and 5819 suicides were reported to the police (total 11,136); 2535 (22.8%) suicides were due to poisoning of which more than 90% of cases are due to pesticides.
Pesticide self-poisoning with highly hazardous pesticides (HHPs) often leads to death, particularly in a situation where medical facilities are distant or antidotal therapy or intensive care unavailable [Citation7]. Ingestion of less harmful pesticides [Citation12] rarely results in death. There is, therefore, a wide variation in case fatality after pesticide self-poisoning [Citation13], irrespective of the level of intent [Citation14]. Removing HHPs from agriculture has been shown to be a highly effective approach to suicide prevention [Citation6,Citation15]; however, this requires identification of the pesticides responsible for most suicides in a country or region. The important HHPs are unknown for Nepal. Methyl parathion and monocrotophos were previously important for suicide but were banned in the 2000s. It is likely that other pesticides have taken their place.
This study aimed to identify the HHPs commonly used for self-poisoning and important for suicide, with the expectation that this knowledge will guide national pesticide regulation decisions, ultimately removing the HHPs from agricultural use [Citation15].
Methods
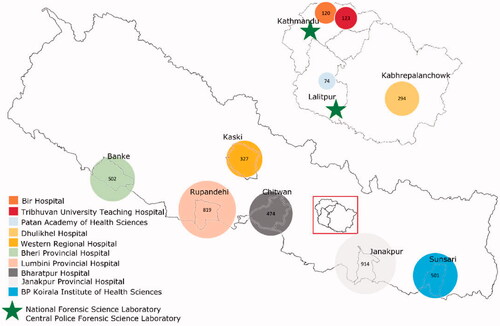
The study took place in 10 tertiary care hospitals of 9 different districts () and in Nepal’s two forensic toxicology laboratories. Since all poisoning cases in Nepal are referred to hospitals with intensive care units, all selected hospitals were large tertiary hospitals with advanced equipment. The study focused on government hospitals since they are more accessible for low income patients not able to pay for private hospitals. Unable to cover all seven provinces of Nepal, the study concentrated on 10 larger hospitals in agriculture-intensive areas and high poisoning rates of five provinces (the agricultural “Terai belt” of Nepal). The hospitals in Kathmandu valley represent central referral centers for the country. Ethical approval was received from Nepal Health Research Council, Government of Nepal (Reg. no. 535/2017).
Figure 1. Map of Nepal showing the hospitals and forensic science laboratories from which data were collected. The size of the circle relates to the case number at each site. Created for this publication using Microsoft excel and QGIS version 3.12.3.
Pesticide self-poisoning data from hospitals
We extracted anonymized, unlinked information from the medical records of patients presenting to hospital with pesticide poisoning by any means (including intentional self-poisoning, occupational and other unintentional). Occupational poisoning resulted from exposure to the pesticide while spraying it in the field.
In our first visit to the medical records department of each hospital, we collected 1 year of retrospective data of all the pesticide poisoning cases before collecting additional data for the next 1–2 years during 1–3 further visits to the hospitals (). Two trained researchers reviewed all medical records of patients with pesticide poisoning presented to emergency department of study hospitals, with only one hospital having an electronic data recording system. Based on the emergency department records (which reported a basic diagnosis for all patients admitted to hospital), the researchers retrieved patient files of each pesticide poisoned patient from medical records department. Data on demographics, pesticide exposure, and patient outcome were recorded in a data collection sheet. The pesticide was identified from the history, referral note and/or clinical toxidrome.
Table 1. Case number and timing by hospital.
Pesticide suicide data from forensic science laboratories
All unnatural deaths, including deaths from poisoning, in Nepal trigger a medicolegal investigation by the police. For poisoning cases, samples of gastric contents are sent to a forensic toxicology laboratory for analysis. We collected data on pesticide poisoning deaths analyzed in Nepal’s two forensic toxicology laboratories, namely the Central Police Forensic Science Laboratory (CPFSL) and the National Forensic Science Laboratory (NFSL). CPFSL receives samples of all fatal poisoning cases from 72 districts while NFSL receives samples from 5 districts (Bhaktapur, Lalitpur, Dhading, Sindhupalchok, Kavrepalanchok) around Kathmandu, at the request of the Nepalese police due to police case overload. Data were collected from 14 July 2017 to 20 February 2020 from CPFSL and 13 April 2017 to 15 July 2019 from NFSL.
NFSL identifies the exact pesticide present in gastric contents. In contrast, CPFSL routinely identifies the exact pesticide but only reports the pesticide chemical class (e.g., “OP insecticide”), unless this information is required by the court.
Statistics
Simple descriptive analysis was done using SPSS version 20 (SPSS Inc., Chicago, IL).
Results
Retrospective review of medical records from ten study hospitals across Nepal identified 4148 patients with pesticide poisoning who presented to their emergency departments between April 2017 and March 2020. A total of 2535 fatal cases of fatal pesticide poisoning were identified from Nepal’s two forensic toxicology laboratories.
Pesticide self-poisoning among patients presenting to hospitals
Of the 4148 hospital pesticide poisoning cases, 1192 (28.7%) did not have information on the type of poisoning (i.e., intentional, occupational, or other unintentional). Where identified, the majority of cases were intentional (2831/2956, 95.8%), with a minority unintentional (124/2956, 4.2%). Only a single case of occupational poisoning was recorded.
Patients were most commonly: women (n = 2533, 61.3%; unknown gender n = 15), of the Janajati ethnic group ((n = 1063 27.7%) [Citation16], and aged 16–30 years ((n = 2350, 57.5%). Median age of patients was 25 years (IQR 19–35), with a small difference between sexes (male: 27 [20–40]; female 24 (18–33).
Poisoning agents and outcome in hospital cases
The pesticide used in poisoning was not reported in the medical notes for 2047/4148 (49.3%) of cases. Where reported (n = 2101), the top five pesticides used in pesticide self-poisoning were zinc phosphide (n = 560, 26.7%), cypermethrin (n = 314, 14.9%), the combination product chlorpyrifos 50% + cypermethrin 5% (n = 292, 13.9%), aluminum phosphide (n = 170, 8.1%) and dichlorvos (n = 161, 7.7%). The majority of pesticides recorded in the notes were WHO hazard class II pesticides (45%) followed by Ib pesticides (32.4%) and Ia pesticides (11.2%) [Citation12].
The final outcome was not reported in the medical notes for about half of the cases (n = 1849, 44.6%). Among the remaining cases (n = 2299), the majority were discharged alive (n = 1476, 64.2%), transferred to another hospital (n = 323, 14.0%), or left against medical advice (n = 222, 9.7%). The medical notes reported deaths in 121 cases, giving a case fatality of 5.3% (). Deaths were more common in men (n = 67, 55.4%); most patients who died (35.6%) were 16–30 years old.
Table 2. Outcome of the hospital poisoning cases.
Information on the specific pesticide involved was available for 62/121 fatal cases (52.9%) () and the chemical class (OP insecticide) was recorded for two more. The key pesticide responsible for death in this case series was aluminum phosphide (n = 38/62, 61.3%); organophosphorus insecticides alone, and in combination products with pyrethroids, were responsible for 14 and five deaths, respectively.
Table 3. Classification of agents responsible for death among hospital cases.
Forensic science laboratories of Nepal
A total of 2535 pesticide suicide poisoning cases were identified from the two forensic laboratories − 1463 (57.7%) were due to ingestion of OP insecticides and 653 (25.7%) due to exposure to phosphine gas after ingesting aluminum or zinc phosphide. Pyrethroids, carbamate and OP and pyrethroid combinations insecticides were responsible for 95, 83, and 31 deaths respectively. The most important OP identified was dichlorvos (273, 60.6%) followed by unidentified OP insecticides (210, 31.8%) ( and ). Aluminum phosphide was identified in 299/891, 33.5% of cases from CPFSL.
Table 4. Classification of pesticides identified at NFSL.
Discussion
Our study shows that OP insecticides and the fumigant aluminum phosphide are the most important pesticides responsible for pesticide suicide deaths in Nepal, based on the forensic science laboratory data, with support from less comprehensive hospital case data. Other than aluminum phosphide, the key pesticide identified was the OP insecticide dichlorvos, followed by chlorpyrifos, either alone or in a combination product with cypermethrin.
Aluminum and zinc phosphide cause toxicity by liberating phosphine gas after ingestion [Citation17]. Aluminum phosphide is formulated as a dark-gray 3 g-tablet that is widely used in Pakistan, India, Iran, Morocco, and Nepal [Citation18]. It is a common self-poisoning agent with very high case fatality in LMIC where agriculture is a key profession [Citation19,Citation20]. Because no antidote is available for treatment, regulation in its sale is warranted. Experience from India shows that a ban of the 3 g tablet formulation can be associated with a marked reduction in fatal aluminum phosphide deaths [Citation21].
OP insecticides are a common means of self-harm in the LMIC because they are very widely used in agriculture [Citation7]. The common OPs currently used in Nepal include dichlorvos, chlorpyrifos, dimethoate and malathion [Citation9,Citation22–24]. A hospital-based study from five major hospitals across Nepal in 2002 showed that OP compounds were the most common agent for self-poisoning, methyl parathion and dichlorvos being the key pesticides involved [Citation25]. Since that time, methyl parathion has been banned (2006) [Citation26]. Many of the pesticides identified by the forensic science laboratories in our study were OP insecticides (dichlorvos, chlorpyrifos, dimethoate, triazophos, sulfotep, quinalphos, phorate, methyl parathion). However, many were uncommon causes of death and several have been banned. The police toxicology data identified the individual compound for relatively few deaths, but was able to provide important chemical class-based identification of responsible pesticides in a much larger sample of cases compared to NFSL which only took cases from around Kathmandu.
We found that a lot of data were missing from the hospital medical records. Hospital staff seemed to have difficulties or little interest in identifying the compounds responsible for poisoning in patients presenting to hospital. When the poisoning agent was recorded in the notes, the patient or their family had brought the pesticide bottle or package to hospital. When the responsible agent was unknown, an atropine challenge test was sometimes used to determine whether the patient had ingested an OP or carbamate insecticide, but this could not identify the individual compound. For non-OP/carbamate pesticides, the identification was based on the container or history only. If the container was not brought to the hospital and the atropine challenge was negative, the pesticide name and class was not recorded in the medical notes, hindering identification of the responsible agent. Such problems of misdiagnosis of pesticides involved in poisoning has been previously reported from Bangladesh [Citation27].
Hospital staff need to be encouraged to collect precise information on particular pesticide ingested and to be provided with guidelines on the treatment of different pesticide classes. This will improve treatment, save lives, and reduce public health and societal costs by decreasing the burden of poisoning and deaths in Nepal’s society.
The CPFSL sample data did not identify the specific compound in most cases, mainly due to limited human resources and a lack of demand for identification of the exact agent from the police and court system. Encouraging the forensic science laboratories by increasing their resources and providing training could reduce the case overload and help identify the poisoning agent for more cases. This would assist with addressing the public health problem of pesticide poisoning and deaths, and guide regulation of HHPs.
Even though our hospital data showed a 5.3% case fatality, the final outcome was unavailable for around half of the cases (44.6%), suggesting that some fatal cases were not reflected in the case fatality estimate. Many hospitals have a low number of intensive care unit (ICU) beds. If an ICU bed was unavailable for a poisoning patient, the patient would have been transferred to another hospital, meaning that the outcome would not have been recorded in the notes. Since many OP poisoning cases require an ICU bed, the 14% of patients who were transferred would likely have included severe cases, for whom the outcome would have been missed.
There was some difference in the main poisons contributing to deaths noted in hospitals (aluminum phosphide, 69%) and in forensic laboratories (OP 58%, phosphine 26%). One key reason will be that many deaths occur pre-hospital or in small peripheral hospitals due to fast onset of action of the highly hazardous OP insecticides. In addition, the outcome for many hospital patients was not recorded (suggesting that others may have died) and the identity of the compound ingested in the fatal hospital cases was only known for about 50% of cases. So missing data may explain some of the differences. Overall, the forensic toxicology data are likely to be more accurate for identifying the pesticides responsible for most deaths nationally since the laboratories cover all seven provinces and there is analytical proof of the compound involved, in contrast to hospital cases where the record keeping and case identification were not ideal.
It would be valuable to compare the pesticides ingested by patients surviving hospital admission with those identified in fatal cases from the forensic toxicology laboratories to provide insight into the relative toxicity of the pesticides and identify pesticides for which deaths appear to be occurring before admission to tertiary hospitals. For such an analysis, prospectively collected hospital admissions – with careful recording of the pesticide ingested by experienced researchers – would be essential, as done previously in Sri Lanka [Citation28,Citation29]. A future study should collect these hospital data for comparison with forensic toxicology data.
Methyl parathion was previously the most important pesticide for suicide before being banned in 2006 [Citation30,Citation31]. It was reported as being responsible for admission in 95 hospital cases and 5 deaths. However, of 242 cases where the agent was identified by the NFSL, only 3 were due to this OP insecticide suggesting that the ban has been largely successful, despite the porous border with India to the south. Similarly, phorate which was banned in 2015 and was identified in only 1 case, although reported in 7 non-fatal hospital cases. It is not clear whether the history of methyl parathion or phorate ingestion in hospital cases was correct (as no analysis of blood samples was done). Further forensic toxicology studies are required to identify whether cases with these banned pesticides are common. If yes, then better enforcement of the pesticide regulatory regime is necessary to take advantage of HHPs ban in Nepal.
Lethal paraquat poisoning is an important problem in some countries [Citation32–34]; however, we did not find any cases of lethal paraquat poisoning in our study. The use of paraquat by farmers is low in Nepal and is highly regulated, such that it is only used by larger scale commercial farmers.
In our study, there was only one case of occupational poisoning. This suggests that the pesticides now being used in Nepal only rarely cause severe occupational poisoning after the previous HHP bans. Less severe poisoning may be taking place but patients are not presenting to, or being transferred to, major secondary hospitals. They may be staying at home and ignoring less severe symptoms of poisoning.
Easy availability and accessibility of HHPs in Nepal could be the reason for pesticide related deaths and poisonings. Removing access to highly lethal suicide methods means that people use other accessible methods that less commonly kill [Citation1]. Pesticide regulation is one of the key methods to remove easy access and reduce deaths and occupational pesticide illness. Replacing HHPs that are most toxic to humans has significantly reduced deaths without affecting the crop productivity [Citation5,Citation15,Citation35]. The Plant Quarantine and Pesticide Management Centre (PQPMC), a regulatory body of Nepal, plays a major role in regulating the use of HHPs. After the results of this study were presented to the PQPMC in 2019, the Pesticide Registration Board banned eight pesticides in Nepal [Citation26], including dichlorvos. The Pesticide Registration Board also deregistered the high concentration (56%) 3 g tablet of aluminum phosphide soon after. According to the government order, import and production was banned from 4 August 2019. During the following 2 years, stockpiles in the country can be sold to farmers; after the 2-year phase out period, all remaining stockpiles will need to be deposited in a government-built warehouse. It will be important to observe the effects of these bans on agriculture, health and suicides.
Limitations
The hospital-based data frequently had missing information, meaning that a comprehensive picture of pesticide poisoning and outcome at the hospital level was not possible. Misclassification of the agent involved was also possible; identification of the pesticide by history in hospitals was likely to be reasonably accurate but was not recorded in the medical notes for many patients. Due to stigma and fear of the negative consequences of medical-legal cases and police investigation, hospital data likely under-represent the actual numbers of pesticide self-poisoning cases. If the death occurred before reaching hospital, which may be the case with some HHPs, the death may not be reported to the authorities at all with burial arranged by the family. If the patient is discharged from the Emergency Department without admission to hospital, the patient record is given to the patient without copy kept at the hospital. We had planned to visit all hospitals for a last time in April–July 2020 but were unable to do so due to the Covid pandemic. The end of data collection, therefore, varied between hospitals and we did not get three years data from each as planned. The toxicology laboratories were able to identify the individual compounds for some cases; however, this was not comprehensive and compound specific data that allowed the responsible pesticide to be identified was only available for 36.4% of cases.
Conclusion
Organophosphorus insecticides and aluminum phosphide are responsible for most pesticide suicides and severe poisonings in Nepal. There may be opportunities to improve management of poisoned patients if the poison is identified on admission. Encouraging toxicology laboratories to identify the individual pesticide compound can provide data to guide further pesticide regulation and public health, as has been successfully performed recently. Poisoning reporting and recording need to be improved to allow for better poisoning treatment and effective decrease in pesticide poisoning and death cases in Nepal.
Author contributions
Study conception and design: M.E., L.U., and R.G.; support in data collection process: B.C., P.N.P., S.R.B., B.B., K.D.D., N.K.P., M.P.B., R.P., P.P., S.K.S., S.B., R.C., G.B.M., D.R.S., B.B., and M.M.; acquisition and analysis of data: R.G., M.P., and N.R.; drafting first manuscript: R.G., M.E., and L.U. All authors read and approved the final manuscript.
Acknowledgments
The authors thank the directors and medical record department staff of the study hospitals for their support, as well as Mr. Birendra Raj Shakya, acting executive Director of National Forensic Science Laboratory, and Mr. Rakesh Kumar Singh (Senior Superintendent of Police, Central Forensic Science Laboratory) and M. Sudan Kumar Bista for providing data.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- World Health Organization. Preventing suicide: a global imperative. Geneva: World Health Organisation; 2014.
- World Health Organization. Suicide in the world: global health estimates. Geneva: World Health Organization; 2019.
- Dandona R, Bertozzi-Villa A, Kumar GA, et al. Lessons from a decade of suicide surveillance in India: who, why and how? Int J Epidemiol. 2017;46(3):983–993.
- Mew EJ, Padmanathan P, Konradsen F, et al. The global burden of fatal self-poisoning with pesticides 2006–15: systematic review. J Affect Disord. 2017;219:93–104.
- Bonvoisin T, Utyasheva L, Knipe D, et al. Suicide by pesticide poisoning in India: a review of pesticide regulations and their impact on suicide trends. BMC Public Health. 2020;20(1):251.
- World Health Organization and Food and Agriculture Organization of the United Nations. Preventing suicide: a resource for pesticide registrars and regulators. Geneva: World Health Organization; 2019. https://www.who.int/publications/i/item/9789241516389
- Eddleston M. Patterns and problems of deliberate self-poisoning in the developing world. QJM. 2000;93(11):715–731.
- Koirala D. Analytical capability on pesticide analysis in food in Nepal. In 5th National Seminar of the Nepal Academy of Science and Technology. Kathmandu, Nepal; 2008.
- Aryal K, Neupane S, Lohani GR, et al. Health effects of pesticides among vegetable farmers and the adaptation level of integrated pest management program in Nepal. Nepal: Nepal Health Research Council Kathmandu; 2014.
- Central Bureau of Statistics and Government of Nepal. Statistical Pocket Book of Nepal, 2018. Kathmandu, Nepal: National Planning Commission; 2018.
- Hagaman AK, Maharjan U, Kohrt BA. Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. Int J Ment Health Syst. 2016;10(1):46.
- World Health Organization. WHO recommended classification of pesticides by hazard and guidelines to classification 2019 edition. Geneva: World Health Organisation; 2020.
- Dawson AH, Eddleston M, Senarathna L, et al. Acute human lethal toxicity of agricultural pesticides: a prospective cohort study. PLOS Med. 2010;7(10):e1000357.
- Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ. 2004;328(7430):42–44.
- Gunnell D, Knipe D, Chang S-S, et al. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: a systematic review of the international evidence. Lancet Global Health. 2017;5(10):e1026–e1037.
- Bennett L, Dahal D, Govindasamy P. Caste, ethnic and regional identity in Nepal: further analysis of the 2006 Nepal Demographic and Health Survey. Macro International Inc. Maryland, USA: Calverton; 2008.
- World Health Organization, International Programme on Chemical Safety, and S.M. WHO Task Group on Phosphine. Phosphides, Phosphine and selected metal phosphides United Nations Environment Programme and International Labour Organisation, Editors. Geneva: World Health Organization; 1988.
- Ghazi M. Wheat pill (aluminum phosphide) poisoning”: commonly ignored dilemma. A comprehensive clinical review. Prof Med J. 2013;20(6):855–8963.
- Mehrpour O, Jafarzadeh M, Abdollahi M. A systematic review of aluminium phosphide poisoning. Arh Hig Rada Toksikol. 2012;63(1):61–73.
- Siwach SB, Gupta A. The profile of acute poisonings in Harayana-Rohtak Study. J Assoc Physicians India. 1995;43(11):756–759.
- Murali R, Bhalla A, Singh D, et al. Acute pesticide poisoning: 15 years experience of a large North-West Indian hospital. Clin Toxicol. 2009;47(1):35–38.
- Timsinha S, Shah R, Kar S. Sociodemographic characteristics and assessment of severity in organophosphorus poisoning in a tertiary care hospital. Int J Res Med Sci. 2017;5(9):3786–3793.
- Bajracharya M, Khadka P, Wagle L. A retrospective study of poisoning cases in Manmohan Memorial Teaching Hospital. J Manmohan Memorial Inst Health Sci. 2018;4(1):55–65.
- Mishra A. Epidemiological study of medicolegal organophosphorus poisoning in central region of Nepal. J Forensic Res. 2012;3:167.
- Gupta S, Joshi M. Pesticide poisoning cases attending five major hospitals of Nepal. J Nepal Med Assoc. 1970;41(144):447–456.
- Sharma DR. Status of chemical pesticides use and their regulation in Nepal. Nepal: Plant Quarantine and Pesticide Management Centre, Government of Nepal; 2019
- Dewan G. Analysis of recent situation of pesticide poisoning in Bangladesh: is there a proper estimate? Asia Pac J Med Toxicol. 2014;3(2):76–83.
- Buckley NA, Fahim M, Raubenheimer J, et al. Case fatality of agricultural pesticides after self-poisoning in Sri Lanka: a prospective cohort study. Lancet Glob Health. 2021;9:e854–862.
- Weerasinghe M, Pearson M, Konradsen F, et al. Emerging pesticides responsible for suicide in rural Sri Lanka following the 2008–2014 pesticide bans. BMC Public Health. 2020;20(1):780.
- Government of Nepal and Plant Quarantine and Pesticide Management Centre. List of registered pesticides and pesticide consumption data 2076/076; 2019 [cited 2020 December 8]; Available from: http://www.npponepal.gov.np/downloadsdetail/2/2018/39799637/.
- Paudyal BP. Organophosphorus poisoning. J Nepal Med Assoc. 2008;47(172):251–258.
- Myung W, Lee G-H, Won H-L, et al. Paraquat prohibition and change in the suicide rate and methods in South Korea. PLOS One. 2015;10(6):e0128980.
- Knipe DW, Chang S-S, Dawson A, et al. Suicide prevention through means restriction: impact of the 2008–2011 pesticide restrictions on suicide in Sri Lanka. PLoS One. 2017;12(3):e0172893.
- Chang SS, Lu TH, Eddleston M, et al. Factors associated with the decline in suicide by pesticide poisoning in Taiwan: a time trend analysis, 1987–2010. Clin Toxicol. 2012;50(6):471–480.
- Manuweera G, Eddleston M, Egodage S, et al. Do targeted bans of insecticides to prevent deaths from self-poisoning result in reduced agricultural output? Environ Health Perspect. 2008;116(4):492–495.