Abstract
Introduction: The annual number of patients > 65 years old about whom the Dutch Poisons Information Center (DPIC) was consulted has more than doubled in the last decade. We aimed to gain insight in the type and circumstances of exposures reported to the DPIC involving older patients, in order to help prevent future poisonings. Methods: Enquiries to the DPIC involving patients > 65 years old were prospectively included from January 2019 to June 2019. Data were collected on patient characteristics (e.g., age, gender, and living situation) and exposure characteristics (e.g., type and exposure scenario). Results: In the first half of 2019, the DPIC was consulted about 1051 patients > 65 years old. The median age of the patients was 77 years old (range: 66–104 years) and women were over-represented (61%). A total of 1650 different substances were reported, 1213 pharmaceutical exposures (74%) and 437 non-pharmaceutical exposures (26%), mostly household products (n = 162). Most pharmaceutical exposures involved cardiovascular agents (n = 367, 30%), central and peripheral nervous system agents (n = 354, 29%), and analgesics (n = 152, 13%). In 71% of the patients exposed to pharmaceuticals, the drugs were taken unintentionally (n = 471), frequently caused by medication errors made by the patients themselves (n = 357, 76%). Most common scenarios included inadvertently taken/given a double (n = 140, 30%) or more than double (n = 94, 20%) dose or the wrong medication (n = 124, 26%). The most common scenario for unintentional exposure to non-pharmaceuticals was “mistook product for food/drink” (n = 122, 37%). Conclusions: The majority of intoxications in older adults are accidental and often involve medication errors. Unintentional poisoning is often preventable. If patients are cognitively impaired, potentially harmful substances should be kept out of their reach and medication should only be administered under direct supervision. Clear labelling, simplified drug regimens and the use of automatic medication dispensers could reduce the risk of medication errors in older patients.
Introduction
Due to increasing life expectancy the number of older people is increasing worldwide. At a global level in 2019, the percentage of the population aged ≥ 65 years old is approximately 9%, and this percentage is estimated to reach ∼12% in 2030, ∼16% in 2050 and it could reach ∼23% by 2100 [Citation1]. Because of the ageing of the population more people are likely to suffer from multiple long-term illnesses. The higher prevalence of multimorbidity and polypharmacy in older individuals increases the risk for medication errors and adverse drug reactions [Citation2]. In addition to a higher risk of unintentional medication-related harm, older individuals are also a high-risk population with respect to suicidal poisonings due to several factors including mental and neurocognitive disorders, chronic physical illnesses, pain, social isolation, loss of relatives, and loss of autonomy [Citation3–5].
Older patients generally have a higher risk of mortality when exposed to a potential toxic compound, compared to younger patients [Citation6,Citation7]. Although patients ≥ 70 years old represent a relatively small proportion of cases reported to American Poison Control Centers (5%), they contributed to 16% of the poison-related deaths in 2020 [Citation8]. In addition, mean length of stay in the intensive care unit was prolonged in elderly patients, compared to younger patients, also indicating a more serious course of acute poisoning [Citation9].
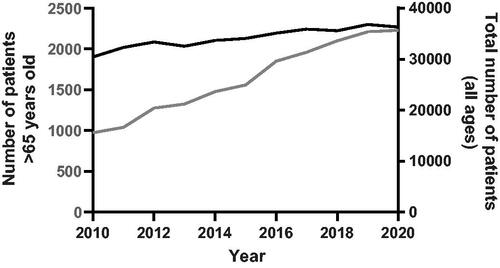
In the Netherlands, the annual number of patients >65 years old about whom the Dutch Poisons Information Center (DPIC) was consulted by telephone disproportionally increased by 129%, from 974 in 2010 to 2230 in 2020. This increase is larger than expected taken into account the rise in the Dutch population aged ≥ 65 years (from ∼2.54 million in 2010 to ∼3.39 million in 2020 [Citation10]) and the overall increase in the number of patients the DPIC was consulted about (19% from 2010 to 2020, regardless of age) ().
Figure 1. Number of patients > 65 years old (grey line) and total number of patients (all ages) (black line) about whom the Dutch Poisons Information Center (DPIC) was consulted by telephone from 2010 to 2020.
The higher risk of major outcomes in elderly poisoned patients and the growing elderly population highlight the importance of implementing poisoning preventing programs targeting older adults. Although the number of poisonings in older people is expected to increase worldwide in line with demographic trends, few studies [Citation11–20] have focused on exposure scenarios of poisoning in older patients. No such data are available yet for the Dutch population. The aim of this study is to gain insight in the number, type, and circumstances of pharmaceutical and non-pharmaceutical exposures reported to the DPIC involving patients > 65 years old in order to identify poisoning prevention strategies to reduce the number of poisonings in older individuals.
Methods
The DPIC provides a 24/7 telephone service providing expert advice to health care professionals on the diagnosis and treatment of poisoned patients, serving the entire Dutch population of 17.6 million. Reports to the DPIC are made on a voluntary basis. In a limited number of cases the DPIC is consulted by members of the public. In these cases, first-aid advice is given and patients are advised to contact their physician for further medical assistance.
Enquiries involving individuals > 65 years old were prospectively included from January 1, 2019 to June 30, 2019. Anonymous case information was recorded using a standard data format to ensure uniform data collection. Standard data fields include patient characteristics (i.e., age and gender), exposure(s), dose, intention (i.e., intentional/unintentional), and the DPIC’s advice (i.e., observation at home, evaluation by a physician, or observation in hospital). For the purpose of the study, additional information regarding the living situation (e.g., living at home or in a nursing home), the presence of comorbidities, and exposure scenario was recorded by the Specialists in Poison Information. During DPIC consultation, data were collected anonymously, i.e., no personal identifiable information was recorded (only age and gender were known). The study is fully GDPR compliant. No explicit consent from the patients was required, because there was no direct contact by researchers with patients during the study and data were collected anonymously.
From the exposure scenario that was explicitly asked during DPIC consultation, the investigators categorized the intentional and unintentional exposures. Cases were discussed in case of discrepancies in order to reach consensus. Unintentional pharmaceutical exposures were categorized as: “too high dose prescribed”, “incorrect dose or product dispensed”, “inadvertently taken or given wrong medication”, “inadvertently taken or given double dose”, “inadvertently taken or given more than double dose”, “medication doses taken or given too close together”, “incorrect dosing route”, “adverse effect/drug interaction” and “taken too high dose because of persistent pain”. Patients with exposure to both medication and another substance were included in the group of patients with pharmaceutical exposures.
Unintentional non-pharmaceutical exposures were categorized by exposure route. Scenarios for unintentional non-pharmaceutical exposure via oral route included: “mistook product for food or drink”, “took non-food item for no apparent reason”, “mistook product for medication” and “other”. Scenarios for unintentional non-pharmaceutical exposure via inhalation included: “occurred while a product was being used”, “mixed two products together” and “other”. Unintentional non-pharmaceutical exposures via ocular route were categorized as: “spray/splash to eye”, “mistook product for eye drop”, “eye exposure via hand contact” and “other”, and via dermal route as: “spray/splash to skin” and “other”. Intentional non-pharmaceutical exposures were categorized as: “(suspected) self-harm or cry for attention”, “use of alcohol”, “use of drugs of abuse (excl. abuse of pharmaceuticals)” and “other”. Pharmaceutical and non-pharmaceutical exposures were subdivided in categories based on the DPIC classification system.
In some cases, the DPIC is contacted more than once about a specific exposure. When we were contacted within a 24 h timespan about a patient with exactly the same age, gender, exposure(s), exposure route and exposure scenario, then the call was classified as a follow-up call. Multiple enquiries regarding the same patient and same exposure(s) were analyzed as a single case. Descriptive statistics (percentage, median, interquartile range [IQR] and full ranges) were used to provide an overview of patient characteristics (e.g., age, gender, comorbidities and living situation) and exposure characteristics (e.g., type of exposures and exposure scenarios). Analyses were conducted using IBM SPSS Statistics version 26.0.0.1 (IBM SPSS, Armonk, NY).
Results
DPIC enquiries
The DPIC received a total of 1045 enquiries regarding 1051 patients > 65 years old from January through June 2019. Six enquiries involved two individuals who were simultaneously exposed and, therefore, separately included. We were mostly consulted by general practitioners (67%), followed by geriatric physicians (9%), paramedics (7%), Emergency Departments (6%), pharmacists (3%), psychiatrists (3%), hospital physicians (2%), and members of the public (1%).
Patient characteristics
The median age of the patients was 77 years old (range 66–104) and women were over-represented (n = 642, 61%) (, stratified by intentionality). Almost two in three patients (n = 660, 63%) lived independently or with care at home, while a smaller part lived in a nursing home (n = 177, 17%) or psychiatric institution (n = 22, 2%). One or more comorbidities were present in at least 64% of the patients (n = 670) (unknown in 286 patients). Almost half of the patients with an underlying illness had a cardiovascular condition (n = 327). Psychiatric disorders were more prevalent in patients with intentional exposures compared to patients with unintentional exposures (50 vs. 7%, respectively), whereas cognitive impairment was more often reported in patients with unintentional exposures compared to patients with intentional exposures (30 vs. 4%, respectively). Demographics of patients exposed to pharmaceuticals and non-pharmaceuticals are shown in .
Table 1. Patient characteristics stratified by intentionality.
Exposure characteristics
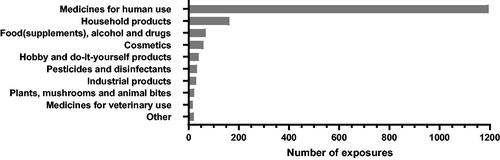
In total, 1051 individuals were exposed to 1650 different substances (range: exposure to 1–18 substances per patient occurring in one poisoning episode). Patients were exposed to a single substance in 79% of the cases (n = 826) and to multiple substances in 21% of the cases (n = 225). In 77% of the patients (n = 805), the exposure was unintentional, in 18% intentional (n = 193) and in 5% the intention was unknown (n = 53) (). 73% of all exposures involved a pharmaceutical (n = 1213 exposures), i.e., drugs for human (n = 1196) or veterinary (n = 17) use. 10% of exposures were household products (n = 162) and 4% involved food (supplements), alcohol and drugs of abuse (n = 69) ().
Figure 2. Number of exposures per product category in patients > 65 years old reported to the Dutch Poisons Information Center (DPIC) from January 2019 to June 2019.
Pharmaceutical exposures
Most pharmaceutical exposures (n = 1213) involved cardiovascular agents (n = 367, 30%), central and peripheral nervous system agents (n = 354, 29%), analgesics (n = 152, 13%) and hormonal and metabolic pathway drugs (n = 92, 8%). In most patients, route of exposure to pharmaceuticals was oral (n = 605, 92%), followed by ocular (n = 32, 5%) and parenteral (n = 21, 3%) route.
In 71% of the patients exposed to medication, the drugs were taken unintentionally (n = 471) (). Drugs often involved were: metoprolol (n = 35 exposures), paracetamol (n = 34), metformin (n = 24), acetylsalicylic acid (n = 22), levodopa (combined with benserazide or carbidopa or carbidopa and entacapone) (n = 20), pantoprazole (n = 19), digoxin (n = 17), clopidogrel (n = 17) and rivaroxaban (n = 16) (see also ). Of the unintentional pharmaceutical exposures, the most common scenarios included: “inadvertent double-dosing” (n = 140, 30%) or “more than double-dosing” (n = 94, 20%) and “inadvertently taken/given the wrong medication” (n = 124, 26%) (). The majority of unintentional pharmaceutical exposures was caused by the patients themselves (n = 357, 76%). Almost three out of four of these patients were living at home (n = 261) and in at least 15% of these cases (n = 40) cognitive impairment was involved (underlying illnesses unknown in 43 cases). A smaller number of unintentional pharmaceutical exposures were caused by mistakes made by nurses (n = 65, 14%), pharmacists (n = 11, 2%), family members (n = 8, 2%), and physicians (n = 7, 1%). The greater part of the patients unintentionally exposed to medication lived independently or with care at home (n = 302, 64%), while a smaller proportion lived in a nursing home (n = 82, 17%). Medication errors made by nurses working in nursing homes (n = 40) most often involved inadvertent administration of medication of another resident (n = 19, 48%) or double dosing (n = 13, 33%). The median age of the patients unintentionally exposed to medication was 79 years old (IQR: 72-85; range: 66–100). The majority of the patients who were unintentionally exposed to medication were advised to be observed at home or in nursing home (n = 308, 65%), whereas in 24% of the cases (n = 114) evaluation by an physician and in 10% of the cases (n = 49) hospital observation was advised.
Table 2. Scenarios for pharmaceutical exposures in patients > 65 years old.
Table 3. Unintentional and intentional pharmaceutical exposures in patients > 65 years old.
In 23% of the patients exposed to medication, the drugs were taken intentionally (n = 152) (). In intentional drug overdose, most commonly involved medication was: oxazepam (n = 32 exposures), paracetamol (n = 30), oxycodone (n = 15), lorazepam (n = 12), temazepam (n = 11), zolpidem (n = 9), quetiapine (n = 9) and citalopram (n = 7) (see also ). The median age of the patients intentionally exposed to medication was 73 years old (IQR: 69–79; range: 66–94). The majority of the patients who were intentionally exposed to medication were advised to be evaluated by a physician (n = 43, 28%) or to be observed in hospital (n = 54, 36%), whereas (from a pure toxicological point of view) in 36% (n = 55) observation at home or in nursing home was advised.
Non-pharmaceutical exposures
Non-pharmaceutical exposures in older adults are shown in . Most of the non-pharmaceutical exposures were unintentional (n = 334, 85%) (), mainly occurring via oral route (n = 246, 74%). Household products (40%, n = 140 exposures) were mainly involved in accidental exposures, mostly cleaning products (n = 80), dishwasher detergents (n = 23) and laundry detergents (n = 9). Other accidental exposures often reported included cosmetics (16%, n = 54), mostly dental care products (n = 30), i.e., denture cleaning tablets (n = 26) or mouthwash (n = 4), followed by hobby and do-it-yourself products (11%, n = 38), and pesticides (4%, n = 14) and disinfectants (4%, n = 14).
Table 4. Scenarios for non-pharmaceutical exposures in patients >65 years old.
The most common scenario for unintentional non-pharmaceutical exposure was “mistook product for food or drink” (). The ingestion of a descaling agent that was still present in a coffee machine or kettle was often reported (n = 27). Another common scenario was “for no apparent reason eating or drinking substances stored within their reach” (n = 78). These cases often involved patients with cognitive impairment (n = 65, 83%), and exposures often reported included: plants (n = 13), shower gel/shampoo/soap (n = 8), dishwasher tablets (n = 7), cigarettes (including butts and ash) (n = 7), and denture cleaning tablets (n = 5). The median age of the patients unintentionally exposed to non-pharmaceuticals was 76 years old (IQR: 71–84; range: 66–104). The majority of the patients was advised to be observed at home or in nursing home (n = 239, 72%), whereas in 25% of the cases (n = 83) evaluation by a physician and in 4% of the cases (n = 12) hospital observation was advised.
A small part of the non-pharmaceutical exposures was intentional (n = 41, 10%), mostly in the context of (suspected) self-harm or cry for attention (n = 23) (). Route of exposure was often oral (n = 35, e.g., ingestion of chlorine bleach (n = 5)), followed by inhalation (n = 4, e.g., inhalation of natural gas or helium). The median age of the patients intentionally exposed to non-pharmaceuticals was 76 years old (IQR: 70–81; range: 66–94). The majority of the patients was advised to be evaluated by a physician (44%) (n = 18) or to be observed in hospital (24%) (n = 10), whereas (from a pure toxicological point of view) in 32% (n = 13) observation at home or in nursing home was advised.
Discussion
The majority of DPIC consultations regarding older patients involve unintentional pharmaceutical exposures. Most common scenarios were inadvertently taken or given a double or more than double dose or the wrong medication, mostly caused by the patients themselves due to forgetfulness or during a state of confusion. American Poison Center data showed similar results, i.e., the most common scenarios for medication errors in older patients were: inadvertently took or given medication twice, wrong medication taken or given, other incorrect dose, medication doses given or taken too close together and inadvertently took or given someone else’s medication [Citation14]. Fortunately, each of these five scenarios resulted in low rates of serious outcomes (<1%) [Citation14]. A Danish Poison Center study showed that in nursing homes most poisonings were caused by administration errors [Citation15]. We showed that approximately half of the medication errors made by nurses working in nursing homes involved inadvertent administration of medication of another resident.
Polypharmacy and complicated drug regimens in older people increases the risk of medication errors and adverse drug reactions [Citation21,Citation22]. A strategy to reduce this type of poisonings is prescribing medication with a wider therapeutic window and using simplified drugs regimens and electronic prescription systems. Furthermore, clear medication instructions by pharmacists and the use of daily or weekly medication dispensers or automatic medication dispensers (automatically releasing the correct dose of the medication at a specified time) will improve medication adherence. Especially, drugs with a narrow therapeutic window, such as digoxin [Citation23] and lithium [Citation24], should be prescribed and monitored carefully. If patients are severely cognitively impaired, medications should be kept out of their reach and only administered under direct supervision. Confusion between medication may be caused by similar appearances of the medications or poor eyesight. Clear labelling of medication and using larger font size may prevent these mistakes [Citation25,Citation26]. Administration errors occurring in nursing homes could be prevented by independent double-checking, especially when high-risk medication is involved.
In our study, cardiovascular, central and peripheral nervous system drugs, hormonal/metabolic pathway agents, and analgesics were most often involved in unintentional pharmaceutical exposures, corresponding with medication commonly used in patients of older age. An American study among patients ≥ 65 years old also showed that most common medication categories associated with preventable adverse drug events include cardiovascular drugs, followed by diuretics, non-opioid analgesics, hypoglycemics, anticoagulants and opioids [Citation27]. An Australian Poison Center study showed that medication errors in patients ≥ 75 years old particularly involved cardiovascular drugs, anticoagulants, antidiabetics, opioids, and paracetamol-containing analgesics [Citation28]. The DPIC does not routinely conduct follow-up to investigate the medical outcome. However, other studies have shown that especially certain medication classes, such as analgesics (e.g., opioids), anticoagulants (e.g., warfarin), asthma therapies (e.g., beta-agonists), psychotherapeutics (e.g., lithium) and some cardiovascular agents (e.g., cardiac glycoside) were associated with high hazard factors in older patients following unintentional exposure [Citation12,Citation14,Citation29].
In our study, 18% of the poisonings were intentional. Cobaugh et al. showed that paracetamol, aspirin, barbiturates, cardiovascular drugs, cyclic antidepressants, and opioids had the greatest risk for harm and lethality in older patients with respect to suicide-related exposures [Citation30]. If suicide is secondary to an underlying psychiatric illness which is not diagnosed or inadequately treated, then these type of poisonings could be preventable [Citation25]. Depression in older patients is often undetected or inadequately treated [Citation31,Citation32]. Therefore, diagnosis and treatment of psychiatric conditions should be optimized in older persons [Citation3,Citation25]. Additional prevention strategies may include prescribing of less toxic medication, and limiting the amount of medication dispensed when an older person is (suspected to be) suicidal [Citation6]. In addition, caregivers should be advised to reduce the availability of dangerous medication and other chemicals at home [Citation25,Citation26,Citation30].
In our study, approximately a quarter of exposures in older patients involve non-pharmaceutical substances, mostly household products and cosmetics. The most common scenario for unintentional non-pharmaceutical exposure was “mistook product for food or drink”, e.g., caused by transfer of substances from the original packaging to a container that would normally contain food or drink. Other common scenarios for non-pharmaceutical exposures involved patients with cognitive impairment who, for no apparent reason, ingested a non-food item stored within their reach, such as plants, dishwasher tablets, cigarettes and cosmetics (e.g., denture cleaning tablets and soap). A French Poison Center study also showed that older adults residing in structured living facilities, with a history of dementia and/or cognitive impairment, are at risk of non-pharmaceutical poisoning, e.g., by ingesting personal hygiene products (e.g., soap) and plants [Citation13]. An Australian Poison Center study showed that hand sanitizers, soap and denture cleaning agents were commonly involved in accidental ingestions in patients with dementia [Citation20]. Most of the accidental non-pharmaceutical exposures seem preventable. Edible products should be stored separated from non-edible products and chemicals should be kept in their original container and should not be transferred to food containers. Moreover, to avoid mistakes, better labelling of products and using clear warning statements and user instructions on products is advised.
The last decade, the number of enquiries to the DPIC involving older adults steadily increased. Although our data cannot identify an underlying cause of this trend, possible explanations could be increased use of medications, or longer waiting lists for home care or admission to nursing homes, which subsequently increases the risk of accidents occurring at home.
There are several limitations to Poison Center data that may bias our results. First, data are based on voluntary reports to the DPIC, which underestimates the true incidence of poisonings in the Netherlands. Moreover, it is expected that especially exposures that require the expertise of a Poison Control Center may be reported, which may lead to an underreporting of cases with minor outcomes that do not require medical attention. In addition, as the DPIC only receives a limited number of calls from members of the public, data are likely to be biased toward more severe poisonings. Furthermore, it is expected that there is underreporting of common poisonings that clinicians have experience with regarding treatment (e.g., paracetamol or benzodiazepines) and cases in which the patient has died and there is no need to consult a Poison Center about clinical management. Therefore, Poison Center data may not reflect the true patterns of poisoning in older adults. On the other hand, using data from Poison Centers enables characterization of poisoning exposures managed at home (or nursing home) or in a health care facility. The DPIC does not routinely follow-up all cases, therefore no outcome data could be reported. In addition, some cases could have been double-counted due to anonymous processing of cases. The study period involved a 6-month period and, therefore, variation in call types associated with seasonal changes could not be evaluated.
Conclusions
Older people are a high-risk group, because of the high prevalence of comorbidities and polypharmacy, and potential cognitive dysfunction. Poisoning prevention strategies need to be tailored to target individuals residing at home and in aged care facilities. In our study, the majority of intoxications in older adults involved medication errors. Most common scenarios were inadvertently taken or given a (more than) double dose or the wrong medication. Simplified drug regimens and the use of innovative technologies, such as automatic medication dispensers could reduce these type of medication errors. In addition, if patients are cognitively impaired, potentially harmful substances should be kept out of their reach and medication should only be administered under direct supervision. Furthermore, manufacturers of pharmaceuticals and consumer products should be encouraged to design labels which can be easily read and understood by older people to avoid mistakes. A multidisciplinary approach involving instruction and monitoring by general practitioners, geriatric physicians, pharmacists, nursing home staff, and home care providers may prevent future poisonings in older individuals.
Supplemental Material
Download MS Word (24.6 KB)Acknowledgments
The authors would like to thank Agnes van Velzen for her assistance in data extraction from the DPIC database.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- United Nations. Department of economic and social affairs, population division (2019). World population prospects. Highlights (ST/ESA/SER.A/423). New York (NY): United Nations; 2019.
- Medication safety in polypharmacy. Geneva, Switzerland: World Health Organization; 2019. (WHO/UHC/SDS/2019.11).
- Conejero I, Olie E, Courtet P, et al. Suicide in older adults: current perspectives. Clin Interv Aging. 2018;13:691–699.
- Hawton K, Harriss L. Deliberate self-harm in people aged 60 years and over: characteristics and outcome of a 20-year cohort. Int J Geriatr Psychiatry. 2006;21(6):572–581.
- Troya MI, Babatunde O, Polidano K, et al. Self-harm in older adults: systematic review. Br J Psychiatry. 2019;214(4):186–200.
- Doak MW, Nixon AC, Lupton DJ, et al. Self-poisoning in older adults: patterns of drug ingestion and clinical outcomes. Age Ageing. 2009;38(4):407–411.
- Rogers JJ, Heard K. Does age matter? Comparing case fatality rates for selected poisonings reported to US poison centers. Clin Toxicol. 2007;45(6):705–708.
- Gummin DD, Mowry JB, Beuhler MC, et al. 2020 Annual report of the American association of poison control centers’ national poison data system (NPDS): 38th annual report. Clin Toxicol (Phila). 2021;59(12):1282–1501.
- Muhlberg W, Becher K, Heppner HJ, et al. Acute poisoning in old and very old patients: a longitudinal retrospective study of 5883 patients in a toxicological intensive care unit. Z Gerontol Geriatr. 2005;38(3):182–189.
- Statistics Netherlands (CBS) [Internet]. Den Haag: Centraal Bureau voor de Statistiek (CBS). [accessed 2022 March 17]. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37296ned/table?ts=1643635230395
- Cassidy N, Lee SK, Donegan CF, et al. Poisoning in older adults: the experience of the national poisons information Centre. Ir Med J. 2008;101(9):268–270.
- Crouch BI, Caravati EM, Mitchell A, et al. Poisoning in older adults: a 5-year experience of US poison control centers. Ann Pharmacother. 2004;38(12):2005–2011.
- Deguigne M, Cellier M, Hamon Y, et al. Poisoning exposure from non-pharmaceutical products in residents of structured living facilities. Clin Toxicol. 2022;60(3):371–378.
- Hayes BD, Klein-Schwartz W, Gonzales LF. Causes of therapeutic errors in older adults: evaluation of national poison center data. J Am Geriatr Soc. 2009;57(4):653–658.
- Jakobsen HN, Vermehren C, Andersen JT, et al. Drug poisoning in nursing homes: a retrospective study of data from the danish poison information centre. Drugs Ther Perspect. 2021;37(7):328–337.
- Karbakhsh M, Zandi NS. Pattern of poisoning in the elderly: an experience from Tehran. Clin Toxicol (Phila). 2008;46(3):211–217.
- Klein-Schwartz W, Oderda GM, Booze L. Poisoning in the elderly. J Am Geriatr Soc. 1983;31(4):195–199.
- Kroner BA, Scott RB, Waring ER, et al. Poisoning in the elderly: characterization of exposures reported to a poison control center. J Am Geriatr Soc. 1993;41(8):842–846.
- Willis S, Slattery A, King W, et al. Therapeutic error calls among older adults reported to a regional poison control center in Alabama. South Med J. 2016;109(6):356–362.
- Wojt IR, Cairns R, Tan ECK. Poisoning exposures in people with dementia (2014–2019): a retrospective study. J Am Med Dir Assoc. 2021;22(7):1553–1557.
- Davies EA, O'Mahony MS. Adverse drug reactions in special populations - the elderly. Br J Clin Pharmacol. 2015;80(4):796–807.
- Rausch C, Laflamme L, Bültmann U, et al. Number of medications and adverse drug events by unintentional poisoning among older adults in consideration of inappropriate drug use: a Swedish population-based matched case-control study. Eur J Clin Pharmacol. 2017;73(6):743–749.
- Currie GM, Wheat JM, Kiat H. Pharmacokinetic considerations for digoxin in older people. Open Cardiovasc Med J. 2011;5:130–135.
- Tueth MJ, Murphy TK, Evans DL. Special considerations: use of lithium in children, adolescents, and elderly populations. J Clin Psychiatry. 1998;59(6):66–73.
- Haselberger MB, Kroner BA. Drug poisoning in older patients: preventative and management strategies. Drugs Aging. 1995;7(4):292–297.
- Klein-Schwartz W, Oderda GM. Poisoning in the elderly. Epidemiological, clinical and management considerations. Drugs Aging. 1991;1(1):67–89.
- Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107–1116.
- Huynh A, Cairns R, Brown JA, et al. Patterns of poisoning exposure at different ages: the 2015 annual report of the Australian poisons information centres. Med J Aust. 2018;209(2):74–79.
- Cobaugh DJ, Krenzelok EP. Adverse drug reactions and therapeutic errors in older adults: a hazard factor analysis of poison center data. Am J Health Syst Pharm. 2006;63(22):2228–2234.
- Cobaugh DJ, Miller MJ, Pham TT, et al. Risk of major morbidity and death in older adults with suicidal intent: a cross-sectional analysis from the national poison data system, 2000–2009. J Am Geriatr Soc. 2015;63(3):501–507.
- Bottino CM, Barcelos-Ferreira R, Ribeiz SR. Treatment of depression in older adults. Curr Psychiatry Rep. 2012;14(4):289–297.
- Kok RM, Reynolds CF. 3rd. Management of depression in older adults: a review. JAMA. 2017;317(20):2114–2122.
