Abstract
Aim
To differentiate the severity of acute opioid toxicity and describe both the clinical and physiological features associated with heroin overdose in a cohort of witnessed overdose cases.
Methods
Witnessed heroin overdose cases over a 12-month period (30 June 2018 – 30 June 2019) at the Medically Supervised Injecting Room (MSIR) in Melbourne, Australia were examined. The severity of acute opioid toxicity was classified according to the level of clinical intervention required to manage the overdose cases where an escalating level of care was provided. Heroin overdose cases were classified into one of three graded severity categories and a fourth complicated heroin overdose category.
Results
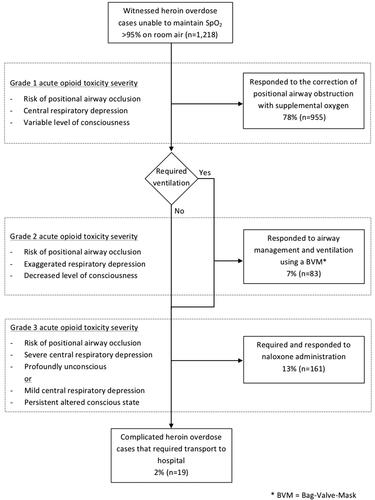
A total of 1218 heroin overdose cases were identified from 60,693 supervised injecting visits over the study period. On the spectrum of toxicity, 78% (n = 955) of overdose cases were classified as Grade 1 severity, 7% (n = 83) as Grade 2 severity, and 13% (n = 161) as Grade 3 acute opioid toxicity severity cases, as well as 2% (n = 19) classified as complicated heroin overdose cases. The median onset time for heroin overdose cases was 17 min (IQR 11–28 min) from the time the individual was ready to prepare and inject heroin until clinical intervention was initiated.
Conclusion
We demonstrated that heroin overdose is a dynamic illness and cases differ in the severity of acute opioid toxicity. The risk of airway occlusion including positional asphyxia was an early and consistent feature across all levels of toxicity, while exaggerated respiratory depression together with exaggerated depression of consciousness was increasingly observed with greater levels of toxicity. We also demonstrated the importance of early intervention in overdose cases, where in a large cohort of heroin overdose cases there were no fatal outcomes, a very low hospitalisation rate and most cases were able to be managed to clinical resolution on-site.
Introduction
Adverse outcomes associated with opioid drugs are a major public health concern and a leading cause of drug-related deaths in Australia and internationally [Citation1–5]. A major issue associated with opioids, including heroin, is acute overdose. Indeed, adverse outcomes associated with heroin use are disproportionately higher compared with the general age-matched population, including an estimated six-time greater risk of premature death with heroin use, with overdose the leading cause [Citation6–9]. A key clinical feature associated with overdose, and more specifically acute opioid toxicity, is respiratory compromise that occurs through a number of contributory mechanisms and which if left untreated, may lead to severe brain injury or death [Citation10]. In fact even in clinical settings, the intravenous administration of opioid drugs has been demonstrated to produce profound ventilatory impairment, a significant reduction in oxygen saturation and apnoea shortly after administration and these studies have been fundamental to our understanding of the acute opioid toxicity effects even at relatively low levels of toxicity [Citation11–14].
Opioid-Induced Ventilatory Impairment (OIVI) consists of three main clinical features: decreased central respiratory drive; depression of supraglottic muscle tone that may lead to upper airway obstruction; and decreased consciousness [Citation15]. In addition to the acute opioid toxicity effects directly associated with OIVI, rapid physiological deterioration in overdose events may also be exacerbated by patient comorbidities, the concomitant use of other opioid drugs or CNS depressants, pulmonary aspiration, or positional asphyxia [Citation16,Citation17]. The extent of acute opioid toxicity associated with OIVI is however difficult to determine in most overdose cases. This is because OIVI is most accurately identified through the measurement of the arterial partial pressure of carbon dioxide, however it is not feasible to measure this routinely in most clinical settings, and particularly not in locations where most heroin overdose cases occur [Citation12,Citation15,Citation18,Citation19]. In routine clinical practice, surrogate measures of opioid-related respiratory and ventilatory impairment, such as the level of sedation, oxygen saturation, and respiratory rate are instead commonly used as part of the overall clinical picture to identify and manage opioid toxicity events.
There is a paucity of information relating to the direct toxicological effects that occur in heroin overdose cases at the time of the overdose event, including the typical clinical and physiological features associated with more severe levels of acute opioid toxicity. A key reason for this is that the majority of heroin overdose cases occur in the community rather than in a clinical setting that enables the identification, assessment, and monitoring of acute opioid toxicity at the time that an overdose occurs. The differentiation and description of opioid toxicity features associated with heroin overdose events are important because it provides evidence to inform public health and harm reduction strategies in order to reduce the frequency and severity of adverse outcomes resulting from heroin overdose. In this study, we aimed to differentiate the severity of acute opioid toxicity and describe both the clinical and physiological features associated with heroin overdose events in a cohort of witnessed overdose cases.
Methods
We retrospectively examined a cohort of heroin overdose cases that occurred over a 12-month period between 30 June 2018 and 30 June 2019 at the Medically Supervised Injecting Room (MSIR) at North Richmond Community Health in Melbourne, Australia. Only witnessed overdose cases associated with a supervised injecting visit that occurred onsite in the MSIR where the client stated that they were injecting heroin were included in this study. Overdose cases involving street-level heroin that may have been adulterated or completely substituted with other drugs including fentanyl were also included. Overdose cases where the client stated that they were not injecting heroin, but rather injecting methadone or other prescription opioids, were excluded from this study.
Setting
The MSIR is an anonymous harm reduction service that provides a medically supervised setting for people who inject drugs, with a range of health and social support services available onsite. To be eligible to register to access the MSIR, individuals must be at least 18 years of age, not pregnant, have no bail or parole conditions that prohibit attendance at the MSIR, and have a history of injecting drug use. Pregnancy, serious intoxication, and/or severe mental or physical ill health upon presentation precluded access to the service. On arrival clients are required to disclose the pre-obtained drugs they intend to inject and their substance use history for the preceding 24 h. Following assessment by staff, clients are given access to the Injecting Zone where other staff members provide clients with their preferred sterile injecting equipment. Once seated in a booth, clients prepare and self-administer their pre-obtained drugs while being regularly monitored by staff who are also located in this space. Staff also provide individualised harm reduction advice and complete a thorough clinical assessment if an adverse clinical event occurs. When safe to do so, clients progress to the Aftercare Zone for post-injection monitoring and support, where they can also access other health and social support services. Any medical issues, including overdose, are assessed and managed by clinical staff onsite.
Heroin overdose cases
An overdose event was included in this study in cases where following the self-administration of heroin, an individual presented in an altered conscious state with respiratory depression and was unable to maintain oxygen saturation (SpO2) of greater than 95% on room air despite encouragement to breathe. Heroin overdose cases were managed in accordance with standard practice protocols. Clinical interventions were provided in an escalating manner to provide basic supportive care including airway management and ventilatory support, as well naloxone administration where clinically indicated. All clients that experienced an overdose were assessed clinically, including an assessment of conscious state, respiratory rate, and SpO2 on room air. Clients that presented with decreased consciousness and low SpO2 were prompted to breathe and any obvious positional airway occlusion corrected. Respiratory rate was physically assessed by staff as part of the initial clinical assessment, including for clients with a low respiratory rate. Clients that required ventilatory support were provided positive pressure ventilation using a Bag-valve-mask (BVM). Clients that required naloxone administration were treated with an initial dose of 400 mcg via intramuscular injection (IMI). Naloxone administration was titrated to effect with subsequent doses of 400 − 800 mcg administered in five-minute intervals as required, to a maximum dose of 2 mg as part of the standard management protocol. Clinical escalation to a medical supervisor occurs for anything outside of the standard overdose management protocol, including for consultation regarding atypical presentations, complications and before transport of a client to hospital.
Differentiating the severity of acute opioid toxicity
For this study, we incorporated a severity scale to differentiate overdose cases based on the severity of acute opioid toxicity consistent with OIVI. Heroin-related OIVI in the overdose cases was unable to be accurately assessed because capnography was not measured. Instead, we differentiated the level of toxicity based on the escalating level of basic supportive care, or the level of clinical intervention required to manage the overdose cases in order to assess the direct opioid-related effects on decreased central respiratory drive, impaired ventilation, and decreased consciousness.
The standard protocol for the management of overdoses included, in order:
Airway management, including the correction of positional asphyxia and insertion of a nasopharyngeal or oropharyngeal airway adjunct if required.
Supplemental oxygen if SpO2 less than 95% on room air.
Positive pressure ventilation using a BVM if not breathing, or hypoxic despite airway management and supplemental oxygen.
Naloxone administration of 400 mcg via IMI if not conscious or breathing adequately after 5 min.
Subsequent doses of naloxone at 400–800 mcg via IMI at 5-min intervals if needed, titrated to a maximum dose of 2 mg.
An emergency ambulance called for transport to hospital if the client is still not breathing after 2 mg naloxone, due to difficulty managing the airway, there are significant medical complications, such as seizures, or if ongoing monitoring of the client is required at the closing time of the service.
After differentiating cases into a severity category, the physiological findings on initial clinical assessment for the overdose cases were reported using standard clinical measures, including an assessment of conscious state (using the AVPU scale), respiratory rate, and SpO2. Heroin overdose cases were classified into one of the following categories of severity:
Grade 1 severity: Overdose cases that responded to supplemental oxygen administration together with the correction of obvious positional airway obstruction if present, and external stimulation including prompts to breathe;
Grade 2 severity: Overdose cases that responded to airway management and positive pressure ventilation using a BVM, together with supplemental oxygen;
Grade 3 severity: Overdose cases that were refractive to more conservative clinical interventions but that adequately responded to treatment with naloxone (400 mcg initial dose, titrated to effect up to 2 mg) in addition to the above interventions;
Complicated heroin overdose cases: Overdose cases where a significant medical complication was identified (including tonic-clonic seizure activity or obvious pulmonary aspiration) or where there was inadequate response to naloxone administration and transport to hospital by emergency ambulance was required.
Onset time for heroin overdose cases
All clients are registered in the MSIR client data management system when presenting to the service. Their movements through the different areas of the service as well as the time of an overdose are recorded and electronically time-stamped. We determined the onset time for the overdose cases in this study from the time a client was progressed through to the Injecting Zone by staff, until the time that an overdose event occurred that required clinical intervention. This period included the time taken by the client to both prepare and subsequently inject the heroin. This timeframe was used as a real-world indication of onset time for heroin overdose events where an individual is already in possession of heroin and the required injecting equipment with the intention of self-administering the drug.
Statistical analysis
Descriptive statistics were used to describe the number and classification of overdose cases, overdose onset time and demographic details of individuals who experienced an overdose. Medians and interquartile range (IQR) presented as upper and lower quartiles were used for comparison due to non-normally distributed data. The Kruskal–Wallis test for one-way ANOVA was used to compare the overdose onset time between the different toxicity groups, with statistical significance considered at p < 0.05. All graphs, descriptive statistics and analysis were conducted using SPSS for Mac version 28 (IBM SPSS Inc., Armonk, NY).
Results
Over the 12-month study period, there were 60,693 supervised injecting visits at the MSIR that involved the self-reported administration of heroin. This included 49,934 supervised injecting visits involving heroin alone and a further 10,517 injecting visits involving the co-administration of heroin with one or more other drugs. From the 60,693 supervised heroin injecting visits, there were a total of 1218 overdose cases (occurring among 473 individuals), equating to an overdose rate of 2% for this study period. The median age of the overdose cohort was 41 years (IQR 35–48 years, range 20 − 66 years) and the majority were male (n = 401, 85%). Almost half (58%, n = 274) had a single overdose event, with 42% (n = 199) having multiple overdose events. The median number of multiple overdose events for an individual during the study period was 3 (IQR 2–5 events, range 2 − 35). There were 193 overdose cases (16%) that involved the self-reported co-administration of heroin and diphenhydramine, nine overdose cases that involved the co-administration of heroin and another drug (including benzodiazepines, other opioids, and methamfetamine) as well as four cases where three or more drugs including heroin were injected concomitantly. The number of heroin overdose cases in each severity category is presented in , with the typical physiological findings associated with the different levels of toxicity summarised in .
Table 1. Typical physiological findings associated with the different severity categories of acute opioid toxicity.
Grade 1 acute opioid toxicity severity
On the spectrum of acute opioid toxicity, 78% (n = 955) of all heroin overdose cases in this study were classified as Grade 1 severity cases. Ventilatory impairment from the combined effects of central respiratory depression and airway occlusion was apparent in this group, with a median respiratory rate of four breaths per minute (IQR 4–6 breaths) and a median SpO2 of 78% (IQR 69–85%) on initial clinical assessment. Cases in this group presented with varying levels of decreased consciousness, including 58% (n = 555) that responded to voice, 17% (n = 163) that responded to a painful stimulus, and 8% (n = 72) of cases that were profoundly unconscious and unresponsive to any external stimuli.
Grade 2 acute opioid toxicity severity
Despite initial clinical intervention to manage obvious airway occlusion and the provision of supplemental oxygen, an additional 7% (n = 83) of heroin overdose cases adequately responded to positive pressure ventilation using a BVM. Clinically, these cases presented with exaggerated opioid toxicity-related effects on the depression of consciousness and depression of central respiratory drive compared to the Grade 1 severity group. Cases in the Grade 2 severity group presented with a median respiratory rate of one breath per minute (IQR 0–4 breaths) and a median SpO2 of 62% (IQR 47–78%) on initial clinical assessment. Furthermore, 46% of cases (n = 38) in this group were entirely apnoeic on initial assessment. Marked depression of consciousness was also typical in this group, with 66% of cases (n = 55) unresponsive to external stimuli and profoundly unconscious, and a further 14% of cases (n = 12) that only responded to a painful stimulus.
Grade 3 acute opioid toxicity severity
There were 161 cases (13%) that did not adequately respond to more conservative clinical interventions. Instead, these cases were treated with and also adequately responded to naloxone administration by staff. These cases were therefore classified as grade 3 severity cases where there were two distinct subgroups: Grade 3a – severe acute respiratory depression cases (55%, n = 89); and Grade 3b – persistent altered conscious state cases (45%, n = 72).
Grade 3a – Severe acute respiratory depression cases
From a clinical perspective, cases in this subgroup presented with further exaggerated opioid toxicity-related depression of central respiratory drive and depression of consciousness compared to both the Grade 1 and 2 acute opioid toxicity severity groups. Clinically, all of the cases in this subgroup did not adequately respond to more conservative clinical interventions including positive pressure ventilation using a BVM in addition to the correction of obvious airway occlusion and supplemental oxygen administration. Cases in the Grade 3a severe acute respiratory depression subgroup had a median respiratory rate of zero breaths per minute (IQR 0–2 breaths) as well as a median SpO2 of 53% (IQR 40–72%) on initial clinical assessment. Furthermore, 62% of cases (n = 55) were entirely apnoeic on initial clinical assessment. Cases also typically presented as profoundly unconscious, with 93% (n = 83) unresponsive to any stimulus on initial clinical assessment.
Grade 3b – Persistent altered conscious state cases
Cases in this subgroup presented with a variable level of depressed consciousness or in an altered conscious state that persisted over an extended period of time and failed to adequately respond to the correction of any obvious positional airway occlusion and supplemental oxygen administration. Cases in this subgroup presented with varying levels of decreased consciousness, including 25% (n = 18) that responded to voice, 35% (n = 25) that responded to a painful stimulus, and 35% (n = 25) that were profoundly unconscious and unresponsive to any external stimuli. Opioid toxicity-related depression of central respiratory drive in this subgroup was also similar to the Grade 1 toxicity group with a median respiratory rate of four breaths per minute (IQR 2–6 breaths) and a median SpO2 of 78% (IQR 70–87%) on initial clinical assessment.
Complicated heroin overdose cases
There were a further 2% (n = 19) of cases where transport to hospital by emergency ambulance was required and they were classified as complicated heroin overdoses cases. Three of these cases involved significant tonic-clonic seizure activity. There were also five cases transported to hospital that involved complex multidrug toxicity presentations. A further 11 cases were transported to hospital that involved a decreased level of consciousness that persisted for between 2 and 6 h in duration and did not respond to standard clinical interventions. This included five cases that were transported to hospital for ongoing monitoring due to closure of the service and two cases involving the inadequate response to naloxone dosing at the maximum or in excess of the maximum standard dosing regimens with 2 and 3.2 mg of naloxone administered through IMI in these cases, respectively. The remaining four cases were transported to hospital following consultation with the medical supervisor due to atypical clinical presentations.
The onset of heroin overdose events
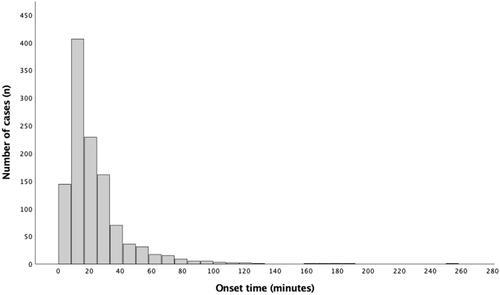
Examination of the onset time for heroin overdose cases in this study revealed that most overdose events occurred in a relatively short time period after an individual was ready to prepare and inject heroin (). Specifically, we found that the median overdose onset time for all cases in this study was 17 min (IQR 11–28 min, range 1 − 258 min), where 22% (n = 263) of overdoses occurred within 10 min, and 15 cases where in which clinical intervention within 2 min. Comparison of the overdose onset time revealed some variance between the different opioid toxicity categories. We found that the Grade 1 acute opioid toxicity severity group had a median onset time of 18 min (IQR 11–29 min) and the Grade 2 acute opioid toxicity severity group had a median onset time of 11 min (IQR 8–18 min). For the two Grade 3 acute opioid toxicity severity sub-groups, the Grade 3a severe acute respiratory depression cases had a median onset time of 14 min (IQR 9–25 min), and the Grade 3b persistent altered consciousness cases a median onset time of 23 min (IQR 15–39 min).
Disposition
For the 1218 heroin overdose cases managed at the MSIR during the study period, there were no known fatal outcomes for any of the individuals. The majority of cases (98%, n = 1199) were managed to clinical resolution on-site, with only the 19 complicated heroin overdose cases transported to hospital for a higher level of clinical care.
Discussion
Our study demonstrates that heroin overdose is a dynamic illness, where rapid physiological deterioration can occur due to ventilatory impairment through a number of mechanisms associated with acute opioid toxicity. By examining a large cohort of witnessed overdose cases, we demonstrated that many individuals were severely hypoxic or apnoeic on initial presentation, and if left untreated may have resulted in adverse outcomes including hypoxic brain injury, respiratory failure, and death. Our study shows the importance of supervised injecting facilities and the ability to provide early intervention in response to overdose, which can dramatically reduce hospitalisation and mortality rates among people who inject drugs. Non-fatal heroin overdose is a common occurrence for people who use heroin, and previous studies in this region have reported fatal outcomes in approximately 3–6% of heroin overdose cases that occurred in the community [Citation20,Citation21]. In our study, there were more than 1200 heroin overdose cases that occurred with no fatal outcomes due to early intervention. Likewise, only 2% of heroin overdose cases in our study required a higher level of care and were transported to hospital. This is in contrast to previous research in this region, which reported 37% of community-based heroin overdose cases treated by paramedics that required transport to hospital [Citation21].
In this study, we also demonstrated that heroin overdose cases differ in the severity of acute opioid toxicity. Our results demonstrate exaggerated effects of central respiratory depression and depression of consciousness with higher levels of toxicity. Another key finding of our study was the risk and impact of airway occlusion in heroin overdose cases, including the inability to autocorrect positional asphyxia as an early and consistent feature across all levels of toxicity. This finding is consistent with a recent study indicating that positional asphyxia may contribute to greater than one-third of all opioid overdose-related deaths in the community [Citation22]. In our study, the impact of airway occlusion as a clinical feature in heroin overdose cases was particularly highlighted in Grade 1 acute opioid toxicity severity cases. Findings showed rapid physiological deterioration and life-threatening hypoxia in many cases due to ventilatory impairment, despite underlying retained central respiratory drive, and where complete clinical resolution of these cases was achieved without the requirement for ventilation or naloxone. These results are important because a comprehensive understanding of the direct toxicological effects of acute opioid toxicity at the time of a heroin overdose is fundamental to implementing evidence-based clinical and public health interventions. Results from our study highlight that early intervention in heroin overdose cases is critical for reducing adverse outcomes in overdose cases, where timely intervention and the correction of airway occlusion, ventilation, and/or naloxone administration may be required.
We also observed atypical clinical presentation for overdose cases in our study, including the persistent altered conscious state group of cases. All of the cases in this group had a presentation consistent with opioid toxicity and where the overdose was reversed following naloxone administration, however, they all presented with an exaggerated and persistent depression of consciousness. Clinically, the presentation of these cases is consistent with the concomitant use of opioids and a central nervous depressant drug including benzodiazepines and alcohol, but this was unable to be confirmed with toxicological analysis in this study. The adulteration or complete substitution of heroin purchased in the local street-based market with other drugs, such as synthetic benzodiazepines or synthetic opioids including fentanyl, may also result in variation to the clinical presentation of overdose cases presented in this study. In Australia, heroin adulterated with fentanyl is uncommon and there have been few reports of fentanyl involvement in fatal heroin overdose cases in this region [Citation23–25]. Fentanyl is a major concern in some regions and overdose cases involving fentanyl or fentanyl analogues may present with a shorter onset time and more rapid physiological deterioration, though more recent reports demonstrate no change in the required naloxone dosing regime to manage these cases [Citation26–33]. More research is required in this area to better understand multiple drug toxicity presentations as well as the complicated heroin overdose cases identified in this study.
There are several clinical and public health implications identified from our study. Based on our findings, the three key components for harm reduction that were identified to reduce adverse outcomes associated with heroin overdose cases were:
That most heroin overdose events occur soon after someone is ready to prepare and inject heroin, with a median onset time in this study of 17 min;
That in overdose cases, correcting airway occlusion (particularly from positional asphyxia) and oxygen administration if available should be considered early and before naloxone administration; and
That heroin overdose is a dynamic illness where early intervention is required because a person can deteriorate rapidly due to ventilatory impairment through a number of mechanisms.
From a public health perspective, the importance of early intervention in heroin overdose cases as well as the importance of correcting obvious positional airway occlusion whether naloxone is available or not, should be incorporated into community overdose education and training programmes. In our study, these interventions were provided at a supervised injecting facility where we demonstrated a reduction in overdose-related adverse outcomes in a population identified to be particularly at risk of harms related to injecting drug use [Citation34]. Furthermore, this service was also able to provide a gateway to other clinical and social support services for this population, including opioid agonist treatment [Citation35].
Limitations
A limitation of this study relates to the onset time for overdose events, where both the preparation and injecting time were included in the onset time which is subject to individual variability. Furthermore, late-onset overdose events may be associated with cases in which a client had multiple injecting episodes in the same visit, and where an overdose event did not occur following the first heroin administration. We were unable to differentiate heroin overdose cases resulting from multiple heroin administration episodes in the same visit which is an additional limitation of this study. Although overdose cases in this study were diagnosed based on the clinical presentation consistent with heroin and opioid toxicity, an additional limitation of this study was the inability to definitively determine the drugs or combination of drugs involved in the overdose cases because toxicological analysis was outside the scope of this study. Further research is required in this area to determine the impact of street-level heroin that is adulterated with or completely substituted for other opioid drugs, as well as the impact of specific combined drug toxicity cases.
Conclusion
In this study, we demonstrated that heroin overdose is a dynamic illness where rapid physiological deterioration can occur due to ventilatory impairment through a number of mechanisms associated with acute opioid toxicity. We demonstrated that heroin overdose cases differ in the severity of acute opioid toxicity. The risk of airway occlusion including positional asphyxia was an early and consistent feature in heroin overdose cases, while exaggerated respiratory depression together with exaggerated depression of consciousness were increasingly observed with greater levels of opioid toxicity. In this study, we demonstrated the importance of early intervention in overdose cases, where in a large cohort of heroin overdose cases managed at a supervised injecting facility there were no fatal outcomes, a very low hospitalisation rate and with most cases able to be managed on-site to clinical resolution.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70.
- Degenhardt L, Day C, Dietze P, et al. Effects of a sustained heroin shortage in three Australian states. Addiction. 2005;100(7):908–920.
- Roxburgh A, Hall WD, Dobbins T, et al. Trends in heroin and pharmaceutical opioid overdose deaths in Australia. Drug Alcohol Depend. 2017;179:291–298.
- Scholl L, Seth P, Kariisa M, et al. Drug and opioid-involved overdose deaths - United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–1427.
- Wilson N, Kariisa M, Seth P, et al. Drug and opioid-involved overdose deaths - United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):290–297.
- Gossop M, Stewart D, Treacy S, et al. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97(1):39–47.
- Darke S, Mills KL, Ross J, et al. Rates and correlates of mortality amongst heroin users: findings from the Australian treatment outcome study (ATOS), 2001-2009. Drug Alcohol Depend. 2011;115(3):190–195.
- Stam NC, Gerostamoulos D, Dietze PM, et al. The attribution of a death to heroin: a model to help improve the consistent and transparent classification and reporting of heroin-related deaths. Forensic Sci Int. 2017;281:18–28.
- Degenhardt L, Bucello C, Mathers B, et al. Mortality among regular or dependent users of heroin and other opioids: a systematic review and Meta-analysis of cohort studies. Addiction. 2011;106(1):32–51.
- Overdyk F, Dahan A, Roozekrans M, et al. Opioid-induced respiratory depression in the acute care setting: a compendium of case reports. Pain Manag. 2014;4(4):317–325.
- Strang J. Death matters: understanding heroin/opiate overdose risk and testing potential to prevent deaths. Addiction. 2015;110(2):27–35.
- Jolley CJ, Bell J, Rafferty GF, et al. Understanding heroin overdose: a study of the acute respiratory depressant effects of injected pharmaceutical heroin. PLoS One. 2015;10(10):e0140995.
- Dursteler-Mac Farland KM, Stormer R, Seifritz E, et al. Opioid-associated effects on oxygen saturation. Addiction. 2000;95(2):285–287.
- Stoermer R, Drewe J, Dursteler-Mac Farland KM, et al. Safety of injectable opioid maintenance treatment for heroin dependence. Biol Psychiatry. 2003;54(8):854–861.
- Macintyre PE, Loadsman JA, Scott DA. Opioids, ventilation and acute pain management. Anaesth Intensive Care. 2011;39(4):545–558.
- White JM, Irvine RJ. Mechanisms of fatal opioid overdose. Addiction. 1999;94(7):961–972.
- Warner-Smith M, Darke S, Lynskey M, et al. Heroin overdose: causes and consequences. Addiction. 2001;96(8):1113–1125.
- Bowen J, Levy N, Macintyre P. Opioid-induced ventilatory impairment: current ‘track and trigger’ tools need to be updated. Anaesthesia. 2020;75(12):1574–1578.
- Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Statement on principles for identifying and preventing opioid-induced ventilatory impairment (OIVI) in the acute pain setting. Victoria, Australia: Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine; 2018.
- Darke S, Mattick RP, Degenhardt L. The ratio of non-fatal to fatal heroin overdose. Addiction. 2003;98(8):1169–1171.
- Stam NC, Pilgrim JL, Drummer OH, et al. Catch and release: evaluating the safety of non-fatal heroin overdose management in the out-of-hospital environment. Clin Toxicol. 2018;56(11):1135–1142.
- deJong JL, Lee J, Grande A, et al. Positional asphyxia in Opioid-Related deaths: is it being overlooked? J Forensic Sci. 2020;65(6):2008–2012.
- Rodda LN, Pilgrim JL, Di Rago M, et al. A cluster of Fentanyl-Laced heroin deaths in 2015 in Melbourne, Australia. J Anal Toxicol. 2017;41(4):318–324.
- Lam T, Barratt MJ, Bartlett M, et al. Infrequent detection of unintentional fentanyl use via urinalysis among people who regularly inject opioids in Sydney and Melbourne, Australia. Addiction. 2022;117(8):2331–2337.
- Stam NC, Gerostamoulos D, Gerstner-Stevens J, et al. Determining the effective dose of street-level heroin: a new way to consider fluctuations in heroin purity, mass and potential contribution to overdose. Forensic Sci Int. 2018;290:219–226.
- Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N Engl J Med. 2017;376(7):605–607.
- Fairbairn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017;46:172–179.
- Schumann H, Erickson T, Thompson TM, et al. Fentanyl epidemic in Chicago, Illinois and surrounding cook county. Clin Toxicol (Phila). 2008;46(6):501–506.
- Sutter ME, Gerona RR, Davis MT, et al. Fatal fentanyl: one pill can kill. Acad Emerg Med. 2017;24(1):106–113.
- Krotulski AJ, Chapman BP, Marks SJ, et al. Sentanyl: a comparison of blood fentanyl concentrations and naloxone dosing after non-fatal overdose. Clin Toxicol (Phila). 2022;60(2):197–204.
- Strang J, McDonald R, Campbell G, et al. Take-Home naloxone for the emergency interim management of opioid overdose: the public health application of an emergency medicine. Drugs. 2019;79(13):1395–1418.
- Bell A, Bennett AS, Jones TS, et al. Amount of naloxone used to reverse opioid overdoses outside of medical practice in a city with increasing illicitly manufactured fentanyl in illicit drug supply. Subst Abus. 2019;40(1):52–55.
- Carpenter J, Murray BP, Atti S, et al. Naloxone dosing after opioid overdose in the era of illicitly manufactured fentanyl. J Med Toxicol. 2020;16(1):41–48.
- Van Den Boom W, Del Mar Quiroga M, Fetene DM, et al. The Melbourne safe injecting room attracted people most in need of its service. Am J Prev Med. 2021;61(2):217–224.
- Weeks A, Cogger S, Clark N. Initial experience with subcutaneous depot buprenorphine in a medically supervised injecting facility. Drug Alcohol Rev. 2021;40(7):1354–1355.