Abstract
Objective: This study aimed to identify dyslipidaemia in human immunodeficiency virus (HIV)-infected children. This was part of a larger study aiming at the treatment of dyslipidaemia in this population.
Design: A cross-sectional quantitative study design was used.
Setting: The Paediatric Outpatient Department HIV Clinic at Dr George Mukhari Academic Hospital (Garankuwa, Pretoria).
Subjects: Children who received antiretroviral treatment (ART) for at least six months and were virologically supressed.
Outcome measures: Fasting lipograms were evaluated against American paediatric thresholds for dyslipidaemia (NCEP ATPIII guidelines), and z-scores for weight-for-age (WAZ) and height-for-age (HAZ) were interpreted.
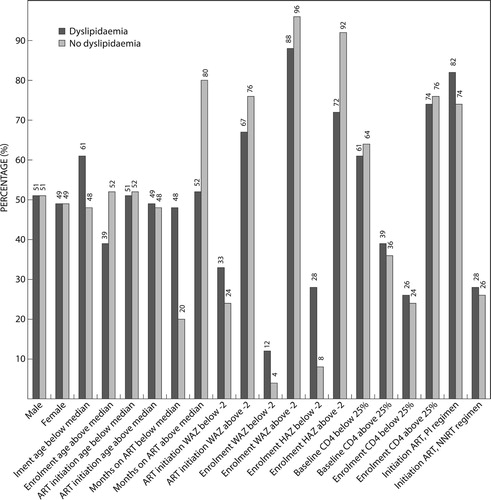
Results: In total, 140 children were enrolled, median age at enrolment was 64.5 months (interquartile range IQR 42.5–94.6) and 51% were female. Median period of ART use was 34.0 months (IQR 23.2–52.8). Median ART commencement age was 18 months (IQR 8.1–34.0). Lipid profile results were available in 108 of the 140 children. Total cholesterol was classified borderline in 33% and elevated in 11% of the children. LDL cholesterol was borderline in 24% and elevated in 7%. HDL cholesterol was borderline in 20% and low in 30%. Triglyceride levels were borderline in 29% and elevated in 39% of the children. Children were considered as having dyslipidaemia if one or more of the four lipid profile levels were abnormal, or if at least two were borderline. By these criteria, 75% of the group were dyslipidaemic. A significant negative correlation was found between dyslipidaemia and enrolment HAZ indicating stunting (r-value −0.31; p < 0.05), also between dyslipidaemia and months’ duration on ART (r-value −0.25; p < 0.05) and a significant positive correlation was found between initiation on protease inhibitor (PI)-based regimen and dyslipidemia (p < 0.05).
Conclusion: The prevalence of dyslipidaemia in HIV-infected children receiving ART is high. Participants who were stunted, or had a shorter ART duration, and those initiated on a PI-based regimen were more likely to have dyslipidaemia.
Introduction
Human immunodeficiency virus (HIV) infection as well as the effect of its treatment with anti-retroviral therapy (ART) can negatively influence children’s physical development and growth.Citation1–3 The efficacy and benefits of ART have been proven to be life-changing, by turning HIV from a fatal prognosis into a manageable chronic condition. Unfortunately, with the benefits of longer survival come many serious metabolic side effects. Children have a higher risk of developing toxicity and possible side effects from ART due to their longer exposure.
HIV infection remains a serious public health problem, despite immense progress in the fields of its prevention and treatment. The total number of persons living with HIV in South Africa was an estimated 7.06 million by July 2017. Therefore, an estimated 12.6% of the total population is HIV-positive.Citation4
Known side effects associated with ART use in children and adults include dyslipidaemia, fat redistribution, glucose metabolism disorders, lactic acidosis, renal dysfunction and osteopenia.Citation5–8 Since many HIV-infected children are also malnourished,Citation9 especially in developing countries such as South Africa, side effects may be exacerbated by their poor nutritional status. Poor nutritional status may also alter the pharmacokinetics of ART.Citation9 Ramteke et al. (2017)Citation3 reported that HIV-infected children on ART are more often stunted than underweight. Stunting is associated with chronic malnutrition and reflects being too short for one’s age, as determined specifically by the height-for-age z-score (HAZ) being below −2 standard deviations, according to the 2006 World Health Organization (WHO) Child Growth StandardsCitation10 for children younger than five years of age, and the 2007 WHO Growth Reference dataCitation11 for those 5–19 years of age.
This study aimed to investigate the prevalence of dyslipidaemia in HIV-infected children who have been on ART for at least six months attending an outpatient clinic in Garankuwa, Pretoria. Dyslipidaemia associated with HIV and ART has been well described Citation5,Citation7,Citation8,Citation12–14 in low- and middle-income countries. Dyslipidaemia in both children and adults increases the risk for developing cardiovascular disease.Citation15 Therefore, it is recommended by the South African Antiretroviral GuidelinesCitation16 that all children should have lipid testing done before initiating ART and then yearly thereafter.
Recent international studies reported that the prevalence of dyslipidaemia in HIV-infected children on ART is in the order of 38% in IndiaCitation12 and 27% in Tanzania.Citation17 In El-Salvador in South America 48% of this population had hypertriglyceridemia and 14.5% had hypercholesterolemia.Citation18 Nampijja et al. (2017)Citation19 investigated the prevalence of dyslipidaemia in HIV-infected children aged 1–17 years in Uganda and found the overall prevalence of dyslipidaemia to be 74%. Of those with dyslipidaemia, 56% had low HDL-C, 22% had elevated triglycerides, 16% had elevated LDL-C, and 11% elevated total cholesterol levels. These researchers also reported that children who started with ART while acutely ill or at WHO clinical staging 3 or 4 had a greater incidence of dyslipidaemia.Citation19 However, HIV-infected children who are not on ART also show a high prevalence of dyslipidaemia as indicated by 40% prevalence found in a group of Indian children.Citation20 As other authors have noted, it is difficult to differentiate between the effect of the HIV itself and the effect of the ART when it comes to the causality of the dyslipidaemia in this population.Citation21,Citation22
ARTs are given as combination therapy, usually as a mix of three medications. They can be broadly categorised into three main groups, called protease inhibitors (PIs), nucleoside reverse transcriptase inhibitors (NRTIs) and non-nucleoside reverse transcriptase inhibitors (NNRTIs). The South African National Department of Health, the National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults (2015)Citation16 requires all infants and children (aged 1 month to 3 years, or weight less than 10 kg) to receive a first-line combination regimen of abacavir, lamivudine and lopinavir/ritonavir (ABC + 3TC + LPV/r). Children aged 3 to 15 years with a weight of more than 10 kg receive abacavir, lamivudine and efavirenz (ABC + 3TC + EFV). If the first-line regimen fails, patients are placed on a second-line regimen, which consists of a combination of zidovudine, lamivudine and lopinavir/ritonavir (AZT + 3TC + LPV/r).
Brazilian research conducted by Paganella et al. (2017) found that children on a PI-containing regimen had a four times greater chance of presenting with elevated TG levels when compared with those not on ART. Their data also showed that those children with viral loads of < 400 copies/ml had a lower risk of developing abnormal total cholesterol levels.Citation22
There is limited information regarding the prevalence of dyslipidaemia in South African HIV-infected children on ART. The topic has been investigated by a group of researchers in JohannesburgCitation8,Citation14 and in Cape Town.Citation7 Innes et al. (2016) found elevated total cholesterol levels in 10%, with abnormal LDL-C, HDL-C and TG in 13%, 12% and 9% respectively, in pre-pubertal South African children.Citation7
Strehlau et al. (2012)Citation14 found elevated total cholesterol in 16%, elevated LDL in 12%, elevated TG in 36%, and lowered HDL in 40% of children treated with a PI-based regimen. They also observed that lipid profiles improved with ART initiation (therefore confirming that the HIV infection itself contributes to the development of dyslipidaemia), and the switching of regimens from a PI-based to NNRTI-based regimen improved the lipid profiles even more. It was also confirmed by Arpadi et al. (2013)Citation8 that lipid profile alterations as well as lipodystrophy occurs more frequently in young children who receive PI-based rather than NNRTI-based regimens.
The current study adds to the body of knowledge regarding the prevalence of dyslipidaemia among South African children who are HIV infected. The objective of the study was to identify dyslipidaemia in children who have received ART for at least six months at an outpatient clinic in Garankuwa, Pretoria.
Methods
A cross-sectional study with a quantitative approach was conducted at the paediatric HIV outpatient clinic of Dr George Mukhari Academic Hospital, which is situated next to Sefako Makgatho Health Sciences University in the north of Pretoria. All HIV-infected children who had received ART for at least six months and were actively attending the paediatric HIV clinic from June 2016 to April 2018 were considered for inclusion, and non-probability convenience sampling was used.
Exclusion criteria included poor viral suppression indicated by a high viral load of > 400 RNA copies/ml (caused by drug resistance or poor adherence to ART), and those who were already on lipid-lowering agents or have another illness predisposing them to dyslipidaemia (e.g. diabetes mellitus, chronic renal/liver disease or hypothyroidism). Those patients no longer attending the hospital outpatient clinic (who were referred to other local clinics) were also excluded.
This study formed part of a larger study, which is aimed at testing treatment interventions for dyslipidaemic HIV-infected children. It was intended to enrol 302 children into the larger study. This was based on sample size calculation using 80% power, 5% level of significance and prevalence of 27%.Citation17
Patient records were accessed on the clinic’s electronic database with the help of the person responsible for entering all patient data into the database. This screening for eligibility was done by the researchers. Caregivers of the eligible children were contacted telephonically to explain the purpose of the study and were requested to bring the children in for fasting lipogram. Those who could not be reached telephonically were contacted during their monthly visit to the HIV clinic. An early-morning appointment was then arranged to obtain a fasting lipogram and anthropometric measurements, to be able to investigate the presence of dyslipidaemia and identify factors associated with its occurrence. It was attempted to coordinate the appointment to coincide with the child’s monthly clinic visit, but in cases where that date was not feasible another date was booked and transport money was provided to enable the caregiver to travel to the clinic with the child. The booking of appointments was arranged by the researchers from June 2016 to April 2018, mostly on Tuesdays when the children were attending the HIV clinic.
During the appointment, one of the researchers first explained the whole procedure of the research project in a private room. Written informed consent was obtained (as well as assent in cases where the child was older than seven years). The caregiver of the child was always present during all procedures. The anthropometric measurements were then taken by the researchers who are registered dietitians. All measurements were taken in a standardised manner according to the research protocol using standardised anthropometric techniques as described by Lee and NiemanCitation23 and recorded on a data-collection sheet. Standing height was measured using a portable stadiometer, with the participant standing barefoot and with the head in the Frankfort horizontal plane, and recorded to the nearest 0.1 centimetre. There were no cases where the measurement of recumbent length was necessary. Weight was measured with the participants wearing only light clothing and recorded to the nearest 0.1 kg. Data regarding viral load, CD4 counts and ART regimen were collected from patient records. Date of birth and ART initiation date were confirmed in the patient records and documented on the data-collection sheet. Confidentiality was ensured on the data-collection sheets by documenting only the participants’ unique study number.
After the anthropometric measurements were completed, a venous blood sample of 2–3 ml was collected by a paediatric registrar. All the blood samples for that specific day were then taken by one of the researchers to the Chemical Pathology Department of Sefako Makgatho University, and analysed by the National Health Laboratory Service (NHLS) located in the same department. Analysed data were entered into an Excel spreadsheet (Microsoft Corp, Redmond, WA, USA) using the participant’s unique study number. Hard copies of the blood results were stored in a file together with all the data-collection sheets and completed written informed consent forms, secured in one of the researchers’ office. Caregivers of the participants were informed by telephone of the lipogram results. Those who were diagnosed with dyslipidaemia were invited to take part in a different leg of this research study related to the treatment of dyslipidaemia, which is not reported in this article.
An Excel spreadsheet was created to store all gathered data electronically. Participants’ height and weight were entered into the statistical program Epi Info™ version 7.2.2.2, to calculate the z-scores or standard deviations of the height-for-age (HAZ), and the weight-for-age (WAZ). Epi Info™ is a trademark of the Centers for Disease Control and Prevention (CDC, Atlanta, GA, USA). The 2006 WHO Child Growth StandardsCitation10 were used for children younger than 5 years of age, and the 2007 WHO Growth Reference dataCitation11 were used for those 5–19 years old.
Statistical analysis
Descriptive statistics were used to determine the minimum, maximum, mean and standard deviation, or median and interquartile ranges (where appropriate) and percentage for ages, blood values and anthropometric measures. Inferential statistics were used to investigate possible correlations between anthropometric values and lipogram results, and a p-value of < 0.05 was considered to be statistically significant. Median and interquartile ranges were used to report results that were not normally distributed. Spearman’s rank correlation was used to assess correlation between participants’ characteristics and their cholesterol and triglyceride levels. The association between dyslipidaemia and participants’ characteristics was assessed by utilising the chi-square test. The statistical software IBM SPSS® version 24 (IBM Corp, Armonk, NY, USA) was used.
American lipid reference values () were used in the absence of South African reference values. Other South African researchersCitation8,Citation14 have also used the same reference values, which makes our study outcomes comparable. Participants were considered as having dyslipidaemia if one or more of the four lipid profile levels was elevated (decreased in case of HDL) or at least two were borderline.
Table 1: Lipid reference values used to classify lipogram results
Ethical considerations
Ethical clearance was obtained from Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC), certificate number SMUREC/M/35/2016:IR.
Participation in this study was entirely voluntary and those selected could refuse to participate or stop at any time without stating any reason. All information obtained during this study was kept strictly confidential as described earlier. A participant information sheet was provided to the caregiver of each participant, including the contact details of the researchers, and they were encouraged to contact the researchers when they had queries. No incentives were given to the participants. Caregivers were assured that their decision to participate or not would not affect their current or future treatment at the hospital or clinic.
Support was given to the participants and caregivers by providing transport money if they had to come in on a different day from their usual scheduled monthly appointment, and the dietitians spent time giving individual nutritional advice where needed (the advice does not, however, form part of this study’s outcomes). The participants were treated with extreme care and dignity.
Funding for this study was provided by the Medical Research Council (MRC) of South Africa. None of the researchers declared any conflict of interest.
Results
In total, 140 HIV-infected children on ART were enrolled for this study. The targeted sample was 302 children as explained in the Methods section, but upon starting the investigation the researchers discovered there were only 275 patients actively visiting the clinic at that stage. The number of participants who could be reached telephonically, and who were eligible and willing to participate, totalled 140. The median age at enrolment was 64.5 months (IQR 42.5–94.6), and 71 (51%) of them were female. The characteristics of the children who participated in the study are reported in .
Table 2: Characteristics of children participating in study (n = 140)
As seen in , the most commonly used ART regimen used in this population was 1A3L, a first-line PI-based regimen consisting of abacavir (ABC), lamivudine (3TC), lopinavir/ritonavir (Aluvia or Kaletra). 1A3L is the first line regimen as prescribed by the South African Antiretroviral Treatment Guidelines for Children.Citation16 The regimen 1A3E (ABC, 3TC and efavirenz) was used by 11% of the children and 4% used 2Z3L (the second-line regimen consisting of zidovudine, lamivudine and lopinavir). The remaining 8% received a variety of other regimens.
Lipid profile results were obtained in 108 of the 140 participants. Reasons for the remaining 32 missing lipid profiles include faulty laboratory results (problems with the specimen), and participants not being fasting at the time of appointment. According to the criteria described in , 81 (75%) of the 108 participants were dyslipidaemic. The most frequently occurring abnormality was elevated TG found in 42 (38.9%) of the participants, followed by decreased HDL-C found in 34 (31.5%) of the participants. These lipid profile distributions are reported in .
Table 3: Lipid profile distribution
A significant negative correlation was found between total cholesterol and enrolment HAZ when using Spearman’s rank correlation test (r-value −0.31; p < 0.05); also between total cholesterol and months on ART (r-value −0.25; p < 0.05). The chi-square test revealed that participants who had received ART for less than 34 months (the median ART duration in this group) had a higher prevalence of dyslipidaemia than those who received ART for longer than 34 months.
A significant positive association was found between dyslipidaemia and initiation with a PI-based ART regimen compared with initiation with an NNRTI-based regimen (chi-square test, p < 0.05). These and other associations are demonstrated in and .
Table 4: Characteristics of enrolled children by their lipid profiles
Discussion
In the current study it was aimed to identify dyslipidaemia among HIV-infected children who have received ART for at least six months at an outpatient clinic in Garankuwa, Pretoria. The researchers were interested in finding correlations between the occurrence of dyslipidaemia and other characteristics. The findings indicate a high prevalence of dyslipidaemia (75%) in this study group, which supports the findings of previous South African researchCitation7,Citation8,Citation14 where the same lipid reference levels were used, as well as international studies.Citation12,Citation19,Citation22
The current study found that children who were stunted at the time of lipid testing were more likely to have dyslipidaemia. This supports the findings of Ramteke et al. (2017)Citation3 Stunting is associated with chronic malnutrition or systemic dysfunction during child development.Citation25 Stunting was found to be an independent predictor of HIV disease progression and viral replication in previous South African research.Citation1 HIV-infected children tend to grow below the healthy standards set for age and gender.Citation2,Citation26 It seems that growth in terms of height warrants further investigation in this population. It was observed by the researchers during the current study, while investigating historical data, that height was not well documented in patient records. This indicates that stunting could be overlooked because height is not measured and plotted routinely, whereas body weight is recorded and plotted routinely. The implication of stunted children being overlooked includes a missed opportunity to rectify chronic malnutrition in terms of macro-and micronutrients. The cause of stunted growth is mostly the vicious cycle between infection and malnutrition, especially in developing countries.Citation25 Stunted children have been shown to retain their shorter stature into adulthood and stunting can also contribute to lower lean body mass and even lower cognitive development.Citation25 Stunting has long-term effects on health and disease, as explained by the ‘Developmental Origins of Health and Disease’ hypothesis.Citation26 Stunted children are predisposed to developing metabolic syndrome and the related cardiovascular risks later in life.Citation27,Citation28
Yotebieng et al. (2015)Citation2 have constructed age- and gender-specific weight-gain norms for children who are HIV infected and on ARTs, since it has become clear that HIV-infected children grow differently from healthy children.Citation1,Citation29,Citation30 A recent study done in 2017 by Scholtz and KrugerCitation31 (unpublished Master’s dissertation), performed on the same population in the same setting, used these newly developed weight-gain normsCitation2 to investigate the growth pattern of the HIV-infected children at specific time frames after ART initiation. Their results indicated that weight improvements take place earlier than height improvements, which confirms the need to investigate monitoring of height in this population.
An unexpected finding from this current study was the negative correlation between dyslipidaemia and months on ART. The researchers expected to find a higher occurrence of dyslipidaemia with a longer ART period. This finding supports the fact that the HIV infection itself also contributes to the development of dyslipidaemia and disorders of lipid metabolism as evidenced by previous HIV-related research.Citation20–22 This study did not investigate causality of the dyslipidaemia; therefore firm conclusions cannot be made in this regard.
The majority of the participants were receiving a PI-based regimen at ART initiation (77% of the group). As demonstrated by previous studies,Citation8,Citation14,Citation22 the current study also found a significant positive association between dyslipidaemia and initiation with a PI-based ART regimen. The current South African ART GuidelinesCitation16 prescribe a PI-based first-line regimen, the reason for this being beyond the scope of this article. These same guidelines also recommend investigating HIV-infected children’s lipid values before ART initiation and yearly thereafter. It was observed by the current researchers, however, that this recommendation is not routinely practised in this clinic and high-risk children may be overlooked. The implications of overlooking dyslipidaemia can be quite serious, putting those affected at increased risk for cardiovascular disease.Citation15
Limitations of this study include that it was a single-centre study with a cross-sectional design and with a relatively small sample. This centre does, however, serve a wide community in Garankuwa, as it is situated at a tertiary hospital. Although the results agree with other similar work, it should not be extrapolated to the wider population. There is no baseline information available regarding the participants’ lipid profiles before the start of ART. The family history of cardiovascular disease was not investigated. Therefore, causality was not investigated and it cannot be concluded that the identified dyslipidaemia is ART-associated, as no information is available on lipid status before the commencement of ART. A strength of the study is that adherence to the ART medication was confirmed by virological suppression as indicated by viral load counts below 400 RNA copies/ml as undertaken by previous South African researchers.Citation8,Citation14
The researchers had no control over whether or not the participants were indeed fasting as per caregivers’ report when they came in for lipid testing, as they were not inpatients whose dietary intake could be controlled. It has been suggested, however, that fasting does not make a significant difference in the lipogram results of children.Citation32
Implications and recommendations
Dyslipidaemia and consequently increased cardiovascular riskCitation15 adds to the health burden in this already strained population. Statins and fibrates are usually indicated for the medical treatment of dyslipidaemia, but these medications are contra-indicated in children younger than 10 years.Citation33 Safe and effective treatment options should be explored for young children with dyslipidaemia, whether HIV infected or not.
Recommendations
Qualitative research would be valuable in this population to determine reasons for poor adherence to ARTs, as this trend was observed by the researchers while screening the patient records for eligibility. Observational studies or qualitative research could also be helpful in determining possible reasons for poor documentation of height in medical records. Reinforcing the SA ART guidelines regarding routine lipid testing and measurement of height among the clinicians and nursing personnel working with children infected with HIV might be helpful with future monitoring of this population to identify dyslipidaemia and stunting sooner in high-risk children. Monitoring the growth patterns of HIV-infected children on ARTs can be done with the recently constructed age- and gender-specific weight gain norms developed by Yotebieng et al.Citation2
Conclusion
The findings showed a high prevalence of dyslipidaemia in HIV-infected children who have been on ART for at least six months at an outpatient clinic in Garankuwa, Pretoria. Children who were stunted at the time of lipid testing were more likely to have dyslipidaemia. Children who were on ARTs for a shorter period (less than 34 months) were more likely to have dyslipidaemia than children who had received ART for a longer period. The majority of children were initiated on a PI-based regimen. Children who were initiated on a PI-based ART regimen were more likely to have dyslipidaemia than those on an NNRTI-based regimen.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Venkatesh KK, Lurie MN, Triche EW, et al. Growth of infants born to HIV-infected women in South Africa according to maternal and infant characteristics. Trop Med Int Health. 2010;15(11):1364–1374. doi: 10.1111/j.1365-3156.2010.02634.x
- Yotebieng M, Meyers T, Behets F, et al. Age- and sex-specific weight gain norms to monitor antiretroviral treatment in children in low- and middle-income countries. AIDS. 2015;29(1):101–109. doi: 10.1097/QAD.0000000000000506
- Ramteke SM, Shiau S, Foca M, et al. Patterns of growth, body Composition, and lipid profiles in a South African Cohort of human immunodeficiency virus-infected and uninfected children: a cross-sectional study. J Pediatr Infect Dis Soc. 2017; 00(00):1–8. doi: 10.1093/jpids/pix026
- Statistics South Africa. STATISTICAL RELEASE P0302 Mid-year population estimates 2017. [cited 2017Sep 22]. Available from: http://www.statssa.gov.za/?s=children+on+ARV&sitem=publications
- Phongsamart W, Orasri W, Vanprapar N, et al. Challenges in Management of Pediatric HIV/AIDS: Thailand Perspective. Siriraj Med J [Online]. 2011;63(1):25–31.
- Barlow-Mosha L, Eckard AR, McComsey GA, et al. Metabolic complications and treatment of perinatally HIV-infected children and adolescents. J Int AIDS Soc. 2013;16:18600. doi: 10.7448/IAS.16.1.18600
- Innes S, Abdullah KL, Haubrich R, et al. High prevalence of dyslipidemia and Insulin resistance in HIV-infected Pre-pubertal African children on antiretroviral therapy. Pediatr Infect Dis J. 2016;35(1):e1–e7. doi: 10.1097/INF.0000000000000927
- Arpadi S, Shiau S, Strehlau R, et al. Metabolic Abnormalities and body Composition of HIV-infected South African children on ritonavir-Boosted Lopinavir-based or Nevirapine-based antiretroviral therapy: a Comparative study. Arch Dis Child. 2013;98(4):258–264. doi: 10.1136/archdischild-2012-302633
- Mda S. Nutritional supplementation in HIV-infected children: a review. J HIV Clin Sci Res. 2015;2(2):045–048. doi:10.17352/2455 doi: 10.17352/2455-3786.000013
- WHO Multicentre Growth Reference Study Group. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006: 312.
- De Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85(9):660–667. doi: 10.2471/BLT.07.043497
- Mandal A, Mukherjee A, Lakshamy R, et al. Dyslipidemia in HIV infected children receiving Highly Active antiretroviral therapy. Indian J Pediatr. 2016;83:226–231. doi: 10.1007/s12098-015-1859-3
- De Lima LRA, Petroski EL, Moreno YMF, et al. Dyslipidemia, chronic inflammation, and subclinical atherosclerosis in children and adolescents infected with HIV: the PositHIVe health study. PLOS ONE; 13(1):e0190785. doi: 10.1371/journal.pone.0190785
- Strehlau R, Coovadia A, Abrams EJ, et al. Lipid profiles in young HIV-infected children initiating and changing antiretroviral therapy. J Acquir Immune Defic Syndr. 2012;60(4):369–376. doi: 10.1097/QAI.0b013e318243760b
- Bușilă C, Stuparu-Crețu M, Barna O, et al. Dyslipidemia in children as a risk factor for cardiovascular diseases. Biotechnol Biotechnol Equip. 2017;31(6):1192–1197. doi: 10.1080/13102818.2017.1376596
- South African National Department of Health. National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults. April 2015.
- Bwakura-Dangarembizi M, Musiime V, Szubert AJ, et al. Prevalence of lipodystrophy and metabolic abnormalities in HIV infected African children after 3 years on first line antiretroviral therapy. Pediatr Infect Dis J. 2015;34(2):e23–e31. doi: 10.1097/INF.0000000000000491
- Sonego M, Sagrado MJ, Escobar G, et al. Diet and physical Exercise in children on treatment with antiretroviral medication in El Salvador: a cross-sectional study. Pediatr Infect Dis J. 2016 Oct;35(10):1111. doi: 10.1097/INF.0000000000001244
- Nampijja D, Kumbakumba E, Bajunirwe F, et al. Dyslipidemia and its Correlates among HIV infected children on HAART attending Mbarara Regional Referral hospital. Int Clin Pathol J. 2017;4(3):00098. doi: 10.15406/icpjl.2017.04.00098
- Padmapriyadarsini C, Shet A, Srinivasan R, et al. High prevalence of lipid abnormalities and insulin resistance among antiretroviral Naïve HIV-infected children in India. Pediatr Infect Dis J. 2018;37(3):253–257. doi: 10.1097/INF.0000000000001829
- Boccara F, Cohen A. HIV and heart disease: what cardiologists should know. Rev Esp Cardiol. 2016;69:1126–30. doi:10.1016/j.rec.2016.05.032 doi: 10.1016/j.recesp.2016.05.037
- Paganella MP, Cohen RA, Harris DR, et al. Association of dyslipidemia and glucose abnormalities with antiretroviral treatment in a Cohort of HIV-infected latin American children. J Acquir Immune Defic Syndr. 2017;74(1):e1–e8. doi: 10.1097/QAI.0000000000001163
- Lee RD, Nieman DC. Nutritional assessment. 6th ed. New York (NY): McGraw-Hill; 2013: 166–220.
- National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and treatment of high blood cholesterol in Adults (Adult treatment Panel III). Third report of the National cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and treatment of high blood cholesterol in Adults (Adult treatment Panel III) final report. Circulation. 2002;106:3143–3421. doi: 10.1161/circ.106.25.3143
- Kyle U, Shekerdemian LS, Coss-Bu JA. Growth failure and nutrition considerations in chronic childhood wasting diseases. Nutr Clin Pract. 2015;30(2):227–238. doi: 10.1177/0884533614555234
- Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health. 2014;34(4):250–265. doi: 10.1179/2046905514Y.0000000158
- Reid BM, Harbin MM, Arend JL, et al. Early life adversity with height stunting is associated with cardiometabolic risk in adolescents independent of body mass index. J Pediatr. 2018;202:143–149. doi: 10.1016/j.jpeds.2018.06.047
- De Lucia Rolfe E, de Franca GVA, Vianna CA, et al. Associations of stunting in early childhood with cardiometabolic risk factors in adulthood. PLoS ONE. 2018;13(4):e0192196. doi: 10.1371/journal.pone.0192196
- Merchant RH, Lala MM. Common clinical problems in children living with HIV/AIDS: systemic approach. Indian J Paediatr. 2012;79(11):1–8.
- Yotebieng M, Van Rie A, Harry Moultrie H, et al. Six-month gain in weight, height, and CD4 predict subsequent antiretroviral treatment responses in HIV-infected South African children. AIDS. 2010;24:139–146. doi: 10.1097/QAD.0b013e328332d5ca
- Scholtz J, Kruger HS. Comparison of weight gain to age- and sex-specific norms in children 2 to 10 years old on highly active anti-retroviral treatment [Unpublished Master’s Mini dissertation], North West University. 2017.
- Steiner MJ, Skinner AC, Perrin EM. Fasting might not be necessary before lipid screening: a nationally representative cross-sectional study. Pediatrics. 2011;128(3):463–470. doi: 10.1542/peds.2011-0844
- Iughetti L, Predieri B, Bruzzi P. Hypercholesterolemia in childhood. Hypercholesterolemia; InTech. 2015;(2):33–53. doi:10.5772/59760