ABSTRACT
Background
Acquired haemophilia A (AHA) is a rare immune-mediated disorder characterised by the development of autoantibodies against factor VIII. Morbidity and mortality are in general high due to multiple factors including the age of the patient, underlying diseases, toxic effects of available treatments and bleeding itself.
Objective
To assess the awareness about AHA among healthcare professionals (HCPs) in Lebanon where patients can present to non-haematologists with life-threatening bleeding disorders.
Methods
A cross-sectional survey was conducted in September and October 2017 all over Lebanon among HCPs. The survey covered: (i) the geographic area of practice and specialty; (ii) bleeding disorders encountered within the last 2 years; (iii) assessment of knowledge on AHA; and (iv) importance of increasing awareness on AHA among HCPs.
Results
A total of 362 participants completed and returned the questionnaire (response rate 100%). The majority of the HCPs were practicing in Beirut (n=164; 45.3%) and were internists (n=106; 29.3%). 332 (93%) HCPs have encountered patients with bleeding problems within the last 2 years all over Lebanon. 327 (92.1%) HCPs agreed that increasing awareness on AHA among health care professionals is important. HCPs gave an average of 75.9% of correct answers on the survey.
Conclusions
Appropriate treatment and diagnosis are essential when dealing with AHA. Knowledge gaps exist in the clinical practice when dealing with patients who have AHA. This study shows the need for increasing awareness about AHA among HCPs in Lebanon regarding the diagnosis and treatment of this disorder.
Introduction
Acquired haemophilia A (AHA) is a rare bleeding disorder and autoimmune disease which incidence increases with age [Citation1,Citation2], ranging worldwide from an estimated 0.045 per million annually in the young population (<16 years) to 14.7 per million per year in elderly (>85 years) [Citation1,Citation3]. It is also dominant in men in non-pregnancy-related AHA and up to 50% of reported cases are idiopathic [Citation1,Citation2]. In the other cases, AHA is secondary to underlying conditions such as medications (e.g. antibiotics, phenytoin, chloramphenicol, methyldopa, interferon alpha, and fludarabine), pregnancy, acute hepatitis B and C infections, respiratory disease (e.g. asthma, chronic obstructive pulmonary disease), malignancy (haematological malignancy and solid organ tumours), and other autoimmune diseases (e.g. systemic lupus erythematosus, rheumatoid arthritis and multiple sclerosis) [Citation1,Citation2,Citation4].
In terms of physiopathology, AHA is caused by immunoglobulin G antibodies against specific domains of the clotting factor (F) VIII molecule [Citation1,Citation2], leading to a partial or complete neutralisation of its coagulant function [Citation2]. On a similar note, FVIII deficiency decreases thrombin generation on the surface of activated platelets, given its role as a cofactor in the activation of FIX in the tenase complex. Thus, FVIII deficiency predisposes to spontaneous or provoked bleeding that can be severe and often life-threatening [Citation2].
AHA should be suspected in persons with a negative personal or family history of a coagulopathy and an unexplained prolonged activated partial thromboplastin time (aPTT) [Citation1,Citation2]. As for the clinical presentation of AHA, it is characterised by spontaneous subcutaneous hematomas and extensive bruising although haematuria, epistaxis, muscle bleeding, gastrointestinal bleeding, and intracranial haemorrhage may occur [Citation2]. It is noteworthy that hemarthrosis (joints bleeding) is not common in AHA in contrast with congenital haemophilia [Citation5].
The management of AHA is challenging given the disease complexity and involves three approaches [Citation1]. The first one requires controlling bleeding using haemostatic therapy depending on the bleeding site and severity [Citation1,Citation14]. The second consists of eradicating the acquired inhibitor by using immunosuppressive agents in all persons with AHA immediately upon diagnosis [Citation1,Citation14]. Data have shown that patients remain at risk for life-threatening haemorrhage until the autoantibody has been eradicated, even if they are not actively bleeding [Citation3], while those who achieve a complete response to inhibitor eradication have an improved overall survival [Citation6]. Third, any underlying cause should be investigated [Citation1].
Similarly to any life-threatening condition, a good prognosis of AHA is ensured by an early diagnosis and treatment [Citation4]. However, the diagnosis and treatment of AHA are often delayed given the rarity of the disease and the non-familiarity of the healthcare professionals (HCPs) with the disease [Citation1,Citation7]. It is critical for the primary health care providers to perform a complete assessment and be aware of rare yet clinically relevant diseases such as AHA [Citation14]. This study aimed to assess the awareness of HCPs about AHA in Lebanon and to identify whether HCPs encounter cases of AHA and whether gaps in knowledge about AHA exist. To our knowledge, no previous study on this issue has been conducted in the Lebanon or the region.
Materials and methods
Study design and target population
A cross-sectional survey initiated by Novo Nordisk was conducted in September and October 2017 all over Lebanon among HCPs, affiliated to the Lebanese Order of Physicians (LOP) and are from different specialities who may be exposed to cases of AHA. An initial random sample of 362 HCPs was chosen from the LOP database.
Data collection
Data were collected anonymously using a 3-page paper self-administered questionnaire written in English language and consisting of 10 questions. The questionnaire was prepared during an advisory board and based on insights from key opinion leaders in haematology. The questions were yes/no questions with the participant requested to check the appropriate answer by simple check and in very few sections the participants were asked to comment in short answers. The HCPs self-reported the answers at their clinic during a 7-minute interview with a study field coordinator who was trained for the purpose of this interview by a clinical research organisation. The questionnaire covered the following: (i) the geographic area of practice and specialty; (ii) bleeding disorders encountered within the last 2 years; (iii) assessment of knowledge on AHA (definition, laboratory results, diagnosis and treatment); and (iv) importance of increasing awareness on AHA among HCPs (Appendix 1).
Statistical analysis
Manual double data entry of data was used for the purpose of this study followed by a quality of control of the completed database. Data were summarised using count distribution (frequency and percentage) since all variables were qualitative. Data were stratified by area and specialty. They were also compared to the correct answers set by a scientific committee without using any statistical test since the study was exploratory. The statistical analysis was carried out using the IBM SPSS software application (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.).
Ethics consideration
A comprehensive description about this study was introduced to participants, before the interview, who were allowed to decline to answer at the first or withdrawing at any time after. Strict confidentiality of the answers was maintained throughout the study. The responses were sealed, collected and analysed after all data was collected. No benefits or hazards were discerned in this context and no patients’ data were to be collected. Thus, no approval was required from ethics committee. The questionnaire completion was equivalent to consenting to participate in the study.
Results
During the 2-month study period, a total of 362 HCP were approached for study participation. A total of 362 participants completed and returned the questionnaire (response rate 100%). No questionnaires were excluded. The majority of the HCPs were practicing in Beirut (n=164; 45.3%) and were internists (n=106; 29.3%; ).
Table 1. Demographic Characteristics of the Participants (n = 362).
In total, 332 (93%) HCPs have encountered patients with bleeding problems within the last 2 years all over Lebanon. HCPs had mainly diagnosed patients with platelets disorders (n=255; 74.6%), followed by coagulation disorders such as liver disease (n=192; 53.9%), disseminated intravascular coagulation (n=174; 48.9%), vitamin K deficiency (n=122; 34.3%), and Von Willebrand disease (n=118; 32.2%) as shown in .
Table 2. Bleeding disorders encountered within the last 2 years.
As for the assessment of knowledge on AHA, results are presented in . 308 (89.3%) HCPs reported that AHA is a spontaneously occurring autoimmune disorder that is caused by inhibitory antibodies against a coagulation factor, 266 (76.4%) HCPs answered that it affects patients with no previous history of bleeding tendency. Less HCPs (n=236; 70.2%) considered that AHA affects all age groups and 235 (68.1%) answered that it is a life-threatening condition. Regarding laboratory tests showing aPTT prolongation, 290 (82.2%) HCPs considered it as an alert for a bleeding problem, 246 (7.7%) reported that they order a second blood test then a mixing test while 107 (36.4%) call the laboratory to check the type of aPTT kit used. The majority of the HCPs (n=333; 94.9%) reported that they rely on the laboratory results (aPTT prolongation, low FVIII level, uncorrected aPTT after a mixing test and a high inhibitor titre) for diagnosing an AHA bleeding patient while 258 (75.2%) rely on the clinical features. As for the mixing test, 268 (80.7%) HCPs had a general knowledge on the test’s purpose and 262 (72.4%) were aware of its technique.
Table 3. Assessment of knowledge on AHA.
Regarding the safety of patient with prolonged aPTT to undergo surgery, 299 (87.9%) HCPs reported that they postpone surgery if the patient has bleeding signs, 294 (84.7%) HCPs chose to refer the case and check it with a haematologist and 288 (84.5%) replied that they investigate immediately the reason of the aPTT prolongation. Only 59 (17.9%) HCPs answered that they proceed with surgery if there is no active bleeding.
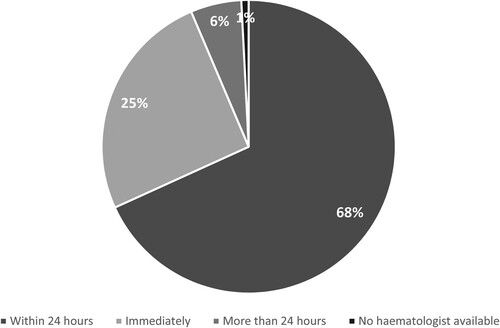
In case a haematologist consultation is requested, 242 (68%) HCPs declared that the haematologist at their institution responds within 24 h while 90 (25%) and 20 (6%) HCPs responded that the consultant responds immediately or after more than 24 h respectively 3 (1%) answered that they have no haematologist at their institution as shown in . In addition, 327 (92.1%) HCPs agreed that increasing awareness on AHA among health care professionals is important. Indeed, 11 HCPs commented that bleeding may be very severe and may have a sudden onset. Therefore, prompt haemostatic control is mandatory in order to reduce morbidity and mortality. HCPs expressed concerns about the under diagnosis of AHA and the need for raising awareness and learning more on the disease because they rarely encounter such cases as shown in and . The importance of increasing awareness was significantly agreed upon by the majority of HCPs regardless of neither the area of practice nor the specialty. With the acquirement of more knowledge on AHA, the HCPs assumed to be able to easily manage this disorder. Finally, data showed that the HCPs gave an average of 75.9% of correct answers ranging from 36.4 to 94.9% ().
Figure 2. Responses regarding the importance of increasing awareness on AHA among health care professionals by area.
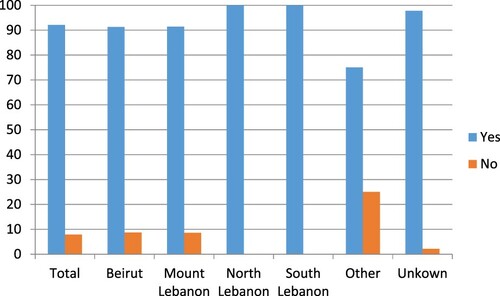
Figure 3. Responses regarding the importance of increasing awareness on AHA among health care professionals by specialty.
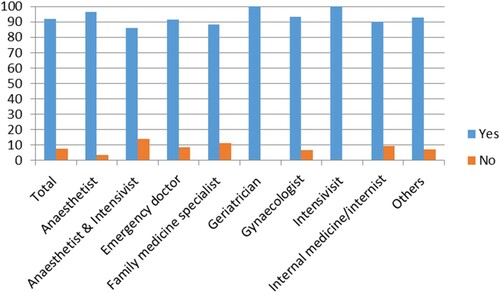
Table 4. Agreement between the participants’ responses to the survey and the correct answers (n=362).
Discussion
AHA is a rare immune-mediated disorder characterised by the development of autoantibodies against factor VIII [Citation11]. Patients with autoantibodies to coagulation factor VIII may present initially to physicians in different specialties, who may not have experience with this rare disorder [Citation9]. Our survey highlighted the gap in awareness and knowledge on AHA given that the HCPs had an average of 75.9% of correct answers. For example, our results showed that not all HCPs had a referring specialist or that the referring haematologist needed more than 24 h to be available, while the literature recommends that doctors managing a patient with suspected or confirmed AHA, with or without bleeding, should consult a haemophilia centre with expertise in managing inhibitors as soon as possible [Citation8]. Although this recommendation is not of high level of evidence, it is supported by the World Federation of Haemophilia [Citation5]. Referral to a specialist is necessary since patients usually present to physicians who are not specialists in the field or familiar with AHA cases. These are typically geriatricians, obstetricians, rheumatologists, oncologists, emergency doctors, intensivists or surgeons and even haematologists [Citation6]. AHA can also be an early manifestation of other diseases such as autoimmune diseases and cancer; thus, specialists must be aware of this life-threatening condition which may develop years prior to the diagnosis of other conditions such has cancer [Citation12].
The importance of raising awareness about AHA among HCPs was highlighted in our study where the vast majority of participants indicated the need for such action. Awareness of this disorder by medical personnel at all levels in the community and in various specialties is important [Citation13]. Haematology specialists should direct their efforts to raise awareness about this disorder among physicians and provide guidance on how to diagnose and treat AHA [Citation10].
Limitations
This study has two major limitations. First, the sample was not representative of all Lebanese HCPs as the study mainly targeted Lebanon’s major cities and few participated from the remote areas. It is expected that HCPs in remote areas would have lower levels of awareness on AHA. The second limitation was the use of a self-assessment tool which is considered to be lacking objectivity and accuracy: participants might have the tendency to under- or over-report. Although using such type of tools is not specific, a self-assessment tool can capture a general picture of the HCPs’ knowledge and awareness on AHA in Lebanon. Notably, we did not display the correct answers during the survey conduct to avoid any additional reporting bias or acquiescent response bias. As such, the participants will not over-report ‘positive aspects’ to be viewed favourably by the surveyor, and results will be more valid.
Conclusion
Knowledge gaps permeate clinical practice in the care of patients with AHA, which is a rare life-threatening bleeding disorder. Our data emphasised the need for conducting continuing and accredited educational lectures and workshops to increase the HCPs’ awareness and knowledge on AHA in Lebanon. These can be organised all over the country and across a range of practice settings by the LOP with the support of haematologists or pharmaceutical companies and can ultimately lead to a prompt diagnosis and a better management of the disease.
Competing interests
Some authors are members of the advisory board of Novo Nordisk. AC and RH supported in drafting the questionnaire and reviewing the manuscript.
Supplemental Material
Download MS Word (16.1 KB)Acknowledgements
We thank the study staff and all participants. The authors thank Phoenix Clinical Research, Lebanon for providing data collection, management and analysis services. Medical writing support was also provided by Racha Aaraj, Pharm D, MSc, MPH from Phoenix Clinical Research, Lebanon.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Janbain M, Leissinger CA, Kruse-Jarres R. Acquired hemophilia A: emerging treatment options. J Blood Med. 2015;6:143–150. doi:https://doi.org/10.2147/JBM.S77332. eCollection 2015.
- Mulliez SM, Vantilborgh A, Devreese KM. Acquired hemophilia: a case report and review of the literature. Int J Lab Hematol. 2014;36(3):398–407. doi:https://doi.org/10.1111/ijlh.12210.
- Collins PW, Hirsch S, Baglin TP, et al. UK haemophilia Centre Doctors’ Organisation Acquired hemophilia A in the United Kingdom: a 2-year national surveillance study by the United Kingdom Haemophilia Centre Doctors’ Organisation. Blood. 2007;109(5):1870–1877.
- Zdziarska J, Musiał J. Acquired hemophilia A: an underdiagnosed, severe bleeding disorder. Pol Arch Med Wewn. 2014;24(4):200–206. Epub 2014 Mar 21.
- Giangarande P. (2014). Acquired hemophilia. In: Treatment of hemophilia. November 2014, No. 38. World Federation of Hemophilia.
- Delgado J, Jimenez-Yuste V, Hernandez-Navarro F, et al. Acquired haemophilia: review and meta-analysis focused on therapy and prognostic factors. Br J Haematol. 2003;121(1):21–35.
- Sakurai Y, Takeda T. Acquired hemophilia a: a frequently overlooked autoimmune hemorrhagic disorder. J Immunol Res. Article ID 320674, 2014;10; doi:https://doi.org/10.1155/2014/320674.
- Collins P, Baudo F, Huth-Kühne A, et al. Consensus recommendations for the diagnosis and treatment of acquired hemophilia A. BMC Res Notes. 2010;3:161), doi:https://doi.org/10.1186/1756-0500-3-161.
- Huth-Kuhne A, et al. International recommendations on the diagnosis and treatment of patients with acquired hemophilia. A.Haematologica. 2020 Jul;105(7):1791–1801.
- Mady AF, et al. Awareness and perspectives on nom haematologist in the management of acquired haemophilia in Arab gulf countries. Esculapio. April–June 2018;14(2).
- Lassila R. Management of coagulation factor VIII (FVIII) inhibitors. Thromb Res. 2019;181(Suppl 1):S60–s61.
- Pacholczak R, et al. Acquired haemophilia A Associated with Subsequent Hepatocellular Carcinoma. Hamostaseologie. 2019 Feb;39(1):95–99. doi:https://doi.org/10.1055/s-0038-1668570. Epub 2018 Aug 15.
- Ab W, Rahman WS, et al. Epidemiology, spectrum of clinical manifestations and diagnostic issue of acquired haemophilia: A case series. Malays J Pathol. 2019 Aug;41(2):185–189.
- Kiam GWP. Acquired Hemophilia in a patient Presenting with Swollen Left Limb. Korean J Fam Med. 2019 Mar;40(2):129–132. doi:https://doi.org/10.4082/kjfm.17.0126. Epub 2018 Jul 13.