ABSTRACT
Background: Obesity has been associated with increased incidence of myelodysplastic syndromes (MDS). Recently intriguing data in mouse models suggested that obesity increases survival in animals with MDS.
Methods: This was a retrospective analysis using the Moffitt MDS database. Obesity was defined by using body mass index (BMI), whereby a BMI ≥ 30 was regarded as obese.
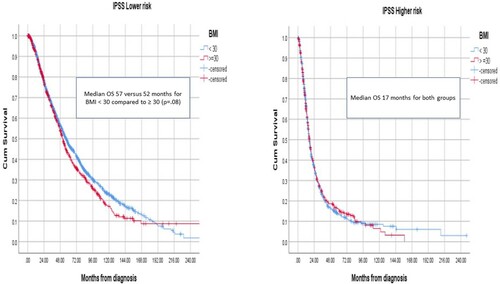
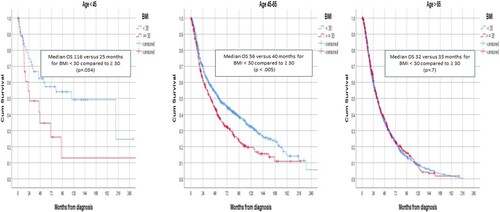
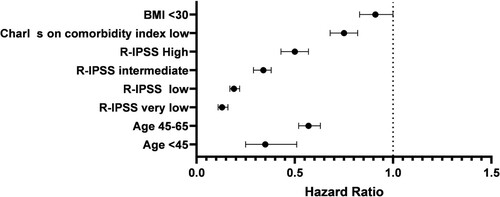
Results: Among 3089 MDS patients with known BMI, 963 patients (31%) were categorized as obese. There were no differences in baseline characteristics between patients with BMI ≥ 30 and those with <30. The median OS for patients with BMI ≥ 30 was 34 months compared to 37 months for those with BMI < 30 (p 0.04). For patients with lower-risk MDS median OS was 52 months versus 57 months, respectively, (p 0.08) while for higher-risk patients median OS was 17 months for both groups. The rate of AML transformation was 36% for patients with BMI ≥ 30 compared to 32% for those with BMI < 30 (p 0.009). There was no difference in response to azacitidine. In multivariable analysis, BMI was associated with inferior OS. For patients < 45 years old, the median OS was 25 months for patients with BMI ≥ 30 compared to 116 months for those with BMI < 30 (p 0.034).
Conclusions: Obesity is associated with inferior overall survival (OS) in MDS patients in less than 65 years old and lower MDS risk. Impact of obesity on the outcome of MDS is being explored in both mice and human. Here we reported the impact of obesity on OS in MDS patients. Obesity is associated with inferior OS in MDS patients particularly younger age groups and lower MDS risk.
Introduction
Myelodysplastic syndromes (MDS) are a group of hematological malignancies characterized by ineffective hematopoiesis and patients are at a higher risk to develop acute myeloid leukemia (AML) [Citation1]. Obesity is defined as a body mass index (BMI) of ≥30, and is a complex and multifactorial disease with genetic and environmental predisposition and results in a wide health sequelae affecting nearly one-third of the world’s population [Citation2].
Many diseases have been linked to obesity including cancers [Citation3]. And in fact, obesity has been associated with an increased incidence of MDS in older people [Citation4].
Some studies suggested that obese people with AML have a favorable course of treatment in term of higher complete remission rate, lower rate of resistant disease and lower toxicity [Citation5] but also with increased re-admission rates after allogeneic hematopoietic stem cell transplantation (AHSCT) without affecting overall survival (OS) in these patients [Citation6].
Different studies both in humans and mice models have investigated this association. Recently intriguing data in mouse models suggested that obesity increases survival in animals with MDS. Greater fat mass of Ob/Ob mice may serve as a reservoir of adipocyte-derived danger-associated molecular patterns (DAMPs) directing skewing and expansion of immature myeloid cells [Citation7].
Given these observations, we hypothesized that obesity might influence OS in MDS patients. As it has not been well-studied, here we retrospectively examined this association in different age groups and risk categories.
Patients and methods
This is a retrospective, single-center study using our institutional database for MDS patients at Moffitt Cancer Center. The patient population consisted of adult MDS patients with different age groups (<45, 45–65 and >65 years old). MDS risk stratification was calculated according to the International Prognostic Scoring System (IPSS) at the time of diagnosis and patients were categorized into two groups with either low and intermediate-1 vs. intermediate-2 and high risk. Revised IPSS (R-IPSS) was also calculated for MDS risk stratification. Obesity was defined by using BMI and patients with BMI > 30 were categorized as obese. Descriptive statistics were used to describe baseline characteristics. Median OS was calculated from the time of diagnosis using Kaplan-Meier estimator. Multivariate analysis was performed adjusting for Charlson Comorbidity Index.
Results
We identified 3089 MDS patients with known BMI in our database. Of these, 963 patients (31%) were categorized as obese, 637 men and 326 women.
There was no difference in baseline characteristics between patients with BMI ≥ 30 and those with <30 (). There was no significant difference in age, IPSS, R-IPSS, therapy-related MDS (t-MDS), myeloblast, hemoglobin, platelets, absolute neutrophil count (ANC), whether or not received AHSCT or Azacitidine.
Table 1. Baseline characteristics for obese vs. non-obese MDS patients.
The median OS for patients with BMI ≥ 30 was 34 months (mo) (95% CI 31–38) compared to 37 mo (95% CI 34–40) for patients with BMI < 30 (p 0.04).
Obese patients with lower-risk MDS (low/int-1 by IPSS) had median OS of 52 mo versus 57 mo in non-obese (p 0.08). Patients with higher-risk MDS (int-2/high) had median OS of 17 mo for both groups (). In patients younger than 45 years old (n = 79), obesity was significantly associated with decreased median OS, where for those patients with BMI ≥ 30 (n = 19) the median OS was 25 mo compared to 116 mo for those with BMI < 30 (n = 60) (p 0.034). For patients between the age of 45–65 years (n = 1052), the median OS was 40 mo for obese (n = 385) vs. 56 mo for non-obese patients (n = 667) (p < 0.005). The impact of obesity was less relevant for older people as in patients > 65 years old (n = 1954), the median OS was 33 mo for obese patients (n = 559) compared to 32 mo, in non-obese patients (n = 1395) (p 0.7) (). There was no difference in rate of t-MDS among different age groups.
There was no difference in the impact of BMI on the outcome based on gender or race.
The rate of AML transformation was 36% for patients with BMI ≥ 30 compared to 32% for those with BMI < 30 (p 0.009). Overall, response rate to Azacitidine was 32% in both groups.
In multivariate analysis, R-IPSS, age, Charlson Comorbidity Index, and BMI were significantly associated with OS ().
Discussion
Obesity is a known risk factor for many types of cancers including hematological malignancies [Citation8,Citation9]. Mechanisms describing the association between obesity and myeloid malignancies including MDS is complex and is currently being further studied. It was found that adiponectin, leptin and fetuin-A may represent potential biomarkers reflecting the association between obesity and MDS, with lower adiponectin and higher leptin and fetuin-A are associated with higher risk of MDS. Adiponectin is a multimeric protein that is secreted mainly by white adipose tissue with various protective biological actions driven by its anti-inflammatory effect and increasing insulin sensitivity in liver and skeletal muscles [Citation10]. Adiponectin receptors are also expressed in the bone marrow environment and result in proliferative effect on the hematopoietic stem cells [Citation11] and its level correlates inversely with MDS risk, as patients with lower-risk MDS found to have higher adiponectin levels [Citation12,Citation13]. On the other hand, both Leptin and fetuin-A were associated with higher-risk MDS [Citation14].
In mice models, it has been suggested that obese mice with MDS have a better OS. It was thought initially that adipose tissue promotes myelopoiesis, and that would accelerate the transition of MDS to AML and increase mortality. However, the same group later hypothesized that adipose tissues in obese mice sequester the increased number of myeloid cells, sparing organs from this burden, eventually limit end-organ damage and prolongs survival [Citation7], although this was suggested in observation of leptin-deficient mice rather than obese over-fed mice making it challenging to know if this applies in MDS patients population.
It was found that obesity increases risk of MDS in female patients, although unclear why is the gender preference in this association but hormones and percentages of adipose tissues might have played a role [Citation15].
Jabbar et al. [Citation16] previously reported that overweight patients had longer survival without progression to AML compared to normal weight patients with the impression that being obese is a favorable factor in MDS. In our study, we found that obesity significantly reduced OS particularly for younger MDS patients less than 65 years old and lower-risk group. It is unclear why is this age preference but might suggest that OS in older people in this population was driven by the comorbidities these patients had thus the no difference between the two groups. Another group also found that obese patients with lower-risk MDS present at a younger age with more severe anemia, thrombocytopenia and a higher proportion of patients needing treatment with hypomethylating agents [Citation17]. The inferior OS being mostly observed in lower-risk MDS is expected as the interaction between disease and comorbidities plays a larger impact among this group compared to higher-risk patients where outcomes are mostly dictated by disease risk features.
Limitations of our study are first, the prevalence of obesity among the United States population overall is 42.4% which is much higher than in our MDS population at Moffitt Cancer Center (31%) [Citation18]. Another limitation is the retrospective nature of our study making it difficult to look at specific parameters that might have an impact on the result that otherwise went unnoticed and lack of socioeconomic demographics which may play role in those differences Given these observations we conclude that obesity affects OS in younger MDS population as opposed to elderly and lower-risk MDS. It is not plausible to assess the interaction between obesity and MDS in this study whether the increased mortality observed in younger obese MDS patients is merely related to obesity in general and its well-known health complications or an effect of obesity on disease biology. It is also not clear if intervening with weight reduction programs will impact outcome. Future prospective studies will be warranted to further address those questions.
Conclusion
Obesity is associated with lower OS in MDS patients particularly younger than 65 years old and lower MDS risk.
Clinical practice points
Obese young MDS patients have lower OS than non-obese MDS patients.
Obesity did not affect over OS in elderly MDS patients
No difference in response rate to hypomethylating agents was observed.
Acknowledgements
ZS wrote the manuscript, NA collected data and analysis. DS and EP contributed patients and reviewed data. RK designed study, analyzed data and contributed patients. All authors read and approved final manuscript submitted.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Klepin HD. Myelodysplastic syndromes and acute myeloid leukemia in the elderly. Clin Geriatr Med. 2016;32(1):155–173. doi:https://doi.org/10.1016/j.cger.2015.08.010.
- Hruby A, Hu FB. The epidemiology of obesity: A Big picture. Pharmacoeconomics. 2015;33(7):673–689. doi:https://doi.org/10.1007/s40273-014-0243-x.
- Djalalinia S, Qorbani M, Peykari N, et al. Health impacts of obesity. Pakistan J Med Sci. 2015;31(1):239–242. doi:https://doi.org/10.12669/pjms.311.7033.
- Ma X, Lim U, Park Y, et al. Obesity, lifestyle factors, and risk of myelodysplastic syndromes in a large US cohort. Am J Epidemiol. 2009;169(12):1492–1499. doi:https://doi.org/10.1093/aje/kwp074.
- Medeiros BC, Othus M, Estey EH, et al. Impact of body-mass index on the outcome of adult patients with acute myeloid leukemia. Haematologica. 2012;97(9):1401–1404. doi:https://doi.org/10.3324/haematol.2011.056390.
- Voshtina E, Szabo A, Hamadani M, et al. Impact of obesity on clinical outcomes of elderly patients undergoing allogeneic hematopoietic cell transplantation for myeloid malignancies. Biol Blood Marrow Transplant. 2019;25(1):e33–e38. doi:https://doi.org/10.1016/j.bbmt.2018.08.031.
- Kraakman MJ, Kammoun HL, Dragoljevic D, et al. Leptin-deficient obesity prolongs survival in a murine model of myelodysplastic syndrome. Haematologica. 2018;103(4):597–606. doi:https://doi.org/10.3324/haematol.2017.181958.
- Castillo JJ, Reagan JL, Ingham RR, et al. Obesity but not overweight increases the incidence and mortality of leukemia in adults: a meta-analysis of prospective cohort studies. Leuk Res. 2012;36(7):868–875. doi:https://doi.org/10.1016/j.leukres.2011.12.020.
- Renehan AG, Tyson M, Egger M, et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–578. doi:https://doi.org/10.1016/S0140-6736(08)60269-X.
- Ziemke F, Mantzoros CS. Adiponectin in insulin resistance: lessons from translational research. Am J Clin Nutr. 2010;91(1):258S–261S. doi:https://doi.org/10.3945/ajcn.2009.28449C.
- DiMascio L, Voermans C, Uqoezwa M, et al. Identification of adiponectin as a novel hemopoietic stem cell growth factor. J Immunol. 2007;178(6):3511–3520. doi:https://doi.org/10.4049/jimmunol.178.6.3511.
- Dalamaga M, Nikolaidou A, Karmaniolas K, et al. Circulating adiponectin and leptin in relation to myelodysplastic syndrome: a case-control study. Oncology. 2007;73(1-2):26–32.
- Dalamaga M, Karmaniolas K, Nikolaidou A, et al. Adiponectin and resistin are associated with risk for myelodysplastic syndrome, independently from the insulin-like growth factor-I (IGF-I) system. Eur J Cancer. 2008;44(12):1744–1753. doi:https://doi.org/10.1016/j.ejca.2008.04.015.
- Dalamaga M, Karmaniolas K, Chamberland J, et al. Higher fetuin-A, lower adiponectin and free leptin levels mediate effects of excess body weight on insulin resistance and risk for myelodysplastic syndrome. Metab Clin Exp. 2013;62(12):1830–1839. doi:https://doi.org/10.1016/j.metabol.2013.09.007.
- Poynter JN, Richardson M, Blair CK, et al. Obesity over the life course and risk of acute myeloid leukemia and myelodysplastic syndromes. Cancer Epidemiol. 2016;40:134–140. doi:https://doi.org/10.1016/j.canep.2015.12.005.
- Jabbar KJ, Yin CC, Bueso-Ramos CE, et al. Higher body mass index is associated with better survival in patients with myelodysplastic syndromes. Leuk Res. 2018;71:63–66. doi:https://doi.org/10.1016/j.leukres.2018.07.008.
- Thibaud S, Adrianzen Herrera D, Snyder R, et al. Obesity Is associated with younger age at presentation and more severe cytopenias in myelodysplastic syndromes. Blood. 2017;130(Supplement 1):5312. doi:https://doi.org/10.1182/blood.V130.Suppl_1.5312.5312.
- Hales C, Carroll M, Fryar C, et al. Prevalence of obesity and severe obesity Among adults: United States, 2017-2018. NCHS Data Brief, MMWR. 2020;69(13).