ABSTRACT
Objective
To explore the relationship between platelet count and bleeding score in immune thrombocytopenia purpura (ITP) and compare the clinical practicability of two bleeding grading systems with adult patients with ITP.
Methods
A total of 204 patients were retrospectively analyzed with the ITP bleeding scale (IBLS) and the ITP bleeding assessment tool (version 2016) (ITP-2016). The correlation between the two bleeding score systems and the relations among the platelet counts were respectively analyzed.
Results
(1) There is a linear relationship between platelet count and bleeding score, no matter which scoring system it is based on (rs = −0.429, p < 0.001; rs = −0.331, p < 0.001, the analysis of the number of sites of Grade 1/2 bleeding were done; and rs = −0.466, p < 0.05, the analysis between platelet count and bleeding score by ITP-2016 respectively). (2) Platelet count and bleeding scores are negatively correlated in those with extremely low platelet counts ( < 10*109/L). The number of sites of Grade 2 bleeding and the ITP-2016 scores are negatively correlated with platelet counts (rs = −0.15 and rs = −0.244, p < 0.05, respectively). Significantly, there is no correlation between the platelet count and bleeding scores when the platelet count is more than 10*109/L. (3) It takes less time to score with ITP-2016 than IBLS (z = −3.825, P < 0.001).
Conclusions
There is good responsiveness, strong assessment consistency, close correlation between ITP-2016 and IBLS. ITP-2016 takes less time-consuming in clinical application. It can be used as an effective tool of condition judgement, risk assessment and efficacy evaluation of patients with ITP.
1. Introduction
Immune thrombocytopenia purpura (ITP) is an autoimmune hemorrhagic disease, characterized by a decreased platelet count ( < 100*109) and suppressed platelet development [Citation1]. The incidence of ITP increases with age, with an incidence rate of 20–40/million adults (over 18 years old) /year and higher in the people over 60 years old [Citation2]. The main clinical manifestations were bleeding symptoms, but heterogeneity between manifestations was noted. Severe thrombocytopenia is considered as a risk factor for bleeding in ITP, but patients with moderate or even mild thrombocytopenia can also experience severe bleeding, which seems like a disproportionate performance [Citation3,Citation4].
Bleeding is one of the leading causes of death in patients with thrombocytopenia [Citation5–7]. Bleeding manifestations in ITP with mild mucocutaneous to life-threatening bleeding, and prediction of severe bleeding is instructive to the management of thrombocytopenia.
Bleeding assessment tools [Citation8–12], such as ITP Bleeding Assessment Tool (ITP-BAT), ITP Bleeding Scale (IBLS) and Khellaf bleeding score, have been developed and studied in a variety of clinical settings for diagnosis and to evaluate the severity of bleeding. Due to time-consuming and complicated program, these guidelines are not widely used. There is still no method for objective evaluation of bleeding in thrombocytopenic patients that has been validated. In the absence of tools to evaluate bleeding risk, a large proportion of patients with ITP without significant bleeding are treated with pharmacologic agents.
In 2007, Page et al. put forward a method for objective quantification of bleeding symptoms in ITP, which is IBLS, which is a prerequisite for examining the relationship between laboratory parameters and bleeding. It creates a denser picture of bleeding symptoms than previously published scales. However, in the absence of large-scale data, this evaluation tool has not been widely used in real world to quantify the bleeding condition of patients with ITP. The ITP-2016, recommended by the Society of Hematology, Chinese Medical Association [Citation13], has the characteristic of more simplicity and less time taking than those exiting tools, improving its clinical practicability.
In this study, we retrospectively assessed the relationship between platelet count and bleeding score in patients with ITP and compared the clinical aspects of existing two ITP bleeding score systems, IBLS and ITP-2016.
2. Methods
2.1. Study design and patient selection
This study assessed 204 patients with ITP between December 2018 and April 2020 and enrolled in the Huaian No.1 People’s hospital and their symptoms and bleeding scores were analyzed. Patients with a diagnosis of primary ITP were eligible for enrollment. Signed informed consent was obtained prior to study procedures. This research was ratified by Ethics Committees of relevant institutions and implemented in conformity with the Declaration of Helsinki.
Patients eligible for enrollment were: (1) male and female patients older than 18 years; (2) with a diagnosis of primary ITP according to the guidelines of the American Society of Hematology. Patients with the following conditions were excluded: (1) malignancy; (2) virus infection: detection of the human immunodeficiency virus (HIV), hepatitis B virus or hepatitis C virus; and (3) pregnancy.
2.2. Bleeding scores over time
Whole-blood samples collected into tubes, following informed consent, were used for the measurement of platelet counts. A total of 204 samples bleeding scores were assessed by IBLS and ITP-2016 at the time of diagnosis to analyze the relationship between bleeding score and platelet counts, gender, disease stage, treatment, also to evaluate consistency between two bleeding grading systems.
The specific scoring method is as follows:
IBLS [Citation9] (shown in )
ITP-2016 [Citation14,Citation15] (shown in )
2.3. Statistical analysis
Data analysis was performed with the Statistical Package (SPSS 22.0 Inc., Chicago, Illinois, USA). Spearman rank correlation was used to describe the relationship between bleeding score and platelet count. Specific as follows: −1 ≤ rs ≤ 1; positive correlation, rs > 0; negative correlation, rs < 0; irrelevant, rs = 0. The analysis of consistency of the two scores was by Kappa text. p-value less than 0.05 indicated a statistical significance.
3. Results
3.1. Patient characteristics
The demographics of patients are summarized in . Totally 204 patients with ITP were included. The patients were divided into the following groups: newly diagnosed ITP (within 3 months of diagnosis of ITP), persistent ITP (312 months after diagnosis of ITP), and chronic ITP (more than 12 months of PLT reduction).
Table 1. Patients’ characteristics.
3.2. Two bleeding systems scoring of these patients
The IBLS () and ITP-2016 () were used to evaluate bleeding. The correlation of bleeding score from two assessment systems with the platelet count was analyzed. The results show that there is a linear relationship between platelet count and bleeding score, no matter which scoring system it is based on. The bleeding score was significantly reduced as the increase of platelet count, with rs = −0.429, p < 0.001; rs = −0.331, p < 0.001, the analysis of the number of sites of Grade 1/2 bleeding were done respectively, and rs = −0.466, by ITP-2016, p < 0.05.
Table 2. IBLS scoring criteria.
Table 3. ITP-2016 scoring criteria.
Patients were divided into several groups depending on platelet count in units of 10*9/L, and their bleeding scores were analyzed sequentially. The results suggest that when the platelet count is below 10*109/L, the number of sites of Grade 2 bleeding and the ITP-2016 scores are negatively correlated with platelet counts (rs = −0.15 and rs = −0.244, p < 0.05, respectively). Significantly, there is no correlation between the two when the platelet count is more than 10*109/L (Tables and ).
Table 4. Patient characteristics and associations with IBLS.
Table 5. Patient characteristics and associations with ITP-2016.
3.3. Evaluation of consistency and time taking between two bleeding grading systems
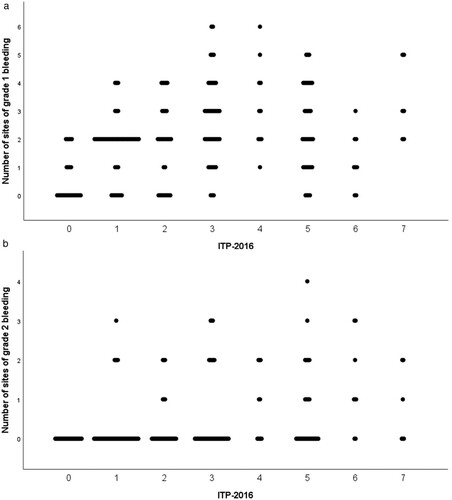
As for scoring tools, IBLS and ITP-2016 are applied for the different scoring details and situations. We evaluate the consistency of two bleeding grading systems. The results showed that the number of sites of Grade 1/2 bleeding was both positively correlated with the ITP-2016 score (rs = 0.357, p < 0.001, rs = 0.356, p < 0.001). ()
Figure 1. Correlation analysis of the IBLS and ITP-2016. The number of sites of Grade 1/2 bleeding was both positively correlated with the ITP-2016 score (rs = 0.357, p < 0.001; rs = 0.356, p < 0.001).
There was a significant difference in the time taking to score between ITP-2016 and IBLS (z = −3.825, p < 0.001). The ITP-2016 takes less time than the IBLS (2.3 [1–3] minutes vs. 6 [3–12] minutes).
4. Discussion
ITP is an autoimmune disease due to immune-mediated destruction of antilogous platelets and ineffective thrombopoiesis. Patients with low platelet counts are treated as increasing risk for serious bleeding. The decision to patients with ITP treatment should be guided by the bleeding scores and patient preferences, not only the low platelet counts. However, due to the lack of effective tools, the evaluation of the risk of bleeding and the curative effect assessment mainly depends on the PLT count in the real condition.
Patients with ITP and with a low PLT count may have minimal or no hemorrhage manifestations. Excessive pursuit of a normal PLT count requires long-term maintenance of drug treatment, resulting in unnecessary drug toxicity, side effects, and increased costs. Therefore, the goals of treatment are the control of bleeding manifestations instead of a single pursuit of the normal PLT count. However, predicting the risk of future bleeding among patients with ITP is challenging. Several scoring systems have been developed, but their clinical use is limited by their complexity and lack of validation in large studies or other reasons.
In this study, we retrospectively assessed the relationship between platelet count and bleeding score in Patients with ITP and found that platelet count and bleeding scores are negatively correlated when the platelet count is below 10*109/L. But when the platelet count is more than 10*109/L, there is no linear correlation between platelet count and bleeding scores. Several points may account for the mechanism. Changes in platelet function could be a big factor. One study found that bleeding severity is consistent with platelet function, not dependent on platelet count merely, which suggests that there is a mechanistic link between desensitization of agonist receptors and bleeding severity [Citation16]. Similar conclusions have been confirmed in other studies [Citation17,Citation18], which indicates that the discovery of a more comprehensive efficacy evaluation system of ITP would guide clinical management better.
IBLS and ITP-2016 were recommended by many specialists as existing commonly applied bleeding assessment tools, but their clinical applications were limited due to the long-term data collection.
A total of 204 patients with ITP were scored by IBLS and ITP-2016 scoring systems. The consistency analysis of platelet count and two bleeding systems indicates that both bleeding scales can reflect the severity of the bleeding and there is a negative correlation between the bleeding grade and platelet count, which can help assess disease more comprehensively. There is no correlation between platelet count and bleeding score when the platelet count is more than 10*109/L, which is consistent with the clinical observation and the results in the relevant literature. Piel-Julian M-L et al. [Citation19]. demonstrated a good correlation between platelet count and the occurrence of any bleeding and of mucosal bleeding at ITP diagnosis in adults. They selected and assessed 302 newly diagnosed ITP adults’ bleeding frequency. Platelet count thresholds were assessed by the use of receiver operating characteristic curves. They found that the best discriminant threshold of platelet count for any bleeding was 20*109/L. After multivariate analysis, factors associated with any bleeding were platelet counts of < 20*109/L and < 10*109/L. Notably, Frelinger AL et al. [Citation16] analyzed the correlation between immature platelet fraction, circulating and agonist-stimulated platelet surface P-selectin, and activated GPIIb–IIIa and GPIbα in patients with ITP, and the results indicated that platelet function in ITP, independent of platelet count, is consistent over time and is associated with both concurrent and subsequent bleeding severity, which supports further evaluation of platelet function testing to help guide patient management in ITP. Those similar findings have been confirmed previously [Citation20]. These findings support further evaluation of platelet function testing rather than platelet count to help guide patient management in ITP.
The correlation analysis of two bleeding systems shows that the number of sites of Grade 1/2 bleeding was both positively correlated with the ITP-2016 score. Different doctors have good consistency in the clinical application of these two scoring systems in patients with ITP, indicating that these two scoring systems can be used as effective tools for patient condition evaluations, risk assessments, and curative effect evaluations. The responsiveness analysis of two bleeding systems indicated that the PLT count increased and the risk of bleeding decreased significantly after the treatments compared with before the treatments, which prompts them to have good clinical responsiveness. Compared with the IBLS, the ITP-2016 system takes less time to score. While ITP-2016 with the characteristics of strong objectivity, high consistency, less time-consuming, and easy to grasp, it is beneficial to be applied in multi-center clinical trials.
Disclosure statement
The authors declare no conflict of interests.
Additional information
Funding
References
- Zhang L, Zhang M, Du X, et al. Safety and efficacy of eltrombopag plus pulsed dexamethasone as first-line therapy for immune thrombocytopenia. Br J Haematol. 2020;189(2):369–378.
- Rodeghiero F, Marranconi E. Management of immune thrombocytopenia in women: current standards and special considerations. Expert Rev Hematol. 2020;13(2):175–185.
- Mithoowani S, Cervi A, Shah N, et al. Management of major bleeds in patients with immune thrombocytopenia. J Thromb Haemost. 2020;18(7):1783–1790.
- Boulware R, Refaai MA. Why do patients with immune thrombocytopenia (ITP) experience lower bleeding events despite thrombocytopenia. Thromb Res. 2020;187:154–158.
- Portielje JE, Westendorp RG, Kluin-Nelemans HC, et al. Morbidity and mortality in adults with idiopathic thrombocytopenic purpura. Blood. 2001;97(9):2549–2554.
- Rodeghiero F, Stasi R, Gernsheimer T, et al. Standardization of terminology, definitions and outcome criteria in immune thrombocytopenic purpura of adults and children: report from an international working group. Blood. 2009;113(11):2386–2393.
- Frederiksen H, Maegbaek ML, Nørgaard M. Twenty-year mortality of adult patients with primary immune thrombocytopenia: a Danish population-based cohort study. Br J Haematol. 2014;166(2):260–267.
- Fogarty PF, Tarantino MD, Brainsky A, et al. Selective validation of the WHO bleeding scale in patients with chronic immune thrombocytopenia. Curr Med Res Opin. 2012;28(1):79–87.
- Page LK, Psaila B, Provan D, et al. The immune thrombocytopenic purpura (ITP) bleeding score: assessment of bleeding in patients with ITP. Br J Haematol. 2007;138(2):245–248.
- Khellaf M, Michel M, Schaeffer A, et al. Assessment of a therapeutic strategy for adults with severe autoimmune thrombocytopenic purpura based on a bleeding score rather than platelet count. Haematologica. 2005;90(6):829–832.
- Buchanan GR, Adix L. Grading of hemorrhage in children with idiopathic thrombocytopenic purpura. J Pediatr. 2002;141(5):683–688.
- Kumar M, Dutta S, Bhattyacharyya M. Application of ITP-BAT bleeding score in clinical practice. Int J Hematol. 2015;101(2):207–208.
- Thrombosis and Hemostasis Group, Hematology Society, Association CM. [Consensus of Chinese experts on diagnosis and treatment of adult primary immune thrombocytopenia (version 2016)]. Zhonghua Xue Ye Xue Za Zhi. 2016;37(2):89–93.
- Rodeghiero F, Michel M, Gernsheimer T, et al. Standardization of bleeding assessment in immune thrombocytopenia: report from the international working group. Blood. 2013;121(14):2596–2606.
- Zhao Y, Ni X, Xu P, et al. Interleukin-37 reduces inflammation and impairs phagocytosis of platelets in immune thrombocytopenia (ITP). Cytokine. 2020;125:154853.
- Frelinger AL 3rd, Grace RF, Gerrits AJ, et al. Platelet function in ITP, independent of platelet count, is consistent over time and is associated with both current and subsequent bleeding severity. Thromb Haemost. 2018;118(1):143–151.
- Hicks SM, Coupland LA, Jahangiri A, et al. Novel scientific approaches and future research directions in understanding ITP. Platelets. 2020;31(3):315–321.
- Huang J, Zeng B, Li X, et al. Comparative study of the clinical application of 2 bleeding grading systems for pregnant women with immune thrombocytopenia. Clin Appl Thromb Hemost. 2020;26:1076029620910790.
- Piel-Julian ML, Mahévas M, Germain J, et al. Risk factors for bleeding, including platelet count threshold, in newly diagnosed immune thrombocytopenia adults. J Thromb Haemost. 2018;16(9):1830–1842.
- Slichter SJ. Relationship between platelet count and bleeding risk in thrombocytopenic patients. Transfus Med Rev. 2004;18(3):153–167.
