ABSTRACT
Aim: To investigate the role of neutrophil CD64 in diagnosing infection in patients with haematological malignancies.
Methods:
The clinical data of 76 patients with haematological malignancies and infection who were treated in our department between January 2014 and October 2019 were retrospectively analysed. To evaluate the diagnostic value of some biomarkers, infection indexes such as white blood cell count (WBC), neutrophil count (NEUT), neutrophil CD64 and procalcitonin (PCT) were compared across the patients with confirmed infection status and infection-control status. Sensitivity, specificity and area under the receiver operating characteristic curve (AUC) were also determined.
Results:
The WBC and NEUT did not differ significantly, whereas the neutrophil CD64 and PCT levels were significantly elevated in patients with a confirmed infection status (p < 0.05), with sensitivity of 31.0%, 45.2%, 76.2% and 50%, respectively, and specificity of 90.5%, 69%, 71.4% and 64.3%, respectively. The AUC of WBC, NEUT, neutrophil CD64 and PCT was 0.528, 0.517, 0.844 and 0.599, respectively. Further highlighting their diagnostic value, the neutrophil CD64 and PCT levels in neutropenia patients were significantly upregulated in patients with infection status (p < 0.05) but the WBC and NEUT were unchanged, with sensitivity of 73.7%, 63.2%, 68% and 68.4%, respectively, and specificity of 68.4%, 52.6%, 57.9% and 63.2%, respectively. The AUC of neutrophil CD64, PCT, WBC and NEUT was 0.864, 0.593, 0.419 and 0.403, respectively.
Conclusion:
These results indicate that neutrophil CD64 is a promising biomarker with superior sensitivity and specificity for diagnosing infection in patients with haematological malignancies, especially neutropenia patients.
1. Introduction
Infections are common complications that can evolve into life-threatening diseases and increase the mortality of patients with haematological malignancies, whose immunity is already impaired either by the malignancy itself or by chemotherapy [Citation1,Citation2]. Therefore, the early diagnosis of infection and appropriate implementation of antibiotic treatments for these patients are crucial for maintaining their health and ensuring continuity of treatment. Blood cultures, which are regarded as clinical gold standards for the detection of infection, usually require 72 h before the confirmatory results are available, and the results can be confounded by antibiotic treatment. To bypass these limitations, we rely on biomarkers such as WBC, NEUT, PCT and CRP to detect infection as early as possible [Citation3,Citation4]. However, these markers appear to lack adequate predictive power, making the identification of biomarkers that can reliably diagnose infection essential [Citation4,Citation5].
Neutrophil CD64, which is a receptor for the Fc fragment of immunoglobulin G, is mainly distributed on the surface of macrophages, monocytes and dendritic cells [Citation3,Citation6,Citation7]. At resting state, the expression level is usually low, but it can sharply increase in the event of infection or tissue injury. This increase initiates the immune response to infection, which comprises the antibody-dependent cellular cytotoxicity (ADCC) reaction and the release of cytokines. Thus, neutrophil CD64 plays an essential role in mediating the immune response to infectious agents [Citation3,Citation5,Citation8]. Previous studies have demonstrated that neutrophil CD64 expression levels can be used as a biomarker for the diagnosis of sepsis (for adults, children and neonates) and post-operation infection and in distinguishing infection from immunological disease [Citation6,Citation7,Citation9–13]. However, its diagnostic value has not been clearly reported in patients with haematological malignancies, especially in neutropenia patients. We retrospectively reviewed clinical data from patients in our department and compared the diagnostic value of neutrophil CD64 with that of other established infection indexes (WBC, NEUT and PCT).
2. Materials and methods
2.1 Study design
Consecutive adult haematological malignancy patients with infection who were treated in our department between January 2014 and October 2019 were enrolled and their data were retrospectively analysed. The diagnoses of haematological malignancies were made in accordance with the NCCN Clinical Practice Guidelines in Haematology. The diagnoses of infections were made in accordance with the Regulatory Guidelines of Nosocomial Infection issued by the Department of Health of China. The infections identified in our study were sepsis, lower respiratory infection, skin and soft tissue infection, herpes virus infection and urinary infection (Supplementary Document 1). Blood samples for blood culture, blood routine examination, PCT and neutrophil CD64 measurements and infection testing were first collected when patients had a fever of >38.5°C. After the infection had been controlled, we again measured the infection index if the patient had gone without fever for five days, had a negative blood culture for sepsis or a negative culture from other non-blood sites, had recovered clinically or showed absorption of inflammation in lung computed tomography (CT) scans or X-rays (lower respiratory infection). Neutropenia was defined as having an absolute count of neutrophils <1.5*109/L. Anti-infective treatment was administered to neutropenia patients in accordance with the China guidelines for the clinical application of antibiotics to neutropenia patients with fever. Anti-infective treatment was administered to patients without neutropenia based on clinical severity and the anti-infective scheme used in our department, which was formulated based on an etiological investigation conducted in our hospital. Anti-neoplastic treatment was administered to patients based on the corresponding guidelines issued by Chinese Society of Clinical Oncology.
Patients were excluded if they were (1) <18 years old; (2) pregnant at any stage; (3) diagnosed with rheumatic disease or acquired immune deficiency syndrome or (4) had any organ dysfunction. Our study was approved by our hospital’s ethics committee, and written informed consent was obtained from either the patients or their legal surrogates.
2.2 WBC and NEUT
We collected 2 mL of peripheral venous blood from every participant and transferred it to an anticoagulant tube containing EDTA. WBC and NEUT were measured using a XN-9000 haematology analyser (Sysmex Corp).
2.3 PCT
We collected 2 mL of peripheral venous blood, which was stored at room temperature in an anticoagulant tube containing EDTA and then centrifuged at 3000 rpm for 10 min to obtain the liquid supernatant (plasma). The PCT level was tested using a VIDAS B.R.A.H.M kit (Biomerieux).
2.4 Neutrophil CD64
We collected 2 mL of peripheral venous blood and stored it in a blood collection tube containing EDTA. To remove the RBCs, we added 500 μL of RBC lysis buffer (Thermo Fisher Scientific) to 50 μL of the peripheral blood sample and then incubated the mixture at room temperature. After centrifuging and washing the mixture with PBS thrice, it was incubated with 2 μg/mL of phycoerythrin (PE)-conjugated anti-CD64 antibody (BD Biosciences) and 2 μg/mL of peridinin chlorophyll protein (Percp)-conjugated anti-CD45 antibody (BD Biosciences) on ice for 40 min in the dark. The sample was then washed with PBS twice and re-suspended in 300 μL PBS before being loaded onto a Beckman Coulter Epics XL flow cytometer (Beckman Coulter Inc.). EXPO32 software (Beckman Coulter Inc.) was used to analyse the data. The reference range of neutrophil CD64 was determined by testing 100 healthy people. We analysed at least 5000 neutrophils from every blood sample to guarantee the accuracy and reliability of the result.
2.5 Statistical analysis
Statistical analyses were performed using SPSS v18.0 (SPSS Inc., Chicago, IL, USA). Based on normality, variables are presented either as mean ± standard deviation or as median with range based on their normality. The levels of the infection indexes were compared using either Student’s t-test or Wilcoxon rank-sum test. ROC curve analysis was conducted to evaluate the performance of the infection biomarkers (WBC, NEU, neutrophil CD64 and PCT). The AUC was calculated from the ROC curve. The sensitivity, specificity and threshold were determined using Youden’s index. Two-sided p < 0.05 was deemed to indicate a statistically significant difference.
3. Results
3.1 Clinical characteristics
Seventy-six consecutive patients were eligible for enrolment in our study. presents the information of the patients, such as their median age, gender, haematological diseases and infection type.
Table 1. Patients’ baseline characteristics.
3.2 Diagnostic value of various infection indexes
Patients with a confirmed infection status showed significantly higher levels of neutrophil CD64 and PCT than their infection-control status counterparts (p < 0.05). There was no difference in the levels of WBC and NEUT between the two groups (). At cut-off values of 2.72 and 0.2, neutrophil CD64 and PCT had a sensitivity of 76.2% and 50%, respectively, and specificity of 71.4% and 64.3%, respectively ().
Table 2. Index in patients’infection and infection-control status.
Table 3. Cut-off value of infection index.
3.3 ROC curve and AUC of various infection indexes
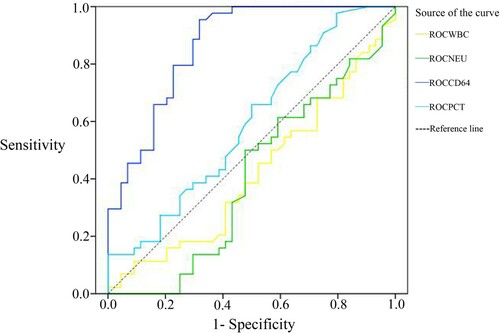
The ROC curves of each biomarker were determined to calculate the AUC and examine their predictive values. The ROC curves for each biomarker are shown in . The AUC for WBC, NEUT, CD64 and PCT was 0.528 (95% CI 0.435–0.621), 0.517 (95% CI 0.424–0.609), 0.844 (95% CI 0.783–0.905) and 0.599 (0.509–0.689), respectively. The AUC of neutrophil CD64 was the largest, reflecting its superior sensitivity and specificity and excellent performance in diagnosing infection.
3.4 Subgroup analysis
Based on the neutrophil count, patients were further classified into a neutropenia subgroup (n = 44). Consistent with the measurements from the whole group, their neutrophil CD64 and PCT levels were also elevated significantly in the neutropenia patients with a confirmed infection status (p < 0.05). However, but the WBC or and NEUT levels remained unchanged (). At cut-off values of 3.60 and 0.19, neutrophil CD64 and PCT had a sensitivity of 73.7%, and 63.2%, respectively, and specificity of 68.4% and, 52.6%, respectively ().
Table 4. Index in neutropenia patients’infection and infection-control status.
Table 5. Cut-off value of infection index in neutropenia group.
3.5 ROC curve and AUC of each infection index in the neutropenia group
Moreover, neutrophil CD64 also appeared to have had the greatest predictive power as its AUC was the largest among of the detected biomarkers (shown in ). The AUC for WBC, NEUT, CD64 and PCT was 0.419 (95% CI 0.299–0.538), 0.403 (95% CI 0.283–0.523), 0.864 (95% CI 0.789–0.939) and 0.593 (0.474–0.712), respectively. Consequently, the AUC of neutrophil CD64 was also the largest in the neutropenia patient group, demonstrating the superiority of its diagnostic value over that of other biomarkers, irrespective of the association with neutropenia.
4. Discussion
In recent years, the serious infection has developed into a major problem in the treatment of patients with haematological malignancies, as their immunity is weakened not only by the disease itself but also by chemotherapy. Infections lower the quality of life, delays therapy interval times and increases mortality [Citation7,Citation14]. Therefore, it is crucial to monitor, prevent and cure infection while managing haematological malignancies to ensure patient safety and the highest possible adherence to the treatment schedule.
Neutrophil CD64, a membrane glycoprotein encoded by a gene on chromosome one, plays a crucial role in the immune response to infection as it is a transfer signal and mediates cytotoxicity and phagocytosis [Citation3, Citation5]. Neutrophil CD64 is usually expressed at a low level in healthy hosts and is elevated in response to inflammatory stimulation and injury. Elevation in the levels of neutrophil CD64 is not correlated with sex or age [Citation16]. Emerging evidence indicates that neutrophil CD64 is a promising marker for the diagnosis of sepsis, identification of infection and autoimmune diseases and prediction of mortality in patients in intensive care units [Citation6,Citation11,Citation17–19]. Its diagnostic value, however, has not been clearly reported in patients with haematological malignancies, especially in neutropenia patients. Our current study retrospectively analysed the data of 76 patients from the haematology department of our hospital to evaluate the diagnostic performance of some clinical biomarkers. Our study indicated that the neutrophil CD64 and PCT levels were significantly elevated in patients with confirmed infection status, with relatively superior sensitivity (76.2% and 50%, respectively) and specificity (71.4% and 64.3%, respectively), unlike WBC and NEUT levels. The AUC of neutrophil CD64 and PCT was 0.844 (95% CI 0.783–0.905) and 0.599 (95%CI 0.509–0.689), respectively. ROC is a comprehensive index that reflects the sensitivity and specificity of the medical test and is used to calculate the AUC. The larger the AUC, the better the diagnostic value of the test or index. The ROC curve showed that neutrophil CD64 had the largest AUC compared with other tested biomarkers. When we further analysed the subgroup of neutropenic patients, consistent with the measurements from the whole group, the neutrophil CD64 and PCT levels were significantly elevated in patients with a confirmed infection status (p < 0.05). We also found that neutrophil CD64 had the greatest power for diagnosing infection compared with PCT, WBC and NEUT, the highest sensitivity and specificity (73.7% and 68.4%, respectively) and the largest AUC (0.864, 95% CI 0.789–0.939). The diagnostic performance of neutrophil CD64 was much better than that of WBC, NEUT and PCT, which is consistent with previous reports on the utility of neutrophil CD64 in diagnosing infection in other patient groups [Citation4,Citation7,Citation9–11,Citation16,Citation17]. Generally, our results suggest that neutrophil CD64 has superior value in diagnosing infection in patients with haematological malignancies, including in neutropenic patients.
The upregulation of neutrophil CD64 occurs in the context of inflammation and injury. Neutrophil CD64 can be stimulated by tumour necrosis factor-α, interferon-γ and lipopolysaccharides, but elevated neutrophil CD64 levels are not associated with sex, age or the count of WBC. Such elevations can occur as early as 5 h after infection [Citation6]. WBC and NEUT are markers that have been traditionally used for detecting and monitoring infection. However, in many cases of serious infection, WBC can either increase, remain normal or even decrease. The AUC of WBC for diagnosing infection or sepsis has been reported to range from 0.49 to 0.6, indicating unsatisfactory diagnostic performance [Citation3,Citation15]. CRP is an acute-phase protein that can be stimulated by inflammatory reactions within 4–6 h of infection. However, CRP has relatively inferior specificity as it can also be stimulated by stress, immunological diseases, myocardial infarction and tumour proliferation [Citation3,Citation20]. PCT is a glycoprotein whose levels are elevated 3–6 h after infection and has been shown to have moderate specificity [Citation21,Citation22]. In our study, the diagnostic performance of WBC, NEUT and PCT were similar to that reported previously. Nevertheless, patients with haematological malignancies, especially febrile patients with neutropenia, constitute a special group who are at high risk of acquiring infection and developing sepsis. The nature of haematological diseases and abnormal WBC in these patients mark neutrophil CD64 as a potential biomarker for effectively diagnosing and monitoring infection in such patients. Our study primarily investigated the value of neutrophil CD64 in diagnosing infection in patients with haematological malignancies, especially in the neutropenic group. Nevertheless, the results of our study should be considered to be preliminary due to its limitations. Specifically, owing to the retrospective nature of the study and the relatively small sample, our findings must be re-interpreted in a larger cohort to affirm the diagnostic value of neutrophil CD64 and avoid overestimation.
5. Conclusions
Our study suggests that neutrophil CD64 is a potential biomarker for the early diagnosis of infection in patients with haematological malignancies owing to its relatively superior sensitivity, specificity and AUC. Its diagnostic value remains superior for neutropenia patients as well.
Supplemental Material
Download MS Word (28 KB)Acknowledgements
Data acquisition was performed by all the authors. We acknowledge the contribution of Jiayu Xu and Xiuqu Mai for their work in the Hospital’s Haematology Laboratory and Lu You for conducting the statistical analysis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Comolli G, Torchio M, Lenta E, et al. Neutrophil CD64 expression: a reliable diagnostic marker of infection in advanced cancer patients? New Microbiol. 2015;38(3):427–430.
- Icardi M, Erickson Y, Kilborn S, et al. CD64 index provides simple and predictive testing for detection and monitoring of sepsis and bacterial infection in hospital patients. J Clin Microbiol. 2009;47(12):3914–3919.
- Hoffmann JJ. Neutrophil CD64: a diagnostic marker for infection and sepsis. Clin Chem Lab Med. 2009;47(8):903–916.
- Yeh CF, Wu CC, Liu SH, et al. Comparison of the accuracy of neutrophil CD64, procalcitonin, and C-reactive protein for sepsis identification: a systematic review and meta-analysis. Ann Intensive Care. 2019;9(1):5.
- Daryapeyma A, Pedersen G, Laxdal E, et al. Neutrophil CD64 as a marker for postoperative infection: a pilot study. Eur J Vasc Endovasc Surg. 2009;38(1):100–103.
- Chen Q, Shi J, Fei A, et al. Neutrophil CD64 expression is a predictor of mortality for patients in the intensive care unit. Int J Clin Exp Pathol. 2014;7(11):7806–7813.
- de Jong E, de Lange DW, Beishuizen A, et al. Neutrophil CD64 expression as a longitudinal biomarker for severe disease and acute infection in critically ill patients. Int J Lab Hematol. 2016;38(5):576–584.
- Shang YX, Cui JY, Ren XX, et al. [Improvement of method for detecting peripheral blood neutrophil CD64 index in patients with hematologic malignancies]. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2019;27(4):1291–1296.
- Kipfmueller F, Schneider J, Prusseit J, et al. Role of neutrophil CD64 index as a screening marker for late-onset sepsis in very Low birth weight infants. PLoS One. 2015;10(4):e0124634.
- Du J, Li L, Dou Y, et al. Diagnostic utility of neutrophil CD64 as a marker for early-onset sepsis in preterm neonates. PLoS One. 2014;9(7):e102647.
- Hu BQ, Yang Y, Zhao CJ, et al. Accuracy of neutrophil CD64 expression in diagnosing infection in patients with autoimmune diseases: a meta-analysis. Clin Rheumatol. 2019;38(5):1319–1328.
- Dal Ponte ST , Alegretti AP, Pilger D, et al. Diagnostic accuracy of CD64 for sepsis in emergency department. J Glob Infect Dis. 2018;10(2):42–46.
- Ajmani S, Singh H, Chaturvedi S, et al. Utility of neutrophil CD64 and serum TREM-1 in distinguishing bacterial infection from disease flare in SLE and ANCA-associated vasculitis. Clin Rheumatol. 2019;38(4):997–1005.
- Xiong SD, Pu LF, Wang HP, et al. Neutrophil CD64 index as a superior biomarker for early diagnosis of infection in febrile patients in the hematology department. Clin Chem Lab Med. 2017;55(1):82–90.
- Hoffmann JJ. Neutrophil CD64 as a sepsis biomarker. Biochem Med (Zagreb). 2011;21(3):282–290.
- Ye Z, Zou H, Liu S, et al. Diagnostic performance of neutrophil CD64 index in patients with sepsis in the intensive care unit. J Int Med Res. 2019;47(9):4304–4311.
- Wang X, Li ZY, Zeng L, et al. Neutrophil CD64 expression as a diagnostic marker for sepsis in adult patients: a meta-analysis. Crit Care. 2015;19:245.
- Feng M, Zhang SL, Liang ZJ, et al. Peripheral neutrophil CD64 index combined with complement, CRP, WBC count and B cells improves the ability of diagnosing bacterial infection in SLE. Lupus. 2019;28(3):304–316.
- Wan S, Han X, Zhao H, et al. Neutrophil CD64 serves as a sensitive and reliable biomarker for the diagnosis of bacterial infection in hematological disorders. J Infect. 2015;70(5):543–545.
- Povoa P, Coelho L., Almeida E, et al. C-reactive protein as a marker of infection in critically ill patients. Clin Microbiol Infect. 2005;11(2):101–108.
- Maruna P, Nedelnikova K, Gurlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000;49(Suppl 1):S57–S61.
- Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008;36(3):941–952.