ABSTRACT
Objectives
Autologous hematopoietic stem cell transplantation (ASCT) is a crucial method used in patients with multiple myeloma (MM). This study aims to evaluate the role of ASCT in immunoglobulin (Ig) reconstitution and long-term outcomes in patients aged ≥ 60 years.
Methods
From March 2008 to May 2019, 93 patients aged ≥ 60 years who were diagnosed with MM and underwent ASCT were retrospectively analyzed. All patients underwent follow-ups and the deadline for follow-up was October 31, 2022. The Ig levels were measured using the immune turbidimetry method at 3, 6, and 12 months after transplantation. Patients who died or experienced relapse were excluded from the analysis. The prognostic value of Ig levels was estimated using the Kaplan-Meier survival curve and Cox regression method.
Results
No patients died, and all patients with complications showed improvements after treatment. Patients in the Ig reconstitution group had a lower international staging system (ISS) stage, whereas those in the immunoparesis group had a higher ISS stage. The median duration of follow-up was 36 (range, 13–120) months. The Ig reconstitution within 12 months indicated a longer overall survival and progression-free survival outcomes. The detection of Ig levels was an independent indicator for the prognosis of MM.
Discussion and conclusion
The Ig reconstitution within 12 months of ASCT could predict the overall outcomes of patients with MM aged ≥ 60 years.
Introduction
Multiple myeloma (MM) is a neoplasm characterized by the excessive proliferation of malignant plasma cells that produces monoclonal immunoglobulins (Igs), leading to the invasion and destruction of adjacent bone tissue [Citation1]. This disease is more common, especially in those aged above 40 years old [Citation2,Citation3]. MM accounts for approximately 10% of hematological tumors [Citation4]. While the exact cause of MM is unknown, it is believed to involve chromosomes, genes, radiation, and chemicals are involved [Citation5]. Common clinical manifestations of MM include osteolytic lesions causing fractures, renal insufficiency, hypercalcemia, anemia, and susceptibility to repeated infections [Citation6]. The early symptoms of MM are hidden, leading to potential misdiagnosis and resulting in many patients being diagnosed at an advanced stage. Despite significant progress in diagnosis and targeted therapies for MM, the prognosis remains poor [Citation7]. There are still no known curative methods for this disease, and MM is associated with a high rate of disease recurrence [Citation8]. Therefore, identifying targets associated with the progression of MM has become a critical focus of research.
The treatment of MM constitutes conventional chemotherapy, radiation therapy targeted at specific symptomatic areas, and targeted drug therapy. The advancement of hematopoietic stem cell transplantation (HSCT) has provided hope for the treatment of hematological tumors, including leukemia, lymphoma, and myeloma, as well as other hematological diseases such as primary immunodeficiency and spinal cord dysplasia. Determining the upper age limit for HSCT qualification remains controversial. However, it is generally believed that the biological age of the recipient is more important than their actual age [Citation9]. Autologous stem cell transplantation (ASCT) is considered the standard treatment for patients with MM, and the development of other novel agents has further solidified its central role in MM care [Citation10,Citation11]. Therefore, it is essential to focus on indicators related to the progression of patients with MM after ASCT.
In the present study, we focused on the significance of ASCT in older patients with MM and analyzed its impact on long-term survival prognosis and Ig reconstitution. A total of 93 patients with MM who underwent ASCT between 2008 and 2019 were included in this study, and their clinical characteristics were recorded. Patients who experienced disease progression or died within 12 months after ASCT were excluded from the study, and the remaining patients were categorized into two groups based on their polyclonal Ig levels after 12 months of ASCT: the Ig reconstitution group and the immunoparesis group. The Kaplan-Meier (K-M) curve was plotted to estimate the overall survival (OS) outcome and the progression-free survival (PFS) outcomes. Furthermore, Cox regression analysis was conducted to identify and explore the prognostic factors relevant to MM in the context of ASCT.
Materials and methods
Recruitment of participants who underwent ASCT
The study included 93 patients with MM who underwent ASCT at The First People's Hospital of Chenzhou from March 2008 to May 2019. The inclusion criteria for the study were as follows: patients aged 60 years old or above, patients diagnosed with MM for the first time, those who received only one transplant, patients with complete clinical data and doctor's advice records available, and patients who signed a written informed consent form. The diagnostic criteria for MM were based on the International Myeloma Working Group (IMWG) guideline updated in 2014 [Citation12]. Patients were excluded from the study if they had received previous treatment for MM; had a history of cardiovascular disease, severe liver dysfunction, or other malignant tumors; or were unable to cooperate with the treatment. All the protocols and designs of this investigation were approved by the ethics committee of The First People's Hospital of Chenzhou. All patients were assessed and deemed eligible for ASCT by the therapist before undergoing transplantation.
Specific cytogenetic abnormalities, including translocation t (4;14), t (14;16), and/or deletion 17p, were considered as high-risk factors [Citation13]. Patients who exhibited these cytogenetic abnormalities were categorized as high-risk patients, whereas those without these risk factors were defined as standard-risk patients. Immunoparesis was defined as a condition in which the levels of at least two uninvolved polyclonal Igs were below the lower limit of the normal range, specifically, IgG levels < 7 g/L, IgM levels < 0.4 g/L, and IgA levels < 0.7 g/L.
Management methods for patients with MM
The treatment procedures mainly included induction therapy before transplantation, mobilization for hematopoietic cells, collection and preservation of these cells, pre-treatment, and cell reinfusion.
For patients newly diagnosed with MM, the induction therapy consisted of various drugs targeting the disease, such as proteasome inhibitors, immunomodulators, cytotoxic drugs, and glucocorticoids. Specifically, 8 patients received the PAD regimen (bortezomib, adriamycin, and dexamethasone), 27 patients received VD therapy (dexamethasone and bortezomib), 23 patients received VCD (dexamethasone, bortezomib, and cyclophosphamide), 6 patients received VTD regimen (bortezomib, thalidomide, and dexamethasone), 5 patients received TAD regimen (thalidomide, doxorubicin, dexamethasone), and 10 received TCD regimen (thalidomide, cyclophosphamide, and dexamethasone), and 14 patients were treated with DCEP ± V/T (cisplatin, cyclophosphamide, etoposide, dexamethasone, bortezomib or thalidomide).
The mobilization scheme used in this study involved chemotherapy combined with granulocyte colony-stimulating factor (G-CSF). Specifically, patients were treated with a high-dose cyclophosphamide regimen (3.0 g/m2). Subsequently, subcutaneous injections of G-CSF (5 µg/kg) were administered for 5–14 days. The collection of autologous peripheral blood hematopoietic stem cells was initiated when certain criteria were met: peripheral blood leukocyte count was over 5.0 × 109 /L, the platelet count was higher than 50 × 109/L, and peripheral blood CD34 + cells count acuity was over 2.0 × 106 /kg. The collection was conducted using a cell separator (Fresenius Kabi, Bad Homburg, Germany) and was carried out continuously 1–3 times; the collected cells were preserved by freezing them in 5% dimethyl sulfoxide at −80°C.
During the ASCT procedure, all patients received a high-dose chemotherapy (HDT) conditioning regimen based on oral or intravenous melphalan. Following the administration of the conditioning regimen, autologous peripheral blood stem cell infusion was performed one day after drug withdrawal. To prepare for the infusion, frozen blood bags containing peripheral stem cells were thawed in water at 37°C to 40°C. After resuscitation, the thawed stem cells were infused back into the patient through a central venous catheter within 30 min. Vital signs and adverse reactions were monitored throughout this procedure to ensure the safety and well-being of the patients.
Detection of polyclonal Ig
In this experiment, immune turbidimetry was used to determine the levels of polyclonal Ig at 3, 6, and 12 months after transplantation. The kits were purchased from MLBIO (Shanghai, China). The determination of Ig level excluded those patients who relapsed or died, so as to exclude the influence of recurrence on Ig levels.
Follow-up
All patients were followed up by outpatient service visits, hospitalizations, or telephonic communication. The deadline for the follow-up period was October 31, 2022. The main endpoints of the study were PFS and OS after treatment. PFS was defined as the time elapsed from the date of ASCT to disease progression, patient death, or the end of the follow-up period. OS was defined as the time from the date of ASCT to the death of the patient or the end of follow-up. According to the evaluation criteria of the IMWG, patients were judged to be in complete remission, very good partial remission, partial remission, stable condition, and progressive condition [Citation14].
Statistical analysis
The statistical software SPSS version 22.0 (IBM, Armonk, NY, USA) was used to analyze the data. After the normality test and variance homogeneity test, the eligible measurement data were compared by the independent sample T-test. The counting data were expressed as the number of cases and percentage, and the χ2 was adopted. The probability of OS and relapse in patients within 12 months was evaluated by the milestone method. Specific milestones were set at 3, 6, and 12 months after ASCT to assess the corresponding outcomes. The K-M survival curve was used for survival analysis, and Cox regression analysis was used for multivariate risk analysis. P < 0.05 was statistically significant.
Results
Basic characteristics of patients with MM
Among the 93 patients with MM, the basic information of the patients in the ASCT group was shown in . The median age of all MM patients was 65.0 (range, 60.0–74.0) years. The group consisted of 55 men and 38 women, and among them, there were 46 cases of IgG type, 20 cases of IgA type, 16 cases of light chain type, and 11 cases of other types. Based on the ISS, there were 32 cases in stage І, 29 cases in stage Ⅱ, and 32 cases in stage Ⅲ. According to the Eastern Cooperative Oncology Group (ECOG) performance status, 83 patients scored 0, and 10 patients scored 1. Patients were divided into a high-risk group (n = 20) and a standard-risk group (n = 73) as per their cytogenetic risk. The Charlson score for 82 patients was < 2, whereas for the remaining patients, it was >2. The median levels of lactate dehydrogenase (LDH), hemoglobin (HGB), serum creatinine (sCR), and serum calcium (sCa) were 207 U/L, 102 g/L, 171 µmol/L, and 2.32 mmol/L, respectively.
Table 1. Clinical information in elderly patients with MM.
Incidence of complications during transplantation
Among the 93, 35 patients developed fever and infections within one week after hematopoietic stem cell infusion. However, these symptoms were improved after anti-infection and physical antipyretic treatments. All patients experienced different degrees of alopecia and gastrointestinal adverse reactions, but no liver function damage was reported. After the treatment to protect the gastric mucosa, enhancing antiemetic therapy, and providing necessary blood transfusions, all patients showed improvements in their condition. No patient died due to transplantation.
Factors influencing of Ig reconstitution
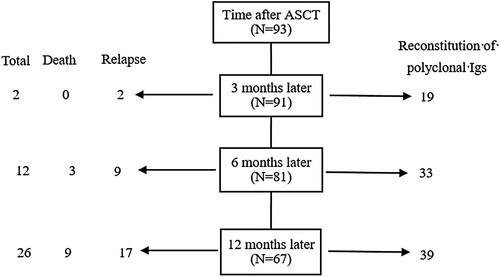
The prognostic outcomes within 12 months and the information related to Ig detection were shown in . Among the 93 patients, 2 experienced relapse after transplantation, and no deaths were reported within the first three months after transplantation. Within 6 months, three patients had died and nine patients had experienced disease relapse. At 12 months, 17 patients had experienced relapse and 9 patients had died. With regard to Ig detection, at three months after transplantation, Ig levels returned to normal in 19 out of 91 evaluable patients, whereas 72 patients still showed abnormal Ig levels. Subsequently, at 6 months, the Ig levels of Ig in 33 patients returned to normal, and 39 patients had normal Ig levels by 12 months. The above results of Igs levels suggested that the proportion of patients with Igs recovery increased over time after ASCT in evaluable patients.
According to the Ig levels, 39 patients with normal Ig levels were included in the Ig reconstitution group, and the remaining 28 patients with unrecovered Igs levels were included in the immunoparesis group. On comparing the clinical characteristics of patients, there was no significant difference in the age, gender, myeloma subtype, ECOG score, cytogenetic risk, and Charlson score between the Ig reconstitution and the immunoparesis group (P > 0.05, ). Patients in the Ig reconstitution group had lower ISS stages than patients in the immunoparesis group (P = 0.025, ). Furthermore, in the immunoparesis group, the levels of LDH, sCR, and sCa were increased and the level of HGB was decreased (all P < 0.05, ).
Table 2. Comparison of clinical indicators between Ig reconstitution group and Immunoparesis group.
Survival analysis and related indicators
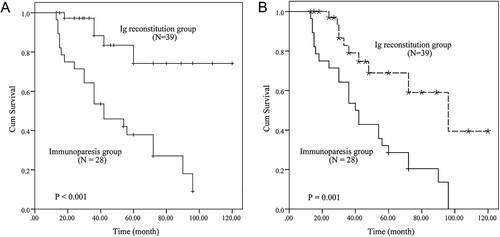
No patients were lost during the follow-up period. Among the 93 patients, 26 died, 8 of whom died of lung infection and 18 died of disease progression. Thirty-five patients experienced disease recurrence. The K-M curve was plotted using the clinical data of the Ig reconstitution and the immunoparesis group. As shown in A, the OS of the Ig reconstitution group was prolonged compared to the immunoparesis group, indicating that Ig reconstitution was associated with a more favorable long-term overall outcome (P < 0.001). The patient in the immunoparesis group showed a comparably unfavorable PFS outcome relative to those in the Ig reconstitution group, indicating that the Igs levels might be a prognostic variable for PFS (P = 0.001, B).
Figure 2. The predictive roles of Ig. (A) The K-M curve was plotted to analyze the OS outcome. (B) Patients in the immunoparesis group had poor PFS outcomes.
Cox analysis was used to construct a statistical model, with prognosis as the dependent variable and clinical indicators as the dependent variables. Cox multivariate regression analysis showed that ISS stage and Ig reconstitution were independent risk factors for the survival prognosis of patients with MM (P < 0.05, ).
Table 3. Cox analysis of independent indicators for prognosing long-term outcome.
Discussion
Many studies believe that sequential ASCT with high-dose chemotherapy is still the preferred treatment for MM patients aged under 65 years old who can tolerate strong chemotherapy [Citation15,Citation16]. However, despite the rapid development of ASCT has developed rapidly in clinical trials and practice, there is a lack of sufficient data on older patients, leaving clinicians with limited guidance in managing this age group effectively. Moreover, the number of cases of MM in the elderly population increased significantly, and the median age of MM increased from 70 to 74 [Citation17]. Therefore, it is urgent to collect and study the treatment data, specifically focusing on ASCT in older patients with MM.
One of the main concerns regarding ASCT for elderly patients is the potential for serious complications. Increased researchers pay attention to the ASCT treatment on elderly patients [Citation18,Citation19]. In cases where elderly patients are in good physical condition without serious complications, the upper age limit for ASCT can be extended to 75 years [Citation20]. In the present study, no patients died during the ASCT procedure and any complications that arose improved after corresponding treatments.
Polyclonal immunoglobulin refers to a mixture of monoclonal antibodies produced after being stimulated by multiple pathogens [Citation21]. A variety of protective antibodies are produced by the multiple B cells [Citation22]. MM is usually accompanied by a decrease in immunoglobulin levels, which leads to a higher risk of infection and mortality [Citation23]. This decline is attributed to the aberrant proliferation of plasma cells and the excessive secretion of monoclonal Igs, which suppresses the synthesis of normal polyclonal Igs [Citation24]. This study retrospectively collected data from older patients with MM and analyzed the levels of Ig reconstitution after ASCT. A total of 93 patients with MM were included, and 39 out of 67 patients with MM achieved normal Igs levels 12 months after ASCT. The results of Igs detection within 12 months after ASCT indicated that Ig reconstitution had occurred in more than half of the patients. Furthermore, a comparison of clinical characteristics between the Ig reconstitution group and the immunoparesis group revealed that the only discrepant factor was the ISS stage. This result documented that patients with lower ISS grades were more likely to experience immune reconstruction.
The preservation of uninvolved Igs in patients newly diagnosed patients with MM is correlated with the progression of MM and it can predict the OS outcomes of MM [Citation25]. Low expression of uninvolved Igs is related to poor clinical status and short PFS, making it an independent risk factor for screening the prognosis of patients with MM [Citation26]. In the current observation, we estimated the Ig levels in older patients with MM. The prognostic analysis documented that patients with Ig reconstitution had prolonged OS and PFS, indicating that the recovery of Igs could serve as a predictor for the prognosis of patients with MM. The Cox regression method also reflected that Ig constitution and ISS stage were independent indicators of outcomes of patients with MM. However, the sample size of this study was relatively small, and only fewer indicators were included. Therefore, further research with a larger sample size, increased clinical indicators, and long-term follow-up is necessary to certify the current results and identify more valuable prognostic biomarkers.
In a word, the percentage of Igs reconstitution increased within 12 months after ASCT. The patients with Ig reconstitution had lower ISS stages. Ig reconstitution after 12 months of ASCT was associated with prolonged OS and PFS.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Brigle K, Rogers B. Pathobiology and diagnosis of multiple myeloma. Semin Oncol Nurs. 2017 Aug;33(3):225–236. doi:10.1016/j.soncn.2017.05.012
- Mikulski D, Robak P, Perdas E, et al. Pretreatment serum levels of IL-1 receptor antagonist and IL-4 are predictors of overall survival in multiple myeloma patients treated with bortezomib. J Clin Med. 2021 Dec 26;11(1). doi:10.3390/jcm11010112
- Tagliafico AS, Dominietto A, Belgioia L, et al. Quantitative imaging and radiomics in multiple myeloma: a potential opportunity? Medicina (Kaunas, Lithuania). 2021 Jan 21;57(2):94), doi:10.3390/medicina57020094.
- Zhao Y, Peng H. The role of N(6)-methyladenosine (m(6)A) methylation modifications in hematological malignancies. Cancers. 2022 Jan 11;14(2). doi:10.3390/cancers14020332
- Rinaldi I, Muthalib A, Edina BC, et al. Role of anti-B-cell maturation antigen (BCMA) in the management of multiple myeloma. Cancers. 2022 Jul 19;14(14). doi:10.3390/cancers14143507
- Rafae A, Malik MN, Abu Zar M, et al. An overview of light chain multiple myeloma: clinical characteristics and rarities, management strategies, and disease monitoring. Cureus. 2018 Aug 15;10(8):e3148.
- Rajkumar SV. Multiple myeloma: every year a new standard? Hematol Oncol. 2019 Jun;37 Suppl 1(Suppl 1):62–65. doi:10.1002/hon.2586
- Xiang RF, Wang Y, Zhang N, et al. MK2206 enhances the cytocidal effects of bufalin in multiple myeloma by inhibiting the AKT/mTOR pathway. Cell Death Dis. 2017 May 11;8(5):e2776. doi:10.1038/cddis.2017.188
- Bazinet A, Popradi G. A general practitioner's guide to hematopoietic stem-cell transplantation. Curr Oncol. 2019 Jun;26(3):187–191. doi:10.3747/co.26.5033
- Al Hamed R, Bazarbachi AH, Malard F, et al. Current status of autologous stem cell transplantation for multiple myeloma. Blood Cancer J. 2019 Apr 8;9(4):44. doi:10.1038/s41408-019-0205-9
- Goel U, Usmani S, Kumar S. Current approaches to management of newly diagnosed multiple myeloma. Am J Hematol. 2022 May;97(Suppl 1):S3–s25.
- Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014 Nov;15(12):e538–e548. doi:10.1016/S1470-2045(14)70442-5
- 中国医师协会血液科医师分会, 中华医学会血液学分会, 中国医师协会多发性骨髓瘤专业委员会. 中国多发性骨髓瘤诊治指南(2020年修订). 中华内科杂志 2020年59卷5期 341–346页 MEDLINE ISTIC PKU CSCD CA. 2021.
- Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia. 2009 Jan;23(1):3–9. doi:10.1038/leu.2008.291
- Gao F, Lin MS, You JS, et al. Long-term outcomes of busulfan plus melphalan-based versus melphalan 200 mg/m(2) conditioning regimens for autologous hematopoietic stem cell transplantation in patients with multiple myeloma: a systematic review and meta-analysis. Cancer Cell Int. 2021 Nov 10;21(1):601. doi:10.1186/s12935-021-02313-z
- Cho HJ, Jung SH, Jo JC, et al. Development of a new risk stratification system for patients with newly diagnosed multiple myeloma using R-ISS and (18)F-FDG PET/CT. Blood Cancer J. 2021 Dec 1;11(12):190. doi:10.1038/s41408-021-00577-2
- Turesson I, Velez R, Kristinsson SY, et al. Patterns of multiple myeloma during the past 5 decades: stable incidence rates for all age groups in the population but rapidly changing age distribution in the clinic. Mayo Clin Proc. 2010 Mar;85(3):225–230. doi:10.4065/mcp.2009.0426
- Sanchez L, Sylvester M, Parrondo R, et al. In-Hospital mortality and post-transplantation complications in elderly multiple myeloma patients undergoing autologous hematopoietic stem cell transplantation: A population-based study. Biol Blood Marrow Tr: J Am Soc Blood Marrow Tr. 2017 Jul;23(7):1203–1207. doi:10.1016/j.bbmt.2017.03.012
- González-Barrera S, Martín-Sánchez G, Parra-Jordán JJ, et al. Feasibility of a hospital-at-home program for autologous hematopoietic stem cell transplantation. Transplant Cell Ther. 2023 Feb;29(2):111.e1–111.e7. doi:10.1016/j.jtct.2022.11.018
- Rajkumar SV, Kumar S. Multiple myeloma: diagnosis and treatment. Mayo Clin Proc. 2016 Jan;91(1):101–119. doi:10.1016/j.mayocp.2015.11.007
- Lu J, Ding J, Liu Z, et al. Retrospective analysis of the preparation and application of immunotherapy in cancer treatment (Review). Int J Oncol. 2022 Feb;60(2).
- Duan Z, Baughn LB, Wang X, et al. Role of Dot1L and H3K79 methylation in regulating somatic hypermutation of immunoglobulin genes. Proc Natl Acad Sci U S A. 2021 Jul 20;118(29):e2104013118.doi:10.1073/pnas.2104013118.
- Vacca A, Melaccio A, Sportelli A, et al. Subcutaneous immunoglobulins in patients with multiple myeloma and secondary hypogammaglobulinemia: a randomized trial. Clin Immun (Orlando, Fla). 2018 Jun;191:110–115. doi:10.1016/j.clim.2017.11.014
- Amjad MA, Hamid Z, Ramakrishna S, et al. Myelomatous pleural effusion: a rare occurrence in multiple myeloma. Cureus. 2022 Jun;14(6):e26045.
- Kastritis E, Zagouri F, Symeonidis A, et al. Preserved levels of uninvolved immunoglobulins are independently associated with favorable outcome in patients with symptomatic multiple myeloma. Leukemia. 2014 Oct;28(10):2075–2079. doi:10.1038/leu.2014.110
- Harutyunyan NM, Vardanyan S, Ghermezi M, et al. Levels of uninvolved immunoglobulins predict clinical status and progression-free survival for multiple myeloma patients. Br J Haematol. 2016 Jul;174(1):81–87. doi:10.1111/bjh.14026