Abstract
Background:
Diabetes self-management education (DSME), a prerequisite for diabetes care, is mostly unstructured and inaccessible in the public health sector in South Africa (SA). Patient education is often delivered by healthcare professionals (HCPs) with limited time and proficiency, resulting in preventable errors with insulin administration. A study was undertaken to assess the knowledge of HCPs on the practical aspects of insulin administration and it was hypothesised that their expertise was insufficient. The unmet needs of DSME often transpire when preventable errors with insulin administration become clinically evident at higher levels of care.
Methods:
A prospective, descriptive study of HCPs’ knowledge before and after attending a ‘Diabetes 101’ workshop was performed. Four workshops at Tygerberg Hospital (TH) and Worcester Provincial Hospital (WPH) were assessed between 2016 and 2019. A total of 146 participants completed a questionnaire before and after the workshops. Knowledge was scored on the correct responses per question and overall. The mean pre- and post-test scores were compared using two sample t-tests. Chi-square tests were used to analyse differences between pre- and post-training responses.
Results:
Of 146 participants, the majority were medical doctors (n = 116; 80%), mostly junior (n = 75; 65%) with 21% nursing practitioners. Before training there were significant deficiencies identified with only 3 of the 19 question items answered correctly by more than 50% of HCPs. The greatest knowledge deficits were with regard to insulin re-suspension and the injection technique and priming of the insulin pen. Following training there was a significant improvement between the pre-test mean percentage score of 36.0% (15) and post-test mean percentage score of 68% (16) (p < 0.001).
Conclusion:
Knowledge on the practical aspects of insulin administration is insufficient amongst HCPs but improved after structured education. Further research is needed to assess the long-term retention of knowledge and the impact of knowledge translation into clinical care.
Introduction
Diabetes mellitus (DM), a metabolic disorder characterised by chronic hyperglycaemia, places a significant burden on health systems. Type 2 DM is reportedly responsible for more deaths than malaria, human immunodeficiency virus and tuberculosis combined.Citation1 The measurable impact on the South African health system is unfortunately limited by the lack of screening and accurate data on DM prevalence and expenditure. Local prevalence figures for diabetes mellitus, based on available published data, vary widely but range between 3.6% and 14.6%.Citation1,Citation2 Experts are, however, of the opinion that some of the reported figures are an underestimation of the true burden of the disease.Citation1 Hyperglycaemia characteristic of DM occurs due to one or a combination of the following: the inability of the pancreatic beta cells to produce adequate amounts of insulin known as insulin secretion (IS) and/or a decrease in insulin action commonly known as insulin resistance (IR). Type 1 DM is an auto-immune disease that primarily targets pancreatic β-cells and impairs IS. Type 2 DM is characterised by a relative insulin deficiency that progresses over time, coupled with mostly acquired, lifestyle-associated IR.Citation3
Chronic hyperglycaemia due to uncontrolled DM, irrespective of the underlying pathophysiology, leads to an array of complications. These complications affect the micro- and macrovascular systems and are especially noteworthy, owed to the fact that each is preventable.Citation1,Citation4 Timeous insulin initiation is of utmost importance to ensure good glycaemic control in people living with diabetes (PLWD) in order to prevent both long-term diabetes complications and acute emergencies.Citation5 Diabetes self-management education (DSME) is essential to ensure long-term health as it empowers and enables PLWD to take control of their own diabetes management.Citation6,Citation7 Even though DSME is a critical component in the management of DM, it is mostly either unattainable or suboptimal in the public health sector in South Africa. The current barriers to DSME are the lack of diabetes educators (DE) coupled with an over-burdened healthcare system. Diabetes education is delivered on an ad hoc basis and it is often incorrectly assumed that healthcare professionals (HCPs) are familiar with the basic aspects of insulin administration.Citation8 In the sporadic event that diabetes education is offered, it is typically non-structured and most often provided by HCPs who themselves are ill-equipped and overburdened.Citation8 DSME has been shown to improve glycaemic control independent of other factors.Citation7 Correct insulin administration is a fundamental component of DSME, and is regarded as equally important in achieving glycaemic control as the type and dose of insulin prescribed.
The gaps in DSME often transpire when errors with insulin administration become evident, often with deleterious consequences. Repercussions of incorrect insulin administration include hypo- and hyperglycaemic emergencies and, in the longer term, diabetic retinopathy, nephropathy, neuropathy and cardiovascular disease or death due to glycaemic targets not being reached.Citation9,Citation10
Studies abroad in HCPs have demonstrated deficiencies in knowledge amongst various groups involved in the provision of insulin therapy.Citation11–14 In South Africa, a few studies have examined diabetes-related knowledge of HCPs,Citation15,Citation16 but no published studies focused on practical insulin-related knowledge. We aimed to assess the knowledge of the practical aspects of insulin administration in public-service HCPs who attended voluntary diabetes education workshops hosted by the Tygerberg Hospital Division of Endocrinology in the Western Cape province of South Africa. We hypothesised that HCPs’ knowledge regarding insulin administration was insufficient before training.
Methods
Study design and setting
We performed a prospective, descriptive study of HCPs’ practical knowledge concerning insulin administration for DM before and after attending one of four Diabetes 101 workshops, three at Tygerberg Hospital (TH) and one at Worcester Provincial Hospital (WPH) in the Western Cape province, South Africa. This study was conducted between December 2016 and April 2019. The structure and course content at the workshops have been standardised and remained unchanged over the four years.
Diabetes 101 workshop
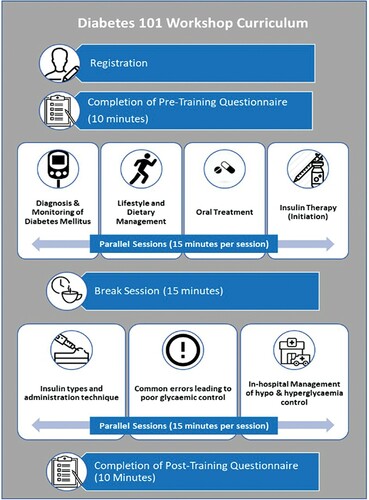
The Division of Endocrinology at TH annually hosted a Diabetes Education Workshop ‘Diabetes 101’ for HCPs. The workshop aimed to improve knowledge on practical aspects of diabetes and insulin administration. The workshop consisted of seven parallel sessions with a planned duration of 15 minutes (10 minutes education and 5 minutes for questions and answers) (). Each session was conducted in separate areas with each area set up with its respective subject matter. Participants were divided into small groups (some 5–6 participants per group) and groups rotated through each session.
All groups completed the workshop curriculum. The duration for participants to rotate through all the sessions spanned two hours. Participants completed a practical knowledge-based, predefined standardised questionnaire before the workshop commenced and completed the same questionnaire thereafter.
One of the 15-minute sessions covers the practical aspects of insulin therapy, which includes insulin administration technique. The education provided at the insulin administration session is standardised and was provided by a single certified diabetes educator and dietitian (Lourentia van Wyk) in all four workshops. Topics addressed in the workshop sessions are noted in . Sessions were presented in English by endocrinologists, endocrinology fellows and two dietitians. The course was advertised via email, posters and the WhatsApp social media platform, and attendance was free of charge.
Study participants were HCPs who attended the Diabetes 101 workshops. The course was accessible to medical registrars (specialist trainees), medical officers (MOs), medical interns and nursing staff from TH, WPH and their referral centres. These HCPs were employed in the public sector in the primary, secondary and tertiary settings at the time of the assessment and provided signed consent via an attendance register. All consecutive questionnaires that were completed were included and a formal power analysis was not performed.
Data collection
Standardised questionnaires used for patient education at TH were utilised (). Participants were requested to complete the questionnaires on arrival before the training commenced and were asked to respond to the same questionnaire upon completion of the training. All data sheets were anonymous, in English and were collected by the administrative clerk of the division at the end of each workshop. The data sheets of pre- and post-training questionnaires were unpaired due to the anonymity of the data. The questionnaire, entitled ‘Practical aspects of insulin administration’, consists of 10 knowledge-based questions. Questions 1–4 and Question 8 have more than one option to complete, totalling 19 items (). A third (30%) of the question items focused on insulin characteristics and initiation and the rest (70%) on insulin preparation and administration. Respondents were asked to indicate whether each of the questions/statements was ‘correct’ or ‘incorrect’. An ‘unsure’ option was also provided to discourage participants from guessing. For every correct answer, a score of 1 was given, and 0 for every incorrect answer. Questions that were left blank or answered ‘unsure’ were considered incorrect. Completed questionnaires were scored manually, totalling a maximum of 19 marks.
Table 1: Topics and list of knowledge-based questions with model answers
Statistical analysis
The data obtained were captured into a Microsoft Excel (Microsoft Corp, Redmond, WA, USA) spreadsheet and imported into SPSS Version 25 (IBM Corp, Armonk, NY, USA) for statistical analysis. Correct responses to questionnaire items were coded as categorical data (correct, incorrect) and compared between the pre- and post-training questionnaires. Scores were computed by totalling the correct responses across the 19 questionnaire items at pre-training and post-training timepoints.
Normally distributed continuous variables such as the scores were summarised as a mean and standard deviation (SD). Categorical variables were summarised comparing the pre-training with post-training questionnaires as frequencies and percentages. Due to the data being unpaired, Chi-square tests were used to analyse differences between pre-training and post-training scores. A two-sample t-test was used to compare the mean score of the questionnaire, consisting of 19 questionnaire items for the participants at the pre- and post-training. Statistical significance was set at p < 0.05.
Ethical considerations
Ethical approval was obtained from the Health Research Ethics Committee of Stellenbosch University (X18/09/2018). Participation was voluntary and all participants provided consent via an attendance register. All data were anonymised, and confidentiality of participants’ personal information ensured.
Results
The questionnaires () were completed by a total number of 146 HCPs, and all questionnaires were analysed. Most of the participants were medical interns (n = 45; 31%), followed by medical registrars (n = 32; 22%). A summary of the designation of HCPs can be seen in . A summary of the participants’ responses to individual questions before and after the workshop can be seen in .
Table 2: Designation of healthcare professionals who completed questionnaires
Table 3: Summary of responses of participants to questions before and after diabetes workshops
Knowledge assessment before training
Based on the pre-training data, only 3 of the 19 question items were answered correctly by more than 50% of HCPs. The question with the highest correct score was Question 9 regarding discarding of insulin vials after 28 days, where 77% (n = 112) of the participants answered correctly. This was followed by Questions 1d (n = 76; 52%) pertaining to insulin initiation when HbA1C is more that 7% on maximal oral doses and Question 2b (n = 75; 51%) on identifying Protaphane® as an example of cloudy insulin.
The major deficits before training were questions 8a (n = 19; 13%), where the least number of HCPs knew it was incorrect to press the plunger down for 3–5 counts, 4a (n = 25; 17%) regarding the method of priming an insulin pen, and Question 4b (n = 30; 20%) concerning the necessity of priming before every use. Only 37 participants (25%) were aware that insulin should be initiated when the HbA1C is > 10% at diagnosis (Question 1c). A minority of the participants (n = 33; 23%) knew that cloudy insulin should be re-suspended 20 times (Question 3) and despite the common use of Actraphane®, less than 40% of HCPs knew it is a cloudy suspension. More than half of the participants (n = 84; 58%) thought that longer needles are needed if the patient is obese as assessed in Question 5, and only about a third of the participants (n = 50; 34.2%) knew insulin is absorbed faster from the abdomen (Question 6). In Question 7, 61% (n = 89) of the participants said that injecting into a skinfold is necessary. With regard to using an insulin pen (Question 8), only 32% (n = 46) of participants knew that needles should be removed from the pen after each injection, 49% (n = 72) knew that needles are ideally made for single use, and less than half (46%; n = 67) of the participants knew that pens whilst in use may be stored at room temperature. Some 32% (n = 46) of participants were aware that air injected into the vial before drawing up the insulin eases the process.
Comparison of knowledge before and after training
The mean correct questionnaire percentage score obtained before training was 36% (15) with an average of 7/19 questions answered correctly. The mean correct percentage score obtained for the questionnaire after training improved significantly to 68% (16), with an average of 13/19 questions answered correctly per participant.
The overall improvement in percentage score for the questionnaire after training was 32 percentage points (95% CI 35.6–28.3). The comparison of the mean correct questionnaire score before and after the diabetes workshops was statistically significant (p < 0.001, standard error 1.3). All but two question items (Question items 1d and 4a) showed notable increases in correct responses following the training.
A significantly higher proportion of HCPs provided correct responses to Question 1 (focus on initiation of insulin in T2DM), following the workshop. The most significant improvement within this question group was the response to Question item 1c (insulin initiation when HbA1C > 10% at diagnosis), with a 44 percentage point increase after the workshop (p < 0.001). The responses to Question item 1d (insulin initiation with HbA1c > 7% on oral medication) showed no improvement after training (p = 0.907). There was a 72 percentage point improvement in knowledge on resuspension of insulin (Question 3) with a 95% yield for the correct answer after training (n = 139) as compared with 23% (n = 33) pre training (p < 0.001). Question 4b (focus on pen-priming with every use) improved by 43 percentage points in correct responses (p < 0.001); however, the correct method of priming a pen (Question 4a) did not improve after training (p = 0.45).
Knowledge assessed in Questions 8b, 8c and 8d (focusing on insulin therapy with a pen) improved significantly after training, with increases in correct responses of 38, 54 and 45 percentage points respectively (p < 0.001). Although Question 8a (the number of counts an insulin pen plunger should be pressed) was answered correctly by only half (n = 74; 50%) of participants, training did result in an improvement of 38 percentage points (p < 0.001). Correct responses to Question 10 improved by 25 percentage points (p < 0.001).
Discussion
This is the first study specifically assessing the knowledge of HCPs regarding insulin administration in South Africa. The hypothesis that HCPs have insufficient knowledge regarding the practical aspects of insulin use was confirmed, and knowledge improved significantly with training as evident by the post-training assessment.
It is universally accepted that DSME is a prerequisite in the management of PLWD.Citation7 In healthcare settings without dedicated and practically trained DEs, the task of diabetes education often falls on doctors or nursing personnel. These HCPs often lack the practical knowledge, have significant time constraints and do not necessarily have the coaching proficiency to impact on this aspect of diabetes care.Citation8
Our findings raise concern that HCPs, as represented in this dataset, are not adequately equipped to provide training on insulin therapy and administration. Chew et al. demonstrated significant knowledge gaps in insulin administration when HCPs at a tertiary hospital in Singapore were assessed.Citation13 Another study in Baltimore assessed the knowledge of HCPs pertaining to insulin use across four tertiary hospitals. In this setting, the percentage of knowledge-based questions answered correctly was ranged from 47% to 59%.Citation12
Clinical inertia in diabetes management is a worldwide phenomenon and a major barrier to improved outcomes. The gap between best practice and actual care results from a complex interaction between the patient, HCP and healthcare system barriers.Citation15 The HCPs’ deficiencies in practical knowledge comprise a significant barrier that arises, in part, from the lack of emphasis on the practical aspects of diabetes education at undergraduate to postgraduate level. This is further perpetuated by multisystem deficiencies and lack of continuous medical education addressing practical diabetes knowledge. Haque and colleaguesCitation16 investigated barriers to initiating insulin in public sector primary health care centres in Cape Town. The MOs in this study confirmed that undergraduate medical training focus on theoretical management and indicated that it was inadequate to equip them with skills to practically manage diabetes.
A multinational study, the Management of Diabetes in Future Years (MODIFY), conducted among 600 primary care physicians from various countries (Germany, Japan, Spain, Turkey, the United Kingdom and the United States), identified physician inexperience and time constraints as major barriers to insulin intensification.Citation17 Most physicians in the study agreed that insulin intensification is crucial in diabetes management, yet as many as 30% never personally intensified insulin. In our study, about 50% of the HCPs were aware that insulin should be initiated if, despite maximal oral hypoglycaemic therapy, the HbA1C exceeds 7%. This could be attributed to the SEMDSA guidelines, which recommends that in high risk and elderly patients, a target HbA1C of 7–8% is acceptable. Fewer participants were aware of the other indications for insulin initiation or intensification.
In a study from Belgium,Citation18 primary care physicians (PCPs) perceived additional ‘upskilling’ by training focused on insulin initiation as an acknowledgement of their importance in caring for PLWD. In this study, the PCPs had the support of a DE who had been trained by a diabetes specialist.
The limited training in practical diabetes management and lack of accreditation of DEs as specialist personnel is another barrier to diabetes care in the public sector in South Africa. Mentorship and specialist diabetes training of DEs who support PCPs is a potential pragmatic solution. The feasibility thereof is unfortunately hampered by the lack of funded posts for endocrinologists, diabetes specialists and DEs in the public sector.Citation8 The critical importance of DEs in the public sector in South Africa, where 85% of PLWD in this country are cared for, cannot be overemphasised.Citation19
In our study, HCPs notably lacked knowledge regarding simple aspects such as insulin administration, re-suspension and priming of the insulin pen. These, per se, may have a major impact on the day-to-day glycaemic control in PLWD, without incurring any additional cost. In our study, only a quarter of participants knew how to re-suspend cloudy insulin. The most recent East Africa Diabetes Study Group guidelinesCitation19 acknowledge that without this crucial step there is no control over the dose injected. A study by Kaiser et al. showed that the actual dose injected may vary between 25% and 200% of the intended dose if NPH is only re-suspended three times instead of 20 times.Citation20 This large variation in dose accuracy was also confirmed by a randomised, crossover study that used the euglycemic glucose clamp technique.Citation21
In our study, 80% of the participants thought priming of insulin pens is done only once and 83% that it is only necessary when using a new needle. Pens should be primed before each injection, and priming should be repeated until a steady stream of insulin is ejected to ensure free and unobstructed flow.Citation22 It is essential to get rid of air bubbles and ensure needle and pen viability to prevent incorrect dosing.Citation23 In our study, 57% thought that longer needles are used in obese individuals, whereas shorter needles are just as effective to ensure subcutaneous delivery.Citation24 Only a third of the participants knew that insulin is absorbed faster from the abdomen. This is important for two reasons. First, given the different absorption rates of the various sites, patients should be educated to rotate within a site and not between sites to decrease the risk of variations in glycaemic control.Citation25 Second, mealtime short-acting insulin injected into the abdomen enhances absorption and expedites the effect whereas NPH should ideally be injected in the thigh region to ensure a more prolonged absorption and duration of action. Lifting a skinfold prior to insulin administration is only required when the needle in use is longer than the distance between the skin and the muscle.Citation22 More than half of the participants (61%) incorrectly perceived that a lifted skinfold is universally required.
A study evaluating six different types of insulin pens concluded that prolonged pressure on the plunger (must be pressed down for at least 10 seconds) is required to ensure that the full intended dose is given.Citation26 Only a small minority of study participants (13%) were aware of this important aspect of insulin injection. Needles are manufactured for single use and should be discarded immediately after the injection. If left attached to the pen, accumulation of air may occur via the needle as both ends are open, which may cause serious under-dosing.Citation27 In addition, when leakage of unsuspended cloudy insulin occurs through the attached needle due to temperature-related expansion of insulin, the concentration of the insulin in the pen is modified. Only a third of our study participants knew that needles should be removed from the pen after each injection. In resource-limited countries and public health care systems, needles may safely be re-used up to five times.Citation19,Citation28 Blanco et al. found, however, that the re-use of needles more than 5 times significantly increases the risk for lipohypertrophy.Citation29,Citation30 Less than half (46%) of the participants knew that pens in use may be stored at room temperature. According to the FIT guidelines,Citation31 insulin may be stored at room temperature once in use as this causes less discomfort and make it easier to re-suspend cloudy insulin.
As there are still many PLWD managed with insulin vials and syringes in the public health system, a practical knowledge of certain aspects unique to the use of vial insulin is also required. Only a third of the participants knew that air is injected into the vial before drawing up the insulin to ease withdrawal, but most knew that insulin vials in use should be discarded after 28 days as indicated by the FIT guidelines.Citation31
Diabetes is a chronic, non-curable condition with lifelong implications that is mostly managed by the patients themselves. To ensure optimal self-management, PLWD require continuous education and support provided by empathic and knowledgably HCPs. There are many guidelines available (e.g. FITTER), but optimal utilisation and implementation requires that the gaps between theory and practice are closed. The diabetes education workshops significantly improved the short-term knowledge of the HCPs. The improvement in knowledge was not universal, with some deficiencies in insulin initiation and administration still noted after the training. It may be related to the fact that only 15 minutes of the 2-hour workshop was dedicated to these specific aspects and this may not have been adequate to impart the knowledge required.
This study had limitations. The sample size was small and could be biased as it is plausible that the workshops were better attended by HCPs who lacked knowledge and felt the need to improve and attain it. The data sheets with the questionnaire responses did not include the professional designation of the participants, therefore the responses could not be analysed according to each designation. We recommend further studies with categorisation of health care workers to highlight where future training should focus on. Although our findings suggest that diabetes education workshops are effective in improving the immediate practical knowledge of HCPs, this does not automatically indicate long-term retention and implementation of the acquired knowledge. This may require repeated contact sessions and continuous education.
Conclusion
This study shows that short and focused diabetes education leads to marked improvement in HCP knowledge on practical aspects of insulin initiation and administration. The lack of DEs and DSME is a major limitation in diabetes care in South Africa. Further research is needed to assess and rectify the gaps in practical training, along with studies on the long-term retention of knowledge and the impact of knowledge translation into clinical care.
Acknowledgements
The authors would like to acknowledge the healthcare professionals who attended the Diabetes 101 workshops at TH and WPH. They would also like to express sincere gratitude to the Department of Endocrinology, including the endocrinologists, endocrinology fellows and dietitians who provided the course content at the various sessions of the workshops. In addition, they would like to acknowledge Tonya Esterhuizen, biostatistician at University of Stellenbosch for data analysis and Dr Karis Moxley from the University of Stellenbosch Registrar Research Support Office for the research support and development.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Amod A, Coetzee A, Kinvig TE, et al. SEMSDA 2017 guidelines for the management of type 2 diabetes. J Endocrinol Metab Diabetes South Africa. 2017;22(1):S1–196.
- Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. https://doi.org/10.1016/j.diabres.2018.02.023.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(SUPPL.1):81–90. https://doi.org/10.2337/dc08-s055.
- Crofford OB, Genuth S, Baker L. Diabetes control and complications trial (DCCT): Results of feasibility study. Diabetes Care. 1987;10(1):1–19. https://doi.org/10.2337/diacare.10.1.1.
- Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926–943. https://doi.org/10.1016/j.pec.2015.11.003.
- Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: A joint position statement of the American Diabetes Association, the American Association of Diabetes educators, and the academy of nutrition and dietetics. Diabetes Educ. 2015;41(4):417–430. https://doi.org/10.1016/j.jand.2015.05.012.
- Dube L, Van den Broucke S, Dhoore W, et al. An audit of diabetes self-management education programs in South Africa. J Public Health Res. 2015;4(3):176–184. https://doi.org/10.4081/jphr.2015.581.
- Dolinar R. The importance of good insulin injection practices in diabetes management. US Endocrinol. 2009;5(1):49–52. https://doi.org/10.17925/use.2009.05.1.49.
- Davel H, Berg GI, Allie R, et al. Injection technique guidelines for diabetes: sharp and to the point. J Endocrinol Metab Diabetes South Africa. 2014;19(1):8–13. https://doi.org/10.1080/16089677.2014.11073595.
- Karara MW, Otieno FC, Okalebo FA, et al. Determinants of insulin-related knowledge among healthcare providers at a county referral hospital in Kenya. Afr J Pharmacol Ther. 2016;5(2):74–80.
- Derr RL, Sivanandy MS, Bronich-Hall L, et al. Insulin-related knowledge among health care professionals in internal medicine. Diabetes Spectr. 2007;20(3):177–185. https://doi.org/10.2337/diaspect.20.3.177.
- Lee MKS, Liu Z, Quek TPL, et al. Insulin-related knowledge among health care professionals at a tertiary hospital. Diabetes Spectr. 2013;26(3):187–193. https://doi.org/10.2337/diaspect.26.3.187.
- Bain A, Kavanagh S, McCarthy S, Babar. Assessment of insulin-related knowledge among healthcare professionals in a large teaching Hospital in the United Kingdom. Pharmacy. 2019;7(1):7–16. https://doi.org/10.3390/pharmacy7010016
- Van Zyl DG, Rheeder P. Survey on knowledge and attitudes regarding diabetic in patient management by medical and nursing staff at kalafong hospital. J Endocrinol Metab Diabetes South Africa. 2008;13(3):90–97. https://doi.org/10.1080/22201009.2008.10872178.
- Haque M, Navsa M, Emerson SH, et al. Barriers to initiating insulin therapy in patients with type 2 diabetes mellitus in public-sector primary health care centres in Cape Town. J Endocrinol Metab Diabetes South Africa. 2005;10(3):94–99. https://doi.org/10.1080/22201009.2005.10872127.
- Reach G, Pechtner V, Gentilella R, et al. Clinical inertia and its impact on treatment intensification in people with type 2 diabetes mellitus. Diabetes Metab. 2017;43(6):501–511. https://doi.org/10.1016/j.diabet.2017.06.003.
- Cuddihy RM, Philis-Tsimikas A, Nazeri A. Type 2 Diabetes Care and insulin intensification. Diabetes Educ. 2011;37(1):111–123. https://doi.org/10.1177/0145721710388426.
- Sunaert P, Willems S, Feyen L, et al. Engaging GPs in insulin therapy initiation: A qualitative study evaluating a support program in the Belgian context. BMC Fam Pract. 2014;15(1):1–9. https://doi.org/10.1186/1471-2296-15-144.
- Erzse A, Stacey N, Chola L, et al. The direct medical cost of type 2 diabetes mellitus in South Africa: a cost of illness study. Glob Health Action. 2019;12(1):1–8, https://doi.org/10.1080/16549716.2019.1636611.
- Bahendeka S, Kaushik R, Swai AB, et al. EADSG guidelines: insulin storage and optimisation of injection technique in Diabetes management. Diabetes Ther. 2019;10(2):341–366. https://doi.org/10.1007/s13300-019-0574-x.
- Kaiser P, Maxeiner S, Weise A, et al. Assessment of the mixing efficiency of neutral protamine hagedorn cartridges. J Diabetes Sci Technol. 2010;4(3):652–657. https://doi.org/10.1177/193229681000400320.
- Lucidi P, Porcellati F, Andreoli AM, et al. Pharmacokinetics and pharmacodynamics of NPH insulin in type 1 diabetes: The importance of appropriate resuspension before subcutaneous injection. Diabetes Care. 2015;38(12):2204–2210. https://doi.org/10.2337/dc15-0801.
- Frid AH, Kreugel G, Grassi G, et al. New insulin delivery recommendations. Mayo Clin Proc. 2016;91(9):1231–1255. https://doi.org/10.1016/j.mayocp.2016.06.010.
- American Diabetes Association. Insulin administration. Diabetes Care. 2003 Jan;26(suppl 1):s121–s124. https://doi.org/10.2337/diacare.27.2007.s106.
- Gibney MA, Arce CH, Byron KJ, et al. Skin and subcutaneous adipose layer thickness in adults with diabetes at sites used for insulin injections: implications for needle length recommendations. Curr Med Res Opin. 2010;26(6):1519–1530. https://doi.org/10.1185/03007995.2010.481203.
- Koivisto VA, Felig P. Alterations in insulin absorption and in blood glucose control associated with varying insulin injection sites in diabetic patients. Ann Intern Med. 1980;92(1):59–61. https://doi.org/10.7326/0003-4819-92-1-59.
- Annersten M, Frid A. Insulin pens dribble from the tip of the needle after injection. Pract Diabetes Int. 2000;17(4):109–111.
- Ginsberg BH, Parkes JL, Sparacino C. The kinetics of insulin administration by insulin pens. Horm Metab Res. 1994;26(12):584–587. https://doi.org/10.1055/s-2007-1001764.
- Puder JJ, Atar M, Muller B, Pavan M, Keller U. Using insulin pen needles up to five times does not affect needle tip shape nor increase pain intensity. Diabetes Res Clin Pract. 2005;67(2):119–123. https://doi.org/10.1016/j.diabres.2004.06.001
- Blanco M, Hernández MT, Strauss KW, et al. Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013;39(5):445–453. https://doi.org/10.1016/j.diabet.2013.05.006.
- Canadian Diabetes Association. Forum for Injection Technique (FIT) Canada - Recommendations for Best Practice in Injection Technique 4th Edition 2020.Canada:CDA,2020. https://www.fit4diabetes.com/files/7816/0803/3133/FIT_Recommendations_2020.pdf (accessed 21 June 2020).