ABSTRACT
Few studies have examined brief transdiagnostic groups. The Take Control Course (TCC) was developed for patients with mild to moderate common mental health problems. We examined whether TCC is non-inferior to individual low-intensity cognitive behaviour therapy (CBT) in a single-blind individually randomised parallel non-inferiority trial. The primary outcomes were depression (PHQ9) and anxiety (GAD7) at 6-month follow-up (primary outcome point) and 12-month follow-up. The non-inferiority margin that we set, based on previous trials, corresponds to approximately 3 points on the PHQ9 and approximately 2.5 points on the GAD7. Intention-to-treat (ITT) and per-protocol (PP) analyses of 6-month data of 156 randomised patients indicated that TCC was non-inferior to individual low-intensity CBT on anxiety (ITT Coefficient = 0.24; 95% CI: −1.45 to 1.92; d = 0.04; p = .79), and depression (ITT Coefficient = 0.82; 95% CI: −1.06 to 2.69; d = 0.14; p = .39) outcomes, and functioning (ITT Coefficient = 0.69; 95% CI: −2.56 to 3.94; d = 0.08; p = .68). The findings at 12 months were inconclusive and require further testing. This randomised trial provides preliminary support that TCC is not less effective than short-term individual CBT within Improving Access to Psychological Therapies (IAPT) services.
Globally, anxiety disorders have remained the most common problems for the last three decades, at around 3–4% of the world population as assessed in 2019 (Yang et al., Citation2021), with a similar prevalence found for depression (Liu et al., Citation2020). These common mental health problems entail a huge burden in terms of days lost to illness (Yang et al., Citation2021), and they are mostly treated in primary care settings (Aillon et al., Citation2014). Due to the prevalence of these problems, psychological therapies are required that can meet such demand. One response to this has been to offer varied intervention modalities, and different lengths of treatment (Bennett-Levy et al., Citation2010). Such approaches have been used within Improving Access Psychological Therapy (IAPT) services in the UK as part of a stepped care model whereby the “least restrictive” treatment option is offered while still providing a treatment that is likely to lead to significant health benefit (Bower & Gilbody, Citation2005). Individual brief CBT, consisting of six one-to-one 30-min sessions, is the most commonly delivered treatment within low-intensity IAPT services (Glover et al., Citation2010).
Two meta-analyses found that brief CBT was more effective than control conditions for patients with anxiety and depression (Cape et al., Citation2010; Nieuwsma et al., Citation2012). Furthermore, a large meta-analytic review of reviews found no difference in effectiveness between using high- and low-intensity CBT (Fordham et al., Citation2021). They clarify that this does not mean that: “low-intensity is equally effective as high-intensity CBT, only that, where it has been deemed appropriate to use and has been empirically tested, low-intensity CBT has been effective” (p.28, Fordham et al., Citation2021). Yet the limitations of low-intensity interventions are also clear, with one study of over 400 patients with anxiety and depression finding that over half of them had relapsed after one year (Ali et al., Citation2017). Given the initial effectiveness of individual brief CBT for patients with common mental health problems, it seems plausible that brief group-based interventions could be effective and provide a cost-effective alternative to individual brief CBT. A review of whether group or individual CBT was more cost-effective found that overall groups were more cost-effective (Tucker & Oei, Citation2007). However, an updated review in this area would be helpful, as the authors concluded that the evidence in favour of groups was stronger for depression than anxiety disorders.
Convergent evidence from genetic, neurophysiological, and cognitive behavioural research suggests that current diagnostic categories do not precisely specify the factors that cause and maintain psychopathology (Buckholtz & Meyer-Lindenberg, Citation2012; Morris & Cuthbert, Citation2012). This has resulted in an increased drive for understanding psychopathology based on mechanistic empirical data (e.g. the Research Domain Criteria project) (Cuthbert & Insel, Citation2013). Brief transdiagnostic groups potentially combine the service delivery advantages of brief interventions and of a transdiagnostic approach. Transdiagnostic interventions target cognitive and behavioural maintenance processes that are common across disorders, such as repetitive thinking and behavioural avoidance (Mansell et al., Citation2009). Therefore, transdiagnostic interventions can address multiple and co-morbid problems within one intervention (Andersson et al., Citation2013).
Previous research into transdiagnostic CBT groups has mainly focussed on specific populations, such as clients with anxiety disorders (Newby et al., Citation2015; Norton & Philipp, Citation2008; Reinholt & Krogh, Citation2014). Although there are protocols aimed at a range of anxiety and mood disorders, these have been primarily developed and evaluated in an individual format (Barlow et al., Citation2017; Ellard et al., Citation2010). Two of the best-established transdiagnostic approaches that have been evaluated in a group format are group CBT for anxiety disorders (Norton & Hope, Citation2008) and the Unified Protocol (Bullis et al., Citation2015; Laposa et al., Citation2017; Osma et al., Citation2022; Reinholt et al., Citation2022). Both interventions demonstrate differences from the Take Control Course (TCC), such as using techniques that challenge distorted thinking. The Unified Protocol has a greater emphasis on the adaptive function of emotions than the transdiagnostic group CBT and is designed to target anxiety and mood disorders (Norton & Hope, Citation2008; Wilamowska et al., Citation2010). Both are substantially longer than the TCC (i.e. twelve 2‐h sessions, almost four times the length of the TCC).
Despite the evidence suggesting that brief interventions in primary care are effective, transdiagnostic groups tend to be delivered using a time-intensive format (e.g. 10–12 2-h sessions); at a minimum of eight 2-h sessions (for a meta-analysis, see Newby et al., Citation2015). In contrast, the TCC is six sessions, with an average session length of an hour. Because it is briefer than established transdiagnostic groups and can be provided by psychological well-being practitioners without training in high-intensity therapies and as a first treatment intervention, it can be considered a low-intensity intervention (Shafran et al., Citation2021). The TCC targets transdiagnostic processes, but it focuses on clients with mild-to-moderate depression and anxiety because these are the clients that have particularly been found to benefit from brief interventions.
Several specific advantages of group-based transdiagnostic treatments have been identified, including the universality of the transdiagnostic processes that cut across mixed presentations, simplicity of training in one protocol, reduced waiting times for a disorder-specific group, reduced pressure to speak compared to individual therapy, and learning new perspectives and getting mutual support from other members of the group with different presenting problems (Coholic et al., Citation2018; McEvoy et al., Citation2009; Mofrad et al., Citation2020; Morris et al., Citation2018).
The TCC can be described as “mechanistically transdiagnostic” because it explicitly targets common underlying mechanisms that are relevant across disorders [“shared mechanism treatment” in Sauer-Zavala et al. (Citation2017)]. It is derived from a theory of psychological functioning known as Perceptual Control Theory (PCT; Powers, Citation1973). PCT has contributed to CBT in a number of ways, including as a theoretical framework to explain the mechanisms of existing CBT interventions (Grawe, Citation2004; Mansell, Citation2005), as the foundation for a transdiagnostic cognitive therapy known as Method of Levels (Carey, Citation2006; Mansell et al., Citation2012), and as a rubric for advancing the practice of existing CBT techniques (Alsawy et al., Citation2014; Healey et al., Citation2017). PCT is based on the tenet that control is a central process to living (Powers, Citation1973). Humans control by trying to ensure their experience is a certain way and corresponds to their internal reference values or goals. There is substantial evidence that problems with control are associated with low well-being and psychopathology (e.g. Chorpita & Barlow, Citation1998; Harrow et al., Citation2009; Teachman et al., Citation2012). Furthermore, enduring conflicts between important goals people are trying to achieve can result in psychopathology (Brockmeyer et al., Citation2013; Kelly et al., Citation2015). From a PCT perspective, enduring conflict between people’s important goals is a primary cause of loss of control and psychopathology (i.e. distress and unwanted symptoms) and these are the processes targeted within TCC (Morris et al., Citation2016).
A preliminary prospective cohort study comparing TCC to individual brief CBT within a clinical primary care sample indicated the potential of TCC to reduce symptoms of anxiety and depression (Morris et al., Citation2015) and a narrative review specified detailed evidence for the conceptual underpinnings (Morris et al., Citation2016). A non-inferiority design was selected for the current trial as individual brief CBT is a well-established treatment and the TCC provides an alternative with other advantages, such as group format, cost-effectiveness, explicitly transdiagnostic basis (Morris et al., Citation2018; Piaggio et al., Citation2012). Low-intensity individual CBT is the primary evidence-based treatment for mild-to-moderate anxiety and depression in the UK. Indeed, earlier reviews have found no significant difference in outcomes between low-intensity CBT, such as guided self-help, and “gold standard” therapist-administered CBT (e.g. Priemer & Talbot, Citation2013). The primary hypothesis was that participants in both groups would show reductions in symptom scores on measures of anxiety and depression, and outcomes in the TCC would be non-inferior to established individual brief low-intensity CBT.
Method
This study is known as PCTEAM (Primary Care Trial of Efficacy of Alternative Modalities) and the protocol provides a detailed rationale, power analysis, and design (Morris et al., Citation2014). The protocol was registered two weeks after the commencement of recruitment for the study owing to a logistical delay, and no changes were made to the design during this time.
Participants
Participants were recruited from Salford Six Degrees Social Enterprise, a low-intensity IAPT Service.
Inclusion criteria were as follows: A) Aged 16 and above. B) Individuals with mild-moderate depression and anxiety that has emerged within 12 months prior to referral (i.e. the problem is not chronic and enduring). C) Sufficient English language skills to understand material (i.e. verbal and written language abilities required to read and complete simple worksheets and understand verbal presentations).
Exclusion criteria were as follows: A) Aged under 16. B) Suitability for higher intensity services that is primarily determined after first assessment with the service, for example, patients with Post-Traumatic Stress Disorder or severe Obsessive-Compulsive Disorder; patients with persistent self-injury requiring clinical management or who were potentially intent on and/or planning suicide; patients who are currently experiencing psychotic symptoms; have current substance dependence; or have an organic brain impairment, such as dementia. C) Literacy or language difficulties that will preclude them from reading simple worksheets or from conversing with a health-care professional without using an interpreter.
Measures
Primary outcome measures
These were firstly, the Patient Health Questionnaire Depression Scale (PHQ9). Secondly, the Generalised Anxiety Disorder Questionnaire (GAD7). The primary endpoint for both PHQ9 and GAD7 was at 6-months after baseline.
Secondary measures
These were, firstly, the Work and Social Adjustment Scale (WSAS). Secondly, the Psychological Outcome Profiles (PSYCHLOPS), which is a patient-generated outcome measure. The Credibility/Expectancy Questionnaire (CEQ) was used to measure treatment credibility and expectancy of improvement prior to treatment. Treatment credibility was also measured at 6-month follow-up using two items from the CEQ.
Procedure
Patients were predominantly referred to Six Degrees by their GP but could also be referred by other health-care professionals. In a generic initial assessment, with a Six Degrees clinician, patients who met the inclusion criteria were informed of the study alongside the service’s other treatment options, and were able to discuss participation. Interested patients were offered an appointment to further discuss the study, give informed written consent, and fill in baseline measures. Written informed consent was obtained from all patients.
After written consent to participate in the RCT and completion of baseline measures, the randomisation process was conducted. Administrators within Six Degrees randomised patients using a computerized randomization programme (Sealed Envelope); therefore, the assignment was concealed from the research team and assessors.
Research assistants primarily conducted follow-up assessments, although the first author conducted some assessments. Assessors were blind to treatment allocation and were not involved in providing the interventions. Although the first author conducted supervision with TCC group facilitators, this focused on group process issues. On a couple of occasions where supervision regarding risk issues, or other matters, required unblinding, the first author did not conduct follow-up appointments with these individuals to preserve the blinded assessments.
The only change to the trial protocol was that £20 vouchers were introduced as a thank you to participants completing either the 6-month or 12-month follow-up appointment to enhance recruitment. In the interests of fairness, all participants who had already completed a 6-month follow-up appointment (n = 18) were retrospectively sent a voucher.
Ethics statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and informed consent was obtained for all participants. All procedures were approved by the National Research Ethics Service Committee in 2014 (ref.14/NW/0160).
Treatments
Take Control Course (TCC): group intervention
The TCC consists of six weekly sessions (the first session is 1 h 15 min and all other sessions are 1 h). Details of the sessional content and the development of the TCC are provided elsewhere (Morris et al., Citation2016). The TCC is not focused on patient self-disclosure and discussion, but rather emphasises experiential learning, videos, facilitator presentations, and worksheets. A detailed therapy manual is available (Morris et al., Citation2018).
TCC is tightly based on a transdiagnostic theory called PCT. Control is the basis of this course. In accordance with a PCT theoretical account, targeted throughout the TCC are as follows: (1) Understanding the degree to which one can and desires, control over various aspects of one’s life; (2) awareness of valued higher-level goals; (3) awareness of higher-level goal conflict; (4) encouragement of flexible ways to control and reduction of processes (including rules, habits, routines, and mental processes), which block valued goals (Morris et al., Citation2016).
Clinicians and treatment integrity
Facilitators were 10 trained clinicians with 0.5–6 years’ clinical experience (degree educated with further training in low-intensity treatments). Many of the clinicians were Psychological Wellbeing Practitioners (PWPs), meaning that they had done a specific training to become a PWP (usually a year long and focusing on low-intensity CBT). However, some clinicians came from other professional backgrounds, such as Social Work or Nursing, and had received other training in CBT interventions. TCC training was a day. Training focused on familiarisation with the content of the TCC and on addressing group process issues, e.g. what to do if a patient becomes distressed during a TCC session. Whenever possible, new facilitators were paired with a more experienced facilitator for their first course. During each TCC, all facilitators accessed two weekly half-h peer supervision sessions. In addition, 1 h of external supervision was provided after session 2 (by the first author). Blinding was explained to all clinicians, and they were asked not to use names. As supervision focused on general group processes and specific issues, unblinding did not occur. However, if a significant risk issue (or similar) had arisen, then it could have been necessary for the supervisor to be unblinded. An adherence and competence checklist was used to assess the fidelity of delivery of sessions. This competence checklist was used in the pilot prospective cohort study (Morris et al., Citation2015; Morris, Citation2013). Two sessions were other-rated for each facilitator. In addition, all facilitators self-rated their adherence for each session, using the same checklist. This checklist was used for supervision purposes and to identify any training needs.
Control condition: individual low-intensity CBT (LI CBT)
The guided self-help interventions offered included cognitive and behavioural strategies; for example, behavioural activation, cognitive restructuring, sleep management, and problem-solving. Emphasis was on participant self-help, and participants were often given homework tasks to do between sessions (Richards & Borglin, Citation2011). There is a debate as to whether such low-intensity interventions should be described as “CBT” due to differences, such as the duration and adherence ratings used; however, given that the techniques used are CBT based, a CBT rationale and a number of common components (e.g. setting homework) then we have generally described the brief individual CBT as “low-intensity” CBT. These interventions differ from the TCC in a number of ways, for example, they consist of traditional CBT techniques (such as cognitive restructuring) and the treatment rationale is explained in terms of traditional CBT (such as thoughts, feelings, and behaviour cycles) rather than control and goal conflict. Sessions were individual, lasted 30-min, and participants were generally offered six sessions.
Clinicians and treatment integrity
All clinicians had completed an undergraduate degree and had received further training to deliver low-intensity treatments. The same clinicians who delivered the TCC also delivered individual low-intensity CBT (LI CBT), alongside additional members of the clinical team; clinicians delivering the LI CBT had a range of 0.5–31 years’ clinical experiences. All clinicians received at least 1.5-h of weekly supervision. Supervision sessions include skill monitoring and development using audio recordings of sessions, and often last 2-h. Additional supervision was provided regarding specific therapeutic skills, for example, fortnightly supervision was available to specifically develop skills in CBT.
Design and power calculation
The design was a randomised single-blind two parallel group non-inferiority trial comparing TCC and LI CBT with outcomes of depression and anxiety measured at baseline, six and twelve months. Block randomisation (using random permuted blocks) was performed with a 1:1 allocation. Trial procedures and analyses were specified prior to recruitment commencement. The database for analysis was fully anonymised and the trial statistician was not involved in any assessment appointments or clinical management.
Power calculations for the primary hypothesis (that TCC would be non-inferior) were based on a non-inferiority trial design comparing two groups, with equal numbers in each group (see Morris et al., Citation2014). Sixty-three participants per group would have 80% power for a non-inferiority margin of 0.5 SD with a significance level of 0.025 (as non-inferiority analyses are one-tailed). To allow for attrition at 27%, we aimed to recruit 173 participants at baseline. This figure is an average of the attrition levels within a meta-analysis of individual CBT treatments by (Hofmann & Smits, Citation2008), two RCTs of group interventions (Allart-van Dam et al., Citation2003; Andersson et al., Citation2013) and a feasibility study of the TCC (Morris et al., Citation2016).
Statistical analysis
All primary analyses followed the intention-to-treat (ITT) principle and involved all patients who were randomly assigned. All analyses were performed using Stata version 13.1.
The two primary outcome measures were the PHQ9 (depression) and GAD7 (anxiety). To test the primary hypothesis (that participants who were randomly allocated to TCC would experience non-inferior reductions in separate anxiety and depression symptom scores) we used a mixed-effect linear regression model. The models were estimated using maximum likelihood estimation, which accounts for missing outcomes assuming a missing at random mechanism. Separate linear mixed models were fitted for anxiety (GAD) and depression (PHQ) scores at 6 months, with randomisation and the respective baseline outcomes as covariates. We included a random intercept for group membership in the TCC arm and considered individuals in the LII arm as clusters of size 1 with their own random intercept. Bootstrapping was used where outcomes were non-normal. These results were examined to establish whether the treatment effect (and 95% confidence interval around the parameter) for the TCC differed by more than 0.5 SD (the non-inferiority value) from the LI CBT. Non-inferiority is established if the upper limit of the confidence interval is within the non-inferiority margin. It was pre-specified in the protocol that if non-inferiority was established, then we would examine whether TCC was superior to LI CBT (Piaggio et al., Citation2012). The actual analysis is the same for both superiority and non-inferiority, so if p values were significant for any of the measures, then this would indicate superiority. The ITT analysis was also conducted on WSAS and PSYCHLOPS.
Per-protocol (PP) analyses were conducted since ITT analysis may increase the risk of falsely claiming non-inferiority, and therefore it is recommended in the CONSORT guidance that both ITT and PP analyses be conducted (Piaggio et al., Citation2012). ITT analyses were conducted as primary because non-compliance and attendance are very likely in routine clinical practice, and such analysis reduces the risk of group and selection bias (Gupta, Citation2011). Further, the study was powered for ITT analyses and smaller sample sizes lead to wider confidence intervals. Participant data was included in the PP analysis if participants attended one or more sessions of the randomised treatment. PP analyses were conducted on each outcome using a mixed-effects regression model accounting for potential clustering effects of the TCC group.
The number of participants who met the criteria for clinically significant change (CSC) and reliable change (RC) is calculated (Jacobson & Truax, Citation1991). CSC requires that a person be above the clinical score cut-off pre-treatment (i.e. in the clinical range), but below it at post-treatment (Jacobson & Truax, Citation1991; Jacobson et al., Citation1999; Richards & Borglin, Citation2011). RC indicates whether the change in scores is greater than that which could be due to the inherent unreliability of the measure.
Non-inferiority margin
The non-inferiority margin was 0.5. The value of 0.6 was originally considered as the non-inferiority margin based on previous non-inferiority studies in similar contexts and/or using similar interventions to the reported trial (Hedman et al., Citation2011; Lovell et al., Citation2006; Norton & Barrera, Citation2012; Norton, Citation2012), in two of these studies the non-inferiority margin was based on previous meta-analyses (Hofmann & Smits, Citation2008; Norton & Price, Citation2007). Margins of non-inferiority in these trials ranged from Δ = 0.50 to 0.67 SD below the mean effect of the established treatment arm for each measure (Mean Δ = 0.59, rounded up to 0.6). However, the effect size of 0.6 corresponds to approximately 4 points on the PHQ9 and approximately 3.5 points on the GAD7. These values were considered too high to be a reliable non-inferiority margin, i.e. a value that is not clinically significant, and therefore the treatment can genuinely be considered non-inferior. For example, only 5-points on the PHQ9 differentiates clients with the highest score in the mildly depressed category from clients with the highest score in the moderately depressed category (Richards & Suckling, Citation2009). Therefore, the value of 0.5 was chosen because this was the lowest non-inferiority margin found in the non-inferiority studies aforementioned (Hedman et al., Citation2011; Lovell et al., Citation2006; Norton & Barrera, Citation2012; Norton, Citation2012). The margin of 0.5 corresponds to 3 points on the PHQ9 and 2.5 points on the GAD7 (Richards & Borglin, Citation2011). The non-inferiority margin we chose therefore exceeded one calculation of minimally clinically important differences for the primary outcomes that were published some years after the trial was designed (Kounali et al., Citation2022).
Results
Patient flow and attrition
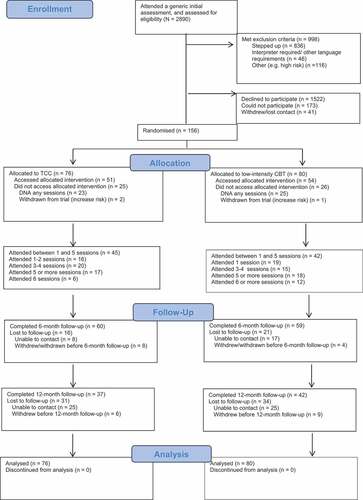
One thousand, seven hundred and thirty-six eligible patients were consecutively asked if they wanted to participate in the project between July 2014 and October 2015. One hundred and ninety-seven agreed to participate, but 41 did not proceed to randomisation (deciding not to access the service 27%, being un-contactable 15%, changing their mind about participation 15%, and other reasons, such as moving out of the country). Some individuals could not take part (6%), e.g. the time of the groups was not convenient, and some did not want to take part (53%). Clinicians were encouraged to include a reason for why patients did not want to take part, and the main reasons given were that patients did not want to access a group or the uncertainty of randomisation when they could directly access brief individual interventions. shows the CONSORT diagram.
Attrition from the baseline to 6-month follow-up was 24%, but due to recruitment difficulties the study was slightly underpowered (119 PHQ9 and 118 GAD7 were available at 6-month follow-up, but the target was 126). Attrition was much higher than predicted at 12-months (79 PHQ9 and GAD7 were available). The trial stopped recruitment as it had exceeded the specified end date and funding was only available for a specified time-period.
Participant characteristics and treatment credibility
shows participant characteristics and includes data on the average number of sessions attended.
Table 1. Sample characteristics.
At baseline, participants rated LI CBT (M = 13.38, SD = 3.07) as significantly more credible than TCC (M = 12.83, SD = 3.33); t(150) = 2.27, p = .03, d = 0.17; although the effect size was very low. At 6-month follow-up, using the PP sample, participants who were randomised to LI CBT (n = 31, M = 12.90, SD = 4.63) did not rate it as more credible than those who were randomised to TCC had rated the TCC (n = 37, M = 11.41, SD = 5.27); t(66) = −1.50, p = .22, d = 0.30.
Primary outcome measures: ITT and PP analyses
displays the means and standard deviations for the outcome variables at each time point for all participants with complete data, and displays the available and missing data across the follow-up period. displays the ITT and PP analysis of 6-month and 12-month follow-up data. At six months, TCC was non-inferior (i.e. no less effective) compared to LI CBT on both the PHQ9 and the GAD7 using ITT and PP analyses. At twelve months the findings were inconclusive, because the upper confidence intervals crossed the non-inferiority margin.
Table 2. Means and standard deviations for the main outcome variables.
Table 3. Available and missing data across outcome variables and analyses.
Table 4. Results of ITT and PP regression analyses of 6-month and 12-month follow-up data for primary outcome measures (PHQ9 and GAD7) and secondary outcome measures (WSAS and PSYCHLOPS).
The majority of the coefficients in were in the positive direction, with the exception of the ITT WSAS at six months, and the PP and ITT WSAS at twelve months. This indicates lower depression and anxiety scores in the LI CBT at follow-up controlling for baseline scores. There was no evidence for superiority of either intervention from any of the analyses (all p values are non-significant; see ) and the ITT analysis on the primary outcomes at 6-months were powered to detect superiority.
Secondary outcome measures: ITT and PP analyses
reports ITT and PP analysis of the WSAS and PSYCHLOPs at 6-month and 12-month follow-up. At six months ITT analyses indicated that the TCC was non-inferior to LI CBT on WSAS but not at 12 months. At six and twelve months using ITT and PP analyses it was not possible to establish non-inferiority for the PSYCHLOPS because the upper confidence intervals crossed the non-inferiority margin.
Clinically significant and reliable change
Using an ITT sample, details of those who experienced CSC, RC, and recovery for each treatment at six months are reported in . Baseline levels of those above the cut-off point on each measure are also reported because CSC and recovery can only be achieved if clients are above the cut-off point at baseline.
Table 5. Participants who experienced clinically significant changes, reliable changes and recovery in the ITT sample at six months.
Discussion
Using ITT and PP analyses at 6-month follow-up, the TCC was found to be non-inferior (no less effective) than individual brief low-intensity CBT on measures of anxiety and depression symptoms, and a measure of social and other functioning. The test for non-inferiority was inconclusive for outcomes at 12 months because the upper confidence intervals crossed the non-inferiority margins. Although analysis using a longitudinal model should have protected the power to some extent, the low sample size at 12-months is likely to increase the confidence interval and therefore makes it not possible to establish non-inferiority.
These findings add tentative evidence to the existing evidence for the effectiveness of transdiagnostic interventions (Newby et al., Citation2015). Further, this study provides preliminary evidence that at 6-months follow-up a brief group, addressing specifically transdiagnostic mechanisms, is non-inferior for patients with a broad range of common mental health problems within a “low-intensity” primary care setting. The average baseline scores on measures of depression and anxiety exceeded the cut-off for “moderate” severity (Kroenke et al., Citation2001; Spitzer et al., Citation2006). It also has a number of strengths including single-blind assessments and pre-specified protocols, accounting for clustering by group within analyses and combining an RCT design with a naturalistic service setting.
Individual versus group therapy
There was no evidence for the superiority of either treatment (see ). However, analyses of 12-month follow-up data were unable to conclusively demonstrate the non-inferiority of TCC. A meta-analysis of CBT for depression indicates that individual therapy can be superior to group therapy with differences in effectiveness present post-treatment but not at follow-up (Huntley et al., Citation2012). Evidence is limited by the risk of bias and small sample sizes. Comparative studies of patients with anxiety are even more limited, but indicate that an individual format maybe more effective (Mayo-Wilson et al., Citation2014; Tucker & Oei, Citation2007). One recent large RCT study has found that the group Unified Protocol, compared to treatment-as-usual in the form of brief individual, disorder-specific CBT, demonstrated larger improvements in depression, anxiety, and quality of life over time (Osma et al., Citation2022). Furthermore, another recent RCT compared two-group CBT interventions—disorder-specific versus transdiagnostic, thereby addressing this issue. They found evidence for non-inferiority with regard to most clinical outcomes at post-treatment, and 6-month follow-up (Reinholt et al., Citation2022).
The current study did not offer optimal delivery of the TCC, which could have influenced results. Due to very frequent staffing changes, the facilitator team regularly changed and it was generally not possible to arrange timings of the TCC around patient preference (e.g. only one evening course was run). Further, a qualitative study of TCC indicated that many patients strongly endorsed the group format compared to individual treatment, suggesting that it is important to offer patients a choice of modalities (Morris et al., Citation2018).
Are recovery levels comparable to other studies?
The percentages of participants who achieved recovery at six months was similar across treatment groups. The RCT of computerised CBT for depression found comparable levels of recovery at 6-months on a depression measure (28.6%) to the current study (TCC 24%; LI CBT 24%) (De Graaf et al., Citation2009). Uncontrolled studies of primary care psychological interventions have found higher recovery rates (Burns et al., Citation2016; Delgadillo et al., Citation2014; Richards & Borglin, Citation2011), including an evaluation of the Stress Control course, which has been found to reduce symptoms of anxiety and depression (Burns et al., Citation2016). However, these differ in design and recovery was calculated post-treatment, so the duration since initial assessment is not clear and some studies conflate low- and high-intensity CBT interventions. In support of the possible effect of design, another RCT of computerised CBT for depression found 23% recovery (Richards et al., Citation2015), while a previous cohort study comparing TCC to individual low-intensity CBT found a 44% recovery for either depression or anxiety scores in TCC treatment [27% on depression measure; (Morris, Citation2013)].
The effect of number of sessions attended
The relatively low average number of sessions attended across both treatments could also have influenced outcomes. Although attrition levels can be high in similar service contexts (Glover et al., Citation2010), studies have indicated that attending more sessions is associated with better outcomes (Burns et al., Citation2016; Delgadillo et al., Citation2014). The reasons why clients cease to attend sessions are often unclear because patients may not attend psychological interventions owing to difficulties, such as fear of disclosure and greater severity of symptoms, such as avoidance and a sense of helplessness (Schauman & Mansell, Citation2012).
On the other hand, research also indicates that early improvements are associated with recovery (Delgadillo et al., Citation2014) and that sudden gains can account for a significant amount of patients’ improvement (Aderka et al., Citation2012). In addition, a large study (N = 102 206) of dose–response effects for low- and high-intensity CBT interventions found that 95% of those clients who attain reliable and clinically significant improvement (or recovery) do so within seven, commonly half hour, sessions of low-intensity CBT (Robinson et al., Citation2020). A systematic review found that 4–6 sessions were optimal for low-intensity guided self-help (Robinson et al., Citation2020). In conjunction with high attrition levels in many primary care studies, it seems possible that some patients access treatment until they have achieved a personal “good enough” level of change and this could be early in treatment (Barkham et al., Citation2006). Therefore, the TCC recognises the variation in attendance by offering “stand-alone” sessions (Morris et al., Citation2015). But it is also acknowledged that non-attendance would be for a variety of reasons (e.g. high socio-economic deprivation is commonly associated with attrition) (O’Brien et al., Citation2009), and so the message given to patients remains “attend if you can”.
Linking this with the wider transdiagnostic group literature, group Unified Protocol is a longer higher-intensity intervention than TCC, at 12 2-h group sessions (Osma et al., Citation2022) and could be more suitable for those with more significant mental health problems than the mild-to-moderate anxiety problems targeted by TCC and other low-intensity interventions. Indeed, one recent large RCT has indicated that group Unified Protocol is associated with greater improvements in depression, anxiety, and quality of life than treatment-as-usual in the form of individual, disorder-specific CBT (Osma et al., Citation2022).
Credibility of groups
Individual low-intensity CBT was found to be more credible than TCC prior to treatment. The effect was low, but qualitative data from participants who accessed TCC indicated that patients could have concerns regarding group interventions (Morris et al., Citation2018). Such concerns did not appear specific to the TCC, as they focused upon fears of significant self-disclosure and being with other people. These findings suggest that how groups are introduced is important in allaying fears. For example, within the TCC, no self-disclosure is required, it can be more accurately described as a “course” rather than “group” format, and the concept of control can be used to explain the overall rationale for the course. Clinicians were encouraged to be clear about what the TCC involved and distinguish it from groups that are highly premised on self-disclosure. Control and choice underpin the principles of the TCC and so in routine practice it would only be offered to patients who expressed an interest in group interventions.
Limitations and future research
In addition to the limitations previously described regarding the non-optimal delivery of TCC, the study has a number of limitations. A key limitation is that participants were not formally diagnosed. Lack of diagnostic certainty is common within primary care contexts because the accuracy of initial diagnosis by GPs is variable (Mitchell et al., Citation2009). Furthermore, in the UK, few clinicians within primary care psychological services are trained to conduct diagnostic interviews (Richards et al., Citation2012). Therefore, limited diagnostic information increases ecological validity, but reduces the ability to predict the response of those with specific disorders.
Another limitation is that the study only recruited from one service and so it is unclear how results would generalise to a population with a different demographic profile. Further, out of 1736 potentially eligible clients, 156 were randomised; this is likely to influence how representative the sample is as potential participants had to agree to both being randomised and being involved in a research study. Attrition levels and recruitment difficulties meant the study was slightly underpowered, and this is a particular issue for PP analysis as this necessitated inclusion of a sub-sample; however, sample size for ITT analysis was approximately double that of previous non-inferiority trials comparing transdiagnostic groups to established treatments (Norton & Barrera, Citation2012; Norton, Citation2012). PP analysis was also limited by relatively low attendance of treatment sessions across both treatment groups; this is likely to reflect the level of socio-economic deprivation within the recruitment area (Morris et al., Citation2015; O’Brien et al., Citation2009). The reliability of the 12-month follow-up data is limited by the considerable attrition at twelve months. All the limits described could be addressed by a larger trial, which included greater clinician availability, formal diagnoses and multiple sites. The choice of an inferiority margin of 0.5 SD could be considered as liberal, even though it was conservative compared to non-inferiority margins used in earlier trials, because it allows a difference on one of the primary outcomes (PHQ-9) of three points, which is higher than one estimate of its minimally clinically important difference (MCID) of 1.7 points (Kounali et al., Citation2022). The TCC was deliberately compared with individual low-intensity CBTs, as this is an established treatment. However, this entails that there will be differences in format that could influence outcomes. For example, the two treatments differed in the maximum amount of clinician time offered. The maximum attendance time for TCC was 6-h 15 min; for individual CBT, this was 3-h (where patients attended the recommended 6-sessions, or up to 4-h for the 5% who attended over 6-sessions). Clearly, this could also be mediated by the ratio of patients to clinicians; in the TCC there will be more patients per clinician so less individual contact time within the group. Further, different interventions (due to their different formats) have different procedures for establishing treatment integrity. Although this is unavoidable, it is possible that this could differentially affect outcomes.
Given that some of the same clinicians deliver both TCC and low-intensity CBT, there is a possibility of contamination across treatments. However, low-intensity CBT is heavily protocol-driven and TCC is manualised, which will go some way to mitigating the risk. Although it is important to note that clinicians from both arms of the trial were drawn from the same professional group and that dropout rates were similar, it is feasible that more intensive training may have improved outcomes. We did not carry out an analysis of the adherence measure, which would benefit from psychometric research.
The findings of this non-inferiority RCT provide preliminary support for a brief transdiagnostic group as an effective treatment for common mental health problems. However, more methodologically robust trials comparing groups to individual interventions in settings outside IAPT in the UK, and to a no-intervention arm, are required to substantiate the study findings. Transdiagnostic groups offer a pragmatic response to the prevalence and comorbidity of common mental health problems, such as greater ease of populating group interventions than recruiting those with a specific disorder (Norton & Barrera, Citation2012). Furthermore, groups can offer greater cost-effectiveness than individual therapies (Tucker & Oei, Citation2007), but data on the cost-effectiveness of transdiagnostic groups are very limited (Andersen et al., Citation2016). In the meantime, it is possible to consider the efficiency of TCC and low-intensity CBT given the offer available (i.e. the manualised session numbers and recommended delivery). Delivering TCC involves 12 h per clinician. The lack of a need for self-disclosure and “adult education” style delivery accommodates large numbers (e.g. 20 or more). Delivering low-intensity CBT (assuming the standard 6-sessions) involves three h per participant, per clinician. Within this “ideal” scenario and not taking into account broader costs, once you have more than four participants within TCC then it makes it more efficient; with eight in a course you would increase efficiency by 100%. However, data regarding the cost-effectiveness of TCC are under analysis and will be an important addition to our understanding of regarding service delivery advantages of transdiagnostic groups.
Acknowledgements
Many thanks to Rebekah Warke, Martina Slapkova, Saoirse Kennedy-Barton, Amel Hamlaoui, and Rebekah Amos (voluntary research assistants). Many thanks also to the team at Six Degrees Social Enterprise for all their support of the research programme that this study forms part of.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aderka, I. M., Nickerson, A., Bøe, H. J., & Hofmann, S. G. (2012). Sudden gains during psychological treatments of anxiety and depression: A meta-analysis. Journal of Consulting and Clinical Psychology, 80(1), 93. https://doi.org/10.1037/a0026455
- Aillon, J.-L., Ndetei, D. M., Khasakhala, L., Ngari, W. N., Achola, H. O., Akinyi, S., & Ribero, S. (2014). Prevalence, types and comorbidity of mental disorders in a Kenyan primary health centre. Social Psychiatry and Psychiatric Epidemiology, 49(8), 1257–1268. https://doi.org/10.1007/s00127-013-0755-2
- Ali, S., Rhodes, L., Moreea, O., McMillan, D., Gilbody, S., Leach, C., Lucock, M., Lutz, W., & Delgadillo, J. (2017). How durable is the effect of low intensity CBT for depression and anxiety? Remission and relapse in a longitudinal cohort study. Behaviour Research and Therapy, 94, 1–8. https://doi.org/10.1016/j.brat.2017.04.006
- Allart van Dam, E., Hosman, C. M. H., Hoogduin, C. A. L., & Schaap, C. P. D. R. (2003). The coping with depression course: Short-term outcomes and mediating effects of a randomized controlled trial in the treatment of subclinical depression. Behavior Therapy, 34(3), 381–396. https://doi.org/10.1016/S0005-7894(03)80007-2
- Alsawy, S., Mansell, W., Carey, T. A., McEvoy, P., & Tai, S. J. (2014). Science and practice of transdiagnostic CBT: A perceptual control theory (PCT) approach. International Journal of Cognitive Therapy, 7(4), 334–359. https://doi.org/10.1521/ijct.2014.7.4.334
- Andersen, P., Toner, P., Bland, M., & McMillan, D. (2016). Effectiveness of transdiagnostic cognitive behaviour therapy for anxiety and depression in adults: A systematic review and meta-analysis. Behavioural and Cognitive Psychotherapy, 44(6), 673–690. https://doi.org/10.1017/S1352465816000229
- Andersson, G., Hesser, H., Veilord, A., Svedling, L., Andersson, F., Sleman, O., Mauritzson, L., Sarkoh, A., Claesson, E., Zetterqvist, V., Lamminen, M., Eriksson, T., & Carlbring, P. (2013). Randomised controlled non-inferiority trial with 3-year follow-up of internet-delivered versus face-to-face group cognitive behavioural therapy for depression. Journal of Affective Disorders, 151(3), 986–994. https://doi.org/10.1016/j.jad.2013.08.022
- Barkham, M., Connell, J., Stiles, W. B., Miles, J. N., Margison, F., Evans, C., & Mellor-Clark, J. (2006). Dose-effect relations and responsive regulation of treatment duration: The good enough level. Journal of Consulting and Clinical Psychology, 74(1), 160. https://doi.org/10.1037/0022-006X.74.1.160
- Barlow, D. H., Farchione, T. J., Bullis, J. R., Gallagher, M. W., Murray Latin, H., Sauer-Zavala, S., Boswell, J. F. Bentley, K. H., Thompson-Hollands, J., Conklin, L. R., Boswell, J. F., Ametaj, A., Carl, J. R., Boettcher, H. T., & Cassiello-Robbins, C. (2017). The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry, 74(9), 875–884. https://doi.org/10.1001/jamapsychiatry.2017.2164
- Bennett Levy, J., Richards, D., Farrand, P., Richards, D., Farrand, P., Christensen, H., Griffiths, K., Kavanagh, D., Klein, B., Lau, M. A., Proudfoot, J., & Ritterband, L. (2010). Low intensity CBT interventions: A revolution in mental health care. In J. Bennett-Levy, J. White, & C. Williams (Eds.), Oxford guide to low intensity CBT interventions (pp. 3–18). Oxford University Press.
- Bower, P., & Gilbody, S. (2005). Stepped care in psychological therapies: Access, effectiveness and efficiency. Narrative literature review. The British Journal of Psychiatry, 186(1), 11–17. https://doi.org/10.1192/bjp.186.1.11
- Brockmeyer, T., Grosse Holtforth, M., Krieger, T., Altenstein, D., Doerig, N., Friederich, H.-C., & Bents, H. (2013). Ambivalence over emotional expression in major depression. Personality and Individual Differences, 54(7), 862–864. https://doi.org/10.1016/j.paid.2012.12.002
- Buckholtz, J. W., & Meyer-Lindenberg, A. (2012). Psychopathology and the human connectome: Toward a transdiagnostic model of risk for mental illness. Neuron, 74(6), 990–1004. https://doi.org/10.1016/j.neuron.2012.06.002
- Bullis, J. R., Sauer-Zavala, S., Bentley, K. H., Thompson-Hollands, J., Carl, J. R., & Barlow, D. H. (2015). The unified protocol for transdiagnostic treatment of emotional disorders: Preliminary exploration of effectiveness for group delivery. Behavior Modification, 39(2), 295–321. https://doi.org/10.1177/0145445514553094
- Burns, P., Kellett, S., & Donohoe, G. (2016). “Stress Control” as a large group psychoeducational intervention at step 2 of IAPT services: Acceptability of the approach and moderators of effectiveness. Behavioural and Cognitive Psychotherapy, 44(4), 431–443. https://doi.org/10.1017/S1352465815000491
- Cape, J., Whittington, C., Buszewicz, M., Wallace, P., & Underwood, L. (2010). Brief psychological therapies for anxiety and depression in primary care: Meta-analysis and meta-regression. BMC Medicine, 8(1), 1. https://doi.org/10.1186/1741-7015-8-38
- Carey, T. A. (2006). The method of levels: How to do psychotherapy without getting in the way. Living Control Systems Publ.
- Chorpita, B. F., & Barlow, D. H. (1998). The development of anxiety: The role of control in the early environment. Psychological Bulletin, 124(1), 3. https://doi.org/10.1037/0033-2909.124.1.3
- Coholic, D. A., Eys, M., McAlister, H., Sugeng, S., & Smith, D. J. S. W. I. M. H. (2018). A mixed method pilot study exploring the benefits of an arts-based mindfulness group intervention with adults experiencing anxiety and depression. Social Work in Mental Health, 16(5), 556–572. https://doi.org/10.1080/15332985.2018.1449774
- Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. https://doi.org/10.1186/1741-7015-11-126
- De Graaf, L., Gerhards, S., Arntz, A., Riper, H., Metsemakers, J., Evers, S., Severens, J. L., Widdershoven, G., & Huibers, M. (2009). Clinical effectiveness of online computerised cognitive–behavioural therapy without support for depression in primary care: Randomised trial. The British Journal of Psychiatry, 195(1), 73–80. https://doi.org/10.1192/bjp.bp.108.054429
- Delgadillo, J., McMillan, D., Leach, C., Lucock, M., Gilbody, S., & Wood, N. (2014). Benchmarking routine psychological services: A discussion of challenges and methods. Behavioural and Cognitive Psychotherapy, 42(1), 16–30. https://doi.org/10.1017/S135246581200080X
- Delgadillo, J., McMillan, D., Lucock, M., Leach, C., Ali, S., & Gilbody, S. (2014). Early changes, attrition, and dose–response in low intensity psychological interventions. British Journal of Clinical Psychology, 53(1), 114–130. https://doi.org/10.1111/bjc.12031
- Ellard, K. K., Fairholme, C. P., Boisseau, C. L., Farchione, T. J., & Barlow, D. H. (2010). Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice, 17(1), 88–101. https://doi.org/10.1016/j.cbpra.2009.06.002
- Fordham, B., Sugavanam, T., Edwards, K., Stallard, P., Howard, R., Das Nair, R., Copsey, B., Lee, H., Howick, J., & Hemming, K. (2021). The evidence for cognitive behavioural therapy in any condition, population or context: A meta-review of systematic reviews and panoramic meta-analysis. Psychological Medicine, 51(1), 21–29. https://doi.org/10.1017/S0033291720005292
- Glover, G., Webb, M., & Evison, F. (2010). Improving access to psychological therapies: A review of the progress made by sites in the first roll-out year. North East Public Health Observatory. http://www.iapt.nhs.uk/silo/files/iapt-a-review-of-the-progress-made-by-sites-in-the-first-roll8208-out-year.pdf
- Grawe, K. (2004). Neuropsychotherapy: How the neurosciences inform effective psychotherapy. Lawrence Erlbaum Associates.
- Gupta, S. K. (2011). Intention-to-treat concept: A review. Perspectives in Clinical Research, 2(3), 109. https://doi.org/10.4103/2229-3485.83221
- Harrow, M., Hansford, B. G., & Astrachan-Fletcher, E. B. (2009). Locus of control: Relation to schizophrenia, to recovery, and to depression and psychosis—A 15-year longitudinal study. Psychiatry Research, 168(3), 186–192. https://doi.org/10.1016/j.psychres.2008.06.002
- Healey, A., Mansell, W., & Tai, S. (2017). An experimental test of the role of control in spider fear. Journal of Anxiety Disorders, 49, 12–20. https://doi.org/10.1016/j.janxdis.2017.03.005
- Hedman, E., Andersson, G., Ljótsson, B., Andersson, E., Rück, C., Mörtberg, E., & Lindefors, N. (2011). Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non-inferiority trial. PloS One, 6(3), e18001. https://doi.org/10.1371/journal.pone.0018001
- Hofmann, S. G., & Smits, J. A. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry, 69(4), 621. https://doi.org/10.4088/JCP.v69n0415
- Huntley, A. L., Araya, R., & Salisbury, C. (2012). Group psychological therapies for depression in the community: Systematic review and meta-analysis. The British Journal of Psychiatry, 200(3), 184–190. https://doi.org/10.1192/bjp.bp.111.092049
- Jacobson, N. S., Roberts, L. J., Berns, S. B., & McGlinchey, J. B. (1999). Methods for defining and determining the clinical significance of treatment effects: Description, application, and alternatives. Journal of Consulting and Clinical Psychology, 67(3), 300. https://doi.org/10.1037/0022-006X.67.3.300
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to denning meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037/0022-006X.59.1.12
- Kelly, R. E., Mansell, W., & Wood, A. M. (2015). Goal conflict and well-being: A review and hierarchical model of goal conflict, ambivalence, self-discrepancy and self-concordance. Personality and Individual Differences, 85, 212–229. https://doi.org/10.1016/j.paid.2015.05.011
- Kounali, D., Button, K. S., Lewis, G., Gilbody, S., Kessler, D., Araya, R., Lewis, G., Duffy, L., Lanham, P., Peters, T. J., Wiles, N., & Lewis, G. (2022). How much change is enough? Evidence from a longitudinal study on depression in UK primary care. Psychological Medicine, 52(10), 1875–1882. https://doi.org/10.1017/S0033291720003700
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
- Laposa, J. M., Mancuso, E., Abraham, G., & Loli Dano, L. (2017). Unified protocol transdiagnostic treatment in group format: A preliminary investigation with anxious individuals. Behavior Modification, 41(2), 253–268. https://doi.org/10.1177/0145445516667664
- Liu, Q., He, H., Yang, J., Feng, X., Zhao, F., & Lyu, J. (2020). Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. Journal of Psychiatric Research, 126, 134–140. https://doi.org/10.1016/j.jpsychires.2019.08.002
- Lovell, K., Cox, D., Haddock, G., Jones, C., Raines, D., Garvey, R., Roberts, C., & Hadley, S. (2006). Telephone administered cognitive behaviour therapy for treatment of obsessive compulsive disorder: Randomised controlled non-inferiority trial. BMJ (Clinical Research Ed), 333(7574), 883. https://doi.org/10.1136/bmj.38940.355602.80
- Mansell, W. (2005). Control theory and psychopathology: An integrative approach. Psychology and Psychotherapy-Theory Research and Practice, 78(2), 141–178. https://doi.org/10.1348/147608304x21400
- Mansell, W., Carey, T. A., & Tai, S. J. (2012). A transdiagnostic approach to CBT using method of levels therapy: Distinctive features. Routledge.
- Mansell, W., Harvey, A., Watkins, E., & Shafran, R. (2009). Conceptual foundations of the transdiagnostic approach to CBT. Journal of Cognitive Psychotherapy, 23(1), 6–19. https://doi.org/10.1891/0889-8391.23.1.6
- Mayo-Wilson, E., Dias, S., Mavranezouli, I., Kew, K., Clark, D. M., Ades, A., & Pilling, S. (2014). Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry, 1(5), 368–376. https://doi.org/10.1016/S2215-0366(14)70329-3
- McEvoy, P. M., Nathan, P., & Norton, P. J. (2009). Efficacy of transdiagnostic treatments: A review of published outcome studies and future research directions. Journal of Cognitive Psychotherapy, 23(1), 20–33. https://doi.org/10.1891/0889-8391.23.1.20
- Mitchell, A. J., Vaze, A., & Rao, S. (2009). Clinical diagnosis of depression in primary care: A meta-analysis. The Lancet, 374(9690), 609–619. https://doi.org/10.1016/S0140-6736(09)60879-5
- Mofrad, L., Tiplady, A., Payne, D., & Freeston, M. J. T. C. B. T. (2020). Making friends with uncertainty: Experiences of developing a transdiagnostic group intervention targeting intolerance of uncertainty in IAPT. Feasibility, acceptability and implications ( p. 13). https://doi.org/10.1017/S1754470X20000495
- Morris, L. (2013). A pilot evaluation of a transdiagnostic group intervention for mental health problems in primary care. Clinical Psychology doctoral thesis, University of Manchester,
- Morris, S. E., & Cuthbert, B. N. (2012). Research domain criteria: Cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience, 14(1), 29. https://doi.org/10.31887/DCNS.2012.14.1/smorris
- Morris, L., Lovell, K., McEvoy, P., Emsley, R., Edge, D., Jacob, I., & Mansell, W. (2014). Primary care trial of efficacy of alternative modalities (PCTEAM): A 12-month randomized parallel group trial to establish whether the take control course is non-inferior to low intensity interventions in primary care mental health services. https://doi.org/10.13140/RG.2.2.18965.81125
- Morris, L., Mansell, W., Amos, R., & Edge, D. (2018). Experiences of a transdiagnostic group, the take control course, for clients with common mental health problems: A qualitative study. Clinical Psychology & Psychotherapy, 25(5), 730–744. https://doi.org/10.1002/cpp.2303
- Morris, L., Mansell, W., Emsley, R., Bates, R., Comiskey, J., Pistorius, E., & McEvoy, P. (2015). Prospective cohort feasibility study of a transdiagnostic group intervention for common mental health problems: The take control course. Psychology and Psychotherapy: Theory, Research and Practice, 89(2), 163–180. https://doi.org/10.1111/papt.12070
- Morris, L., Mansell, W., & McEvoy, P. (2016). The take control course: Conceptual rationale for the development of a transdiagnostic group for common mental health problems. Frontiers in Psychology, 7, 99. https://doi.org/10.3389/fpsyg.2016.00099
- Morris, L., McEvoy, P., Bates, R., Wallwork, T., Comiskey, J., & Mansell, W. (2018). Transdiagnostic group therapy training and implementation: The take control course. Elsevier.
- Newby, J. M., McKinnon, A., Kuyken, W., Gilbody, S., & Dalgleish, T. (2015). Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clinical Psychology Review, 40, 91–110. https://doi.org/10.1016/j.cpr.2015.06.002
- Nieuwsma, J. A., Trivedi, R. B., McDuffie, J., Kronish, I., Benjamin, D., & Williams, J. W. Brief psychotherapy for depression: A systematic review and meta-analysis. (2012). International Journal of Psychiatry in Medicine, 43(2), 129–151. doi. https://doi.org/10.2190/PM.43.2.c
- Norton, P. J. (2012). A randomized clinical trial of transdiagnostic cognitive-behavioral treatments for anxiety disorder by comparison to relaxation training. Behavior Therapy, 43(3), 506–517. https://doi.org/10.1016/j.beth.2010.08.011
- Norton, P. J., & Barrera, T. L. (2012). Transdiagnostic versus diagnosis-specific CBT for anxiety disorders: A preliminary randomized controlled noninferiority trial. Depression and Anxiety, 29(10), 874–882. https://doi.org/10.1002/da.21974
- Norton, P. J., & Hope, D. A. (2008). The “Anxiety Treatment Protocol” a group case study demonstration of a transdiagnostic group cognitive—Behavioral therapy for anxiety disorders. Clinical Case Studies, 7(6), 538–554. https://doi.org/10.1177/1534650108321307
- Norton, P. J., & Philipp, L. M. (2008). Transdiagnostic approaches to the treatment of anxiety disorders: A quantitative review. Psychotherapy, 45(2), 214–226. https://doi.org/10.1037/0033-3204.45.2.214
- Norton, P. J., & Price, E. C. (2007). A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. The Journal of Nervous and Mental Disease, 195(6), 521–531. https://doi.org/10.1097/01.nmd.0000253843.70149.9a
- O’Brien, A., Fahmy, R., & Singh, S. P. (2009). Disengagement from mental health services. Social Psychiatry and Psychiatric Epidemiology, 44(7), 558–568. https://doi.org/10.1007/s00127-008-0476-0
- Osma, J., Peris-Baquero, O., Suso-Ribera, C., Farchione, T., & Barlow, D. J. P. R. (2022). Effectiveness of the unified protocol for transdiagnostic treatment of emotional disorders in group format in Spain: Results from a randomized controlled trial with 6-months follow-up. Psychotherapy Research, 32(3), 329–342. https://doi.org/10.1080/10503307.2021.1939190
- Piaggio, G., Elbourne, D. R., Pocock, S. J., Evans, S. J., Altman, D. G., & Group, C. (2012). Reporting of noninferiority and equivalence randomized trials: Extension of the CONSORT 2010 statement. Jama, 308(24), 2594–2604. https://doi.org/10.1001/jama.2012.87802
- Powers, W. T. (1973). Behavior : The control of perception. Aldine.
- Priemer, M., & Talbot, F. (2013). CBT guided self-help compares favourably to gold standard therapist-administered CBT and shows unique benefits over traditional treatment. Behaviour Change, 30(4), 227–240. https://doi.org/10.1017/bec.2013.22
- Reinholt, N., Hvenegaard, M., Christensen, A. B., Eskildsen, A., Hjorthøj, C., Poulsen, S., Arendt, M., Rosenberg, N., Gryesten, J., Aharoni, R., Alrø, A., Christensen, C., & Arnfred, S. M. (2022). Transdiagnostic versus diagnosis-specific group cognitive behavioral therapy for anxiety disorders and depression: A randomized controlled trial. Psychotherapy and Psychosomatics, 91(1), 36–49. https://doi.org/10.1159/000516380
- Reinholt, N., & Krogh, J. (2014). Efficacy of transdiagnostic cognitive behaviour therapy for anxiety disorders: A systematic review and meta-analysis of published outcome studies. Cognitive Behaviour Therapy, 43(3), 171–184. https://doi.org/10.1080/16506073.2014.897367
- Richards, D. A., & Borglin, G. (2011). Implementation of psychological therapies for anxiety and depression in routine practice: Two year prospective cohort study. Journal of Affective Disorders, 133(1), 51–60. https://doi.org/10.1016/j.jad.2011.03.024
- Richards, D. A., Bower, P., Pagel, C., Weaver, A., Utley, M., Cape, J., Leibowitz, J., Pilling, S., Lovell, K., Gilbody, S., Leibowitz, J., Owens, L., Paxton, R., Hennessy, S., Simpson, A., Gallivan, S., Tomson, D., & Vasilakis, C. (2012). Delivering stepped care: An analysis of implementation in routine practice. Implementation Science : IS, 7(3). https://doi.org/10.1186/1748-5908-7-3
- Richards, D. A., & Suckling, R. (2009). Improving access to psychological therapies: Phase IV prospective cohort study. British Journal of Clinical Psychology, 48(4), 377–396. https://doi.org/10.1348/014466509X405178
- Richards, D., Timulak, L., O’Brien, E., Hayes, C., Vigano, N., Sharry, J., & Doherty, G. (2015). A randomized controlled trial of an internet-delivered treatment: Its potential as a low-intensity community intervention for adults with symptoms of depression. Behaviour Research and Therapy, 75, 20–31. https://doi.org/10.1016/j.brat.2015.10.005
- Robinson, L., Delgadillo, J., & Kellett, S. (2020). The dose-response effect in routinely delivered psychological therapies: A systematic review. J Psychotherapy Research, 30(1), 79–96. https://doi.org/10.1080/10503307.2019.1566676
- Robinson, L., Kellett, S., & Delgadillo, J. (2020). Dose‐response patterns in low and high intensity cognitive behavioral therapy for common mental health problems. J Depression Anxiety, 37(3), 285–294. https://doi.org/10.1002/da.22999
- Sauer-Zavala, S., Gutner, C. A., Farchione, T. J., Boettcher, H. T., Bullis, J. R., & Barlow, D. H. (2017). Current definitions of “transdiagnostic” in treatment development: A search for consensus. Behavior Therapy, 48(1), 128–138. https://doi.org/10.1016/j.beth.2016.09.004
- Schauman, O., & Mansell, W. (2012). Processes underlying ambivalence in help‐seeking: The loss of valued control model. Clinical Psychology: Science and Practice, 19(2), 107–124. https://doi.org/10.1111/j.1468-2850.2012.01277.x
- Shafran, R., Myles-Hooton, P., Bennett, S., Öst, L.-G.J.B.R, & Therapy. (2021). The concept and definition of low intensity cognitive behaviour therapy. Behaviour Research and Therapy, 138, 103803. https://doi.org/10.1016/j.brat.2021.103803
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Teachman, B. A., Joormann, J., Steinman, S. A., & Gotlib, I. H. (2012). Automaticity in anxiety disorders and major depressive disorder. Clinical Psychology Review, 32(6), 575–603. https://doi.org/10.1016/j.cpr.2012.06.004
- Tucker, M., & Oei, T. P. (2007). Is group more cost effective than individual cognitive behaviour therapy? The evidence is not solid yet. Behavioural and Cognitive Psychotherapy, 35(1), 77. https://doi.org/10.1017/S1352465806003134
- Wilamowska, Z. A., Thompson‐hollands, J., Fairholme, C. P., Ellard, K. K., Farchione, T. J., & Barlow, D. H. (2010). Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depression and Anxiety, 27(10), 882–890. https://doi.org/10.1002/da.20735
- Yang, X., Fang, Y., Chen, H., Zhang, T., Yin, X., Man, J., Yang, L., & Lu, M. (2021). Global, regional and national burden of anxiety disorders from 1990 to 2019: Results from the Global Burden of Disease Study 2019. Epidemiology and Psychiatric Sciences, 30, e36. https://doi.org/10.1017/S2045796021000275