ABSTRACT
The aim of this observational study was to examine the predictive and discriminant validity of patient motivation and adherence in metacognitive therapy (MCT) for depression. Motivational development for recovered- and non-recovered patients was also investigated. Motivation in sessions 1, 4, and 7 was measured using the Motivational Interviewing Skill Code 2.5 (MISC) in a 10-session trial of MCT for depression (N = 37). Adherence was assessed with the CBT compliance measure in session 7. The Beck Depression Inventory measured treatment outcome at 3-year follow-up. Recovered patients developed significantly more change talk and taking steps, and less sustain talk, as therapy progressed, compared to non-recovered patients. Evidence of the predictive validity of motivation in sessions 1 and 4 was limited. Higher sustain talk and taking steps in session 7 were significant predictors of more and less depressive symptoms, respectively. There was a moderate-strong correlation between motivation and adherence. The results confirm the predictive value of MISC in sessions 7 of MCT for depression, and establish differential motivational development between recovered and non-recovered patients. Subsequent research should clarify the discriminant validity and temporal relationships between motivation, adherence, and other clinical variables.
Introduction
Metacognitive therapy (MCT; Wells, Citation2009) has demonstrated promising results in the treatment of depression (Normann & Morina, Citation2018). The Motivational Interviewing literature (MI; Miller & Rollnick, Citation2012) has underlined the importance of patient motivation in depression treatment (Keeley et al., Citation2016). Yet, research on motivation in MCT for depression is lacking. Patient motivation has been defined as “the probability that a person will enter into, continue, and adhere to a specific change strategy” (Miller & Rollnick, Citation1991, p. 19). In depression, lack of motivation towards reducing rumination is suggested to maintain the disorder and impede treatment response (Nolen-Hoeksema et al., Citation2008). Self-report measures of motivation have yielded inconsistent findings as treatment predictors (Lombardi et al., Citation2014; Solem et al., Citation2016). This could be rooted in questionnaires’ susceptibility to social desirability bias and ceiling effects. Thus, development and validation of reliable measures of motivation are necessary.
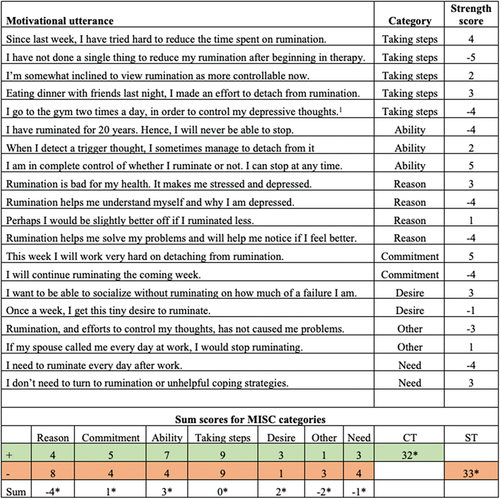
The observation-based instrument entitled Motivational Interviewing Skill Code (MISC; Glynn & Moyers, Citation2009) measures patients’ motivation, and could be a viable alternative to self-report assessment. The MISC version 2.5 (Houck et al., Citation2011) quantifies patients’ in-session motivational utterances, concerning a specified target behavior (e.g., rumination). Motivational language is quantified into sustain talk (ST; utterances arguing against target behavior change) or change talk (CT; utterances arguing for target behavior change), with scores ranging from −5 to −1 (ST) and +1 to +5 (CT), depending on the motivational strength of the utterance (Houck et al., Citation2011). Additionally, each motivational utterance is categorized into one of seven categories: Reason, desire, commitment, taking steps, need, other, and ability. Commitment pertains to statements where the patient commits to changing or maintaining the target behavior. Taking steps concerns recent efforts by the patient to change or maintain the target behavior. presents this study’s employed coding system, with example-utterances.
Figure 1. Illustration of the utilized coding system (MISC 2.5; Houck et al., Citation2011). CT and ST scores were summed for each category, as displayed. CT: change talk; ST: sustain talk; +: CT; −: ST. *The variables included in analyses. 1use of distraction and thought control, which are considered components of the cognitive attentional syndrome in MCT for depression.
According to the technical MI-hypothesis, ST and CT impedes and facilitates target behavior change, respectively (Miller & Rollnick, Citation2012). Conceptually, the change-facilitating effects of CT, as well as the change-disrupting consequences of ST, are related to cognitive dissonance theory (Festinger, Citation1957, Citation1962) and self-perception theory (Bem, Citation1967, Citation1972). Only one study has investigated MISC’s predictive value of outcome in depression treatment. Ewbank et al. (Citation2020) included patients with depression (n = 11,333) in a transdiagnostic sample (N = 28,809). The study encoded CT- and ST-frequency in the first session of text-based internet-enabled Cognitive Behavioral Therapy (CBT). High ST diminished reliable improvement in therapy, whereas high CT enhanced such improvement. However, there is no data on CT and ST in face-to-face treatment of depression.
The MISC-literature is more developed in the domain of generalized anxiety disorder (GAD). The overlap between GAD and depression is considerable. Thus, the MISC-studies of GAD constitutes the best available background literature for this study. Studies have established the frequency of ST in initial treatment sessions of CBT for GAD as a significant predictor of higher worry-levels after treatment (Button et al., Citation2015; Lombardi et al., Citation2014; Sijercic et al., Citation2016). CT was not a significant predictor of treatment outcome in these studies. Contrastingly, Goodwin et al. (Citation2019) and Poulin et al. (Citation2019) confirmed that both CT- and ST-frequency in session 1 were significantly associated with better and worse treatment outcome, respectively.
Joramo et al. (Citation2021) examined the predictive capacity of CT and ST in a trial of MCT and CBT for GAD. Higher frequency of CT and ST in session 4 were significant predictors of better and worse treatment outcome, respectively. Reduction in ST from session 1 to 4 was a significant predictor of lower worry-scores at post-treatment. Positive (i.e. CT) commitment in session 1 and positive taking steps in session 4 were significantly associated with better treatment outcome.
Lassen et al. (Citation2022) examined motivational language in metacognitive group therapy for GAD, applying identical coding-procedures as the current study. As therapy progressed, patients responding to treatment developed significantly more CT and positive (i.e. CT) taking steps utterances, and significantly less ST, compared to the non-responders. Furthermore, CT and ST in sessions 4 and 7 were significant predictors of lower and higher worry scores at post-treatment, respectively. The effect was especially pronounced for positive taking steps. The study discussed whether taking steps was confounded with treatment adherence. The discussion was, however, curtailed by the lack of data to clarify the discriminant validity of taking steps and adherence, as well as the constructs’ relative impact on treatment outcome. Yet, no studies have examined this.
The aim of this study was to examine the predictive validity of motivation and adherence for treatment outcome in MCT for depression. Moreover, the study investigated whether recovered patients’ motivational development across sessions 1, 4, and 7, diverged from non-recovered patients motivation. This study is the first to examine the role of patient motivation and adherence in MCT for depression. The first hypothesis postulated that recovered patients develop higher CT and taking steps, and lower ST, during treatment compared to non-recovered patients. This hypothesis was hinged on the presented theory and the findings of Lassen et al. (Citation2022). The second hypothesis theorized that motivation in session 4 and 7 would predict treatment outcome at 3-year follow-up. Based on the presented theory, as well as the results of Joramo et al. (Citation2021) and Lassen et al. (Citation2022), ST was hypothesized to predict more symptoms, whereas CT (including positive commitment and taking steps) was presumed to predict less symptoms. Due to heterogeneity in previous research findings, there is uncertainty associated with the predictive validity of motivational utterances in session 1. The third hypothesis was exploratory, due to the lack of background literature. Based on the theoretical discussion of Lassen et al. (Citation2022), it examined the discriminant validity and relative impact on treatment outcome of motivation (CT, ST, and taking steps) and adherence.
Methods
Participants and procedure
This study is an observational analysis based on a trial of MCT for depression (Hagen et al., Citation2017). One-hundred and five patients were assessed for eligibility using clinician- administered interviews. Diagnoses were established using the Structured Clinical Interview for the DSM-IV axis I (First et al., Citation2002), the Structured Clinical Interview for DSM-IV axis II (First et al., Citation1997), and the Hamilton Rating Scale for Depression (Hamilton, Citation1967).
Inclusion criteria were major depressive disorder (mild, moderate, severe; single episode or recurrent) as primary disorder, written informed consent, and age 18 or older. A total of 66 patients were excluded due to other primary disorder (n = 39), cluster A or B personality disorder (n = 10), no psychiatric diagnosis (n = 8), subclinical depression (n = 5), somatic diseases (n = 2), substance dependence (n = 1), and antipsychotic medication (n = 1). Further exclusion criteria included known somatic diseases, psychosis, current suicidal intent, PTSD, substance dependence, not willing to accept random allocation, use of benzodiazepines during the trial, and concurrent therapy elsewhere.
Accordingly, thirty-nine patients were included and randomized to immediate MCT (n = 20) or a waiting list (n = 19). Patients in both conditions received 10 therapy sessions (after a 10-week delay in the waiting list). Two patients in the waiting list dropped out before starting treatment, due to receiving treatment elsewhere. Thus, video therapy-recordings of 37 (age: M = 33.86, SD = 10.52) patients were available for this study. The majority had recurrent depressive disorder (n = 31), whereas six were diagnosed with a single depressive episode. One, 22, and 14 patients had mild, moderate, and severe depression, respectively. displays further sample characteristics.
Table 1. Sample demographic and diagnostic characteristics at pre-treatment (N = 37).
Motivation was coded in sessions 1, 4, and 7. The coders were three graduate students in clinical psychology. Adherence was coded in session 7. Coders were blinded to treatment outcome. Due to damaged DVDs, some recordings were unavailable. In these instances, the nearest recorded session was encoded. Ten percent of the study’s coded recordings were randomly selected for double coding. Inter-rater reliability analyses were performed using two-way mixed, absolute agreement, intraclass correlation coefficients (ICCs). ICCs were 0.92 for CT, 0.89 for ST, and 0.96 for taking steps. The inter-rater estimates for CT and taking steps were within the range of excellent inter-rater agreement, whereas the ST inter-rater estimate was indicative of good inter-rater agreement (Koo & Li, Citation2016).
Treatment
The treatment was MCT for depression (Wells, Citation2009). Important therapeutic interventions included socialization and case formulation, increased meta-awareness of rumination triggers, elevated metacognitive control using detached mindfulness and the attention training technique, modification of positive and negative metacognitions, and relapse prevention (Wells, Citation2009). Motivation was not directly addressed during therapy. No MI-interventions were used, but the process of challenging metacognitions often elicited utterances regarding patients’ readiness or resistance to change.
Therapists
Four senior clinical psychologists (level-1 MCT-therapists) delivered the treatment. The four therapists treated similar number of patients (8, 9, 9, and 11). The originator of MCT supervised the clinicians and performed quality assurance. No formal rating of therapist competence or adherence were applied. There were no significant differences between the clinicians’ respective patients’ BDI scores at pre-treatment, post-treatment, or 3-year follow-up. The same held true for the clinician’s respective patients’ adherence in session 7, and CT, ST, and taking steps in sessions 1, 4, and 7 (supplemental ). However, there was a difference in therapists’ patients’ ST in session 1 (F [3, 33] = 6.25, p = .002).
Measures
The Motivational Interview Skill Code version 2.5 (MISC 2.5; Houck et al., Citation2011) measured patient motivation. Accordingly, motivational utterances were quantified and categorized as described in the introduction. The target behaviors were defined in accordance with the metacognitive model of depression (i.e., rumination, worry, positive and negative metacognitions, threat monitoring, and dysfunctional coping strategies). Neutral utterances (i.e., follow/neutral/ask) and utterances unrelated to the target behaviors were left uncoded. displays the coding system, examples of motivational utterances from the current study, and data handling procedures. The MISC was developed on the basis of MI theory (Miller & Rollnick, Citation1991; Miller & Rose, Citation2009), and has been thoroughly empirically validated (e.g. Miller & Mount, Citation2001; Moyers et al., Citation2005).
Patients’ adherence in session 7 was measured with the CBT compliance measure (CCM; Wootton et al., Citation2021), which is an 8-item (0–4 scale) observational instrument. Examples of items include the patients’ understanding of treatment goals, and cooperation in the process of cognitive- and behavioral restructuring. A total score is calculated by averaging item scores, with higher scores indicating higher adherence. CCM has demonstrated good validity and inter-rater reliability (Wootton et al., Citation2021). As the therapy in the current study was MCT, the item concerning cognitive restructuring was adapted to concern modification of metacognitions.
Depressive symptomatology was measured with the Beck Depression Inventory (BDI; Beck et al., Citation1961). The self-report questionnaire consists of 21 items which are scored on a 0–3 scale. A total BDI-score of 0–9, 10–18, 19–29, and 30–63 is indicative of no, mild, moderate, and severe depression, respectively.
Statistical analyses
Pearson’s correlation investigated the relationships between motivation, adherence, and treatment outcome. Two linear regression models were applied. Both models controlled for depressive symptoms at baseline in step 1, and adherence in step 2. Model 1 tested the predictive validity of CT and ST in session 7. Model 2 examined the predictive capacity of taking steps in sessions 4 and 7. An effect size (correlation: r; regression: β) of above .10, .30, and .50 was considered a small, moderate, and large effect size, respectively (Cohen, Citation1988).
Three factorial repeated-measures ANOVAs were applied to investigate differential motivational development. To ensure groups of approximately the same size, conservative recovery criteria were applied. Patients who met the recovery criteria of Frank et al. (Citation1991; BDI ≤ 8) at post-treatment and all times during the 3-year follow-up measurement, were considered recovered. Those who did not, were considered non-recovered. Mauchly’s test of sphericity was significant, with Greenhouse-Geisser ε-estimates exceeding 0.75, in the analyses of ST and taking steps. Thus, Greenhouse-Geisser corrected F-statistics were employed. A Partial Eta Squared (ηp2) above .03, .13, and .26 was considered a small, moderate, and large effect size, respectively (Bakeman, Citation2005).
Due to non-participation in the 3-year follow-up, five patients had missing BDI scores. Little’s MCAR test was not significant (χ2[937] = 416.44, p = 1.00), indicating the data was missing at random. Imputation was performed with expectation-maximization (EM). Sensitivity analyses (raw data and multiple imputation) were applied to investigate whether the EM-imputation impacted the results. The dichotomization of recovered and non-recovered patients was based on EM-imputed data for 3-year follow-up BDI scores. Dichotomization based on raw data produced identical groups.
Results
summarizes descriptive statistics for motivation and adherence. Patients uttered approximately twice as strong CT compared to ST, across sessions. The patients expressed few ability-, desire- and need-utterances across sessions. Positive other- and reason-utterances were relatively strong in session 1. The strength of ability- and reason-utterances took a V-shape during therapy, and the development of taking steps took an A-shape. Commitment-utterances increased in strength. The strength of other-, need-, and desire-utterances decreased as therapy progressed. also displays descriptive statistics for repeated measures of the BDI. Depressive symptoms decreased throughout treatment. The imputation procedures produced converging BDI-estimates.
Table 2. Descriptive statistics (N = 37).
The discriminant validity of patient adherence and different categories of motivation
There were statistically significant associations between adherence in session 7, and CT (r = .75, p < .001), ST (r = −.60, p < .001), taking steps (r = .64, p < .001), ability (r = .63, p < .001), reason (r = .59, p < .001), commitment (r = .44, p < .01), and need (r = .34, p < .05). The effect sizes ranged from moderate to large. Desire and other statements showed no statistically significance with adherence.
Predicting long-term treatment outcome using motivation and adherence
The evidence for statistically significant relationships between sessions 1 and 4 MISC-scores and treatment outcome was scarce (see supplemental Table 2–4). No session 1- and 4-variables showed statistically significant correlations with outcome when Bonferroni-corrected correlations were applied.
displays the regression models. Both models accounted for 43% variance in outcome. Motivation explained outcome variance beyond adherence in both models. In model 1, more symptoms at baseline and higher ST in session 7, were statistically significant predictors of more depressive symptoms at 3-year follow-up. The effect size of symptoms at baseline and ST in session 7 were small and moderate, respectively. Neither adherence nor CT were statistically significant predictors in the last step of the equation. In model 2, more positive taking steps in session 7 was a statistically significant predictor of less depressive symptoms at 3-year follow-up. The effect size was large. The other predictors were not statistically significant in the last step of the equation. The Durbin-Watson statistics were 1.15 (model 1) and 1.27 (model 2), indicating acceptable autocorrelation. No issues with multicollinearity were found (VIF = 1.16–2.69). Results diverged marginally in sensitivity analyses utilizing raw data (model 1 and 2: R2 change was no longer statistically significant for adherence; see supplemental table 5).
Table 3. Predicting depressive symptoms at 3-year follow-up using motivation and adherence (N = 37).
Motivational development
Pertaining to changes in CT across sessions 1, 4 and 7, there was a moderate, statistically significant effect of time (F [2, 70] = 6.04, p = .004, ηp2 = .15). The analyses unveiled a moderate, statistically significant interactional effect between group and time on CT scores (F [2, 70] = 6.90, p = .002, ηp2 = .17). Recovered and non-recovered patients had different development of CT across sessions. Recovered patients developed stronger CT as therapy progressed, compared to their non-recovered counterparts (see ).
Figure 2. Graphs of estimated marginal means of motivational utterances in sessions 1, 4, and 7 for recovered and non-recovered patients. Dependent variable: MISC strength-scores.
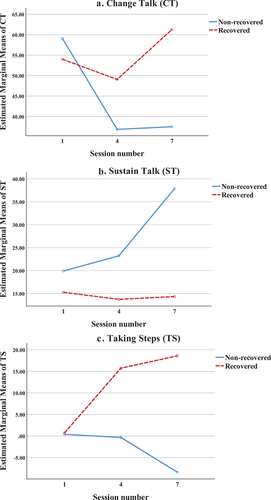
Concerning changes in ST across sessions, there was a moderate, statistically significant effect of time (F [1.68, 58.76] = 5.26, p = .011, ηp2 = .13). The results revealed a moderate, statistically significant interaction effect between time and group on ST scores (F [1.68, 58.76] = 5.78, p = .008, ηp2 = .14). This result indicates that the development of ST differed between recovered and non-recovered patients as therapy progressed. Non-recovered patients developed significantly stronger ST within the course of therapy, compared to the patients in the recovered group (see ).
Regarding development of taking steps across sessions, there was a small, statistically significant effect of time (F [1.64, 57.24] = 4.66, p = .019, ηp2 = .12). The results revealed a large, statistically significant interaction effect between time and group on taking steps-scores (F [1.64, 57.24] = 16.01, p < .001, ηp2 = .31). Thus, there was differential development of taking steps strength-scores between recovered and non-recovered patients. Recovered patients developed significantly stronger taking steps -scores as therapy progressed, compared to the non-recovered patients (see ).
There were no statistically significant time-group interaction effects for the other categories of motivation. There was a statistically significant difference in adherence between recovered (M = 3.61, SD = 0.32) and non-recovered (M = 3.08, SD = 0.51) patients in session 7 (t[35] = −3.54, p = .001, d = 1.24).
Discussion
Summary and main findings
This study set out to examine potential differential development of motivation between recovered- and non-recovered patients, as well as the predictive validity of motivation and adherence on treatment outcome, in a trial of metacognitive therapy for depression. Furthermore, the discriminant validity between adherence and motivation was examined.
The results revealed differential motivational development between recovered and non-recovered patients. Recovered patients developed more CT and less ST, compared to non-recovered patients. This trend was particularly pronounced for taking steps. Furthermore, ST and taking steps in session 7 were significant predictors of higher and lower depressive symptomatology at 3-year follow-up, respectively. There were no significant associations between motivational utterances in sessions 1 and 4, and treatment outcome. Finally, there were significant relationships between motivation factors and adherence in session 7.
Differential motivational development between recovered and non-recovered patients
The development of taking steps among the recovered patients, could indicate enhanced motivation to practice metacognitive techniques between sessions. Dialogue regarding practice of target behavior change (taking steps) might diminish resistance, and bolster patients’ commitment to change, as postulated by MI-theory (Miller & Rose, Citation2009). Such dialogue could also resolve potential misunderstandings in the patients’ appreciation and execution of metacognitive techniques.
Differential motivational development between recovered and non-recovered patients, might reflect relational-motivational processes (Miller & Rose, Citation2009). Sijercic et al. (Citation2016) demonstrated that ST that opposes the therapist, had superior predictive validity of treatment outcome, relative to ST arguing against target behavior change. Also, higher ST predicts poorer working alliance throughout therapy (Norouzian et al., Citation2020). Overall, these results might indicate interactional effects between motivational and alliance variables during the course of therapy. Future research should map such conceivable effects, to examine whether motivational and alliance variables interact over time. Such research could elucidate important precursors of favorable alliance and motivational development in therapy.
The predictive capacity of motivational language on treatment outcome
No session 1 and 4 motivational variables correlated significantly with outcome. These results diverge partially from previous MISC-studies within the CBT-domain, which have established initial ST as a predictor of poor treatment outcome (Ewbank et al., Citation2020; Lombardi et al., Citation2014). However, neither session 1 CT or ST predicted treatment outcome in previous MCT-studies on GAD (Joramo et al., Citation2021; Lassen et al., Citation2022). Finally, the insignificant session 4-findings contradict those of Joramo et al. (Citation2021) and Lassen et al. (Citation2022), who demonstrated the predictive validity of CT, ST, and taking steps in session 4. A possible reason for the divergent results could be that our study was on depression and used a longer follow-up period, but it could also be due to lower statistical power. Consequently, there is a risk of type II errors, as the effect sizes are modest.
In session 7, ST and taking steps were significant predictors of higher and lower depressive symptomatology, respectively. These findings confirm the change-inhibiting effect of ST, and the change-facilitating effect of taking steps (Miller & Rose, Citation2009). Thus, focus on motivation throughout therapy could be imperative. However, increasing predictive capacity of motivation as therapy progressed, could suggest that the development and predictive validity of motivation could be secondary to other change-mechanisms (e.g. symptoms and metacognitions). Moreover, the session 7 ST-finding is consistent with the results of Lassen et al. (Citation2022). Discordant with the current findings, Lassen et al. (Citation2022) established the predictive validity of CT in session 7. In addition to previously discussed reasons for divergent findings, the discrepant session 7 CT-results could be rooted in different treatment formats (individual- versus group). Thus, group processes (e.g. social facilitation, observational learning) could influence motivation. The session 7 taking steps-finding corroborates the results of Lassen et al. (Citation2022). Thus, there is preliminary evidence of the importance of taking steps in later phases of MCT for anxious-depressive disorders. These findings accentuate the importance of in-session discussion of patients’ endeavors to practice target behavior change (taking steps). It appears that the motivation for practicing target behavior change, not the ability of target behavior change, is the deciding factor for outcome.
Discriminant validity of patient adherence and motivation
There were significant moderate to strong correlations between adherence and motivation. Moreover, adherence significantly explained variance in treatment outcome, but was not a significant predictor in the last steps of the regression models. ST and taking steps in session 7 predicted treatment outcome above and beyond adherence. These results indicate that motivation and adherence are strongly related, but differ in their relative impact on treatment outcome. There is potential for overlap in the definitions of taking steps and adherence. The absence of background literature impedes comparison of results. However, adherence predicts outcome in CBT for anxious-depressive disorders (Glenn et al., Citation2013). Furthermore, higher motivation could be indicative of higher adherence (Alfonsson et al., Citation2016). These findings resonate well with the technical MI-hypothesis (Miller & Rose, Citation2009) and adherence could mediate the relationship between motivation and outcome.
Limitations and implications
This study has limitations that warrants consideration. Due to the sample size, there is a risk of elevated family-wise error-rates. Furthermore, a multilevel model could have suited the data. However, due to the sample size, multilevel modelling with three levels was inapplicable (Maas & Hox, Citation2005). Moreover, a larger sample would have enabled random intercept cross-lagged panel analyses. Such analyses could have assessed the temporal dynamics of motivation, adherence, metacognitions, and depressive symptoms throughout therapy. Change in these variables might precede motivational changes. Future research should include repeated measurement of these variables, in samples sufficiently large for random intercept cross-lagged panel models. The modest sample size also limits the generalizability of the results. Future research, using larger samples, should investigate possible predictors of motivation (e.g. previous treatment attempts, comorbidity, and use of SSRIs). Finally, although coders were blinded for treatment outcome, absolute blinding was impossible, as some patients spontaneously reported symptom-improvement or lack thereof.
Due to the aforementioned limitations, the results and their implications should be interpreted with caution. Therapists should monitor patients’ motivational utterances throughout the course of depression treatment. A reduction in CT and taking steps, combined with increased ST, could be a cause for concern. Dialogue regarding practice of target behavior change (taking steps) in the middle to late treatment phases could be of special importance for treatment outcome.
Author contributions
Design: ERL and SS. MISC-coding: ERL, SAL and IH. CCM-coding: ERL. Statistical analyses: ERL. First draft of manuscript: ERL. Therapists: RH, SS, OH, and LEOK. Principal researcher: RH. Ethical approval: RH. All authors revised the manuscript and approved its submission.
Ethical approval
The study obtained ethical approval from the Regional Committee for Medical and Health Research Ethics in Norway (REK Midt, ref.nr. 2011/1138).
Informed consent from participants
All participants provided written informed consent before inclusion.
Supplemental Material
Download MS Word (35.7 KB)Disclosure statement
The authors declare no competing interests.
Data availability statement
The data that support the findings of this study are available from the corresponding author, ERL, upon reasonable request.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/16506073.2023.2289863
References
- Alfonsson, S., Olsson, E., & Hursti, T. (2016). Motivation and treatment credibility predicts dropout, treatment adherence, and clinical outcomes in an internet-based cognitive behavioral relaxation program: A randomized controlled trial. Journal of Medical Internet Research, 18(3), e5352. https://doi.org/10.2196/jmir.5352
- Bakeman, R. (2005). Recommended effect size statistics for repeated measures designs. Behavior Research Methods, 37(3), 379–384. https://doi.org/10.3758/BF03192707
- Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004
- Bem, D. J. (1967). Self-perception: An alternative interpretation of cognitive dissonance phenomena. Psychological Review, 74(3), 183. https://doi.org/10.1037/h0024835
- Bem, D. J. (1972). Self-perception theory. In I. L. Berkowitz (Ed.), Advances in experimental social psychology (Vol. 6, pp. 1–62). Academic Press.
- Button, M. L., Westra, H. A., Hara, K. M., & Aviram, A. (2015). Disentangling the impact of resistance and ambivalence on therapy outcomes in cognitive behavioural therapy for generalized anxiety disorder. Cognitive Behaviour Therapy, 44(1), 44–53. https://doi.org/10.1080/16506073.2014.959038
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum.
- Ewbank, M., Cummins, R., Tablan, V., Catarino, A., Buchholz, S., & Blackwell, A. (2020). Understanding the relationship between patient language and outcomes in internet-enabled cognitive behavioural therapy: A deep learning approach to automatic coding of session transcripts. Psychotherapy Research, 31(3), 1–13. https://doi.org/10.1080/10503307.2020.1788740
- Festinger, L. (1957). A theory of cognitive dissonance. Stanford University Press.
- Festinger, L. (1962). Cognitive dissonance. Scientific American, 207(4), 93–106. https://doi.org/10.1038/scientificamerican1062-93
- First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2002). Structured Clinical Interview for DSM-IV-TR axis I disorders, Research version, patient edition (SCID- I/P). Biometrics Research, New York State Psychiatric Institute.
- First, M. B., Spitzer, R. L., Williams, J. B. W., & Benjamin, L. S. (1997). Structured Clinical Interview for DSM-IV axis II personality disorders (SCID-II). American Psychiatric Press, Inc.
- Frank, E., Prien, R. F., Jarrett, R. B., Keller, M. B., Kupfer, D. J., Lavori, P. W., Rush, A. J., & Weissman, M. M. (1991). Conceptualization and rationale for consensus definitions of terms in major depressive disorder: Remission, recovery, relapse, and recurrence. Archives of General Psychiatry, 48(9), 851–855. https://doi.org/10.1001/archpsyc.1991.01810330075011
- Glenn, D., Golinelli, D., Rose, R. D., Roy-Byrne, P., Stein, M. B., Sullivan, G., Bystritksy, A., Sherbourne, C., & Craske, M. G. (2013). Who gets the most out of cognitive behavioral therapy for anxiety disorders? The role of treatment dose and patient engagement. Journal of Consulting and Clinical Psychology, 81(4), 639–649. https://doi.org/10.1037/a0033403
- Glynn, L. H., & Moyers, T. B. (2009). Manual for the Motivational Interviewing Skill Code (MISC), Version 1.1. http://casaa.unm.edu/download/MISC_1.1_Manual.pdf
- Goodwin, B. J., Constantino, M. J., Westra, H. A., Button, M. L., & Antony, M. M. (2019). Patient motivational language in the prediction of symptom change, clinically significant response, and time to response in psychotherapy for generalized anxiety disorder. Psychotherapy Theory, Research, Practice, Training, 56(4), 537. https://doi.org/10.1037/pst0000269
- Hagen, R., Hjemdal, O., Solem, S., Kennair, L. E. O., Nordahl, H. M., Fisher, P., & Wells, A. (2017). Metacognitive therapy for depression in adults: A waiting list randomized controlled trial with six months follow-up. Frontiers in Psychology, 8, 31. https://doi.org/10.3389/fpsyg.2017.00031
- Hamilton, M. (1967). Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology, 6(4), 278–296. https://doi.org/10.1111/j.2044-8260.1967.tb00530.x
- Houck, J. M., Moyers, T. B., Miller, W. R., Glynn, L. H., & Hallgren, K. A. (2011). Motivational Interviewing Skill Code (MISC) 2.5. https://casaa.unm.edu/download/misc25.pdf
- Joramo, I., Solem, S., Romundstad, B., & Nordahl, H. M. (2021). Change talk and sustain talk in treatment of generalized anxiety disorder: A secondary analysis of cognitive behavioral therapy and metacognitive therapy in adult outpatients. Journal of Behavior Therapy and Experimental Psychiatry, 72, 101650. https://doi.org/10.1016/j.jbtep.2021.101650
- Keeley, R. D., Brody, D. S., Engel, M., Burke, B. L., Nordstrom, K., Moralez, E., Dickinson, L. M., & Emsermann, C. (2016). Motivational interviewing improves depression outcome in primary care: A cluster randomized trial. Journal of Consulting and Clinical Psychology, 84(11), 993. https://doi.org/10.1037/ccp0000124
- Koo, T. K., & Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of Chiropractic Medicine, 15(2), 155–163. https://doi.org/10.1016/j.jcm.2016.02.012
- Lassen, E. R., Touil, M., Svendsen, T. L., Haseth, S., & Solem, S. (2022). Patient motivation in group metacognitive therapy for generalized anxiety disorder. Psychotherapy Research, 32(5), 585–597. https://doi.org/10.1080/10503307.2021.2001068
- Lombardi, D. R., Button, M. L., & Westra, H. A. (2014). Measuring motivation: Change talk and counter-change talk in cognitive behavioral therapy for generalized anxiety. Cognitive Behaviour Therapy, 43(1), 12–21. https://doi.org/10.1080/16506073.2013.846400
- Maas, C. J. M., & Hox, J. J. (2005). Sufficient sample sizes for multilevel modeling. Methodology: European Journal of Research Methods for the Behavioral & Social Sciences, 1(3), 86–92. https://doi.org/10.1027/1614-2241.1.3.86
- Miller, W. R., & Mount, K. A. (2001). A small study of training in Motivational interviewing: Does one workshop change clinician and client behavior? Behavioural and Cognitive Psychotherapy, 29(4), 457–471. https://doi.org/10.1017/S1352465801004064
- Miller, W. R., & Rollnick, S. (1991). Motivational interviewing: Preparing people to change addictive behavior. Guildford Press.
- Miller, W. R., & Rollnick, S. (2012). Motivational interviewing: Helping people change (3rd ed.). Guilford Press.
- Miller, W. R., & Rose, G. S. (2009). Toward a theory of motivational interviewing. American Psychologist, 64(6), 527–537. https://doi.org/10.1037/a0016830
- Moyers, T. B., Martin, T., Manuel, J. K., Hendrickson, S. M., & Miller, W. R. (2005). Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment, 28(1), 19–26. https://doi.org/10.1016/j.jsat.2004.11.001
- Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x
- Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: A systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. https://doi.org/10.3389/fpsyg.2018.02211
- Norouzian, N., Westra, H. A., Button, M. L., Constantino, M. J., & Antony, M. M. (2020). Ambivalence and the working alliance in variants of cognitive‐behavioural therapy for generalised anxiety disorder. Counselling and Psychotherapy Research, 1–10. https://doi.org/10.1002/capr.12332
- Poulin, L. E., Button, M. L., Westra, H. A., Constantino, M. J., & Antony, M. M. (2019). The predictive capacity of self-reported motivation vs. early observed motivational language in cognitive behavioural therapy for generalized anxiety disorder. Cognitive Behaviour Therapy, 48(5), 369–384. https://doi.org/10.1080/16506073.2018.1517390
- Sijercic, I., Button, M. L., Westra, H. A., & Hara, K. M. (2016). The interpersonal context of client motivational language in cognitive–behavioral therapy. Psychotherapy Theory, Research, Practice, Training, 53(1), 13–21. https://doi.org/10.1037/pst0000017
- Solem, S., Husby, A. S., Håland, A. T., Launes, G., Hansen, B., Vogel, P. A., & Hagen, R. (2016). The University of Rhode Island change assessment as predictor of treatment outcome and dropout in outpatients with obsessive- compulsive disorder treated with exposure and response prevention. Psychotherapy and Psychosomatics, 85(2), 119–120. https://doi.org/10.1159/000441361
- Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guildford press.
- Wootton, B. M., Bragdon, L. B., Worden, B. L., Diefenbach, G. J., Stevens, M. C., & Tolin, D. F. (2021). Measuring within-session and between-session compliance in hoarding disorder: A preliminary investigation of the psychometric properties of the CBT compliance measure (CCM) and patient exposure/response prevention adherence scale for hoarding (PEAS-H). Assessment, 28(6), 1694–1707. https://doi.org/10.1177/1073191120918024
