ABSTRACT
Background: Sub-Saharan Africa (SSA) has had more major armed conflicts (wars) in the past two decades – including 13 wars during 1990–2015 – than any other part of the world, and this has had an adverse effect on health systems in the region.
Objective: To understand the best health system practices in five SSA countries that experienced wars during 1990–2015, and yet managed to achieve a maternal mortality reduction – equal to or greater than 50% during the same period – according to the Maternal Mortality Estimation Inter-Agency Group (MMEIG). Maternal mortality is a death of a woman during pregnancy, or within 42 days after childbirth – measured as maternal mortality ratio (MMR) per 100,000 live births.
Design: We conducted a selective literature review based on a framework that drew upon the World Health Organisation’s (WHO) six health system building blocks. We searched seven databases, Google Scholar as well as conducting a manual search of sources in articles’ reference lists – restricting our search to articles published in English. We searched for terms related to maternal healthcare, the WHO six health system building blocks, and names of the five countries.
Results: Our study showed three general health system reforms across all five countries that could explain MMR reduction: health systems decentralisation, the innovation related to the WHO workforce health system building block such as training of community healthcare workers, and governments-financing reforms.
Conclusion: Restoring health systems after disasters is an urgent concern, especially in countries that have experienced wars. Our findings provide insight from five war-affected SSA countries which could inform policy. However, since few studies have been conducted concerning this topic, our findings require further research to inform policy, and to help countries rebuild and maintain their health systems resilience.
Responsible Editor Stig Wall, Umeå University, Sweden
Background
War-affected healthcare systems in sub-Saharan Africa has adopted some reforms to rebuild their healthcare systems, and to mitigate the aftermath of disasters such as wars. These reforms are essential since SSA is the region of the world that has had the highest number of armed conflicts (including major armed conflicts (wars) with at least 1,000 battle-related direct deaths per year) in the past two decades [Citation1–Citation3]. In addition to causing health systems destruction, wars have disproportionately affected women’s and children’s health and severely impaired the provision of maternal health services [Citation4–Citation7].
The high prevalence of armed conflicts in SSA and their detrimental effect on health systems’ provision of maternal health services could be one of the reasons why the region also has the highest numbers of maternal deaths worldwide – a death of a woman while pregnant or within 42 days after childbirth [Citation8]. The 2015 Maternal Mortality Estimation Inter-Agency Group (MMEIG) showed that SSA accounted for 66% of all maternal deaths worldwide [Citation8]. Besides, 19 of the 49 SSA countries have an extremely high maternal mortality – measured as the maternal mortality ratio (MMR) – equal to or greater than 500 deaths per 100,000 live births [Citation8].
Despite SSA’s poor record in reducing its MMR during 1990–2015, there have been some notable successes to reduce MMR. For example, amongst 14 SSA countries that achieved MMR reductions equal to or greater than 50%, five of those countries managed to achieve a remarkable MMR reduction despite their long history of wars. These countries – listed alphabetically – are Angola, Eritrea, Ethiopia, Mozambique, and Rwanda. The wars experienced by these countries include the longest recent war in SSA – 50 years – between Eritrea and Ethiopia (1961–1991; 1998–2000; 2004), the brutal genocide in Rwanda (1994) when one million people are estimated to have been killed, and the long wars in the two the Portuguese former colonies, Angola (1975–2002) and Mozambique (1977–1992).
While some studies have examined health system reforms in low- and middle-income countries [Citation9–Citation14], to our knowledge, no study has examined the relationship between successful MMR reduction and health system reforms in relation to the war in SSA. To better understand this relationship in such contexts, we conducted a selective literature review of health system reforms in the five war-affected SSA countries during 1990–2015, using a framework that includes the WHO six health system building blocks [Citation2,Citation3,Citation15]. We aimed to understand these countries' best health system practices which enabled them to achieve an MMR reduction equal to or greater than 50% despite the effect of war.
Methods
This study investigated war-affected SSA countries that successfully reduced maternal mortality. Therefore, we chose to restrict our study design to these five countries, rather than to extend it to all war-affected countries in SSA.
Selection of study countries
We used two criteria for the selection of the SSA countries: (1) those that experienced major armed conflicts (wars) during 1990–2015 [Citation2]; (2) those that achieved ≥ 50% MMR reduction during 1990–2015 – as MMR reduction is indicative of the robustness of health systems performance [Citation16,Citation17].
According to the Uppsala Conflict Data Program’s definition of war (major armed conflicts with at least 1,000 battle-related direct deaths per year), during the period 1990–2015, 13 SSA countries experienced wars [Citation2,Citation3]. These countries with their MMRs per 100,000 live births in 2015 (alphabetically) are: Angola (477), Burundi (712), Central African Republic (CAR) (882), Democratic Republic of Congo (DRC) (693), Eritrea (501), Ethiopia (353), Liberia (725), Mozambique (489), Rwanda (290), Sierra Leone (1,360), Somalia (732), South Sudan (789), and Sudan (311) [Citation2,Citation8]. Sudan and South Sudan were excluded because both countries shared the same MMR data until the latter gained independence in 2011. Amongst the 11 remaining countries, we identified five countries (alphabetically) that had achieved an MMR reduction equal to or greater than ≥ 50% during 1990–2015: Angola, Eritrea, Ethiopia, Mozambique, and Rwanda.
Data extraction and analysis
We aimed to identify the common health system reforms across the five countries as follows. First, for each country categorised under the headings listed in the following framework (), articles that met the inclusion criteria () were extracted. Second, grey literature findings were combined with results from peer-reviewed studies for cross-validation. Third, all articles were analysed to identify any patterns across all five countries. All the previous steps were conducted by the first author (CC) and the inclusion criteria were discussed with three public health experts – RGC, JN, and SA. Finally, the results were shared for cross-validation of the findings with country-specific experts based in each of the five countries, to review and contribute further insights into the context of each country.
Because our research aimed to explore a wide range of factors that could explain health systems strengthening in five SSA countries that experienced wars during 1990–2015, we conducted a selective literature search as used by Gabrysch and Campbell [Citation18]. We did not conduct a systematic review because such analyses are better suited for investigating defined and specific questions, rather than questions of an exploratory nature [Citation18].
We conducted a literature review limited to articles published in English. We searched databases such as the Cochrane Library, Cinahl, Ovid Global Health, Ovid Medline, PubMed, Web of Science, Embase and Google Scholar, and performed a manual search of sources in articles’ reference lists. Grey literature was extracted manually through website search. However, some unpublished government documents (grey literature) in Portuguese were provided from Angola.
Our search was conducted in four steps. First, we searched maternal healthcare terms (obstetric delivery, pregnancy, childbirth, obstetric, birth, pregnancy, parturition, home childbirth, maternal death, reproductive health services, health provision). Then, we searched for terms related to the WHO six health system building blocks (health service, health workforce, health information, medical products, vaccine and technology, health finance, leadership and governance), and health service utilisation. Third, we searched for the names of the five countries (Angola, Eritrea, Ethiopia, Mozambique, and Rwanda). We combined the results of searching using these three sets of search terms. Finally, after screening the titles and then the abstracts, we included only the articles that met the framework criteria in the final step of our analysis.
Results
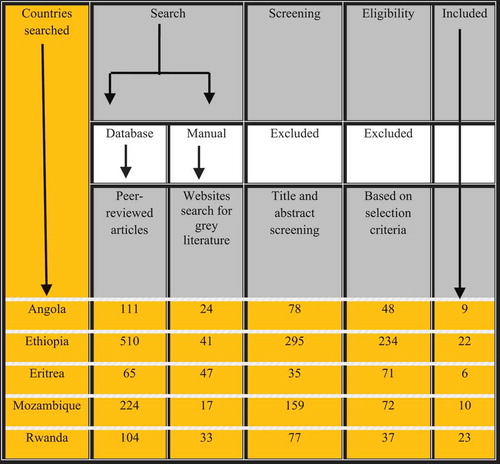
We found a total of 1,176 articles of which 1,014 (86.2%) were peer-reviewed articles and 162 (13.8%) grey literature. Our final group of papers comprised 70 articles of which 51 (71.8%) were peer-reviewed articles and 19 (26.8%) grey literature (). shows the descriptive results of the demographic and health profile for each of the five countries that achieved ≥ 50% MMR reduction. Rwanda is the most densely populated country amongst the five countries (471 people per sq. Km), while Angola is the least densely populated (20 people per sq. Km). During 1990–2015, amongst all five countries, Ethiopia had the greatest MMR reduction (71.8%) followed by Eritrea (68.5%).
Table 1. *Demographic and health profiles of sub-Saharan African countries that experienced war between 1990 and 2015 and reduced their maternal mortality ratios by more than 50%, 1990–2015.
Figure 1. Factors affecting access to maternal health services in war affected sub-Saharan African countries, 1990–2015. Adapted from the WHO six health system blocks (2010).
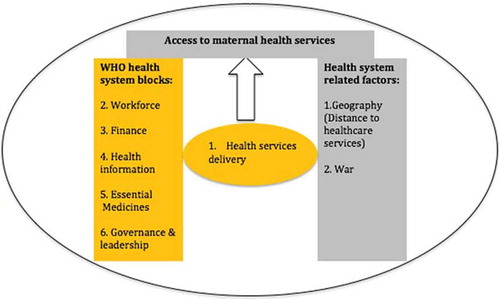
Figure 2. Studies inclusion criteria for the literature search and the number and type of papers included.
shows the three areas of health system reforms common across all five countries that could explain MMR reduction equal to or greater than 50% as shown in . These areas of reform were: (1) health systems decentralisation (related to Governance and Leadership WHO health system building block); (2) innovation related to the WHO workforce health system building block such as training of community healthcare workers (CHWs) (related to WHO workforce health system building block); and (3) health financing (related to WHO health system building financing block). All three findings contribute to health services delivery. However, our literature search did not reveal significant reforms concerning health information, essential medicine and geographical distance to healthcare services in any of the countries. Below we consider the three health system reforms that were common to the five countries we studied.
Figure 3. Maternal mortality decline in five sub-Saharan African countries affected by war during 1990–2015 (from the most significant decline in 2014). Data source: The 2015 Maternal Mortality Estimation Inter-Agency Group (MMEIG).
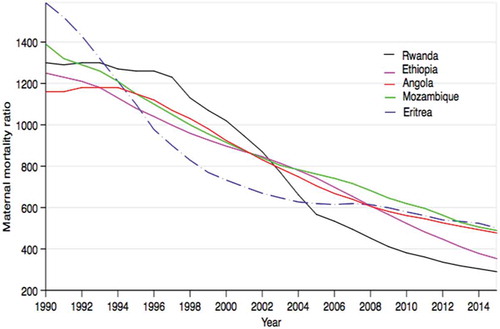
Figure 4. Total health expenditure in five "war-affected" countries compared to the median sub-Saharan region (most countries had no data prior to 1995). Data source: WHO
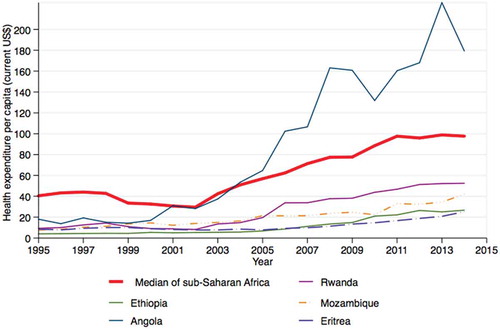
Table 2. Health system reforms with a significant effect on the provision of maternal health services in five sub-Saharan African countries, which experienced wars during 1990–2015, and achieved a significant maternal mortality reduction equal to or greater than 50% during the same period.
Health systems decentralisation
While the design of this study makes it difficult to link devolution of the health systems to MMR reduction directly, there were some noticeable governance reforms across all five countries that suggest that the decentralisation platform – the transfer of power, funding and decision-making to lower-level governments and communities – may have facilitated initiatives that contributed to the reduction in maternal mortality [Citation15,Citation19,Citation20].
Angola
After experiencing a protracted civil war (1975–2000) just after its independence from Portugal, Angola implemented district-level fiscal decentralisation and a district health strategy to build municipalities’ capacity to improve primary healthcare services [Citation21–Citation23]. The plan was to create the Basic Law for the National Health Service through the decree n. 21-B/92 ruling that users should contribute reasonable fees to the public healthcare sector [Citation24]. Under this law, health services were provided by the National Health Service, by the Military Health Services, and by the health services of large companies (public and private). These health services, in turn, were managed by the Ministry of Health, the Ministry of Defence and large corporations such as Chevron-Texaco [Citation25]. By 2008, the government had implemented fiscal decentralisation in 68 out of all 164 municipalities nationwide, and by 2010 it was completed across the whole country [Citation26].
These reforms aimed to address vulnerabilities in municipal health policy and healthcare provision in both the public and private sectors. Other efforts were made in 2010 by another presidential decree to improve the national health systems, through further regulation of infrastructure and health units [Citation27,Citation28].
Eritrea
Eritrea established a decentralisation policy before its independence from Ethiopia in 1991 by designing policies such as the Post-Independence Macro-Economic Policy Framework (MEPF) [Citation29,Citation30]. One aim of the MEPF was to improve access to healthcare facilities [Citation29–Citation31]. As a result of these significant policies such as the MEPF, the number of health facilities had increased by 170% by 2010 [Citation32]. In 2012, maternal and other health services were decentralised to zoba (region) and sub-zoba levels [Citation33]. Also, to ensure community participation, health policies are jointly reviewed annually by the Ministry of Health with the zoba health management teams [Citation34].
Ethiopia
Decentralisation from the regional to the woreda (district) level was initiated in 2002 by implementing a flexible form of decentralisation in which power was devolved to ethnically diverse communities [Citation20,Citation35–Citation38]. Each woreda has an administrative council composed of elected members [Citation39,Citation40]. The overall effectiveness of decentralisation to woreda level is suggested by an increase in contraception use by more than 200%, especially among the poor [Citation37]. Ethiopia also implemented a series of health policies between 1997 and 2010 to decentralise healthcare [Citation40–Citation43]. For example, maternity care is now provided at three levels: health posts offer first aid, health centres provide primary essential maternity care, and district hospitals offer comprehensive emergency obstetric care [Citation42].
Mozambique
Mozambique faced enormous challenges in rebuilding its healthcare systems following a protracted civil war that continued from 1975 to 1992 [Citation44]. These challenges derived not only from the lack of health systems infrastructure, personnel and financing but also from the high burden of HIV, TB and malaria [Citation44]. Nevertheless, and despite these challenges, Mozambique has undertaken steps to decentralise its health system. For example, in 1990 it introduced policies to devolve its health system to provinces, districts and then to autarquias (municipalities) [Citation45–Citation47]. However, while implementing decentralisation to the province level is seen as a sign of development, it remains a challenge [Citation46,Citation47].
Rwanda
Rwanda implemented decentralisation in 2000 as part of the government reconciliation process after the 1994 genocide [Citation48,Citation49]. Between 2005 and 2010 Rwanda designed the Twubakane ‘Let’s build together’ program to strengthen decentralisation of the health system at local government levels. Twubakane was undertaken with international partners and focussed on initiatives such as family planning and reproductive health in 12 out of the country’s 30 districts [Citation48]. Twubakane resulted in the strengthening of the health system and improvement in health services [Citation48]. By 2014, Rwanda had a network of 45,000 CHWs delivering decentralised health services in their communities as well as attending to essential maternal health needs – particularly important where access to health facilities is a barrier [Citation50–Citation56]. Rwanda also implemented partial fiscal decentralisation through Performance-Based Financing (PBF). While centrally managing maternal health service finances to prevent financial mismanagement, PBF provided incentives to staff and well-performing health facilities, allowing them to retain 40% of the revenues generated from both private and public healthcare sources [Citation49,Citation57,Citation58].
Innovation related to community healthcare workers (CHWs)
Boosting the number of healthcare workers is a standard feature of all the five war-affected countries. While they remain short of the recommended WHO requirement of 2.3 skilled healthcare workers (physicians and nurses/midwives) per 1000 population, all five countries have undertaken steps to address this particular problem [Citation59]. For example, all five countries introduced an innovation related to the WHO workforce health system building block such as community healthcare workers programme [Citation60]. Our study focuses on the paid "CHWs" cadre not volunteers.
Angola
Angola has the highest overall density of healthcare workers per 1,000 population of the five countries in this study, but the number of CHWs has been low [Citation60]. In 2007, Angola introduced a training programme for CHWs, known as Community Development and Health Agents, and there were 3,045 CHWs in Angola in 2014 [Citation60–Citation62].
Other health reforms have led to increased numbers of other types of healthcare workers. For example, in 2005, the government introduced an administrative health reform linkage between the Ministry of Public Administration, Employment and Social Security, the Ministry of Finance, the provincial governments, and the central hospitals. This administrative health reform aimed to enable more reliable health services that offered adequate mobility and placement, doing so by providing both public and private institutions throughout the country [Citation63,Citation64]. In 2015, these institutions produced a total of 1547 graduates in medicine, medical sciences, and health studies, about 400 more than the previous year [Citation65]. Also, between 2005 and 2010, Angola increased its number of doctors by 248% (from 849 to 2956) and the number of nurses increased by 85% (from 16,037 to 29,592) [Citation66,Citation67]. Angola also contracted approximately 1,500 Cuban-trained doctors [Citation62,Citation68]. However, despite the high health workforce numbers, as of 2016, half of the population in rural areas of Angola still had inadequate access to health services due to staff shortages [Citation61,Citation62].
Eritrea
Eritrea emphasised combining midwifery and nursing as a task-shifting strategy, as well as using foreign doctors from countries such as Cuba to deal with its health workforce shortage [Citation29,Citation69–Citation71]. Consequently, between 2002 and 2012, the number of nurses/midwives increased by 48% (from 846 to 1,253) and associate nurses (diploma and certificate) increased by 70% (from 1,488 to 2,537) [Citation29]. In 2005, Eritrea piloted a CHW program, and there were 800 CHWs, also known as community health agents, in the country by 2014 [Citation60].
Ethiopia
In 2003, Ethiopia implemented the Health Extension Programme (HEP), managed by district governments [Citation10,Citation41]. As a result, overall health service delivery – measured by the number of people utilising health services – increased from 51% in 2000 to 92% in 2011[Citation10,Citation72]. The HEP policy was aimed at training CHWs to provide maternal health services in remote communities [Citation73–Citation77]. Each kebele (village) of 3,000–5,000 people is assigned two Health Extension Workers (HEWs) that have received a year of training [Citation76–Citation78]. In 2014, there were 34,000 HEWs with a ratio of 1:2,437 population (target: 1:2,500) [Citation60,Citation79]. HEWs are responsible for community mobilisation and deliver preventative maternity care services [Citation76,Citation77,Citation80]. HEWs are required to spend 15% to 20% of their time at health posts and 75% to 80% of their time providing community outreach support [Citation42,Citation81]. Due to the critical shortage of physicians, Ethiopia also implemented task shifting by training of non-physician clinicians (NPCs) with skills needed for the provision of comprehensive emergency obstetric and neonatal care [Citation82]. These NPCs were found to perform 63% of emergency procedures including caesarean sections [Citation82].
Mozambique
shows the size of the health workforce in Mozambique. Mozambique was one of the first countries in SSA to pioneer task shifting and training of healthcare workers including nurses, midwives, and CHWs (1,213 CHWs in 2014) to address health workforce shortages [Citation60]. In 1978, Mozambique introduced the training program for CHWs who were known as Agentes Polivalentes Elementares (APEs) [Citation83]. The task of these APEs was health promotion, including directing patients to the nearest health facility [Citation83]. Another reform in Mozambique that was championed in 1984 by Pascoal Mocumbi (Minister of Health in Mozambique between 1980 and 1987) was the introduction of a category of healthcare workers with 2–3 years training specialising in obstetric surgery to address the shortage of doctors in rural areas [Citation84,Citation85]. By 2010, these healthcare workers were performing more than 90% of obstetric operations (including caesarean sections in rural areas) and 35% of emergency surgeries in urban areas, as well as helping pregnant women reach healthcare facilities [Citation86–Citation90].
Rwanda
In 2007, Rwanda introduced a CHWs’ initiative in each of its districts, involving three CHWs being elected by their community and providing preventive and curative services in their communities [Citation52–Citation54,Citation56]. By 2014, there was a network of 45,000 CHWs in Rwanda implementing the decentralisation of health services by mobilising their communities, as well as attending to women’s urgent maternal needs – notably where access to health facilities was a barrier [Citation50–Citation56,Citation60]. In addition to CHWs, Rwanda deployed more nurses, midwives and general doctors to the rural areas and trained traditional birth attendants [Citation91,Citation92].
Health-financing system
State-sponsored public-financing systems play a significant role in shielding citizens from the catastrophic effects of out-of-pocket health expenditure – an expense that is a major barrier to increasing the number of facility-based deliveries, and improving utilisation of antenatal care, and other maternal health services [Citation93–Citation96]. As shown in , health expenditure per capita in all countries, except Angola, is low compared to the average for SSA. We found the most current innovation in the state-sponsored public-financing system is in Rwanda, where Community-Based Health Insurance (CBHI) is more comprehensive than in the other four countries [Citation21].
Angola
Health financing in Angola is less influenced by external donor funding than it is in the other four countries examined in this paper, with only 14% of Angola’s health funding being provided by aid [Citation97]. The government contributes 80% of the total health expenditure, and out-of-pocket expenditure accounts for only 20% [Citation21,Citation88]. Twenty per cent of revenue is generated from private health insurance through the National Insurance Company of Angola, and the government provides the rest of the public funding [Citation21].
Eritrea
Since 2006, Eritrea has attempted to enhance its financial pooling system and reduce the burden of out-of-pocket expenditure by increasing fees retention by healthcare facilities, as highlighted in the National Health Policy of 2010 [Citation98,Citation99]. Between 1988 and 2017, Eritrea introduced community health insurance and private health insurance as well as tax funds plus individual health insurance embedded within the public healthcare system, as by 2016 there were no privately owned clinics in the country [Citation69,Citation88,Citation98,Citation100,Citation101]. However, there is no direct evidence as to the extent to which these initiatives impact on access to health services.
Ethiopia
Ethiopia has taken significant steps towards universal health coverage, although it is faced with the challenge of sustainability – donors contribute 40% of the health financing, while 37% is provided by householders’ payments [Citation100,Citation101]. Although out-of-pocket payments are still one of the barriers to accessing healthcare in the country, in 1998 Ethiopia started some decentralising reforms aimed at improving the health-financing system [Citation96,Citation102]. In 2006, Ethiopia initiated a woreda – based system that was financed by the government and development partners [Citation37]. Between 2005 and 2008, the Ministry of Health developed a fees retention policy to provide revenues for local health facilities, as well as introducing the CBHI scheme in 2008 [Citation94,Citation102–Citation104].
Mozambique
Mozambique receives some of the most substantial international donor funding in SSA, with 50% of the government funding depending on aid [Citation87,Citation105]. Due to the high level of donor funding, out-of-pocket health expenditure is minimum, and services are free for the poor, therefore enabling broader access to health services [Citation106]. In 2000, the Ministry of Health and donors signed an agreement regarding coordination of aid to be channelled through the government financing system [Citation87,Citation107,Citation108]. This agreement led to a decrease in vertical financing – funds directed towards specific interventions not fully integrated within the health system – from 82% in 2001 to 50% in 2007 [Citation108,Citation109]. In 2008, the government created a single financing pooling system and provincial coordination teams to coordinate donor funding [Citation46,Citation108].
Despite the numerous efforts by Mozambique to coordinate and direct donor funding towards building its local capacity, international donor funding remains under criticism for not contributing enough to strengthening the health system, for adding to dis-harmony in coordinating external resources, and for creating an unequal distribution of resources, thereby leading to disparities within the health system [Citation109,Citation110].
Rwanda
In Rwanda, two significant health-financing policies were introduced post-conflict: CBHI and PBF [Citation49,Citation57,Citation111]. The introduction of CBHI led to a sharp increase in facility-based deliveries [Citation112,Citation113]. Rwanda piloted CBHI in 1999, and it was then fully implemented nationally in 2005 [Citation54,Citation88,Citation114]. Fifty per cent of the CBHI funding comes from annual membership premiums, with the very poor exempt [Citation115]. The national government funds cover the rest of the cost of CBHI from local and international organisations [Citation116]. By 2015, CBHI comprised 90% of the population, removing financial barriers to accessing healthcare and therefore increasing utilisation of health services [Citation114–Citation116]. Non-covered services (10%) are paid for by users at the point of service but are free for the poorest [Citation54,Citation117]. CBHI currently covers facility-based delivery and provides caesarean sections free of charge [Citation118].
Poor quality of care is one of the barriers to the utilisation of maternal health services [Citation119,Citation120]. In 2005, Rwanda initiated PBF as a form of financial incentive to improve the quality of care, subsequently leading to an increase in facility-based deliveries [Citation112,Citation121–Citation123]. In addition to enhancing the quality of care, PBF also contributed to building local district capacity as a part of Rwanda’s decentralisation policy [Citation123,Citation124].
Discussion
This study aimed to understand best health system practices in five war – affected SSA countries that experienced wars during 1990–2015 and yet managed to achieve a maternal mortality reduction – equal to or greater than 50% during the same period. Analysis of recent data from these five countries illustrates how some countries have used reforms to rebuild their health systems after the war. Taking MMR reduction as a sensitive indicator for the outcome of these reforms on health systems performance, three common reforms emerged as good practices: health systems decentralisation, health workforce innovations such as training of CHWs, and country’s ownership of health finance to minimise the influence of external donors on the provision of healthcare services.
One indicator of good governance is decentralisation, including decentralisation which facilitates the participation of sub-national stakeholders in decision-making [Citation15]. SSA has seen progress in leadership to address its health challenges [Citation125], and one example of such development is the varying degrees of decentralisation that have been achieved and have enabled the reform of healthcare systems [Citation20,Citation126]. Implementation of decentralisation requires political will. In all five countries that we studied, devolution was mainly driven by the political commitment of the same leaders or parties that were instrumental in ending the wars. This political commitment could be, at least in part, responsible for the success of decentralisation efforts in these countries, as it is implemented as part of a healing process towards reconciliation. The progress of decentralisation in the five countries also needs to be considered, particularly in relation to factors such as the duration of the war and the magnitude of any influence of the HIV epidemic. For example, Mozambique experienced both a lengthy war as well as the HIV/AIDS epidemic, which could have contributed to its relatively slow progress in the decentralisation of its health services and therefore slowed its MMR reduction [Citation8].
Shortages in the healthcare workforce are another challenge facing most SSA countries. The current WHO recommendation requires a minimum of 4.45 doctors, nurses and midwives per 1,000 population to achieve the SDG goals [Citation59]. Shortages in the healthcare workforce indicate that SSA countries, including the five countries examined in this study, need to employ more innovative approaches to increase their workforce. One such reform already in place is CHWs. All five countries use CHWs to address shortages in the health workforce and to improve access to health services in geographically isolated regions [Citation18,Citation96,Citation127–Citation130]. CHWs provide low-cost services and are easier to retain than doctors and nurses, especially in rural areas [Citation131,Citation132]. Despite CHWs playing an essential role in healthcare delivery, there are challenges related to absenteeism and perception of the services they provide as being of poor quality [Citation37,Citation133–Citation137]. However, these challenges could be overcome by proper training and by offering incentives to reduce absenteeism.
This study is one of the very few studies to have examined health system reforms in war-affected SSA countries during 1990–2015 and their relationship to MMR reduction. However, our results are in line with the general findings described globally by other scholars [Citation9,Citation10,Citation138,Citation139] who investigated health system reforms in low-income countries, and how countries managed to deliver good healthcare with little resources. For example, like Balabanova et al., we found that an increase in the number of CHWs was one of the critical factors driving improvement in health systems performance in Ethiopia [Citation9,Citation10,Citation138,Citation139]. The important contribution of our study is the finding that factors identified by previous studies across multiple developing countries – particularly a study conducted by Pavignani and Colombo [Citation140] about war-affected health systems – also apply in SSA countries affected by war. In their report, they analysed health services in Mozambique and Angola during 1975–2000 and concluded that health systems in war-affected regions should be a concern for the international community. Our study extends their work by analysing health systems in five countries.
Establishing causal links between health system reforms and outcomes is challenging – not least in a context of armed conflict where change can be rapid and unpredictable. While the lack of MMR reduction in the other six war-affected countries in SSA could be related to deficiencies in the three health system factors that we identified, lack of success could also be due to a combination of contextual circumstances that are peculiar to each country. Hence, this exploratory literature review is only able to identify relatively discrete reforms (hardware), with the understanding that there may be less tangible reasons for improved outcomes (software) [Citation141]. Examples of such software include the strong determination for progress after the devastation of war; political deals between warring factions leading to decentralised governance; and significant amounts of foreign aid from strategic allies to support rebuilding efforts. Future research should seek to both disentangle and connect these hardware and software elements in real time, as countries undergo recovery and reform.
Although we conducted a broad literature review and consulted country experts, this study had some limitations. First, there was an imbalance in the number of published peer-reviewed articles among the five countries. Second, it was not possible to establish a link between decentralisation and health services delivery in Angola, Mozambique and Eritrea. Nevertheless, we have shown direct examples in both Rwanda and Ethiopia that suggest improvements in health systems performance associated with decentralisation. Third, it was difficult to get reliable data about the countries before their wars, which often dated back to the 1960s and 1970s. Fourth, while it is challenging to theorise and assume that the experiences of one country could be transferable to another, there is evidence to suggest that some reforms may be effectively employed across different countries. Two examples are the CHW reforms in SSA that started in Mozambique and the community-based health insurance schemes currently operating in Ethiopia and Rwanda (as well as in other SSA countries). Finally, we did not analyse war-affected SSA during 1990–2015 that did not achieve ≥ 50% MMR reduction. This means that we might have missed some valuable lessons that could be learned from those countries.
Conclusion
Restoring health systems after disasters is an urgent concern, especially in SSA countries that have had wars. Reforms across all five countries that are examined in this study – Angola, Eritrea, Ethiopia, Mozambique, and Rwanda – were mainly driven by political commitment within each country to decentralise health systems and health workforce innovations such as CHWs’ programs. Our findings provide an insight from these countries which with further research could inform policy and thereby help other countries rebuild and maintain their health systems resilience, particularly in the aftermath of disasters such as wars. This is particularly relevant to countries emerging from conflict or instability including the Central African Republic, the Democratic Republic of Congo, and South Sudan. Further research on decentralisation models appropriate in different settings and their implementation challenges will be important, alongside governance research into how to bring women and children’s health to the fore amidst post-conflict policymaking.
Ethics and consent
Not applicable.
Paper context
Recently, there have been calls to strengthen health systems in sub-Saharan Africa. However, reforming those healthcare systems remains a challenge in some sub-Saharan African countries that have experienced wars. To our knowledge, this study is the first to explore a wide range of health system reforms in the five SSA countries that experienced wars during 1990–2015 and achieved ≥ 50% MMR reduction in the same period. Maternal mortality reduction is used as a sensitive measure of robustness of these countries’ health systems.
Acknowledgments
This analysis is a part of a broader research study being conducted by the first author to fulfil the requirement for a PhD at the School of Public Health, the University of Sydney, Australia.
Disclosure statement
The authors have no conflict of interest to declare.
Additional information
Funding
Notes on contributors
Chol Chol
The first author conceptualised the study design; collected the data; produced the tables and figures; initiated the interpretation of the results (which was then cross-examined by all co-authors including experts from those countries); and completed the first draft of the manuscript. All authors provided crucial input into the data interpretation and reviewed and approved the final manuscript.
References
- Human Security Research Group. The decline in global violence: evidence, explanation, and contestation. 2013. [ Cited 2017 Jun 5]. Available from: https://www.ualberta.ca/~tkeating/HSR13.pdf
- Strand H, Wilhelmsen L, Gleditsch N. Armed conflict dataset codebook. Stockholm, Uppsala: International Peace Research Institute Oslo (PRIO); 2003.
- Themnér L, Wallensteen P. Armed conflicts, 1946–2011. J Peace Res. 2012;49:565–15.
- Campbell J, Cometto G, Rasanathan K, et al. Improving the resilience and workforce of health systems for women’s, children’s, and adolescents’ health. BMJ. 2015;351:h4148.
- Witter S, Falisse J-B, Bertone MP, et al. State-building and human resources for health in fragile and conflict-affected states: exploring the linkages. Hum Resour Health. 2015;13:1.
- Ghobarah HA, Huth P, Russett B. The post-war public health effects of civil conflict. Soc Sci Med. 2004;59:869–884.
- Roberts L, Muganda CL. War in the Democratic Republic of Congo. London: Oxford University Press; 2008. p. 279–288.
- Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis. Lancet. 2016;387:462–474.
- Van Lerberghe W, Matthews Z, Achadi E, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet. 2014;384:1215–1225.
- Balabanova D, Mills A, Conteh L, et al. Good health at low cost 25 years on: lessons for the future of health systems strengthening. Lancet. 2013;381:2118.
- Parkhurst JO, Penn-Kekana L, Blaauw D, et al. Health systems factors influencing maternal health services: a four-country comparison. Health Policy. 2005;73:127–138.
- Kruk ME, Leslie HH, Verguet S, et al. Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Global Health. 2016. DOI:10.1016/S2214-109(16)30180-2
- Koblinsky MA. Reducing maternal mortality: learning from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe. Washington: World Bank Publications; 2003.
- Maine D. Lessons for program design from the PMM projects. Int J Gynecol Obstetrics. 1997;59:S259–S65.
- WHO. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva: WHO; 2010 [ Cited 2017 May 21st]. Available from: http://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf?ua=1
- Abouzahr C, Wardlaw T, Stanton C, et al. Maternal mortality. World Health Stat Q. 1996;49:77–87.
- Zureick-Brown S, Newby H, Chou D, et al. Int Perspect Sex Reprod Health. 2013;39. DOI:10.1363/3903213.
- Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth. 2009;9:34.
- Joshi DK, Hughes BB, Sisk TD. Improving governance for the post-2015 sustainable development goals: scenario forecasting the next 50 years. World Dev. 2015;70:286.
- Ndegwa S. Decentralization in Africa: a stocktaking survey. Africa Region: World Bank; 2002.
- Connor C, Averbug D, Miralles M. Angola health system assessment. Washington:USAID. 2010. [ Cited 2017 Sep 5th]. Available from: http://pdf.usaid.gov/pdf_docs/Pnadx702.pdf
- Mac Dowell M, Araújo E, Cialdini A, et al. Diagnosis of fiscal decentralization in Angola. Luanda: UNDP; 2006. [ Cited 2017 May 9]. Available from: http://www.ao.undp.org/content/angola/en/home/library/democratic_governance/fiscal-decentralization.html
- Frøystad M, Mæstad O, Villamil N. Health services in Angola: availability, quality and utilisation 2011. [ Cited 2017 May 9]. Available from: http://www.cmi.no/publications/file/4319-health-services-in-angola.pdf
- Diário da República (Official Gazette). Angola: lei no. 21-B/92 - Lei de Base do Sistema Nacional de Saúde (Lei no. 21-B/92 - Basic Law of the National Health System). Portuguese: Luanda; 1992. 4.5 MB pdf.
- Ministério da Saúde de Angola (Ministry of Health of Angola). Conjunto de Instituição de Saúde sob Tutela do Ministério da Saúde (Health Institution set under tutelage of the Ministry of Health). Luanda: Política Nacional da Saúde (National Health Policy) - 5º Esboço; 2009.
- UNDP Angola. Decentralization and Local Governance Project (DLG). Lunda: UNDP Angola; 2013 [ Cited 2017 Nov 11]. Available from: http://www.ao.undp.org/content/dam/angola/docs/projectdocuments/UNDP_AO_DLG-Final-Project-Report_July2013.pdf
- Instituto Nacional de estatistica (National Institute of Statistics). Inquerito dos indicadores multiplo por amostragem implemenated (Survey indicators of multiple samples implemented). Luanda: Instituto Nacional de estatistica (National Institute of statistics); 1996.
- Sobre a Politica Nacional de Saude (About the National Health Policy). Diário da República (Republic Diary) nº 222, I série (Decreto nº 262/10 de 22 de Novembro). Luanda; 2010.
- Ministry of Health Eritrea. Eritrea annual health service activity report of year 2012. Asmara: Eritrea Ministry of Health; 2013.
- Ministry of Health Eritrea. National health policy. Asmara: Eritrea Ministry of Health; 2010. [ Cited 2017 Nov 22]. Available from: http://www.who.int/medical_devices/survey_resources/health_technology_national_policy_eritrea.pdf
- UNDP. Innovations driving health MDGs in Eritrea. Asmara: UNDPA Eritrea; 2014 [ Cited 2017 Oct 9]. Available from: http://www.er.undp.org/content/dam/eritrea/docs/MDGs/Abridged%20MDG%20report_final.pdf
- National Statistics and Evaluation Office (NSO) [Eritrea]. Fafo AIS. Asmara: Eritrea Population and Health Survey 2010; 2013.
- Ministry of Health Eritrea. Second national integrated monitoring and evaluation framework 2012–2016. Asmara: Eritrea Ministry of Health; 2012. [ Cited 2017 Oct 9]. Available from: http://www.nationalplanningcycles.org/sites/default/files/planning_cycle_repository/eritrea/national_me_plan.pdf
- Green A, Collins C, Stefanini A, et al. The role of strategic health planning processes in the development of healthcare reform policies: a comparative study of Eritrea, Mozambique and Zimbabwe. Int J Health Plann Manage. 2007;22:113–131.
- Ayenew M. Decentralization in Ethiopia. In: Bahru Z, Siegfried P, editors. Ethiopia: the challenge of democracy from below. Stockholm, Nordiska Afrikainstitutet: Uppsala and Forum for Social Studies, Addis Ababa; 2002. p. 212.
- Tegenu T The model and making of ethnic federalism in Ethiopia: identifying the problems to find the solution. 9th International Conference on African Development. Ethiopia: Addis Ababa University; 2016.
- Khan QM, Faguet J-P, Gaukler C, et al. Improving basic services for the bottom forty per cent: lessons from Ethiopia. Washington DC: World Bank Group; 2014.
- HuiHui W, Tesfaye R, Ramana G, et al. Ethiopia health extension program: an institutionalized community approach for Universal Health Coverage. Washington DC:World Bank Group. 2016. [ Cited 2017 Feb 18th]. Available from: https://openknowledge.worldbank.org/handle/10986/24119
- Federal Democratic Republic of Ethiopia. The constitution of the transitional government of Ethiopia 1993. Addis Ababa: The Government of Ethiopia; 1994.
- Ethiopia Ministry of Health. Ethiopia Health Sector Development Programme (EHSDP) 1997/98-2001/02. Addis Ababa; 2003. [Cited 2017 Nov 22]. Available from: http://www.etharc.org/resources/download/finish/33/88.
- Ethiopia Ministry of Health. Health Sector Development Programme III. Annual Performance Report 2002 EFY (2009/2010). Addis Ababa; 2010.
- Ethiopia Ministry of Health. Health Sector Development Program IV 2010/11 – 2014/15. Addis Ababa; 2010. [Cited 2017 Nov 22]. Available from: http://phe-ethiopia.org/admin/uploads/attachment-721-HSDP%20IV%20Final%20Draft%2011Octoberr%202010.pdf. .
- Ethiopia Ministry of Health. Ethiopia Health Sector Development Programmes (HSDP II) 2002/03 – 2004/05. Addis Ababa; 2006. [Cited 2017 Nov 22]. Available from: http://www.nationalplanningcycles.org/sites/default/files/planning_cycle_repository/ethiopia/report_of_the_final_evaluation_of_hsdp_ii_with_indicator_trends1.5.2006-fin.pdf. .
- González R, Augusto OJ, Munguambe K, et al. HIV incidence and spatial clustering in a rural area of Southern Mozambique. PloS One. 2015;10:e0132053.
- UNDP. Decentralization and District Development. Participatory & multi-sectoral framework for decentralized policies and local development strategies addressed to millennium development goals. Maputo: UNDP Mozambique; 2005 [ Cited 2017 Nov 28]. Available from: http://www.undp.org/content/dam/mozambique/docs/Decentralization%20and%20District%20Development.pdf
- Global Health Initiative. Mozambique strategy 2011–2015. [ Cited 2017 Nov 28]. Available from: https://www.ghi.gov/wherewework/docs/mozambiquestrategy.pdf
- Ames B, Connerley E, Rosário D, et al. Comparative assessment of decentralization in Africa: Mozambique in country assessment report. Report prepared for the USA Agency for International Development. Washington: USAID; 2010. [Cited 2017 Jan 19]. Available from: https://pdfs.semanticscholar.org/7170/3844afc30d61e792c212fb6b03e8e53014c6.pdf.
- Brinkerhoff D, Fort C, Stratton S Good governance and health: assessing progress in Rwanda. TWUBAKANE Decentralization and Health Program Rwanda Report 2009. [cited 2017 Jun 11]. Available from: https://www.rti.org/sites/default/files/resources/goodgovernanceandhealth-assessingprogressinrwandafinal.pdf.
- Bucagu M, Kagubare JM, Basinga P, et al. Impact of health systems strengthening on coverage of maternal health services in Rwanda, 2000–2010: a systematic review. Reprod Health Matters. 2012;20:50–61.
- Bhutta ZA, Lassi ZS, Pariyo G, et al. Global experience of community health workers for delivery of health related millennium development goals: a systematic review, country case studies, and recommendations for integration into national health systems. Global Health Workforce Alliance. 2010;1:249–261.
- Mugeni C. Rwanda’s community health system: from policy to action. First annual international community health summit. Kigali, Rwanda; 2011. [ Cited 2013 Jan 10]. Available from: www.icchrwanda.org/index.php?Option=com_content&view=article&id/60&itemid=3
- Chambers V, Golooba-Mutebi F. Is the bride too beautiful? Safe motherhood in rural Rwanda. London:ODI. 2012. [ Cited 2016 Aug 30]. Available from: http://www.institutions-africa.org/filestream/20120312-appp-research-report-04-safe-motherhood-in-rural-rwanda-by-v-chambers-and-f-golooba-mutebi-march-2012
- Drobac PC, Basinga P, Condo J, et al. Comprehensive and integrated district health systems strengthening: the Rwanda Population Health Implementation and Training (PHIT) partnership. BMC Health Serv Res. 2013;13:S5–S.
- Farmer PE, Nutt CT, Wagner CM, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ. 2013;346. (jan18 1): f65. Doi: 10.1136/bmj.f65.
- Pierce H, Heaton TB, Hoffmann J. Increasing maternal healthcare use in Rwanda: implications for child nutrition and survival. Soc Sci Med. 2014;107:61–67.
- Condo J, Mugeni C, Naughton B, et al. Rwanda’s evolving community health worker system: a qualitative assessment of client and provider perspectives. Hum Resour Health. 2014;12:71.
- Meessen B, Musango L, Kashala JPI, et al. Reviewing institutions of rural health centres: the performance initiative in Butare, Rwanda. Trop Med Int Health. 2006;11:1303–1317.
- Rusa L, Schneidman M, Fritsche G, et al. Rwanda: performance-based financing in the public sector. Washington DC: Center for Global Development; 2009. [Cited Jan 10th 2013; Jan 1st 2017]. Available from: https://www.cgdev.org/doc/books/PBI/10_CGD_Eichler_Levine-Ch10.pdf.
- WHO. Health workforce requirements for universal health coverage and the sustainable development goals. Geneva: WHO; 2016 [ Cited 2017 May 26]. Available from: http://apps.who.int/iris/bitstream/10665/250330/1/9789241511407-eng.pdf
- UNICEF. Access to healthcare through community health workers in East and Southern Africa. New York: UNICEIF; 2014 [ Cited 2018 Jul 1]. Available from: https://www.unicef.org/health/files/Access_to_healthcare_through_community_health_workers_in_East_and_Southern_Africa.pdf
- Craveiro I, Dussault G. The impact of global health initiatives on the health system in Angola. Glob Public Health. 2016;11:475.
- Giugliani C, Duncan BB, Harzheim E, et al. Community health workers programme in Luanda, Angola: an evaluation of the implementation process. Hum Resour Health. 2014;12:68.
- Fonseca PL. In Editorial. Nzila, editor: preparação e organização das administrações locais para a implementação do programa do governo e acções complementares (Preparation and organization of local administrations for the implementation of the government program and complementary actions). Luanda: Encontro Nacional sobre Administração Local em Angola Luanda (National Meeting on Local Administration in Angola Luanda); 2005:99-113.
- Queza AJ. Sistema de Saúde em Angola (Health System in Angola): uma proposta à luz da reforma do Serviço Nacional de Saúde em Portugal (A proposal in light of the reform of the National Health Service in Portugal). Luanda: Mestrado Integrado em Medicina (Integrated Master in Medicine), Universidade do Porto; 2010.
- Ministério do Ensino Superior, editor (Ministry of Higher Education). Sistema de Saúde em Angola: uma proposta à luz da reforma do Serviço Nacional de Saúde em Portugal (Statistical Yearbook of Higher Education). Luanda: Anuário estatístico do Ensino Superior; 2015.
- Connor C, Rajkotia Y, Lin S, et al. Angola health system assessment. Washington:USAID. 2005. [ Cited 2017 May 9]. Available from: https://sarpn.org/documents/d0001872/Angola_Health_Sept2005.pdf
- WHO. Global Health Observatory data repository 2015. [ Cited 2016 Jun 3]. Available from: http://apps.who.int/gho/data/node.main.HWF1?lang=n
- World Bank. Angola - Municipal health service strengthening (Revitalizacao) project: restructuring. Lunda: World Bank Angola; 2015 [ Cited 2017 May 9]. Available from: http://documents.worldbank.org/curated/en/2015/11/25256019/angola-municipal-health-service-strengthening-revitalizacao-project-restructuring
- Chol C, Hunter C, Debru B, et al. Stakeholders’ perspectives on facilitators of and barriers to the utilisation of and access to maternal health services in Eritrea: a qualitative study. BMC Pregnancy and Childbirth. 2018;18:35.
- Holzgreve W, Greiner D, Schwidtal P. Maternal mortality in Eritrea: improvements associated with centralization of obstetric services. Int J Gynecol Obstetrics. 2012;119:S50–S4.
- Sharan M, Ahmed S, Ghebrehiwet M, et al. The quality of the maternal health system in Eritrea. Int J Gynaecol Obstetrics. 2011;115:244.
- Banteyerga H. Ethiopia’s health extension program: improving health through community involvement. MEDICC Rev. 2011;13:46–49.
- Kinfu Y, Dal Poz MR, Mercer H, et al. The health worker shortage in Africa: are enough physicians and nurses being trained? Bull WHO. 2009;87:225–230.
- Hongoro C, McPake B. How to bridge the gap in human resources for health. Lancet. 2004;364:1451–1456.
- Central Statistical Authority. Ethiopia mini demographic and health survey. Addis Ababa: Ethiopia Ministry of Health; 2014.
- Ethiopia Ministry of Health. Health extension programme implementation guidelines. Addis Ababa: Ethiopia Ministry of Health; 2004.
- Ethiopia Ministry of Health. Health extension programme in Ethiopia. Addis Ababa: Ethiopia Ministry of Health; 2007.
- Warren C. Care seeking for maternal health: challenges remain for poor women. Ethiopian J Health Dev. 2010;24:100–104.
- WHO. WHO country cooperation strategy 2009–2013. Geneva: WHO; 2013. [Cited 2015 May 22]. Available from: https://afro.who.int/sites/default/files/2017-06/ccs_eritrea_2009_2013.pdf.
- Gebrehiwot T, San Sebastian M, Edin K, et al. Health workers’ perceptions of facilitators of and barriers to institutional delivery in Tigray, Northern Ethiopia. BMC Pregnancy and Childbirth. 2014;14:137.
- Koblinsky M, Tain F, Gaym A, et al. Responding to the maternal healthcare challenge: the Ethiopian health extension program. Ethiopian J Health Dev. 2010;24:105–109.
- Gessessew A, Ab Barnabas G, Prata N, et al. Task shifting and sharing in Tigray, Ethiopia, to achieve comprehensive emergency obstetric care. Int J Gynecol Obstetrics. 2011;113:28–31.
- Lindelöw M, Ward P, Zorzi N. Primary healthcare in Mozambique: service delivery in a complex hierarchy: human development sector. Africa Region: The World Bank; 2004.
- Da Luz Vaz M, Bergström S. Mozambique – delegation of responsibility in the area of maternal care. Int J Gynecol Obstetrics. 1992;38:S37–S9.
- Binagwaho A, Crisp N. African health leaders: claiming the future. Lancet. 2015;385:2134–2135.
- Pereira C, Cumbi A, Malalane R, et al. Meeting the need for emergency obstetric care in Mozambique: work performance and histories of medical doctors and assistant medical officers trained for surgery. Int J Obstetrics Gynaecol. 2007;114:1530–1533.
- Clarke J, Visser-Valfrey M. Results and value for money: a performance review of the human development Portfolio in Mozambique. Maputo: Department of International Development; 2010. [ Cited 2017 Nov 28]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/67676/perf-rev-hum-dvmt-portf-mz.pdf
- WHO, UNICEF, Countdown to 2015 decade report (2000–2010) with country profiles: taking stock of maternal, newborn and child survival. Geneva: WHO; 2010. Available from. http://apps.who.int/iris/bitstream/10665/44346/1/9789241599573_eng.pdf. [ Cited 2016 Apr 15th].
- Koblinsky M, Matthews Z, Hussein J, et al. Going to scale with professional skilled care. Lancet. 2006;368:1377–1386.
- Munguambe K, Boene H, Vidler M, et al. Barriers and facilitators to healthcare seeking behaviours in pregnancy in rural communities of southern Mozambique. Reprod Health. 2016;13:31.
- Logie DE, Rowson M, Ndagije F. Innovations in Rwanda’s health system: looking to the future. Lancet. 2008;372:256–261.
- Hong R, Ayad M, Ngabo F. Being insured improves safe delivery practices in Rwanda. J Community Health. 2011;36:779–784.
- Wang WJ, Temsah G, Mallick L. Health insurance coverage and its impact on maternal healthcare utilization in low- and middle-income countries. DHS Analytical Studies No. 45. Rockville: ICF International; 2014 (as cited by BMC Pregnancy and childbirth)
- Pearson L, Gandhi M, Admasu K, et al. User fees and maternity services in Ethiopia. Int J Gynecol Obstetrics. 2011;115:310–315.
- Sambo LG, Kirigia JM, Ki-Zerbo G. Health financing in Africa: overview of a dialogue among high level policy makers. BMC Proc. 2011;5:S2–S.
- Shiferaw S, Spigt M, Godefrooij M, et al. Why do women prefer home births in Ethiopia? BMC Pregnancy and Childbirth. 2013;13:5.
- WHO. WHO country cooperation strategy 2009–2013: Angola 2013. [ Cited 2018 May 21]. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccs_ago_en.pdf?ua=1
- Kirigia JM, Asbu EZ. Technical and scale efficiency of public community hospitals in Eritrea: an exploratory study. Health Econ Rev. 2013;3:1–16.
- Habtom GK. Designing innovative pro-poor healthcare financing system in sub-Saharan Africa: the case of Eritrea. J Public Adm Policy Res. 2017;9:51–67.
- WHO. The world health report: health systems financing: the path to universal coverage. Geneva: WHO; 2010 [ Cited 2015 Mar 3]. Available from: http://apps.who.int/iris/bitstream/handle/10665/44371/9789241564021_eng.pdf;jsessionid=7DB9CA5BA1CAA633DB6C2C777FEF9B04?sequence=1
- Ethiopia Ministry of Health. Ethiopia’s FourthNationalHealthAccounts, 2007/2008. Addis Ababa: Ministry of Health; 2010.
- Ali EE. Healthcare financing in Ethiopia: implications on access to essential medicines. Value in Health Regional Issues. 2014;4:37–40.
- Zelelew H Healthcare financing reform in Ethiopia: improving quality and equity 2012. [ Cited 2017 Nov 22]. Available from: https://www.hfgproject.org/wp-content/uploads/2015/02/Ethiopia_Health_Care_Reform_Brief1.pdf
- Feleke S, Mitiku W, Zelelew H, et al. Ethiopia’s community-based health insurance: a step on the road to universal health coverage. Washington: World Bank Group; 2015.
- Pérez Niño H, Le Billon P. Foreign aid, resource rents, and state fragility in Mozambique and Angola. Ann Am Acad Pol Soc Sci. 2014;656:79–96.
- Tadeu BTM, Geelhoed D. “This thing of testing our blood is really very important”: a qualitative study of primary care laboratory services in Tete Province, Mozambique. Int J Equity Health. 2016;15:133.
- Brentlinger PE, Assan A, Mudender F, et al. Task shifting in Mozambique: cross-sectional evaluation of non-physician clinicians’ performance in HIV/AIDS care. Hum Resour Health. 2010;8:23.
- Visser-Valfrey M, Umarji M. Sector budget support in practice case study health sector in Mozambique. Maputo: Overseas Development Institute (ODI). 2010. [ Cited 2017 Nov 28th]. Available from: https://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/6405.pdf
- Mussa AH, Pfeiffer J, Gloyd SS, et al. Vertical funding, non-governmental organizations, and health system strengthening: perspectives of public sector health workers in Mozambique. Hum Resour Health. 2013;11:26.
- Pfeiffer J, Chapman R. An anthropology of aid in Africa. Lancet. 2015;385:2144–2145.
- WHO. WHO country cooperation strategy 2009–2013. Rwanda. Geneva: WHO regional office for Africa; 2009. [Cited 2018 May 21]. Available from: http://www.who.int/countryfocus/cooperation_strategy/ccs_rwa_en.pdf?ua=1
- Basinga P. Impact of performance -based financing on the quantity and quality of maternal health services in Rwanda. Thesis: Tulane University; 2009.
- Joharifard S, Rulisa S, Niyonkuru F, et al. Prevalence and predictors of giving birth in health facilities in Bugesera District, Rwanda. BMC Public Health. 2012;12:1049.
- Lu C, Chin B, Lewandowski JL, et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One. 2012;7:e39282.
- Kalisa I, Musange S, Collins D, et al. The development of community-based health insurance in Rwanda - experiences and lessons. Kegali:MOH. 2016. [ Cited 2016 Dec 19]. Available from: https://www.msh.org/sites/msh.org/files/the_development_of_cbhi_in_rwanda_experiences_and_lessons.pdf
- Saksena P, Antunes AF, Xu K, et al. Mutual health insurance in Rwanda: evidence on access to care and financial risk protection. Health Policy. 2011;99:203–209.
- Kalk A, Groos N, Karasi JC, et al. Health systems strengthening through insurance subsidies: the GFATM experience in Rwanda. Trop Med Int Health. 2010;15:94–97.
- Dhillon RS, Bonds MH, Fraden M, et al. The impact of reducing financial barriers on utilisation of a primary healthcare facility in Rwanda. Glob Public Health. 2012;7:71–86.
- Langer A, Horton R, Chalamilla G. A manifesto for maternal health post-2015. Lancet. 2013;381:601.
- Bhutta ZA, Salam RA, Lassi ZS, et al. Approaches to improve quality of care (QoC) for women and newborns: conclusions, evidence gaps and research priorities. Reprod Health. 2014;11:S5–S.
- Basinga P, Gertler PJ, Binagwaho A, et al. Effect on maternal and child health services in Rwanda of payment to primary health-care providers for performance: an impact evaluation. Lancet. 2011;377:1421–1428.
- Musgrove P Rewards for good performance or results: a short glossary. 2011. [ Cited 2016 Feb 26]. Available from: https://olc.worldbank.org/sites/default/files/Musgrove_2011_3.pdf
- Meessen B, Soucat A, Sekabaraga C. Performance-based financing: just a donor fad or a catalyst towards comprehensive health-care reform? Bull WHO. 2011;89:153–156.
- Soeters R, Habineza C, Peerenboom PB. Performance-based financing and changing the district health system: experience from Rwanda. Bull WHO. 2006;84:884–889.
- Omaswa F, Crisp N, eds. African health leaders: making change and claiming the future. Oxford: Oxford University Press; 2014.
- Kauzya J-M. Political decentralization in Africa: experiences of Uganda, Rwanda and South Africa. In: Decentralizing governance: emerging concepts and practices. Washington DC: Brookings Institution Press; 2007. p. 75–91.
- Reich MR, Harris J, Ikegami N, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387:811.
- Manzi A, Munyaneza F, Mujawase F, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy and Childbirth. 2014;14:290.
- Yao J, Murray AT, Agadjanian V. A geographical perspective on access to sexual and reproductive healthcare for women in rural Africa. Soc Sci Med. 2013;96:60–68.
- Fetene N, Linnander E, Fekadu B, et al. The Ethiopian health extension program and variation in health systems performance: what matters? PLoS One. 2016;11:e0156438.
- Vaz F, Bergström S. Training medical assistants for surgery. Bull WHO. 1999;77:688.
- Dovlo D. Wastage in the health workforce: some perspectives from African countries. Hum Resour Health. 2005;3:6.
- WHO. Community health workers: what do we know about them. Geneva: WHO Department of Human Resources for Health; 2007 [ Cited 2017 Jan 21]. Available from: http://www.who.int/hrh/documents/community_health_workers.pdf
- Light DW. The rhetorics and realities of community healthcare: the limits of countervailing powers to meet the healthcare needs of the twenty-first century. J Health Polit Policy Law. 1997;22:105–145.
- Dovlo D. Using mid-level cadres as substitutes for internationally mobile health professionals in Africa. A Desk Review. Human Resources for Health. 2004;2:7.
- Standing H, Amr C. Producing effective knowledge agents in a pluralistic environment: what future for community health workers? Soc Sci Med. 2008;66:2096–2107.
- Stekelenburg J, Kyanamina SS, Wolffers I. Poor performance of community health workers in Kalabo District, Zambia. Health Policy. 2003;65:109–118.
- Balabanova D, Mills A, McKee M. Good health at low cost 25 years on: lessons for the future of health systems? London: London School of Hygiene and Tropical Medicine; 2011.
- Halstead S, Walsh J, Warren K. Good health at low cost. Bellagio: Rockefeller Foundation; 1985.
- Pavignani E, Colombo A. Providing health services in countries disrupted by civil wars: a comparative analysis of Mozambique and Angola 1975–2000. Geneva:WHO. 2001. [ Cited 2017 Nov 28]. Available from: http://apps.who.int/disasters/repo/14052.pdf
- Sheikh K, Gilson L, Agyepong IA, et al. Building the field of health policy and systems research: framing the questions. PLoS Med. 2011;8:e1001073.
